Highlights
-
•
We firstly report a patient of synchronous esophagus and lung cancer with thymoma.
-
•
The video-assisted esophagectomy and VATS lobectomy and thymomectomy in a single operation are feasible and safe.
-
•
Our case illustrates a dilemma: what to do and what to expect when managing a patient with triple primary tumors.
-
•
Good clinical outcomes could be achieved with minimally invasive surgery.
Keywords: Multiple primary neoplasms, Esophageal cancer, Lung cancer, Thymoma, Minimally invasive thoracoscopic surgery
Abstract
Introduction
Reports of synchronous multiple primary tumors are very rare. We report a case of synchronous esophagus and lung cancer combined with thymoma treated with a minimally invasive approach.
Presentation of case
In a 63-year-old patient, cT2 esophageal squamous cell carcinoma was found. Chest computed tomography revealed a lesion in the right upper lobe combined with an antero-superior mediastinal mass. She was treated with one-stage bilateral video-assisted thoracoscopic + laparoscopic esophagectomy with lymph node dissection and lobectomy with complete lymphadenectomy followed by thymomectomy and demonstrated a favorable response at early follow-up, without severe adverse surgical complications and evidence of local recurrence or distant metastasis. But the long-term follow-up is still needed for the evaluation of therapeutic effects of surgery.
Discussion
In the diagnostic procedure we excluded the probability of esophageal carcinoma metastasizing to the lung. Considering the patient's physical condition permit, we performed a minimally invasive surgery for three tumors. Besides, suitable operative incisions are important for the success of surgery.
Conclusion
To our knowledge, this is the first case report in which simultaneous minimally invasive resection of esophagus and lung cancer combined with thymoma.
1. Introduction
Reports of synchronous multiple primary neoplasms have been increasing due to advances in diagnostic techniques and multimodality therapies [1]. But the synchronous triple primary tumors are very rare. We report here a case of a patient with esophagus and lung cancer combined with thymoma successfully treated by simultaneous minimally invasive resection of triple tumors.
2. Case report
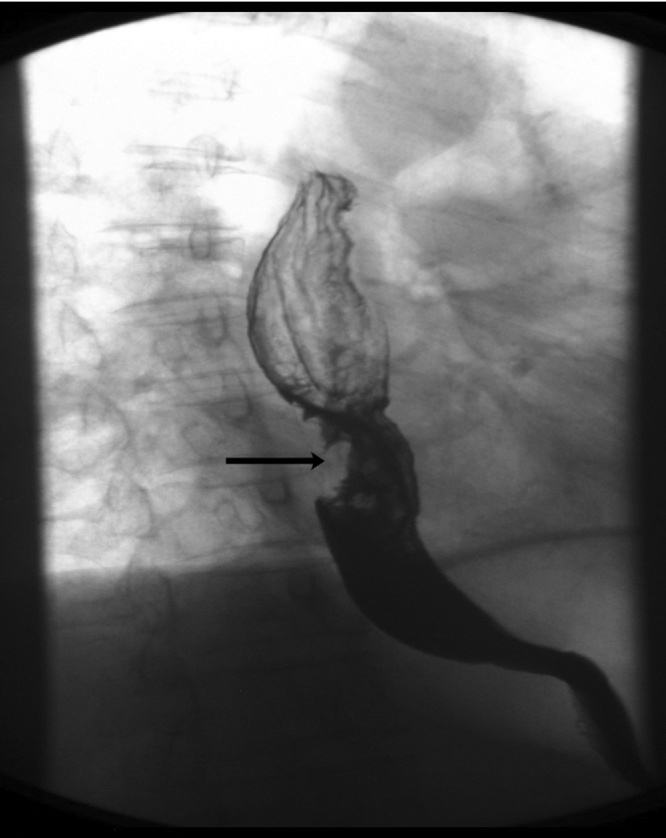
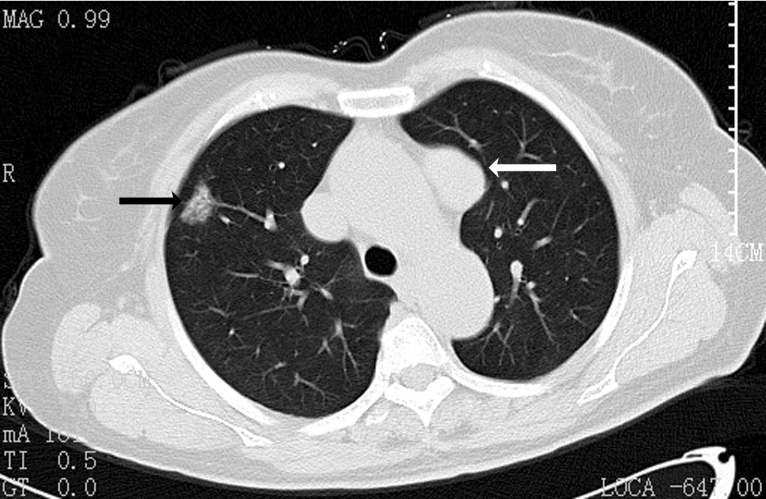
A 63-year-old woman, not an alcohol and tobacco user, was admitted to our hospital with progressive dysphagia for two months. An endoscopy was performed which found an ulcerated circumferential mass extending from 30 to 35 cm in the thoracic esophagus and histopathological examination of the biopsy showed a poorly differentiated squamous cell carcinoma (cT2). An upper gastrointestinal series revealed irregular filling defect and niche in the thoracic esophagus, the length 4.5 cm (Fig. 1). Further computed tomography (CT) of the thorax displayed the esophageal tumor with no signs of mediastinal infiltration and a 20 mm lesion in the right upper lobe, as well as an antero-superior mediastinal mass (Fig. 2). However, lymphadenopathy or distant metastasis was not observed. Endobronchial tumor growth and tumorous infiltration could be excluded bronchoscopically. Endoscopic esophageal ultrasound was not performed due to little effect on the next remedy. The patient had a 5 year history of hypertension. She had no family history of cancer and liked to eat hot food. There was no obvious abnormality in the laboratory data.
Fig. 1.
Upper gastrointestinal series revealed the tumor was in the thoracic esophagus.
Fig. 2.
CT-scan of the chest showing a ground-glass opacity in the right superior lobe (black arrow) associated with an anterior mediastinal solid lesion (white arrow).
Considering the patient’s physical condition and lung function permit, after deliberate discussion of an operational manner we performed the minimally invasive esophagectomy with two-field lymphadenectomy, the VATS right upper lobectomy associated with complete lymph node dissection and radical thymomectomy in a simultaneous surgery.
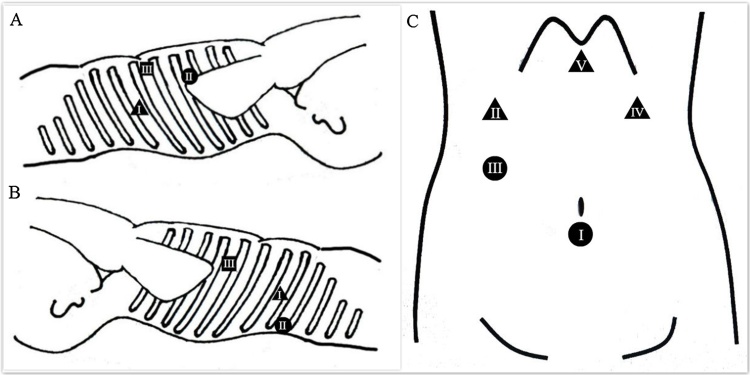
We performed the VATS thymectomy and thymomectomy first. The patient was rotated 45° to the right in a supine position following the double-lumen endotracheal intubation under general anaesthesia. The positions of trocars were shown in Fig. 3A. A mass about 4.5 × 4.5 × 3 cm was found beside the pulmonary artery in the antero-superior mediastinal space. The mediastinal pleura was incised superiorly and dissection started on the left side with careful identification of the left phrenic nerve. When the surgery was completed, the specimen was removed using an endoscopic bag.
Fig. 3.
A Port placement during VATS thymomectomy, filled triangle, 10-mm port for observation; filled circle, 20-mm port; filled square, 30-mm port. B Port placement during VATS lobectomy, filled triangle, 10-mm port for observation; filled circle, 30-mm port; filled square, 40-mm port. C Port placement in the abdomen, filled triangle, 5-mm port; filled circle, 10-mm port, I-port for observation.
The second step was the VATS lobectomy with complete lymph node dissection. The positions of trocars were shown in Fig. 3B. The patient was placed in the left-lateral decubitus. The right upper lobectomy was carried by cutting the superior vein first, followed by the superior artery and fissures, the bronchus last. Complete lymphadenectomy was then performed.
Then the video-assisted thoraco-laparoscopic esophagectomy and two-field lymphadenectomy were performed. The esophagus which was ready to remove was separated in the same position. After above procedures the patient was turned to the supine position. After five abdominal trocars (Fig. 3C) were introduced and CO2 was insufflated at a pressure of 10 mmHg to expand the abdomen, stomach mobilization and paracardial lymph node dissection were performed by an ultrasonic scalpel with the right gastroepiploic artery reserved. Intraoperative frozen section found no residual tumor at the proximal margins. Then the 4-cm wide gastric conduit was pulled up through a mediastinal route, and intrathoracic esophagogastric anastomosis was carried.
The surgical duration was 412 min and blood loss was 200 mL, without serious complications in the operation. The patient began to have liquid diet on the eighth post-operative day and no anastomotic leakage or severe infection found. The final histopathology confirmed the diagnosis of stage IIA poorly differentiated squamous cell carcinoma p-G3, p-T2, p-N0, p-R0. The histopathological result of the lung tumor showed stage IA invasive adenocarcinoma p-T1a, p-N0, p-R0. The antero-superior mediastinal mass was confirmed to be a type AB, stage I thymoma. The post-operative course was uneventful and the patient was discharged to rehabilitation after 18 days. Additionally, no further adjuvant therapy was scheduled. After six months’ follow-up there were no signs of recurrence.
3. Discussion
The coincidence of synchronous triple primary tumors is rare. Until now, only a few cases of multiple primary neoplasms have been reported [2], [3], [4]. The mechanisms of this association are still not clear. The clinical negligence may lead to missed diagnosis, so appropriate and comprehensive examination is important for correct diagnosis and prompt treatment.
In the present case, we thought the probability of esophageal carcinoma metastasizing to the lung was existed in the beginning. But the chest CT revealed the lesion was ground-glass. Border irregularity and pleural indentation were also found, which not metastatic signs. So we diagnosed she mostly got synchronous primary esophagus and lung cancer combined with thymoma. The final postoperative histopathological results approved the assumption. Therefore, appropriate examination and accurate staging of each cancer are obviously mandatory to plan a safe operation. But we still considered the histopathological diagnosis was amazing for each of the three synchronous tumors in the relatively early stage.
Synchronous resection is apparently the optimal treatment for cancer patients who have no else organ and lymph node metastasized. However, esophagectomy is a highly invasive surgery and especially simultaneous surgery for three tumors, including lymphadenectomy, may induce severe, even life-threatening complications. Recently, a staged surgery, for example a two-stage operation, can reduce adverse effects of the concurrent surgery, although it is possible that this could delay treatment for the second cancer. And the interval time between two surgeries is indefinable. Ishii et al. reported four cases of double carcinoma of the esophagus and the lung and thought a two-stage operation is considered a suitably safe surgical procedure [5].
Compared with open surgery, patients undergoing minimally invasive surgery may benefit from smaller incisions, lower blood loss and shorter hospital stay. However, better evidence on outcomes is needed before any claims can be made for the superiority of the minimally invasive approach. Besides, suitable operative incisions are important for the success of surgery. Overall, the synchronous minimally invasive surgery was a preferred choice for the patient in this case. To our knowledge, this is the first case report in which simultaneous minimally invasive resection of esophagus and lung cancer combined with thymoma. We confirm that the video-assisted thoraco-laparoscopic esophagectomy and VATS lobectomy and thymomectomy in a single operation are feasible and safe.
Conflict of interest
None declared.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Funding
This work was not supported by any funding agency.
Ethical approval
Yes.
Consent
This research had obtained the ethics committee approval in our hospital.
Author contribution
Study concept or design: Fengmin Wang.Data collection: Xiao Song, Haibo Shen.Writing the paper: Xiao Song, Jie Li.
Guarantor
Xiao Song.
References
- 1.Li F., Zhong W.Z., Niu F.Y., Zhao N., Yang J.J., Yan H.H., Wu Y.L. Multiple primary malignancies involving lung cancer. BMC Cancer. 2015;15:696. doi: 10.1186/s12885-015-1733-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Honda M., Daiko H., Kinoshita T., Fujita T., Shibasaki H., Nishida T. Minimally invasive resection of synchronous thoracic esophageal and gastric carcinomas followed by reconstruction: a case report. Surg. Case Rep. 2015;1:12. doi: 10.1186/s40792-015-0018-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dolci G., Dell’Amore A., Asadi N., Caroli G., Greco D., Stella F., Bini A. Synchronous thymoma and lung adenocarcinoma treated with a single mini-invasive approach. Hear. Lung Circ. 2015;24:e11–e33. doi: 10.1016/j.hlc.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Lindenmann J., Matzi V., Maier A., Smolle-Juettner F.M. Transthoracic esophagectomy and lobectomy performed in a patient with synchronous lung cancer and combined esophageal cancer and esophageal leiomyosarcoma. Eur. J. Cardiothorac. Surg. 2007;31:322–324. doi: 10.1016/j.ejcts.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Ishii H., Sato H., Tsubosa Y., Kondo H. Treatment of double carcinoma of the esophagus and lung. Gen. Thorac. Cardiovasc. Surg. 2008;56:126–130. doi: 10.1007/s11748-007-0200-0. [DOI] [PubMed] [Google Scholar]