Abstract
Palytoxin is one of the most potent toxins known to mankind and poses a high risk to humans through ingestion, inhalation and dermal routes [1,2]. Although the exact mechanism of action is unknown it is postulated that palytoxin binds to the Na+/K + ATPase pump resulting in K+ efflux, Ca2+ influx and membrane depolarization leading to widespread secondary pharmacological actions [2]. Palytoxin is highly toxic and can affect multiple organs causing severe symptoms including death. Palytoxin poisoning is mainly developed after ingesting seafood. We are reporting a case of suspected inhalational palytoxin poisoning in a healthy healthcare provider from who developed severe respiratory distress within 12 hours of exposure to vapors. We have highlighted diagnostic clues and clinical features in the patients' history that may help intensivists to diagnose a case of ARDS secondary to palytoxin poisoning.
1. Introduction
Palytoxin is one of the most potent toxins known to mankind and poses a high risk to humans through ingestion, inhalation and dermal routes [1], [2]. Although the exact mechanism of action is unknown it is postulated that palytoxin binds to the Na+/K + ATPase pump resulting in K+ efflux, Ca2+ influx and membrane depolarization leading to widespread secondary pharmacological actions [2]. Palytoxin is highly toxic and can affect multiple organs causing severe symptoms including death. Palytoxin poisoning is mainly developed after ingesting seafood. We are reporting a case of suspected inhalational palytoxin poisoning in a healthy healthcare provider from who developed severe respiratory distress within 12 hours of exposure to vapors. We have highlighted diagnostic clues and clinical features in the patients' history that may help intensivists to diagnose a case of ARDS secondary to palytoxin poisoning.
2. Case report
We present the case of a 61-year-old male from Danville, PA who presented to the local hospital with fever, chills and shortness of breath. The previous night he was cleaning his salt-water aquarium and noted corals on the rocks of the aquarium, which he proceeded to clean with boiled water and vinegar. The subject reported having an itchy sensation in his throat, cough, runny nose, sweating and myalgia. Overnight the symptoms progressed to include shortness of breath. His wife alerted EMS after almost 2 hours of continued symptoms. At the time of admission to the ED, his temp. was 101 °F and RR was 30/min. Initial lab results reported BUN 31 mg/dL, Creatinine 1.86 mg/dL and WBC 27 K/mcL. Furthermore, an ABG test reported a PaO2/FiO2 (PF) ratio of 170 (N:300–500) and a chest X-ray showed bilateral infiltrates (Fig. 1).
Fig. 1.
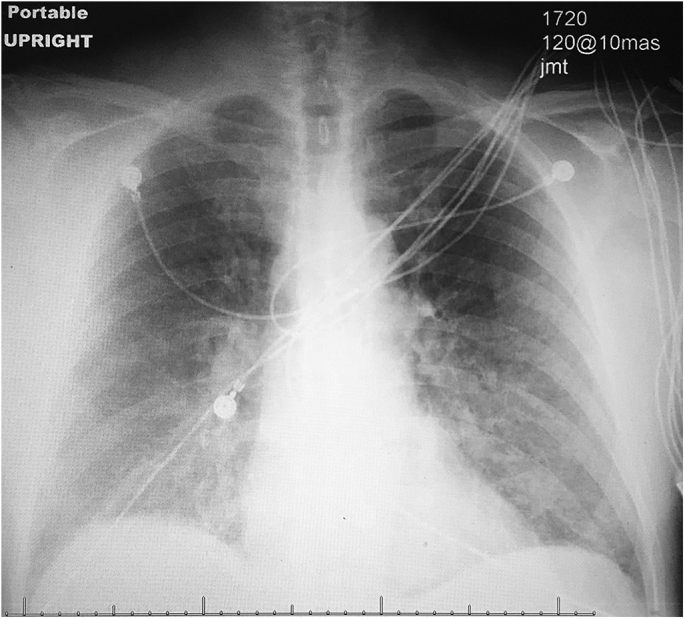
Chest X-ray showing bilateral infiltrates on 1st day of admission.
He was treated with IV steroid, Ranitidine, Benadryl, Albuterol, Lorazepam, Levofloxacin and Ketorolac.
Due to worsening respiratory status the subject was transferred to our center for ICU admission and further management. Upon evaluation he was alert and orientated to time, location and person while respiratory distress continued and a cough with pink frothy sputum had emerged. Chest auscultation revealed occasional wheezing and bibasilar crackles. On admission, lab results reported BUN 30 mg/dL, creatinine 2 mg/dL, Na 137 mEq/L, K 4.2 mEq/L, WBC 31 K/mcL, and Procalcitonin 7.09 ng/mL (N: <0.05 ng/mL). ABG showed worsening hypoxia with a PF ratio of 120. The subject refused intubation so Non-invasive mechanical ventilation (CPAP) was utilized with PEEP of 10 cmH2O and he responded well with conservative management. On day three, after improvement in symptoms and chest radiograph CPAP was discontinued (Fig. 2).
Fig. 2.
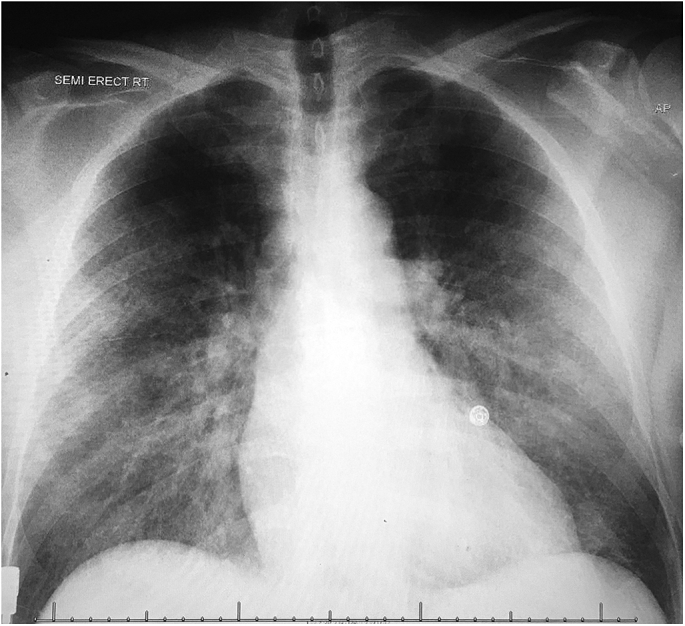
Chest X-ray showing improvement on the 3rd day of admission.
He was transferred to regular floor with the intent to discharge thefollowing day.
3. Discussion
Palytoxin is heat-stable, therefore boiling water is not effective in eliminating the toxin [3]. Poisonings associated with palytoxin contaminated soft corals occur via different routes such as oral, cutaneous, inhalational or ocular exposure. Oral exposure is the most harmful route of human exposure while palytoxin toxicity after cutaneous and inhalational exposure also represents a grave problem for human health [2]. Common symptoms include numbness, paraesthesia and swelling around the site of exposure (cutaneous exposure), rhinorrhea, cough, dyspnea (inhalational exposure), perioral paraesthesia, dysgeusia (oral exposure) and eye irritation (ocular exposure) [1], [2].
An increasing number of palytoxin poisonings secondary to inhalational exposure have been reported. In 2005, 200 patients reported inhalational exposure to palytoxin after algal bloom in Italy [4]. Patients presented with fever, cough, sore throat and dyspnea. In another case of suspected palytoxin inhalation exposure in Virginia, the patient developed respiratory symptoms after pouring boiling water over the zoanthid coral [1], [2]. Common clinical presentations including fever and cough appear suddenly, from minutes to hours, after cleaning or destruction of coral with boiling water [3], [5], [6]. Upon examination patients were febrile, tachypneic, tachycardic, some had wheezing and laboratory investigation consistently revealed leukocytosis. In all cases treatment was supportive, such as corticosteroid [3], [5], [6]. Patients were admitted and supportive treatment was provided for mild to severe respiratory reactions [3], [5], [6].
Our patient was trying to clean a salt-water aquarium with boiling water and inhaled steam during the process. This was followed by the development of his symptoms including shortness of breath and myalgia. Rhabdomyolysis has been described in cases of palytoxin toxicity [7] however our patient did not have an elevated CK level. He developed shortness of breath which progressed to acute hypoxic respiratory failure, likely due to pulmonary edema. He refused intubation, so bronchoscopy for Broncho Alveolar Lavage(BAL) analysis was not possible. Our patient had severe ARDS, As per Berlin criteria; clinically developed acute lung injury within 1 week of an apparent clinical insult, had bilateral opacities on chest radiograph, had respiratory failure without volume overload or heart failure and a PF ratio of ≤100 mmHg. He was delivered 10 cmH2O of PEEP when his PF decreased rapidly.
Pre-clinical studies have demonstrated that palytoxin is a potent vasoconstrictor in the renal and coronary vasculature [8], [9]. Vasodilators such as nitrates have been proposed as an antidote [10]. It was also shown that palytoxin can stimulate mast cells to release histamine and increase histidine decarboxylase activity [11], [12]. This could be the possible etiology of the itching of throat, wheeze and other symptoms in our patient. However, there is no known antidote for palytoxin poisoning and treatment is generally focused on meticulous supportive care [3].
It has long been known among aquarium hobbyists that coral may cause poisoning by cutaneous, inhalation and/or ocular exposure. Since the 1980s the popularity and trade of home aquaria containing living corals has dramatically increased. As a result, concern has been raised about the possible adverse effects and impact on human health from the maintenance and manipulation of these corals [1], [2]. In home aquaria these corals find favorable conditions to proliferate and eventually accumulate toxic compounds. Targatoline et al. demonstrated that the presence of high levels of palytoxins (palytoxin and hydroxypalytoxin) in both soft coral and seawater from a home marine aquarium was involved in the poisoning of an entire family. Based on the chemical and symptomatological data palytoxins were implicated in their respiratory disorders. Despite the proven toxicity, the risk posed by keeping soft corals in home aquaria are mostly underestimated and unrecognized by the store owners and aquarium hobbyists. On top of that, these corals are sold without any warning about their toxic potential or guidelines for their use and maintenance. It is a burgeoning yet still underestimated sanitary problem.
The confirmatory diagnosis of palytoxin toxicity is difficult as detection of the toxin requires liquid chromatography which is not available at most medical centers. Our patients' symptoms after exposure, clinical presentation and improvement with supportive care are suggestive of palytoxin toxicity. The management of palytoxin is supportive [3] and no antidotes are available for human treatment.
4. Summary
In our case High-Pressure Liquid Chromatography was not done due to lack of availability. It was also not possible to obtain the original coral to detect palytoxin because it was destroyed. Thus, the diagnosis was based on the clinical presentation and synchronicity of symptomatic onset which were highly suggestive of inhalational exposure to a toxin from the coral species in their home aquarium. Due to variable presentation and lack of confirmatory marker, palytoxin poisoning is rarely reported. It should be considered as a differential in patients who own or work with fish tanks and present with respiratory complaints, hemolysis, myalgia, neuromuscular dysfunction, and cardiac toxicity. Palytoxin toxicity remains a potential poison with little public and professional awareness. There is a need for improved awareness among aquarium enthusiast and medical professionals.
Source(s) of support
There was no source of support.
Presentation at a meeting
This case report was not presented at any meeting.
Conflicting interest
There is none.
Contributor Information
Lokendra K. Thakur, Email: lthakur@geisinger.edu.
Kunal K. Jha, Email: kunaljhamd@gmail.com.
References
- 1.Deeds J.R., Schwartz M.D. Human risk associated with palytoxin exposure. Toxicon Off. J. Int. Soc. Toxinol. 2010;56:150. doi: 10.1016/j.toxicon.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 2.Tubaro A., Durando P., Del Favero G. Case definitions for human poisonings postulated to palytoxins exposure. Toxicon Off. J. Int. Soc. Toxinol. 2011;57:478. doi: 10.1016/j.toxicon.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Sud P., Su M.K., Greller H.A., Majlesi N., Gupta A. Case series: inhaled coral vapor—toxicity in a tank. J. Med. Toxicol. 2013;9(3):282–286. doi: 10.1007/s13181-013-0307-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Durando P., Ansaldi F., Oreste P. Ostreopsis ovata and human health: epidemiological and clinical features of respiratory syndrome outbreaks from a two-year syndromic surveillance, 2005–06, in north-west Italy. Euro Surveill. 2007;12 doi: 10.2807/esw.12.23.03212-en. E070607.1. [DOI] [PubMed] [Google Scholar]
- 5.Bernasconi M., Berger D., Tamm M., Stolz D. Aquarism: an innocent leisure activity? Palytoxin-induced acute pneumonitis. Respiration. 2012;84:436–439. doi: 10.1159/000338789. [DOI] [PubMed] [Google Scholar]
- 6.Snoeks L., Veenstra J. Family with fever after cleaning a sea aquarium. Ned. Tijdschr. Geneeskd. 2012;156:A4200. [PubMed] [Google Scholar]
- 7.Okano H., Masuoka H., Kamei S. Rhabdomyolysis and myocardial damage induced by palytoxin, a toxin of blue humphead parrotfish. Intern Med. 1998;37:330–333. doi: 10.2169/internalmedicine.37.330. [DOI] [PubMed] [Google Scholar]
- 8.Ramos V., Vasconcelos V. Palytoxin and analogs: biological and ecological effects. Mar. Drugs. 2010;8:2021–2037. doi: 10.3390/md8072021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kockskamper J., Ahmmed G.U., Zima A.V., Sheehan K.A., Glitsch H.G., Blatter L.A. Palytoxin disrupts cardiac excitation-contraction coupling through interactions with P-type ion pumps. Am. J. Physiol. Cell Physiol. 2004;287:C527–C538. doi: 10.1152/ajpcell.00541.2003. [DOI] [PubMed] [Google Scholar]
- 10.Wiles J.S., Vick J.A., Christensen M.K. Toxicological evaluation of palytoxin in several animal species. Toxicon. 1974;12:427–433. doi: 10.1016/0041-0101(74)90011-7. [DOI] [PubMed] [Google Scholar]
- 11.Kitamura Y., Taguchi T., Yokoyama M., Tamai M., Yamatodani A., Watanabe T. Increase in histidine decarboxylase activity in mouse skin after application of tumor promoters. Princess Takamatsu Symp. 1983;14:327–334. [PubMed] [Google Scholar]
- 12.Chhatwal G.S., Ahnert-Hilger G., Beress L., Habermann E. Palytoxin both induces and inhibits the release of histamine from rat mast cells. Int. Arch. Allergy Appl. Immunol. 1982;68:97–100. doi: 10.1159/000233075. [DOI] [PubMed] [Google Scholar]


