Abstract
Purpose
To determine the value of the 2D multiple-echo data image combination (MEDIC) sequence relative to the short-tau inversion recovery (STIR) sequence regarding the depiction of chondral lesions in the patellofemoral joint.
Materials and methods
During a period of 6 month patients with acute pain at the anterior aspect of the knee, joint effusion and suspected chondral lesion defect in the patellofemoral joint underwent MRI including axial MEDIC and STIR imaging. Patients with chondral lesions in the patellofemoral joint on at least one sequence were included. The MEDIC and STIR sequence were quantitatively compared regarding the patella cartilage-to-effusion contrast-to-noise ratio (CNR) and qualitatively regarding the depiction of chondral lesions independently scored by two radiologists on a 3-point scale (1 = not depicted; 2 = blurred depicted; 3 = clearly depicted) using the Wilcoxon-Mann-Whitney-Test. For the analysis of inter-observer agreement the Cohen's Weighted Kappa test was used.
Results
30 of 58 patients (male: female, 21:9; age: 44 ± 12 yrs) revealed cartilage lesions (fissures, n = 5 including fibrillation; gaps, n = 15; delamination, n = 7; osteoarthritis, n = 3) and were included in this study. The STIR-sequence was significantly (p < 0.001) superior to the MEDIC-sequence regarding both, the patella cartilage-to-effusion CNR (mean CNR: 232 ± 61 vs. 40 ± 16) as well as the depiction of chondral lesion (mean score: 2.83 ± 0.4 vs. 1.75 ± 0.7) with substantial inter-observer agreement in the rating of both sequences (κ = 0.76–0.89).
Conclusion
For the depiction of chondral lesions in the patellofemoral joint, the axial STIR-sequence should be chosen in preference to the axial MEDIC-sequence.
Abbreviations: STIR, short-tau inversion recovery sequence; MEDIC, 2D multiple-echo data image combination sequence
Keywords: MRI, Chondral Lesion, Patellofemoral Joint, STIR, MEDIC
1. Introduction
Chondral lesions in the patellofemoral joint are the most common cause for acute pain at the anterior aspect of the knee. They can be roughly divided in cartilaginous fissures or gaps. When the fissure is located at the medial retro patellar aspect and a plica mediopatellaris exists, it is assumed that the fissure is caused by the plica as incision injury so that the removal of the plica is indicated to prevent further cartilaginous incision injuries. How to prevent cartilaginous gap injuries is unclear. However, the method of choice to diagnose chondral lesions is MRI. There are cartilage specific gradient echo sequences like the 2D multiple-echo data image combination sequence (MEDIC) which are used in musculoskeletal imaging to delineate cervical disc herniation, tiny ligaments such as the scapholunate ligament [2], labrum injuries such as the Bankart lesion, calcific deposits like in tendinitis calcarea or loose bodies in the joint. This sequence is used to determine the thickness of the cartilage and can be performed in 3D to quantify and map the volume of the cartilage. On the other hand, there are spin echo sequences which in contrast to the gradient echo-sequence better demarcate bone marrow edema when fat suppressed. In addition, these sequences provide a kind of indirect arthrography due to the high contrast between cartilage and surrounding fluid. Thus, the short-tau inversion recovery sequence (STIR) seems to be the optimal sequence to demarcate both, tiny cartilaginous fissures and bone marrow edema as their consequence. However, the value of the MEDIC is still unclear. The Medic has been only absolutely assessed but not relatively to other sequences Schmid MR et al. [1]. Thus, the purpose of our study was to determine the value of the 2D multiple-echo data image combination sequence relative to the short-tau inversion recovery sequence regarding the depiction of chondral lesions in the patellofemoral joint.
2. Materials and methods
During a period of 6 month patients with acute pain at the anterior aspect of the knee, joint effusion and suspected chondral lesion in the patellofemoral joint underwent MRI including axial MEDIC and STIR imaging. The study was approved by the local ethics committee. Informed consent was obtained from all patients.
MRI was performed on a 70 cm open bore and 125 cm short 1.5T scanner (MAGNETOM Espree, Siemens Healthcare, Erlangen, Germany) using a circular polarized knee coil. The MRI protocol is outlined in Table 1.
Table 1.
MR Imaging protocol.
| Sequence | plane | fat saturation | TR/TE/flip/TI | matrix | voxel size | TA |
|---|---|---|---|---|---|---|
| T2w | sagittal | + | 3440/45 | 384 | 0.5 × 0.5 × 3 mm | 3:59 |
| T1w | sagittal | 692/15 | 448 | 0.4 × 0.4 × 3 mm | 3:47 | |
| PD | coronal | + | 3360/31 | 384 | 0.5 × 0.4 × 3 mm | 3:00 |
| STIR (2D) | axial | 6870/60/160 | 320 | 0.7 × 0.6 × 3 mm | 3:07 | |
| MEDIC (2D) | axial | 472/24/30° | 384 | 0.5 × 0.4 × 3 mm | 3:28 |
Only patients with chondral lesions in the patellofemoral joint on at least one MRI sequence were elected for sequence comparison.
2.1. Objective/quantitative Comparison
The MEDIC and STIR sequence were quantitatively compared regarding the patella cartilage-to-effusion contrast-to-noise ratio (CNR). For that purpose the mean signal intensity (SI) of retropatellar cartilage and effusion as well as the standard deviation (SD) of air were measured by standardized region-of-interest (ROI) measurement at the level of the chondral lesion with 3–6 mm diameter depending on the thickness of the retropatellar cartilage. The standard deviation of air served as noise, so that CNR was calculated according to the formula: CNR: = (SIcartilage − SIEffusion)/SDair
2.2. Subjective/qualitative Comparison
The MEDIC and STIR sequence were qualitatively compared by two radiologists with 2 and 6 years experiences in musculoskeletal imaging who independently scored the depiction of the chondral lesion on a 3-point scale (1 = not depicted; 2 = blurred depicted; 3 = clearly depicted).
2.3. Statistical analysis
The comparison in objective CNR and subjective rating was performed by the Wilcoxon-Mann-Whitney-Test using a p-value less than 0.05 as level of significance. Inter-observer agreement was analyzed with Cohen κ analysis using the four categories in agreement: fair (κ = 0.21–0.40), moderate (κ = 0.41–0.60), substantial (κ = 0.61–0.80), almost perfect (κ = 0.81–1.00) [3].
3. Results
30 of 58 patients (male: female, 21:9; age: 44 ± 12 yrs) revealed cartilage lesions (fissures, n = 5 (Fig. 1, Fig. 2) including fibrillation (Fig. 3); gaps, n = 15 (Fig. 4, Fig. 5); delamination, n = 7 (Fig. 6); osteoarthritis, n = 3) and were included in this study. The STIR-sequence was significantly (p < 0.001) superior to the MEDIC-sequence regarding both, the patella cartilage-to-effusion CNR (mean CNR: 232 ± 61 vs. 40 ± 16) as well as the depiction of chondral lesion (mean score: 2.83 ± 0.4 vs. 1.75 ± 0.7) with substantial inter-observer agreement in the rating of both sequences (κ = 0.76-0.89).
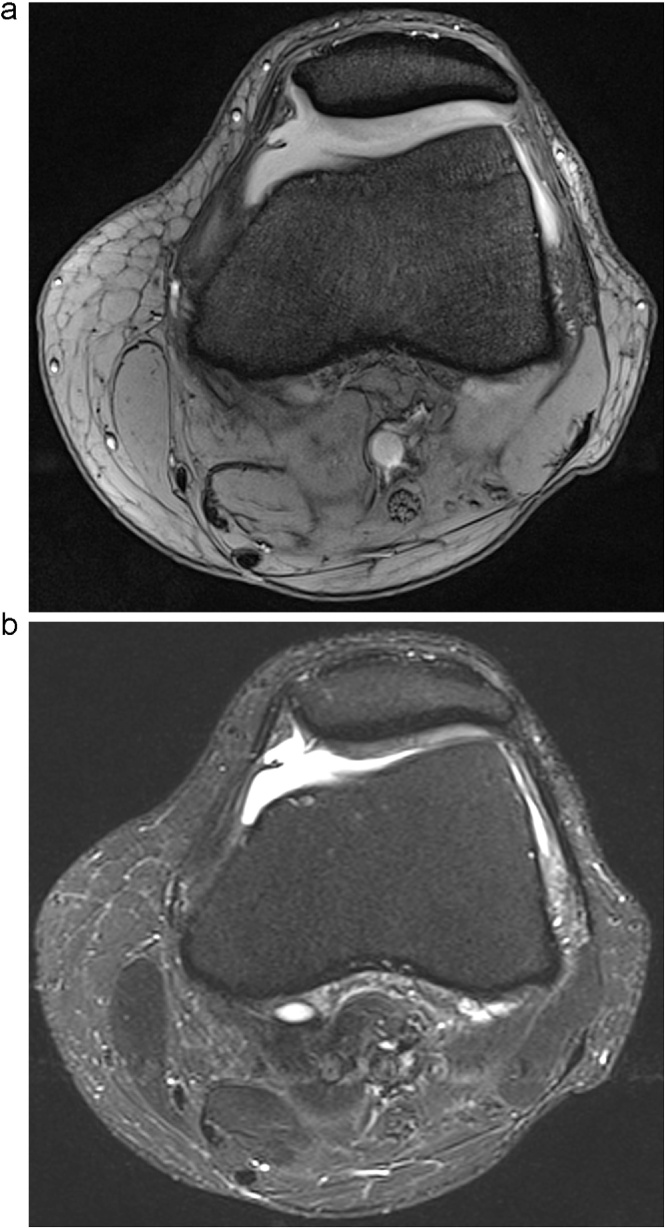
Fig. 1.
Cartilaginous fissure of the medial aspect of the patella imaged with MEDIC (a) and STIR (b). The fissure is presumably caused by a plica mediopatellaris as incision injury. The chondropathia patellae is better depicted by the STIR-sequence (b) due to the higher cartilage-to-effusion contrast-to-noise ratio (STIR = 219 vs. MEDIC = 20).
Fig. 2.
Cartilage damage imaged with MEDIC (a) and STIR (b). The cartilage lesion is better depicted by the STIR-sequence (b) due to the higher cartilage-to-effusion contrast-to-noise ratio (STIR = 215 vs. MEDIC = 26).
Fig. 3.
Fibrillation of the retropatellar cartilage imaged with MEDIC (a) and STIR (b). The chondropathia patellae is better depicted by the STIR-sequence (b). In contrast to the MEDIC the STIR also depicts subchondral bone edema due to the higher cartilage-to-effusion contrast-to-noise ratio (STIR = 197 vs. MEDIC = 32).
Fig. 4.
Cartilage lesion in the femoral sulcus imaged with MEDIC (a) and STIR (b). The lesion is better depicted by the STIR-sequence (b) due to the higher cartilage-to-effusion contrast-to-noise ratio (STIR = 215 vs. MEDIC = 34).
Fig. 5.
Focal cartilage damage imaged with MEDIC (a) and STIR (b). The lesion is better depicted by the STIR-sequence (b) due to the higher cartilage-to-effusion contrast-to-noise ratio (STIR = 205 vs. MEDIC = 23).
Fig. 6.
Retropatellar delamination imaged with MEDIC (a) and STIR (b). The delamination is better depicted by the STIR-sequence (b) due to the higher cartilage-to-effusion contrast-to-noise ratio (STIR = 231 vs. MEDIC = 29).
4. Discussion
Our results show that the STIR-sequence is significantly superior to the MEDIC-sequence regarding the depiction of chondral lesions in the patellofemoral joint (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6). Thus, the STIR-sequence should be preferred over the MEDIC-sequence for the depiction of chondral lesions in the patellofemoral joint.
Although the MEDIC-sequence provides a higher spatial resolution (0.5 × 0.4 mm vs. 0.7 × 0.6 mm) (Tab. 1) it masks tiny injuries like fissures (Fig. 1, Fig. 2), defibrillation (Fig. 3) or delamination (Fig. 6). Due to the high prevalence of mediopatellar plica in up to 80% of cases [4] and its association with cartilage damage [5], [6] the depiction of plica induced cartilage damage seems crucial. In contrast to the MEDIC-sequence the STIR- sequence also depicts reactive edemas in the bone marrow as indirect sign of cartilage stress or damage (Fig. 3). Furthermore, edema depiction facilitates the assessment of severity, acuteness and consequence of cartilage stress or damage (Fig. 3). Also, the STIR-sequence gave better depiction of the liquid film under the delamination, highlighting this pathology (Fig. 6).
Both, the objective analysis and subjective analysis with substantial inter-observer agreement accordingly confirm the superiority of the STIR-sequence. We saw no advantage for the T2*-weighting of the MEDIC-sequence in the depiction of chondral lesions in the patellofemoral joint. On the MEDIC the cartilage signal was homogeneous in every case thus any inner inhomogeneity reflecting pressure induced focal dehydration was not resolved. The MEDIC-sequence may be superior to the STIR-sequence in the depiction of loose bodies in the joint due to its higher (not saturated) contrast between fat in tissue and bone. However, in the one case with a loose body in the patellofemoral joint there was no difference in the depiction of the loose body between the MEDIC and STIR-sequence. There was also no difference in the depiction of the plica mediopatellaris, which is anyway also and even better depicted on the sagittal fat-saturated T2 w sequence in the protocol of the entire knee.
A mixed T1/T2*-weighted so-called double-echo steady state (DESS) sequence has also been proposed as a cartilage specific sequence. The DESS-sequence is currently being used in the Osteoarthritis Initiative to assess the cartilage of the knee joint [7]. Regarding the cartilage-to-effusion contrast there seems to be no significant difference between the MEDIC- and DESS-sequence. Ruehm et al. [8] also used the model of the patellar cartilage to evaluate the diagnostic value of the DESS-sequence and found that the DESS-sequence was inferior to the conventional T2 w spin echo (SE)-sequence. Both, the MEDIC- and DESS-sequence provide less contrast than the STIR-sequence for both, bone edema and cartilage injuries. Thus, the STIR-sequence combines the advantage of indirect arthrography with delineation of subchondral edema. However, the MEDIC and DESS 3D-sequences provide mapping of the cartilage volume with the intention to facilitate the prevention of osteoarthritis, thus providing prophylactic meaning. In contrast, the STIR-sequence depicts focal damage of the cartilage and bone marrow edema as causes of pain. If other prior performed sequences reveal an effusion as indirect sign of damage we therefore prefer the STIR-sequence to better depict the cause for the effusion. In the younger patient group (here with a mean age of 44 ± 12 years (range: 21–68 years)) with acute pain and effusion in the PFJ in particular, the STIR-sequence seems to be more helpful in directing therapy decisions as the pretest-probability cause of pain and effusion is less likely to be chronic.
We did not compare the STIR sequence with the fat-saturated T2w or PD sequences because the STIR-fat saturation is known to optimally depict bone edema, which seems crucial to indicate lateral release or any other surgical procedure to prevent or treat osteoarthritis. In this manner, the knee protocol (Table 1) also includes the maximum of bone edema-to-bone contrast.
The study is limited through the lack of a standard of reference. Thus, for the benefit of non-invasiveness we compared the sequences regarding the cartilage-to-effusion CNR and depiction of lesion and not regarding their accuracy in the lesion detection. But the significant superiority of the STIR over the MEDIC sequence in both, the objective and subjective analysis is so clear that it seems not likely that the lack of a standard of reference biases the message of the study.
4.1. Conclusion
The STIR sequence should be preferred over the MEDIC sequence for the depiction of chondral lesions in the patellofemoral joint.
Conflict of Interest Statement
-
•
There is no actual or potential conflict of interest in relation to this article (no disclosures).The work has not been published before
-
•
No funding was received for this work.
-
•
This paper describes the authorś own work.
-
•
It is not under consideration elsewhere, and all authors have read and approved the manuscript.
References
- 1.Schmid M.R., Pfirrmann C.W., Koch P., Zanetti M., Kuehn B., Hodler J. Imaging of patellar cartilage with a 2D multiple-echo data image combination sequence. AJR Am. J. Roentgenol. 2005;184(6):1744–1748. doi: 10.2214/ajr.184.6.01841744. [DOI] [PubMed] [Google Scholar]
- 2.Pahwa S., Srivastava D.N., Sharma R., Gamanagatti S., Kotwal P.P., Sharma V. Comparison of conventional MRI and MR arthrography in the evaluation wrist ligament tears: a preliminary experience. Indian J. Radiol. Imaging. 2014;24(3):259–267. doi: 10.4103/0971-3026.137038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen J. A coefficient of agreement for nominal scales. Educ. Psychol. Meas. 1960;20:37–46. [Google Scholar]
- 4.Nakayama A., Sugita T., Aizawa T., Takahashi A., Honma T. Incidence of medial plica in 3,889 knee joints in the Japanese population. Arthroscopy. 2011;27(11):1523–1527. doi: 10.1016/j.arthro.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Hayashi D., Xu L., Guermazi A., Kwoh C.K., Hannon M.J., Jarraya M. Prevalence of MRI-detected mediopatellar plica in subjects with knee pain and the association with MRI-detected patellofemoral cartilage damage and bone marrow lesions: data from the Joints On Glucosamine study. BMC Musculoskel. Disord. 2013;14:292. doi: 10.1186/1471-2474-14-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christoforakis J.J., Sanchez-Ballester J., Hunt N., Thomas R., Strachan R.K. Synovial shelves of the knee: association with chondral lesions. Knee Surg. Sports Traumatol. Arthrosc. 2006;14(12):1292–1298. doi: 10.1007/s00167-006-0085-y. [DOI] [PubMed] [Google Scholar]
- 7.Peterfy C.G., Schneider E., Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee Osteoarthritis and cartilage/OARS. Osteoarthritis Res. Soc. 2008;16(12):1433–1441. doi: 10.1016/j.joca.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruehm S., Zanetti M., Romero J., Hodler J. MRI of patellar articular cartilage: evaluation of an optimized gradient echo sequence (3D-DESS) J. Magn. Reson. Imaging JMRI. 1998;8(6):1246–1251. doi: 10.1002/jmri.1880080611. [DOI] [PubMed] [Google Scholar]