Abstract
Background and Objectives
Compared with conventional treatment, early surgery significantly reduced the composite end point of all-cause death and embolic events during hospitalization, but long-term data in this area are lacking. This study sought to compare long-term outcomes of early surgery with a conventional treatment strategy in patients with infective endocarditis (IE) and large vegetations.
Subjects and Methods
The Early Surgery versus Conventional Treatment in Infective Endocarditis (EASE) trial randomly assigned patients with left-sided IE, severe valve disease and large vegetation to early surgery (37 patients) or conventional treatment groups (39 patients). The pre-specified end points were all-cause death, embolic events, recurrence of IE and repeat hospitalizations due to the development of congestive heart failure occurring during follow-up.
Results
There were no significant differences between the early surgery and the conventional treatment group in all-cause mortality at 4 years (8.1% and 7.7%, respectively; hazard ratio [HR] 1.04; 95% CI, 0.21 to 5.15; p=0.96). The rate of the composite end point of death from any cause, embolic events or recurrence of IE at 4 years was 8.1% in the early surgery group and 30.8% in the conventional treatment group (HR, 0.22; 95% CI, 0.06-0.78; p=0.02). The estimated actuarial rate of end points at 7 years was significantly lower in the early surgery group than in the conventional treatment group (log-rank p=0.007).
Conclusion
There was a substantial benefit in having early surgery for patients with IE and large vegetations whose health was sustained up to 7 years, and late clinical outcome after surgery was excellent in survivors of IE. (EASE clinicaltrials.gov identifier: NCT00750373)
Keywords: Infective endocarditis, Echocardiography, Embolism, Valvular heart disease, Cardiac surgery
Introduction
Despite improvements in medical and surgical treatment, infective endocarditis (IE) remains a serious disease that carries considerable mortality and morbidity.1),2),3),4) The Early Surgery versus Conventional Treatment in Infective Endocarditis (EASE) trial previously demonstrated that early surgery in patients with IE and large vegetations significantly reduced the composite end point of all-cause death and embolic events during hospitalization when compared with conventional treatment.5) However, there was no significant difference in all-cause mortality rates at 6 months and more patients treated with early surgery received valve replacement than patients who were treated conventionally.5) Long-term risks of mortality and morbidity in IE survivors who underwent early surgery or experienced systemic embolic events remain controversial.4),6),7),8),9) This study reports the long-term outcomes of the EASE trial.
Subjects and Methods
Study design
The EASE trial design has been previously reported.5) Briefly, we enrolled consecutive patients who were at high risk for embolisms and had a left-sided, native valve IE. For all patients suspected of IE, blood cultures were obtained and a transthoracic echocardiography was performed within 24 hours after hospitalization. Patients with definite IE according to the modified Duke criteria10) were eligible for enrollment if they had severe mitral or aortic valve disease and a vegetation diameter >10 mm. In line with the 2006 American College of Cardiology/American Heart Association guidelines on surgical indications for IE,11) the exclusion criteria were defined as patients with moderate to severe congestive heart failure (CHF), IE complicated by heart block, annular or aortic abscess, or destructive penetrating lesions requiring urgent surgery, fungal endocarditis, those who were not candidates for early surgery on the basis of age >80 years, coexisting major embolic stroke with a risk of hemorrhagic transformation at the time of diagnosis, and/or poor medical status, such as the presence of malignancy. Patients with prosthetic valve IE, right-sided vegetations, small vegetations with a diameter ≤10 mm and patients referred from other hospitals more than 7 days after the diagnosis of IE were also excluded. The trial enrollment period was September 2006 through March 2011. Patients were randomly assigned on a 1:1 basis to early surgery or conventional treatment using an interactive web response system. The protocol specified that patients assigned to the early surgery group should undergo surgery within 48 hours of randomization. Patients assigned to the conventional treatment group were treated according to the current guidelines,11),12),13) and surgery was performed only if complications requiring surgery developed during medical treatment or if symptoms persisted after the completion of antibiotic therapy. The institutional review board at each participating center approved the study protocol and written informed consent was obtained from all patients prior to randomization.
Follow-up
All patients were followed during hospitalization at 4 weeks, 6 weeks, 3 months, 6 months, and 1 year and at 6-month intervals thereafter. Patients were asked to call a study coordinator if they experienced any symptoms during follow-up. Data were obtained to the time of death or until March 2015, and follow-up was complete for all patients. The pre-specified end points were all-cause death, embolic events, recurrence of IE and repeat hospitalizations due to development of CHF that occurred during follow-up. An embolic event was defined as a systemic embolism fulfilling prespecified criteria: the acute onset of clinical symptoms or signs of embolism, and the occurrence of new lesions confirmed by follow-up imaging studies. Cutaneous manifestations or metastatic abscesses were not considered as embolic events. An experienced neurologist confirmed a specific diagnosis of cerebral embolism according to additional magnetic resonance imaging of the brain.
Statistical analysis
Analyses were performed on an intention-to-treat basis. Estimates of cumulative event rates were calculated by the Kaplan-Meier method and compared with the use of the log-rank test. For the Kaplan-Meier analysis, we analyzed all clinical events according to the time of the first event. Hazard ratios with 95% confidence intervals were derived with the use of the Cox proportional hazards model. All reported p values are two-sided, and a value of p<0.05 was considered statistically significant. SAS software, version 9.1 (SAS Institute Inc., Cary, NC, USA), was used for statistical analyses.
Results
Trial patients
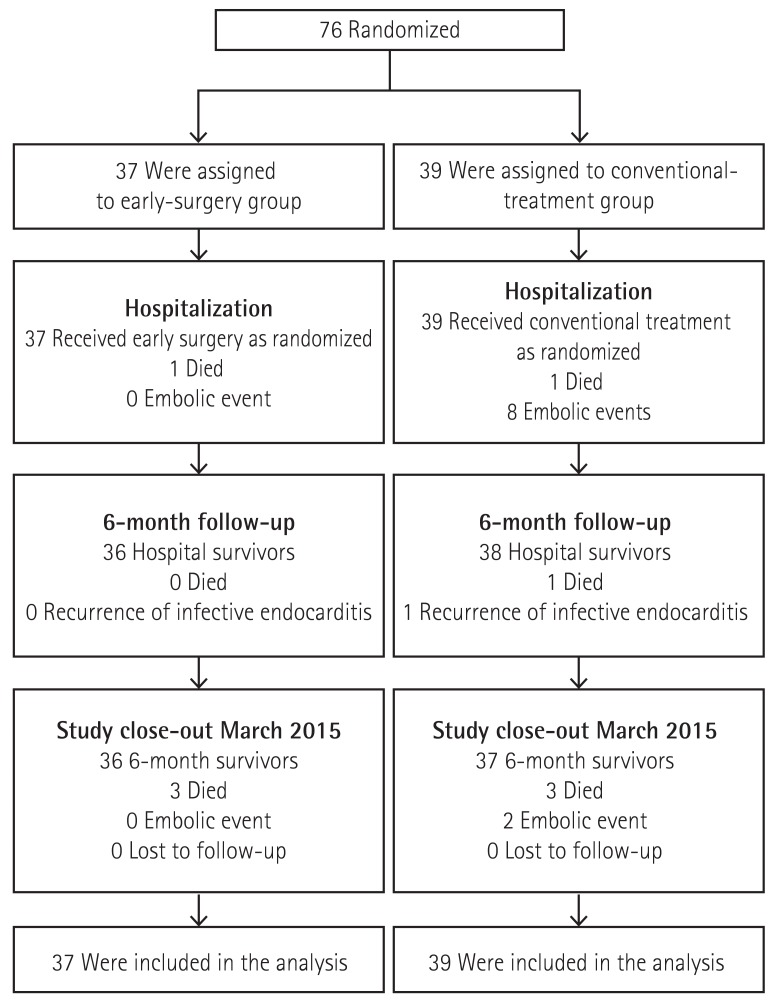
A total of 76 patients with left-sided IE who were potential candidates for early preemptive surgery were randomized; 37 were assigned to early surgery and 39 to conventional treatment (Fig. 1).
Fig. 1. Flow diagram of study patients.
The treatment groups were generally well balanced with regard to baseline clinical characteristics. The mean age of the patients was 47 years with 67% being male. The mitral valve was involved in 45 patients, the aortic valve in 22, and both valves in 9. The median diameter of vegetation was 12 mm (interquartile range, 11 to 17). The most common pathogens in both groups were viridians streptococci (30%), other streptococci (30%) and Staphylococcus aureus (11%).
Surgical procedures
All patients in the early surgery group underwent valve surgery within 48 hours after randomization; the median time between randomization and surgery was 24 hours (interquartile range, 7 to 45). Of the 39 patients assigned to the conventional treatment group, 30 (77%) patients underwent surgery during the initial hospitalization (n=27) or during follow-up (n=3). No patients died within 30 days after surgery in either group. All patients with involvement of the aortic valve underwent valve replacement, but among patients with involvement of the mitral valve, 6 (35%) of the 17 in the conventional group underwent valve replacement, as compared with 14 (64%) of the 22 in the early surgery group.
End point
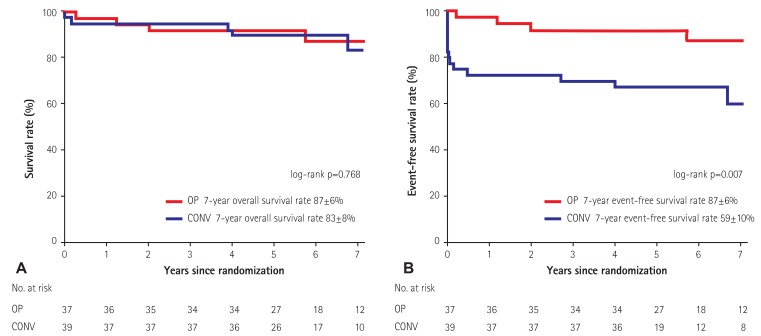
There was 1 in-hospital death, each in the early surgery group and in the conventional treatment group. During median follow-up of 5.8 years (interquartile range, 4.8 to 7.1), 3 deaths occurred in the early surgery group and 4 deaths in the conventional treatment group. The causes of death were malignancy (n=1), trauma (n=1), acute renal failure (n=1) and sudden death (n=1) in the early surgery group, and malignancy (n=1), cerebral infarction (n=2) and sudden death (n=2) in the conventional treatment group. There was no significant difference between the early surgery and conventional treatment groups in all-cause mortality at 4 years (8.1% and 7.7%, respectively; hazard ratio 1.04; 95% CI, 0.21 to 5.15; p=0.96) (Fig. 2A). There were no embolic events in the early surgery group and 8 embolic events in the conventional treatment group during hospitalization. During follow-up, no embolic event or recurrence of IE occurred in the early surgery group and 2 embolic events and 1 recurrence of IE in the conventional treatment group. No patient in either group was hospitalized for CHF during follow-up. The rate of the composite end point of death from any cause, embolic events or recurrence of IE at 4 years was 8.1% in the early surgery group and 30.8% in the conventional treatment group (hazard ratio, 0.22; 95% CI, 0.06-0.78; p=0.02). The estimated actuarial rate of end points at 7 years was significantly lower in the early surgery group than in the conventional treatment group (p=0.007 by log-rank test) (Fig. 2B).
Fig. 2. Kaplan-Meier curve of cumulative probabilities of survival (A) and event-free survival (B) according to treatment group. OP: early surgery, CONV: conventional treatment.
Discussion
In this randomized trial involving IE patients complicated with severe valve disease and large vegetations, early surgery significantly reduced the composite end point of death from any cause and embolic events during hospitalization, and the substantial benefit for early surgery was sustained throughout the follow-up period extending up to 7 years. After six months, the event-free survival curves remained parallel and late clinical outcomes were excellent in both groups.
Long-term clinical outcome in IE survivors remain controversial.4),6),7),8),9) In a prospective, population-based study of left-sided IE, the in-hospital mortality rate was 19% and increased to 41% at 5 years.6) The crude survival rate at 1 and 5 years was 90% and 70% in an observational cohort study, and it was significantly worse compared with expected survival.7) A nationwide cohort study in Sweden showed that long-term relative mortality risk in IE survivors continued to increase, even up to 5 years.8) A recent nationwide population-based study in Taiwan also demonstrated that the risk of long-term major adverse cardiac events and all-cause mortality substantially increased in IE survivors.4) In contrast, a Dutch cohort study of patients who were operated on for IE showed that IE survivors had a survival rate similar to the general population.9) In this study, more than 80% of our patients underwent valve surgery and long-term mortality was substantially lower than previously reported, whereas only 13% of the Sweden cohort and only 14% of the Taiwan cohort underwent valve surgery.4),8) Our aggressive surgical approach may be related to the lower risk of long-term mortality and morbidity.
More patients in the early surgery group received valve replacement than those in the conventional treatment group,5) and the timing of surgery might be related to the differences in rates of repair. On the other hand, a higher rate of valve replacement in the early surgery group did not result in an increase in thromboembolism and recurrence of IE associated with prosthetic valves. Our results suggest that a surgeon's ability to completely excise infected tissues and careful long-term monitoring is more important in controlling infection and preventing adverse cardiovascular events after surgery than the actual type of surgery (repair versus replacement).
This study has several limitations. First, the trial was a limited study in scope, in that it excluded those with moderate to severe heart failure, major stroke, prosthetic valve endocarditis or aortic abscess. However, the limitation related to our exclusion criteria is inherent to a randomized clinical trial conducted in infective endocarditis. According to guidelines,13),14) early surgery is recommended to patients with moderate to severe CHF or to those with uncontrolled infection such as prosthetic valve endocarditis or aortic abscess. In addition, medical treatment is preferred to early surgery in those with major stroke or intracerebral hemorrhage,15) and random assignment of such patients to a treatment arm of early surgery or medical treatment is against the principle of clinical equipoise that forms the ethical basis for a randomized trial.16) Thus, those with specific indications of early surgery or medical treatment were excluded in this trial. Second, our study had insufficient power to evaluate the effect of early surgery on long-term survival. Third, the operative mortality was very low in the study, and the study patients had low operative risks. The results of the study may not be applicable to patients with high operative risks.
Conclusion
In this randomized trial, the beneficial effect of early surgery in patients with IE and large vegetations was maintained during long-term follow-up, and late clinical outcome after surgery was excellent in survivors of IE.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463–473. doi: 10.1001/archinternmed.2008.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mylonakis E, Calderwood SB. Medical progress: infective endocarditis in adults. N Engl J Med. 2001;345:1318–1330. doi: 10.1056/NEJMra010082. [DOI] [PubMed] [Google Scholar]
- 3.Hoen B, Duval X. Clinical practice. Infective endocarditis. N Engl J Med. 2013;368:1425–1433. doi: 10.1056/NEJMcp1206782. [DOI] [PubMed] [Google Scholar]
- 4.Shih CJ, Chu H, Chao PW, et al. Long-term clinical outcome of major adverse cardiac events in survivors of infective endocarditis: a nationwide population-based study. Circulation. 2014;130:1684–1691. doi: 10.1161/CIRCULATIONAHA.114.012717. [DOI] [PubMed] [Google Scholar]
- 5.Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366:2466–2473. doi: 10.1056/NEJMoa1112843. [DOI] [PubMed] [Google Scholar]
- 6.Bannay A, Hoen B, Duval X, et al. The impact of valve surgery on short- and long-term mortality in left-sided infective endocarditis: do differences in methodological approaches explain previous conflicting results? Eur Heart J. 2011;32:2003–2015. doi: 10.1093/eurheartj/ehp008. [DOI] [PubMed] [Google Scholar]
- 7.Thuny F, Giorgi R, Habachi R, et al. Excess mortality and morbidity in patients surviving infective endocarditis. Am Heart J. 2012;164:94–101. doi: 10.1016/j.ahj.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Ternhag A, Cederström A, Törner A, Westling K. A nationwide cohort study of mortality risk and long-term prognosis in infective endocarditis in Sweden. PLos One. 2013;8:e67519. doi: 10.1371/journal.pone.0067519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mokhles MM, Ciampichetti I, Head SJ, Takkenberg JJ, Bogers AJ. Survival of surgically treated infective endocarditis: a comparison with the general Dutch population. Ann Thorac Surg. 2011;91:1407–1412. doi: 10.1016/j.athoracsur.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 11.Bonow RO, Carabello BA, Kanu C, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006;114:e84–e231. doi: 10.1161/CIRCULATIONAHA.106.176857. [DOI] [PubMed] [Google Scholar]
- 12.Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation. 2005;111:e394–e434. doi: 10.1161/CIRCULATIONAHA.105.165564. [DOI] [PubMed] [Google Scholar]
- 13.Habib G, Hoen B, Tornos P, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC) Eur Heart J. 2009;30:2369–2413. doi: 10.1093/eurheartj/ehp285. [DOI] [PubMed] [Google Scholar]
- 14.Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:e57–e185. doi: 10.1016/j.jacc.2014.02.536. [DOI] [PubMed] [Google Scholar]
- 15.Kang DH. Timing of surgery in infective endocarditis. Heart. 2015;101:1786–1791. doi: 10.1136/heartjnl-2015-307878. [DOI] [PubMed] [Google Scholar]
- 16.Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987;317:141–145. doi: 10.1056/NEJM198707163170304. [DOI] [PubMed] [Google Scholar]