Introduction
D-Transposition of great arteries (d-TGA) also known as ‘complete transposition of great arteries’ is characterised by atrioventricular concordance and ventriculoarterial discordance. Though d-TGA is one of the most common critical cardiac lesions seen in new born, yet is most oftenly missed on antenatal sonography. Recent studies have reported that only 23% of cases with isolated cardiac anomaly are detected antenatally.1 We report 4 cases of d-TGA, which were antenatally diagnosed by demonstrating parallel outflow tracts. The other important differential diagnosis, L-Transposition of great arteries (l-TGA) or physiologically corrected TGA was excluded by following systematic approach.
Case report
Case 1
A 22-year-old female patient primigravida, on her first visit at 24 weeks of period of gestation (POG), was referred for anomaly scan. Anomaly scan revealed isolated fetal cardiac anomaly with following description: visceral-atrial situs and standard four chamber view were normal, outflow tract evaluation revealed main pulmonary artery (MPA) originating from left ventricle, aorta was seen originating from right ventricle (RV), ventricular septal defect and parallel relationship of outflow tracts was also seen (Fig. 1). Colour Doppler convincingly demonstrated parallel outflow tracts with VSD (Fig. 2). Patient was referred to tertiary care hospital in 3rd trimester. Post natal echocardiography confirmed findings and neonate was operated upon. There was no other associated anomaly.
Fig. 1.

Outflow tract view showing aorta (Ao) originating from right ventricle (RV), MPA origination LV, parallel relation of MPA and aorta (Ao), ventricular septal defect (**).
Fig. 2.
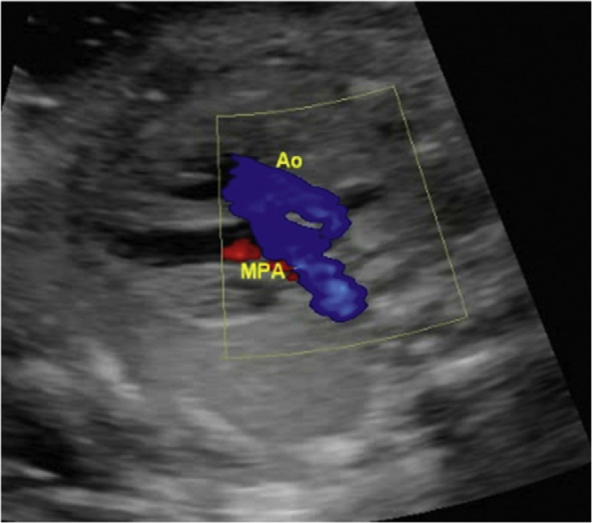
Colour Doppler in outflow tract showing parallel relationship of outflow tracts.
Case 2
A 24-year female patient primigravida was referred for anomaly scan at 20 wk POG. Anomaly scan revealed isolated outflow tract anomaly with following findings: Aorta was seen originating from RV, MPA was seen originating from LV and had a component of overriding. Color Doppler confirmed parallel outflow tracts (Fig. 3). Patient was referred to tertiary care hospital in 3rd trimester. Post natal echo confirmed findings. No other anomaly was found. Unfortunately neonate died of complications secondary to cardiac anomaly prior to scheduled date of surgery.
Fig. 3.

Colour Doppler at level of outflow tracts reveling parallel relation of outflow tracts at origin. MPA – main pulmonary artery, Ao – ascending aorta, RV – right ventricle.
Case 3
A 20 year-old female patient primigravida was referred for anomaly scan at 18 wk POG. Anomaly scan revealed isolated fetal cardiac anomaly with following findings: MPA was seen originating from LV, aorta was seen originating from RV. Both outflow tracts had parallel relationship at origin. Patient was referred to tertiary care hospital however baby was born prematurely at 32 Wks in zonal hospital. After initial management, was transferred to tertiary care hospital where neonate was operated upon for d-TGA. Unfortunately infant died of complications at 6 month of age at zonal hospital.
Case 4
A 23 year-old female patient, G2P1 reported for anomaly scan at 18 wk POG. Anomaly scan revealed isolated fetal cardiac anomaly. Parallel outflow tracts with ventriculoarterial discordance were seen (Fig. 4).
Fig. 4.
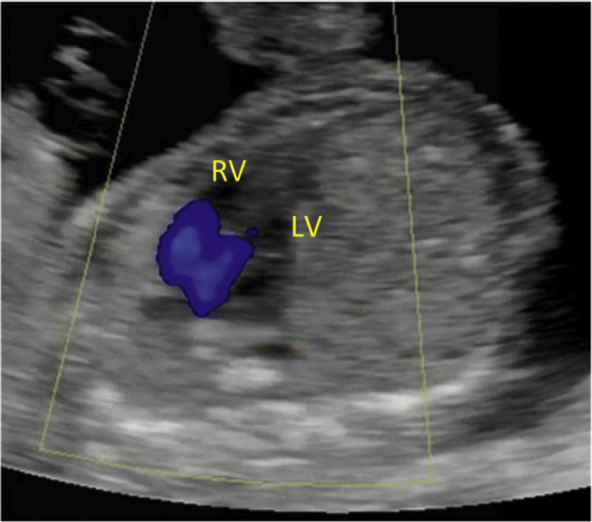
Modified outflow tract view with Colour Doppler showing parallel relation of outflow tracts.
Discussion
d-TGA is the second most common cyanotic congenital heart disease diagnosed in first year of life. Reported incidence of it is 315 per million live births.2 d-TGA is predominantly seen in males with male to female ratio varying from 2:1 to 3:1. Embryologically it has been hypothesized that failure of conoventricular rotation and persistence of subaortic conus with complete resorption of subpulmonic conus results in this conotruncal anomaly.3
Unlike other conotruncal anomalies d-TGA is rarely associated with chromosomal anomalies or extracardiac malformations, as is found in our cases.4 Maternal diabetes is considered to be associated with almost three fold increase in risk for TGA as compared to non diabetic patients.5 However in none of our cases patient was diabetic. Animal studies also implicated maternal use of phenobarbitone as a risk factor for cardio vascular anomalies including TGA.6
Antenatal diagnosis of this anomaly essentially depend on demonstration of parallel outflow tracts or absent crisscrossing of great arteries. With inclusion of following steps to routine fetal heart evaluation, this anomaly can be reliably differentiated from physiologically corrected TGA. These simple, systematic and reproducible steps are: (A) Demonstration of normal visceral-atrial situs and axis. It must be remembered that flap of foramen ovale opens into left atrium, interatrial septum bulges from right to left side and right atrium appears larger. (B) Demonstration of atrioventricular concordance, this remains crucial step and can be achieved by differentiating RV from LV. Important differences which are easy to identify and reproducible are (i) Echogenic moderator band is present in RV (ii) Tricuspid valve insertion into septum has an offset toward apex (iii) Lumen of LV is longer in length than RV and cavity of LV has triangular shape (iv) Irregularity of endocardial surface of RV as compared to LV.7 Some of these differences are conspicuous in Fig. 1. (C) Demonstration of branching pattern of great vessels. In our experience branching pattern of MPA is more easily demonstrated and especially so in cases of TGA. Since Ductus arteriosus often originate at an acute angle from left pulmonary artery in cases of TGA, intactness of same can be demonstrated in outflow view itself.
Since antenatal diagnosis allows planned delivery at tertiary care hospital, it reduces mortality among survivors.8
Conclusion
D-Transposition of great arteries, most common cause of critical heart anomaly in new borns still remains associated with significant mortality and morbidity. By inclusion of step wise scientific approach this uncommonly antenatally detected conotruncal anomaly can be easily diagnosed during anomaly scan.
Conflicts of interest
The authors have none to declare.
References
- 1.Levi S., Zhang W.H., Virat P., Grandjean H. Short-term outcome of isolated and associated congenital heart defects in relation to antenatal ultrasound screening. Ultrasound Obstet Gynecol. 2003;21:532–538. doi: 10.1002/uog.146. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman J.I., Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 3.Goor D.A., Edwards J.E. The spectrum of transposition of great arteries with specific reference to developmental anatomy of conus. Circulation. 1973;48:406–415. doi: 10.1161/01.cir.48.2.406. [DOI] [PubMed] [Google Scholar]
- 4.Sidi D., Vouhe P., Ou P. Transposition and malposition of great arteries with ventricular septal defects. In: Maller James H., Hoffman Julien I.E., editors. Pediatric Cardiovascular Medicine. 2nd ed. Wiley-Black well; 2012. pp. 638–650. [Google Scholar]
- 5.Wren C., Birrell G., Howthorne G. Cardiovascular malformation in infants of diabetic mothers. Heart. 2003;89:1217–1220. doi: 10.1136/heart.89.10.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okuda H., Nagao T. Cardiovascular malformation induced by prenatal exposure to phenobarbital in rats. Congenit Anom (Kyoto) 2006 Jun;46:97–104. doi: 10.1111/j.1741-4520.2006.00109.x. [DOI] [PubMed] [Google Scholar]
- 7.Mcewing R.L., Chaoui R. Congenitally corrected transposition of great arteries: clues for prenatal diagnosis. Ultrasound Obstet Gynecol. 2004;23:68–72. doi: 10.1002/uog.896. [DOI] [PubMed] [Google Scholar]
- 8.Blyth M., Howe D., Gnanapragasam J., Wellesley D. The hidden mortality of transposition of great arteries and survival advantage provided by prenatal diagnosis. BJOG. 2008;115:1096–1100. doi: 10.1111/j.1471-0528.2008.01793.x. [DOI] [PubMed] [Google Scholar]


