Abstract
Aim
This trial (NCT: 01713036) investigated the absolute bioavailability, mass balance and metabolite profile of pimasertib in a new design combining these investigations in a single group of patients.
Methods
Six male patients with pathologically confirmed, locally advanced or metastatic solid tumours were enrolled. Exclusion criteria included Eastern Cooperative Oncology Group performance status >1. In Part A of the trial, patients received a 60 mg oral dose of unlabelled pimasertib followed by an intravenous (i.v.) tracer dose of [14C]pimasertib 2 μg (equalling 9 kBq) as a bolus injection, one hour after the oral dose, on Day 1. On Day 8, all patients received 60 mg pimasertib capsules spiked with 2.6 MBq of [14C]pimasertib. Patients received 60 mg oral unlabelled pimasertib twice daily from Day 3 to Day 21 of Part A and in subsequent 21‐day cycles in Part B.
Results
Following i.v. administration, [14C]pimasertib exhibited a geometric mean total body clearance of 45.7 l h−1 (geometric coefficient of variation [geometric CV]: 47.2%) and a volume of distribution of 229 l (geometric CV: 42.0%). Absolute bioavailability was 73%. The majority of the oral [14C] dose (85.1%) was recovered in excreta. Total radioactivity was mainly excreted into urine (52.8%) and faeces (30.7%) with 78.9% of the [14C] dose recovered as metabolites. Two major circulating metabolites were identified in plasma: a carboxylic acid (M445) and a phosphoethanolamine conjugate (M554). The safety profile was in line with the published pimasertib trials.
Conclusion
Pimasertib showed a favourable pharmacokinetic profile with high absolute bioavailability and a unique metabolic pathway (conjugation with phosphoethanolamine).
Keywords: 14C, absolute bioavailability, elimination route, mass balance, pimasertib
What is Already Known about this Subject
Pimasertib is a new selective, oral inhibitor of mitogen‐activated protein kinases 1 and 2 (MEK1/2).
Comprehensive information about the pharmacokinetics, including absolute bioavailability, metabolism and elimination routes, of cancer drugs is often incomplete.
What this Study Adds
Description of a trial design combining investigation of absolute bioavailability and mass balance/metabolite identification in a single group of six male cancer patients.
Identification of a new metabolic pathway for drugs, i.e. conjugation with phosphoethanolamine.
Information about key pharmacokinetic parameters and the drug disposition of pimasertib in cancer patients.
Tables of Links
| LIGANDS | |
|---|---|
| Pimasertib |
These Tables list key protein targets and ligands in this article, which are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY 1, and are permanently archived in the Concise Guide to PHARMACOLOGY 2015/16 2.
Introduction
Pimasertib (MSC1936369B/AS703026) is a highly selective, orally bioavailable, small molecule inhibitor of mitogen‐activated protein kinases 1 and 2 (MEK1/2) of the MAPK pathway (the chemical structure and synthesis of pimasertib are available 3, 4, 5). Pimasertib has demonstrated potent antitumour activity either alone or in combination with other agents in cell lines and xenograft models 3, 6, 7 and is currently undergoing phase I/II clinical trials in patients with different tumour types; it has demonstrated clinical activity both as monotherapy and in combination with gemcitabine, the PI3K inhibitor SAR245409, and the HDM‐2 inhibitor SAR405838 8, 9, 10.
To fully understand the impact of pimasertib and any of its metabolites on pharmacology, safety and drug–drug interaction potential, we determined its absorption, distribution, metabolism and elimination (ADME) and identified its major metabolites in the systemic circulation, in keeping with recommendations by regulatory agencies worldwide 11, 12, 13. Furthermore, we investigated the excretion of unchanged pimasertib and its metabolites in order to understand any potential impact of hepatic or renal impairment on the pharmacokinetics (PK) of pimasertib.
Since pimasertib is intended for oral administration, the determination of absolute bioavailability, i.e. the rate and extent to which a drug reaches the systemic circulation, is an additional important PK parameter. Incomplete absolute bioavailability has been shown to increase the inter‐individual variability of exposure to drugs 14 and can indicate poor performance of the formulation and/or poor absorption, as well as an extensive first‐pass effect of a drug. Non‐clinical studies determining absolute bioavailability in laboratory animals, although frequently applied as a surrogate for human bioavailability, have been shown to be inaccurate predictors of absolute bioavailability in humans 15. Absolute bioavailability is considered a mandatory requirement by some health authorities, such as the Australian Therapeutic Goods Administration. However, of the nine small molecule anticancer agents intended for oral administration approved by the FDA in 2014/2015 (belinostat, ceritinib, ibrutinib, idelalisib, lenvatinib, olaparib, palbociclib, panobinostat, sonidegib), absolute bioavailability has been determined for only two (panobinostat and palbociclib) 16.
Mass balance trials, involving the application of 14C‐radiolabelled drug and the collection of plasma and excreta, represent the standard approach undertaken to understand these ADME properties. Advances in technology over the past decade have generated alternative methods that maximize the information gained from these complex trials and minimize the use of radiolabelled compounds (for a review see 17). New approaches include microdose‐ and microtracer‐based trials using accelerator mass spectrometry (AMS). Mass balance trials are complex and require extensive PK sampling in plasma/excreta and are therefore typically carried out in healthy male volunteers. However, results from trials in healthy volunteers may not translate to patients and the safety profile of an investigational drug may be unsuitable for use in healthy volunteers, which is often the case for anticancer drugs 18. Given the safety profile of pimasertib, which is comparable to other MEK 1/2 inhibitors 19, we chose to conduct this trial in cancer patients despite additional technical challenges for trial design and bioanalytics (reviewed in 18 and 20), as well as the possibility of having to halt the trial due to wrong assumptions in the calculation of the radioactive burden to patients, as recently published for the MEK inhibitor, trametinib 17, 21. Here, we report the findings of a phase I, single centre, open‐label, absolute bioavailability, mass balance and metabolite identification trial of pimasertib in six male patients with pathologically confirmed locally advanced or metastatic solid tumours. We combined the determination of these critical PK parameters in a single trial to maximize knowledge about pimasertib disposition in its patient population.
Materials and methods
Trial design
This was an open‐label, single centre, absolute bioavailability, mass balance and metabolite identification trial of pimasertib in six male patients with locally advanced or metastatic solid tumours (Part A), followed by optional pimasertib monotherapy in Part B (Clinical Trials.gov identifier NCT01713036, EUDRA CT2012‐002562‐12). The study was conducted by PRA International in Budapest, Hungary. Part A lasted from November 2012 until June 2013. The last patient's final visit took place in July 2014 for Part B. The trial comprised a screening and baseline evaluation period up to 28 days before start of trial treatment, a 21‐day treatment period (Part A), and a follow‐up period of 21‐day treatment cycles (Part B) (Figure 1). Patients were enrolled sequentially. The clinical trial protocol and the informed consent form (ICF) were approved by the Ethics Committee for Clinical Pharmacology of the Medical Research Council, Budapest, Hungary. The trial was conducted in accordance with the principles of the Declaration of Helsinki, the International Conference on Harmonisation (ICH) E6 Guideline for Good Clinical Practice (GCP), and compliant with the European Union Clinical Trial Directive (EU CTD). All patients signed the ICF before any trial‐related procedures were started.
Figure 1.
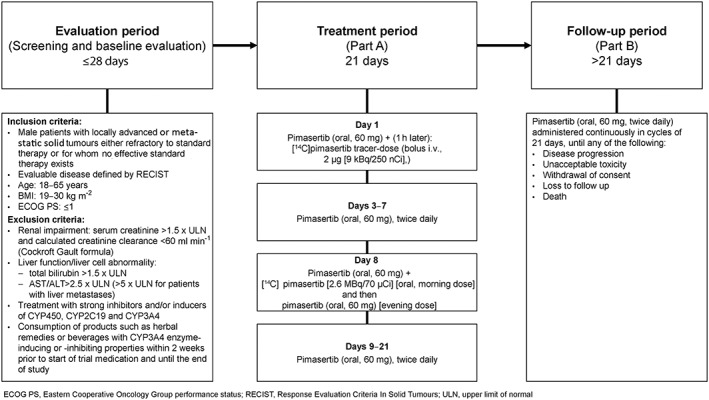
Schematic design of the trial including the treatment period (Part A) and the follow‐up period (Part B)
Part A of the trial comprised a single 21‐day treatment period. For determination of pimasertib absolute bioavailability, patients received a single oral dose of pimasertib in the morning of Day 1, followed, 1 hour later, by an intravenous (i.v.) tracer dose of radioactive [14C]pimasertib (9 kBq/250 nCi, equivalent to approximately 2 μg [14C]pimasertib, injected as a bolus) (Figure 1). Blood samples for determination of pimasertib and [14C]pimasertib in plasma were collected from each patient pre‐dose and up to 48 h post administration of unlabelled pimasertib (see Supplementary Table S1 for more information on blood sampling). Thereafter, all patients received repeated oral doses of pimasertib twice daily (BID) from Day 3 to Day 21. On Day 8, patients received a single dose of 60 mg pimasertib as an oral capsule spiked with 2.6 MBq (71 μCi) [14C]pimasertib for determination of mass balance, and identification and profiling of metabolites. Blood samples for PK evaluations of total 14C‐radioactivity in plasma and determination of blood/plasma ratio of total 14C‐radioactivity were collected pre‐dose and up to 168 h post‐dose. An additional blood sample was taken from each patient at 1.5 h post‐dose for determination of total and unbound parent drug concentrations. For the analysis of total 14C‐radioactivity and metabolite profiling, urine and faeces were collected up to 168 h post‐dose. If >1% of administered radioactivity was recovered in excreta (i.e. urine and faeces by daily stand‐by analysis after Day 12) over two consecutive days, the collection schedule was extended by further 24 h intervals up to Day 21 (346 h post‐dose). During Part A of the trial, patients were hospitalized from the evening of Day −1 until the morning of Day 2. Thereafter, patients were hospitalized again in the evening of Day 7 and discharged from the clinic between Day 12 and Day 21.
In Part B of the trial, following assessment of safety and tolerability data for each patient obtained in Part A, 60 mg pimasertib BID was administered continuously in cycles of 21 days (i.e. the dosing regimen currently applied as a continuous regimen in pimasertib phase II trials [NCT01693068; NCT01936363]) until progression of the disease, unacceptable toxicity, withdrawal of consent by the patient, loss to follow up, or death (Figure 1).
Patients
Male patients with pathologically confirmed, locally advanced or metastatic solid tumours either refractory to standard therapy or for whom no effective standard therapy existed were enrolled into the trial. See Figure 1 for inclusion and exclusion criteria.
Investigational medicinal products (IMPs)
Pimasertib was used as three different IMPs in this trial: (1) unlabelled pimasertib (hard gelatin capsule containing 15 mg pimasertib); (2) a tracer dose of 9 kBq (250 nCi) [14C]pimasertib (equivalent to approximately 2 μg [14C]pimasertib) formulated as an i.v. solution; and (3) 15 mg unlabelled pimasertib spiked with 0.13 mg [14C]pimasertib (equivalent to 0.65 MBq [17.5 μCi] [14C]pimasertib) (hard gelatin capsule). All capsule presentations of pimasertib were of green colour, capsule size 0. The structural formula of [14C]pimasertib including the position of the [14C]label is provided in Figure 2.
Figure 2.
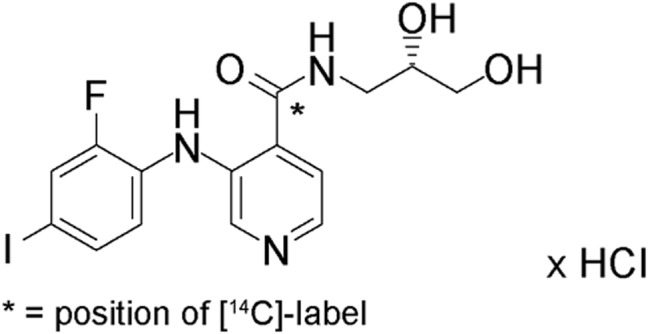
Structural formula of [14C]pimasertib. The asterisk indicates the position of the [14C]atom
Dosing rationale
[ 14 C ]pimasertib. The estimation of the radioactive [14C]pimasertib dose administered on Day 8 was based on animal data, i.e. [14C]pimasertib oral administration to male pigmented and albino rats. For dosimetry calculations, the assumption was made that the levels of uptake and retention by tissues would be the same in man. Administration of 2.6 MBq (71 μCi) [14C]pimasertib chosen in this trial is equivalent to a radioactive dose of 0.5 mSv, corresponding to category Ia of the 1990 Recommendations of the International Commission on Radiological Protection (ICRP) and in accordance with the Hungarian National Institute for Quality and Organizational Development in Healthcare and Medicines (GYEMSZI). Fixed dosing of [14C]pimasertib was chosen to ensure that no patient would exceed the above‐mentioned radioactive dose.
A tracer dose of 9 kBq (250 nCi), equivalent to approximately 2 μg [14C]pimasertib was given on Day 1 in order to minimize the overall radioactivity administered in the trial. This [14C]pimasertib tracer dose was detected using ultra‐sensitive AMS 22 measuring 14C atoms instead of radioactivity. No separate dosimetry was carried out for the i.v. tracer dose.
Unlabelled pimasertib multiple doses in Parts A and B. A dose of 60 mg BID, currently applied as a continuous regimen in pimasertib phase II trials (NCT01693068; NCT01936363), was used.
Bioanalytics
[ 14 C ]pimasertib i.v. tracer‐dose. For the determination of [14C]pimasertib (MSC1936369, [S]‐configuration) and separation of its pharmacologically inactive (R)‐enantiomer (MSC1940796) a two‐stage, reverse phase and enantioselective liquid chromatography (LC) method followed by AMS was used (see Supplementary Information for full methodology).
Pimasertib oral (p.o.) dose. For the determination of pimasertib (MSC1936369, [S]‐configuration) and separation of its (R)‐enantiomer (MSC1940796), an enantioselective high‐performance LC (HPLC) tandem mass spectrometry (MS/MS) assay was used (see Supplementary Information for full methodology). The racemate of deuterated [2H5]pimasertib was used as the internal standard (see Supplementary Information for full methodology).
Total radioactivity. Plasma, urine and faeces homogenate were analyzed by liquid scintillation counting. All scintillation counting was carried out using a Perkin Elmer Tri‐CarbTM 3100 TR Liquid Scintillation analyzer (Waltham, MA‐02541, USA) (see Supplementary Information for full methodology).
Metabolite identification. The metabolic profile of [14C]pimasertib was investigated in plasma, urine and faeces using a radiometric ultra‐performance LC (UPLC) method. For urine and faeces, metabolites were identified in pooled samples covering more than 90% of the total radioactivity excreted for each matrix. Intervals with low radioactivity were not used for the generation of the pooled samples to avoid dilution of the latter and to increase the signal‐to‐noise ratio of the respective chromatograms.
Identification and structural elucidation of metabolites were performed using an LTQ Orbitrap XL (Thermo Scientific, Dreieich, Germany) high‐resolution mass spectrometer for full scan and fragments for metabolite identification, and an API4000 QTrap mass spectrometer (AB Sciex, Darmstadt, Germany) with multiple reaction monitoring (MRM) for allocation and confirmation of metabolite structures. A detailed description of pimasertib metabolite identification will be published by Scheible et al. elsewhere.
Pharmacokinetics
The PK parameters of pimasertib following oral administration and of [14C]pimasertib following i.v. administration on Day 1, as well as of total [14C]radioactivity and pimasertib metabolites following oral administration on Day 8, were evaluated by non‐compartmental analysis using the software Phoenix WinNonlin v.6.3.0 (Certara USA Inc., Princeton, NJ, USA). For calculation of the area under the plasma concentration‐time curves (AUC) the mixed log linear trapezoidal rule was used. Absolute bioavailability (F) of pimasertib was calculated as F = (AUC0‐∞ p.o./AUC0‐∞ i.v.) × (dosei.v ./dosep.o.) × 100%, based on the exposures of oral pimasertib and i.v. [14C]pimasertib administration on Day 1 (see Supplementary Table S2 for more details on the PK parameters). The geometric mean and geometric coefficient of variation (CV) were used as descriptive statistics for all PK parameters except t max, for which values are provided as median (range).
Safety and efficacy assessments
The safety of pimasertib was assessed by evaluating adverse events (AEs) according to Common Terminology Criteria for AEs (CTCAE v.4.0), clinical chemistry, haematology, urinalysis, vital signs, 12‐lead electrocardiograms, echocardiogram, ophthalmologic assessments and by physical examinations. Efficacy was defined as tumour response and was based on tumour evaluations performed every two cycles in accordance with Response Evaluation Criteria In Solid Tumours (RECIST) v1.1.
Statistics
This was an exploratory trial and no formal statistical analysis was applied in this trial. Descriptive statistics, calculated using Phoenix WinNonlin v.6.3.0 (Certara USA Inc., Princeton, NJ, USA), were used when appropriate.
Results
Patient demographic characteristics
Patient characteristics are shown in Table 1.
Table 1.
Patient and disease characteristics
| Patient number | Primary cancer diagnosis / histology | ECOG status | Age (years) | Height (cm) | Weight (kg) | BMI ( kg m −2 ) |
|---|---|---|---|---|---|---|
| 1 | Non‐small cell carcinoma/squamous cell carcinoma | 1 | 59 | 169 | 82 | 28.7 |
| 2 | Head and neck squamous cell carcinoma | 1 | 56 | 168 | 59.5 | 21.1 |
| 3 | Colorectal cancer/ adenocarcinoma | 0 | 40 | 185 | 98 | 28.6 |
| 4 | Non‐small cell lung cancer | 0 | 62 | 171 | 77.2 | 26.4 |
| 5 | Colorectal cancer/ adenocarcinoma | 0 | 56 | 182 | 80.3 | 24.2 |
| 6 | Non‐small cell lung cancer | 0 | 64 | 177 | 91.2 | 29.1 |
| Median | 57.5 | 174 | 81.2 | 27.5 | ||
| Min ., Max. | 40, 64 | 168.0, 185.0 | 59.5, 98.0 | 21.1, 29.1 | ||
BMI, body mass index; ECOG, Eastern Cooperative Oncology Group
Pimasertib pharmacokinetics following single dose intravenous administration
Following i.v. bolus injection of a tracer dose of 2 μg [14C]pimasertib, [14C]pimasertib plasma concentrations decreased in a multi‐exponential fashion with the lower limit of quantification (LLoQ) being reached between 12 and 16 h post‐dose (Figure 3). A geometric mean clearance (CL) of 45.7 l h−1 and a geometric mean V z of 229 l exceeding total plasma water were observed. Inter‐individual variability was 47.2% for CL and 42.0% for V z (geometric mean CV). The t 1/2 in the six patients who had post‐dose PK samples up to 24 h available for regression analysis was 3.5 h (geometric mean; range 2.7–4.7 h). For other PK parameters and individual values, see Table 2.
Figure 3.
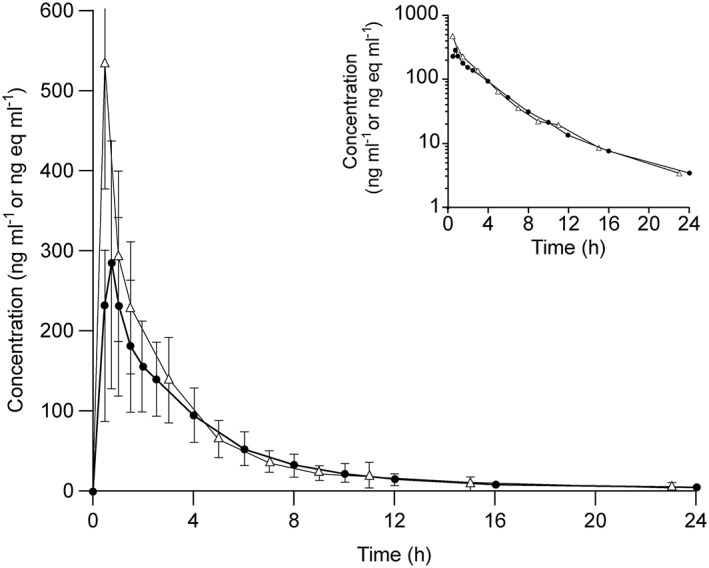
Dose normalized (60 mg) linear and semi‐log (insert) mean plasma concentration time profiles of pimasertib (filled dots) following oral administration of pimasertib and of [14C]pimasertib (open triangles) following i.v. administration of a 2 μg tracer dose of [14C]pimasertib during tmax of the oral 60 mg pimasertib dose on Day 1. The error bars represent the standard deviation for n = 6 patients
Table 2.
Individual pharmacokinetic data for pimasertib following oral administration of 60 mg pimasertib on Day 1, [14C]pimasertib following i.v. administration of a 2 μg tracer dose of [14C]pimasertib during t max of the oral 60 mg pimasertib dose on Day 1, and total [14C]radioactivity following oral administration of 2.6 mBq [14C]pimasertib on Day 8
| PK parameter | Unit | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Geo. mean | Geo. mean CV |
|---|---|---|---|---|---|---|---|---|---|
| [ 14 C ]pimasertib i.v. tracer dose Day 1 | |||||||||
| C max | pg eq ml−1 | 144.3 | 19.1 | 12.7 | 18.9 | 6.0 | 10.5 | 12.7 | 45.3 |
| t max | h | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5a | – |
| AUC 0‐t | h × pg eq ml−1 | 38.9 | 63.8 | 37.1 | 47.5 | 16.7 | 29.9 | 36.0 | 48.0 |
| CL | l h−1 | 38.7 | 26.5 | 45.6 | 35.6 | 97.4 | 56.5 | 45.7 | 47.2 |
| V z | l | 179 | 181 | 264 | 161 | 480 | 220 | 229 | 42.0 |
| t 1/2 | h | 3.2 | 4.7 | 4.0 | 3.1 | 3.4 | 2.7 | 3.5 | 20.1 |
| pimasertib p.o Day 1 | |||||||||
| C max | ng ml−1 | 219 | 370 | 339 | 497 | 74.2 | 342 | 265 | 76.2 |
| t max | h | 1.50 | 0.75 | 0.75 | 0.75 | 2.50 | 0.50 | 0.75a | – |
| AUC 0‐t | h × ng ml−1 | 1132 | 1317 | 1276 | 1311 | 339 | 802 | 937 | 57.3 |
| CL/f | l h−1 | 52.3 | 45.2 | 46.4 | 44.2 | 173 | 72.0 | 62.7 | 57.0 |
| V z /f | l | 776 | 227 | 629 | 564 | 774 | 722 | 572 | 49.6 |
| F | % | 74.0 | 58.6 | 98.2 | 80.5 | 56.1 | 78.4 | 73.0 | 21.2 |
| t 1/2 | h | 10.3 | 3.5 | 9.4 | 8.8 | 3.1 | 7.0 | 6.3 | 56.4 |
| Total‐[ 14 C ] p.o., Day 8 | |||||||||
| C max | ng eq ml−1 | 909 | 1042 | 608 | 813 | 503 | 914 | 774 | 28.4 |
| t max | h | 2.0 | 0.75 | 1.5 | 2.0 | 1.5 | 1.0 | 1.5a | – |
| AUC 0‐t | h × ng eq ml−1 | 6979 | 7752 | 4876 | 6317 | 2464 | 5506 | 5318 | 42.9 |
| CL R | l h−1 | 6.04 | 3.59 | 6.65 | 5.22 | 10.2 | 5.32 | 5.87 | 35.4 |
| CL nonR | l h−1 | 2.49 | 3.07 | 4.46 | 3.60 | 11.2 | 5.03 | 4.36 | 56.4 |
| t 1/2 | h | 17.0 | 59.8 | 11.8 | 20.3 | 8.87 | 11.0 | 17.0 | 77.7 |
| f e urine | % of dose | 67.9 | 47.5 | 57.1 | 55.1 | 43.1 | 49.5 | 52.8 | 16.1 |
| urine t b | h | 156 | 132 | 156 | 300 | 204 | 156 | 156a | – |
| f e faeces | % of dose | 17.6 | 37.0 | 25.7 | 43.8 | 34.7 | 32.8 | 30.7 | 33.1 |
| faeces t c | h | 132 | 156 | 156 | 204 | 180 | 132 | 155a | – |
| f e | % of dose | 85.6 | 84.5 | 82.7 | 98.9 | 77.8 | 82.3 | 85.1 | 8.1 |
| Pimasertib f u | |||||||||
| f u | % | 7.1 | 7.0 | 5.4 | 6.8 | 6.9 | 7.1 | 6.9 | 9.9 |
| HSA | g l−1 | 28.9 | 38.4 | 34.6 | 37.0 | 32.3 | 33.9 | 34.0 | 10.2 |
| AAG | g l−1 | 1.57 | 1.02 | 1.98 | 1.02 | 1.56 | 1.41 | 1.39 | 26.7 |
Median values presented
Time post‐dose up to when urine was collected
Time post‐dose up to when faeces was collected
AAG, alpha‐1 acid glycoprotein; AUC, are under the curve; CL, clearance; CV, coefficient of variation; F, absolute bioavailability; Geo, geometric; HSA, human serum albumin; i.v., intravenous; PK, pharmacokinetics; p.o., oral; vz, volume of distribution
Pimasertib pharmacokinetics following single dose oral administration
Following a 60 mg oral dose, pimasertib was rapidly absorbed with maximum plasma concentrations appearing with a median t max of 0.75 h post‐dose (range 0.5–2.5 h; Table 2). Pimasertib CL/f was comparable to the CL determined after i.v. administration of [14C]pimasertib, with a geometric mean of 62.7 l h−1. V z/f was higher following oral administration compared with the i.v. parameter V z, with a geometric mean of 572 l. Inter‐individual variability was 57.0% for CL/f and 49.6% for V z /f, i.e. only slightly increased in comparison to CL and V z determined after i.v. administration. The apparent t 1/2 was 6.3 h (geometric mean) ranging from 3.1 to 10.3 h. For other PK parameters and individual values, see Table 2.
Absolute bioavailability
Plasma concentration time plots for [14C]pimasertib administered i.v. (dose adjusted) and for pimasertib administered orally appeared to be comparable (Figure 3). In keeping with this observation, the statistical analysis of absolute bioavailability resulted in an estimate of 73% with 90% confidence interval (CI) ranging from 61% to 87%, indicating high absolute bioavailability of pimasertib at a 60 mg dose. For individual values, see Table 2.
Pharmacokinetics of total radioactivity following a single dose of [14C]pimasertib
On Day 8, all patients received 60 mg unlabelled pimasertib capsules spiked with 2.6 MBq of [14C]pimasertib. Total radioactivity appeared rapidly in plasma in all but one patient in the first post‐dose PK sample at 0.5 h. The median t max of total radioactivity was noted 1.5 h post‐dose (range 0.75–2.0 h), and formed a plateau between 1–2 h post‐dose (Figure 4A). Subsequently, total radioactivity decreased in a bi‐exponential fashion, with a rapid drop up to 8 h post‐dose, followed by a slower decline up to 96 h post‐dose. Total radioactivity levels remained above the LLoQ in five out of six patients at 48 h post‐dose. The apparent t 1/2 of total radioactivity in the six patients was 17.0 h (range 8.9–59.8 h). The geometric mean CL R of total radioactivity was 5.87 l h−1, while the geometric mean CL NonR was calculated at 4.36 l h−1. For other PK parameters and individual values, see Table 2.
Figure 4.
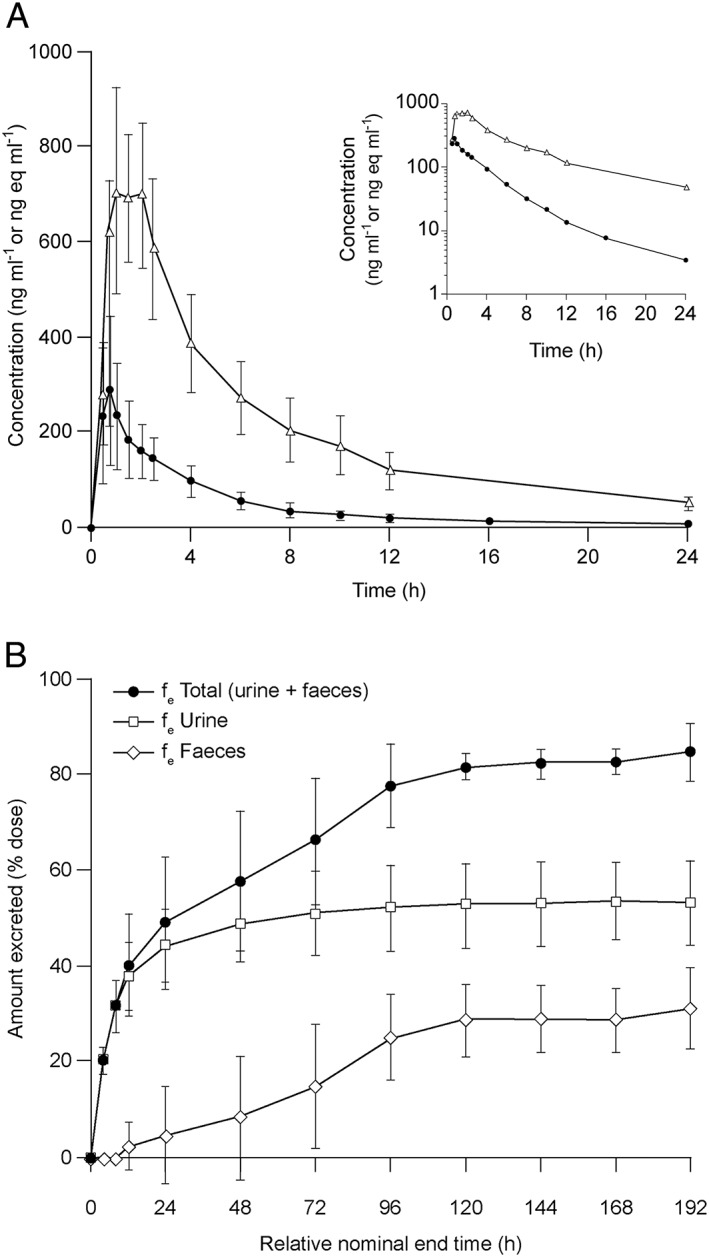
(A) Linear and semi‐log (insert) mean plasma concentration time profiles of pimasertib (filled dots) following oral administration of 60 mg pimasertib on Day 1 (concentrations provided in ng ml−1) and of 2.6 mBq [14C]pimasertib (open triangles) following oral administration of 2.6 mBq [14C]pimasertib on Day 8 (concentrations provided as ng eq ml−1). The error bars represent the standard deviation for n = 6 patients. (B) Cumulative recovery of total [14C]radioactivity following oral administration of 2.6 mBq [14C]pimasertib on Day 8 expressed as a percentage of the administered [14C]dose in excreta (urine + faeces, filled black dots), urine (open squares), and faeces (open diamonds). The error bars represent the standard deviation for n = 6 patients
Pimasertib mass balance/major elimination routes
Pimasertib mass balance, i.e. the recovery of total radioactivity ([14C]pimasertib and its metabolites) in excreta, was determined post‐dosing on Day 8. A total of 85.1% (geometric mean) of the 14C‐labelled dose was recovered (range 77.8–98.9%) in urine and faeces within 192 h post‐dose (Figure 4B). During the trial, urine was sampled up to 300 h post‐dose and faeces were sampled up to 204 h post‐dose.
Following administration of [14C]pimasertib on Day 8, 47.9% of the radioactive dose was recovered within 24 h, and the majority of total radioactivity (geometric mean 81.6%) was recovered within 120 h. Total radioactivity was mainly excreted into urine (geometric mean 52.8%), with urinary excretion completed after approximately 48 h. In faeces, 30.7% (geometric mean) of the 14C‐labelled dose was recovered. In all patients, excretion into faeces occurred with a lag time of 48–96 h, except in two patients where elimination into faeces was found to occur in parallel with elimination into urine. Faecal elimination increased steadily up to 192 h and did not reach a plateau during the collection period.
Identification of major pimasertib metabolites in human plasma and their plasma concentration‐time profiles
Investigation of major pimasertib metabolites following dosing of [14C]pimasertib on Day 8 was carried out in plasma samples drawn from 1 to 24 h post‐dose. In these plasma samples, all radiochromatographic peaks of >1% could be structurally identified. In total, 14 different [14C]pimasertib metabolites were identified, all of which had been observed previously in in vitro and/or in in vivo animal studies. In addition to pimasertib, two metabolites were identified in plasma with AUC0–24 ≥ 10% relative to total radioactivity exposure, namely M445 and M554, which, in keeping with ICH M3(R2) 11, qualify as major metabolites.
The AUC0–24 of M445 and M554 amounted to 19.2% and 29.8% of the AUC0–24 of total radioactivity in plasma, respectively. Relative to the AUC0–24 of [14C]pimasertib in plasma, the AUC0–24 of M445 and M554 amounted to 152% and 183%, respectively. M445 (MSC2359570) was identified as a carboxylic acid metabolite, formed by oxidation of the propanediol moiety of pimasertib. M554 was formed by conjugation of pimasertib with phosphoethanolamine. The structural information of the two metabolites was defined using high‐resolution mass spectrometric data and comparison with synthesized reference standards.
PK analysis of [14C]pimasertib and its major metabolites, M445 and M554, is provided in Supplementary Information Table S3 and the plasma concentration‐time profiles are shown in Supplementary Information Figure S1. The elimination half‐life of both metabolites could not be reliably estimated during the 24 h post‐dose observation period. Inspection of the plasma concentration‐time plots suggested that M554 was eliminated at a lower rate than pimasertib, while M445 was eliminated at a higher rate (Supplementary Figure S1).
Identification of pimasertib metabolites in urine and faeces
Identification of pimasertib metabolites following dosing on Day 8 was carried out in pooled urine and faeces samples. The geometric mean of the administered radioactive dose excreted into urine was 52.8% (range 43.1–67.9%). In the investigated pools (mean of 48.7% of the total radioactivity recovered), 99.2% of the administered radioactive dose could be structurally identified (i.e. 92.2% of the total radioactivity recovered). Trace amounts of unchanged [14C]pimasertib (0.1%) were excreted into urine. Pimasertib metabolites excreted into urine constituted 48.6% of the radioactive dose administered. In urine, 19.1% of the administered radioactive dose was excreted as the oxidative metabolite, M445, and 16.8% as the phosphoethanolamine conjugate, M554. Apart from the (R)‐enantiomer of M445 amounting to −0.9% of the radioactive dose administered, no secondary metabolites resulting from the metabolism of M445 or M554 could be identified in urine.
The geometric mean of the administered radioactive dose recovered in faeces was 30.7% (range 17.6–43.8%). In the investigated pool (mean of 30.4% of the total radioactivity recovered), all peaks could be structurally identified (i.e. 99.0% of the radioactivity recovered in faeces), with unchanged [14C]pimasertib amounting to 5.4% and pimasertib metabolites adding up to 25%. In faeces, 18.2% of the administered radioactive dose was found to be excreted as the oxidative metabolite, M445, whereas only trace amounts (0.1%) were found to be eliminated as the phosphoethanolamine conjugate, M554.
In total, 85.1% of the total radioactive dose was recovered, 78.9% of which was in the form of metabolites, indicating that [14C]pimasertib was almost completely metabolized. Pimasertib's main metabolic pathways included: oxidation to M445 (37.3% of the administered radioactive dose); and conjugation with phosphoethanolamine to M554 (16.9% of the administered radioactive dose). The remaining 25.6% was eliminated via six distinct metabolic pathways including oxidation, glucuronidation and isomerization. Notably, in urine and faeces, apart from the (R)‐enantiomer of M445 amounting to 1.6% of the administered radioactive dose, no secondary metabolites derived from the metabolism of M445 or M554 could be identified.
Pimasertib fraction unbound/blood:plasma ratio
The mean f u of pimasertib was 6.7% (range 5.4–7.1%). Human serum albumin (HSA) concentrations in the plasma samples varied 1.29‐fold (range 28.9–38.4 g l−1), whereas alpha‐1 acid glycoprotein (AAG) concentrations varied 1.94‐fold (range 1.02–1.98 g l−1). AAG levels were not found to influence the f u of pimasertib in human plasma. For individual values, see Table 2.
Blood to plasma ratios for total radioactivity (i.e. pimasertib and its metabolites) ranged from 0.687 to 0.834 in PK samples taken 0.5 to 24 h post‐dose. The mean hematocrit in the plasma samples was 0.38 (range 0.29–0.42).
Safety
All six patients (100%) who continued treatment in part B of the study experienced at least one treatment‐emergent AE (TEAE). The most common events reported were fever, diarrhoea and rash. Of the events, 81% were considered related to pimasertib and were mostly grade 1 or 2 in severity, with seven events (reported by three patients) being grade 3. Two patients required hospitalization. One patient with squamous non‐small cell lung cancer (NSCLC) had a fatal unrelated bronchopneumonia, while another patient experienced grade 2 pyrexia and diarrhoea, the latter considered pimasertib‐related, that resolved or improved. Two patients had events leading to study drug withdrawal.
Serous retinal detachment and retinal vein occlusion, common events with MEK inhibitors, were observed in two and one patient, respectively, and resolved. Increase in creatinine phosphokinase (CPK), another adverse event observed on treatment with MEK inhibitors, was reported in three patients, grade 2 in two and grade 3 in one. All resolved after dose reduction or dose interruption.
The majority of laboratory findings were in line with the underlying condition of the patients. Laboratory‐related findings were mostly of mild intensity. Vital signs, electrocardiogram results (including echocardiograms) and Eastern Cooperative Oncology Group (ECOG) performance status were generally in line with the underlying medical condition of the patients.
Efficacy
Of the six patients with measurable and evaluable advanced cancer enrolled in the trial, three patients with squamous cell carcinoma of the head and neck (SCCHN), NSCLC and colorectal cancer, respectively, experienced stable disease. Two of these three patients had stable disease up to cycle 4 and 17, respectively, corresponding to 84 (SCCHN) and 336 (NSCLC) days on study, while the third patient withdraw consent early and had stable disease at the only post‐dose assessment in cycle 2. Two patients were not evaluable for efficacy, while one patient had progressive disease.
Discussion
This trial investigated the absolute bioavailability, mass balance, elimination route, identification of metabolites and metabolite profile of pimasertib in a single trial. Pimasertib absolute bioavailability was determined by concomitant administration of an oral, unlabelled pimasertib dose of 60 mg and an i.v. tracer dose of 2 μg [14C]pimasertib (equalling 9 kBq) as a bolus injection on Day 1. Administration of the oral and i.v. doses on the same day allowed for determination of absolute bioavailability, thereby limiting the imprecision which can be associated with the commonly applied two‐period design. Formulation of the i.v. solution was straightforward because no solubilizing excipients were required to dissolve such a low dose in isotonic saline. Moreover, the use of an i.v. tracer dose required neither an additional trial assessing acute toxicity following i.v. administration nor a local tolerability trial, in line with ICH M3(R2) 11. Intra‐individual PK variability, which is of particular concern in trials assessing patients with cancer, did not influence the absolute bioavailability determined in this trial. The high absolute bioavailability of pimasertib (73%) in combination with the low inter‐individual variability observed for this parameter (geometric CV: 21%) indicate that pimasertib is not prone to drug–drug interactions affecting its absorption, which can increase the absolute bioavailability of a drug that is incompletely absorbed 23. This is remarkable as small molecular kinase inhibitors are generally characterized by a poor oral, and thus variable, bioavailability 23.
Administration of the i.v. tracer dose produced a practically negligible radioactive burden that was 284‐fold lower than the oral dose of [14C]pimasertib applied on Day 8 for the determination of pimasertib mass balance/metabolite identification. Determination of absolute bioavailability could thus be combined with mass balance/metabolite identification in a single trial using a single radio‐labelled isotope (14C), thereby reducing the development time and cost of an additional tracer (e.g. 13C 24). However, administration of the [14C]pimasertib tracer dose on Day 1 had to be carried out before administration of the oral mass balance dose of [14C]pimasertib on Day 8 to prevent [14C] carry‐over effects.
Pimasertib mass balance, i.e. the recovery of total radioactivity (pimasertib and its metabolites) in excreta, was high, with 85.1% (range 77.8–98.9%) of the radioactive dose recovered. The most likely explanation for the variability in the recovery of total radioactivity may be incomplete sampling, in particular of faeces, as recovery of total radioactivity in faeces did not result in a plateau in two patients. Furthermore, defaecation is known to be irregular in patients with advanced cancer.
Simultaneous determination of pimasertib absolute bioavailability provided information about the fraction of the dose that was not bioavailable (i.e. 1–F). A negligible fraction of the dose was recovered in faeces as unchanged pimasertib. Therefore, the fraction of the dose that was not bioavailable was apparently lost due to intestinal metabolism and/or hepatic first‐pass effect. Although the trial design allowed the estimation of the fraction absorbed (f abs) and fraction escaping gut metabolism (f g), we did not conduct this analysis because (i) absolute bioavailability of pimasertib was almost complete and (ii) determination of f abs would have required additional blood volume to be sampled on Day 1. No inference could be made as to whether total radioactivity recovered in faeces was derived from elimination into bile or intestinal secretion. Further investigation using bile sampling devices 25 was not undertaken due to the minimal recovery of unchanged drug in faeces, and also to avoid additional complexity for a trial conducted in patients with cancer.
This trial showed that [14C]pimasertib was almost completely metabolized, with 78.9% of the administered radioactive dose recovered as metabolites and only 5.5% of the dose recovered unchanged in excreta. Renal elimination of unchanged pimasertib, therefore, appeared as a minor elimination pathway. In urine and faeces, 92.2% and 99.0% of the recovered radioactivity could be structurally identified. The identification of metabolite structure in this trial was thorough, and excluded the possible existence of an additional unidentified metabolite contributing >25% to the elimination of an oral pimasertib dose.
Comparison of the plasma concentration time plots of single doses of pimasertib administered orally on Day 1 with total radioactivity resulting from [14C]pimasertib administration on Day 8 suggested that elimination rate‐limited metabolites were formed in plasma, as indicated by the difference in apparent t 1/2 (pimasertib: 6.32 h; total radioactivity: 17.0 h).
Pimasertib's elimination is based on two main metabolic pathways: oxidation to M445 and conjugation with phosphoethanolamine to M554. The remainder was eliminated via other metabolic pathways, e.g. oxidation, glucuronidation and isomerization. For the quantification of pimasertib fraction metabolized (f m), the quantitative contribution of individual CYP isoenzymes is currently being elucidated by determination of enzyme kinetics for M445 formation in recombinantly expressed CYP isoenzymes. The structure of the two major metabolites was elucidated using high resolution mass spectrometry data and by comparison to synthesized reference standards. Synthesis of the major plasma metabolite, M554, proved to be particularly useful, indicating that to the best of our knowledge pimasertib is the first drug to be identified as being eliminated by conjugation to phosphoethanolamine. The identification of the enzyme(s) involved in the formation of M554 is currently ongoing.
Based on these data, the potential for other drugs to influence the PK of pimasertib appears to be limited, given that the two main elimination pathways of the compound are via oxidation to M445 and conjugation to M554 and mediated by two CYP isoenzymes. In addition, since conjugation of pimasertib with phosphoethanolamine has not been reported for xenobiotics before, this metabolic pathway appears to be unique and is currently not known to be altered by concomitant administration of other drugs.
AAG levels have been found to vary substantially and to influence the f u of drugs that bind to AAG 26, 27. In order to determine the dependence of pimasertib's plasma protein binding, HSA as well as AAG concentrations were measured in blood samples used for determination of pimasertib f u. In the six patients enrolled, HSA concentrations varied very little (range 28.9–38.4 g l−1), whereas AAG concentrations varied 1.94‐fold. AAG levels did not influence the f u of pimasertib in human plasma, indicating that pimasertib is not strongly bound to AAG and that differences in AAG levels frequently observed in plasma of patients with cancer 26, 27 will not affect the f u of pimasertib.
The safety profile of pimasertib is consistent with previously published experiences, with fever, diarrhoea and rash being the most commonly reported adverse events. Increase in CPK and retinal events were also observed. Although the study was not designed to address efficacy, it is noteworthy that three of six patients had stable disease, in one case lasting for almost one year.
In conclusion, we report here for the first time the determination of absolute bioavailability, mass balance, elimination route and metabolite profile of pimasertib in a single group of patients with cancer in a single trial. Pimasertib showed a favourable PK profile after oral and i.v. dosing with high absolute bioavailability. Pimasertib is metabolized via two major elimination pathways, with one of them, i.e. conjugation with phosphoethanolamine, being unique. The data obtained in this trial provide confidence for the favourable PK profile of pimasertib in cancer patients early in the development of the compound.
Competing Interests
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: the trial was sponsored by Merck KGaA, Darmstadt, Germany; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; GM, HS and AJ are employees of Merck KGaA, Darmstadt, Germany and OvR is a former employee of Merck KGaA, Darmstadt, Germany, who sponsored the trial. IU was principal investigator of the trial and a full‐time employee of PRA International (during clinical trial execution until 31 March 2014), which conducted the trial on behalf of the sponsor.
This trial was sponsored by Merck KGaA, Darmstadt, Germany. The authors would like to thank the patients, the patients' families and the study teams at the participating centres. We are grateful to Peter Rueckert for his assistance in the non‐compartmental PK analysis of this trial. Accelerator mass spectrometry was performed at Xceleron Inc., Germantown, MD, USA. Enantioselective high‐performance liquid chromatographic tandem mass spectrometry was performed at Slotervaart Hospital/Netherlands Cancer Institute, Amsterdam, The Netherlands. Oliver von Richter's current affiliation is Sandoz Biopharmaceuticals, Holzkirchen, Germany. Istvan Udvaros's current affiliation is SGS Life Sciences, Mechelen, Belgium. We would also like to thank Emily Heath (Bioscript Science, Macclesfield, UK) for medical writing assistance, which was funded by Merck KGaA, Darmstadt, Germany.
Contributors
OvR, GM, HS, IU and AJ all made substantial contributions to the concept and design of the study, acquisition, analysis and interpretation of the data. OvR and AJ drafted the manuscript. All authors participated in reviewing/revising the content and approved the final submitted version.
Supporting information
Figure S1 Linear and semi‐log (insert) mean plasma concentration time profiles of pimasertib (filled dots) and pimasertib metabolites (M445, a carboxylic acid metabolite, formed by oxidation of the propanediol moiety of pimasertib – open squares; M554, conjugate of pimasertib with phosphoethanolamine – open triangles) following oral administration of 2.6 mBq [14C]pimasertib on Day 8 (concentrations provided as ng ml−1 for pimasertib and ng eq ml−1 for pimasertib metabolites). The error bars represent the standard deviation for n = 6 patients.
Table S1 Blood, urine and faeces sampling scheme following administration of 60 mg pimasertib and 2 μg [14C]pimasertib on Day 1 and administration of 2.6 mBq [14C]pimasertib on Day 8.
Table S2 Pharmacokinetic parameters for pimasertib oral administration and [14C]pimasertib tracer dose i.v. administration on Day 1, as well as total [14C]radioactivity in plasma following administration of 2.6 mBq [14C]pimasertib p.o. on Day 8.
Table S3 Pharmacokinetic analysis of [14C]pimasertib and its major metabolites, M445 and M554.
Supplementary Methods: Bioanalytics.
Supporting info item
Supporting info item
Supporting info item
Supporting info item
Supporting info item
Supporting info item
von Richter, O. , Massimini, G. , Scheible, H. , Udvaros, I. , and Johne, A. (2016) Pimasertib, a selective oral MEK1/2 inhibitor: absolute bioavailability, mass balance, elimination route, and metabolite profile in cancer patients. Br J Clin Pharmacol, 82: 1498–1508. doi: 10.1111/bcp.13078.
References
- 1. Southan C, Sharman JL, Benson HE, Faccenda E, Pawson AJ, Alexander SP, et al. The IUPHAR/BPS Guide to PHARMACOLOGY in 2016: towards curated quantitative interactions between 1300 protein targets and 6000 ligands. Nucl Acids Res 2016; 44: D1054–D1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alexander SPH, Fabbro D, Kelly E, Marrion N, Peters JA, Benson HE, et al. The Concise Guide to PHARMACOLOGY 2015/16: Enzymes. Br J Pharmacol 2015; 172: 6024–6109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim K, Kong S‐Y, Fulciniti M, Li X, Song W, Nahar S, et al. Blockade of the MEK/ERK signalling cascade by AS703026, a novel selective MEK1/2 inhibitor, induces pleiotropic anti‐myeloma activity in vitro and in vivo . Br J Haematol 2010; 149: 537–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Intellectual Property Organization . WO2006045514. 3‐arylamino pyridine derivatives. 2006. Available at https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2006045514&redirectedID=true (last accessed 12 August 2015).
- 5. World Intellectual Property Organization . WO2013178320. Solid state forms of n‐((s)‐2,3‐dihydroxy‐propyl)‐3‐(2‐fluoro‐4‐iodo‐phenylamino)‐isonicotinamide. 2013. Available at https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2013178320&redirectedID=true (last accessed 12 August 2015).
- 6. Martinelli E, Troiani T, D'Aiuto E, Morgillo F, Vitagliano D, Capasso A, et al. Antitumor activity of pimasertib, a selective MEK 1/2 inhibitor, in combination with PI3K/mTOR inhibitors or with multi‐targeted kinase inhibitors in pimasertib‐resistant human lung and colorectal cancer cells. Int J Cancer 2013; 133: 2089–2101. [DOI] [PubMed] [Google Scholar]
- 7. Yoon J, Koo K‐H, Choi K‐Y. MEK1/2 inhibitors AS703026 and AZD6244 may be potential therapies for KRAS mutated colorectal cancer that is resistant to EGFR monoclonal antibody therapy. Cancer Res 2011; 71: 445–453. [DOI] [PubMed] [Google Scholar]
- 8. Naing A, Mita M, Komarnitsky P, Milner A, von Richter O, Ogden J, et al. 608 Phase I dose‐escalation trial of a selective oral MEK1/2 inhibitor, PIMASERTIB (MSC1936369B), combined with an mTOR inhibitor, temsirolimus, in patients with advanced solid tumors. Eur J Cancer 2012; 48: 187.22100904 [Google Scholar]
- 9. Delord JP, Houédé N, Awada A, Lebbe C, Lesimple T, Schellens JHM, et al. 616 Pimasertib (MSC1936369B/AS703026), a selective oral MEK1/2 inhibitor, shows clinical activity in melanoma. Eur J Cancer 2012; 48: 190. [Google Scholar]
- 10. Infante JR, Gandhi L, Shapiro G, Burris HA, Bendell JC, Baselga J, et al. Phase lb combination trial of a MEK inhibitor, pimasertib (MSC1936369B), and a PI3K/mTOR inhibitor, SAR245409, in patients with locally advanced or metastatic solid tumors. J Clin Oncol 2012; 30. [Google Scholar]
- 11. Food and Drug Administration . Guidance for industry. M3(R2) Nonclinical safety studies for the conduct of human clinical trials and marketing authorization for pharmaceuticals. Questions and answers. 2012. Available at http://www.fda.gov/downloads/biologicsbloodvaccines/guidancecomplianceregulatoryinformation/guidances/general/ucm292164.pdf (last accessed 12 August 2015).
- 12. Food and Drug Administration . Guidance for Industry – Safety testing of drug metabolites. 2008. Available at http://www.fda.gov/OHRMS/DOCKETS/98fr/FDA‐2008‐D‐0065‐GDL.pdf (last accessed 12 August 2015).
- 13. European Medicines Agency . Guideline on the investigation of drug interactions. 2012. Available at http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/07/WC500129606.pdf (last accessed 12 August 2015).
- 14. Hellriegel ET, Bjornsson TD, Hauck WW. Interpatient variability in bioavailability is related to the extent of absorption: implications for bioavailability and bioequivalence studies. Clin Pharmacol Ther 1996; 60: 601–607. [DOI] [PubMed] [Google Scholar]
- 15. Grass GM, Sinko PJ. Effect of diverse datasets on the predictive capability of ADME models in drug discovery. Drug Discov Today 2001; 6: 54–61.11165174 [Google Scholar]
- 16. Food and Drug Administration . Drug safety data. Available at https://www.accessdata.fda.gov/scripts/cder/drugsatfda/ (last accessed 12 August 2015).
- 17. Beaumont C, Young GC, Cavalier T, Young MA. Human absorption, distribution, metabolism and excretion properties of drug molecules: a plethora of approaches. Br J Clin Pharmacol 2014; 78: 1185–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Beumer JH, Beijnen JH, Schellens JHM. Mass balance studies, with a focus on anticancer drugs. Clin Pharmacokinet 2006; 45: 33–58. [DOI] [PubMed] [Google Scholar]
- 19. Zhao Y, Adjei AA. The clinical development of MEK inhibitors. Nat Rev Clin Oncol 2014; 11: 385–400. [DOI] [PubMed] [Google Scholar]
- 20. Dubbelman A‐C, Rosing H, Schellens JHM, Beijnen JH. Bioanalytical aspects of clinical mass balance studies in oncology. Bioanalysis 2011; 3: 2637–2655. [DOI] [PubMed] [Google Scholar]
- 21. Ho MYK, Morris MJ, Pirhalla JL, Bauman JW, Pendry CB, Orford KW, et al. Trametinib, a first‐in‐class oral MEK inhibitor mass balance study with limited enrollment of two male subjects with advanced cancers. Xenobiotica 2014; 44: 352–368. [DOI] [PubMed] [Google Scholar]
- 22. Barker J, Garner RC. Biomedical applications of accelerator mass spectrometry‐isotope measurements at the level of the atom. Rapid Commun Mass Spectrom 1999; 13: 285–293. [DOI] [PubMed] [Google Scholar]
- 23. Herbrink M, Nuijen B, Schellens JH, Beijnen JH. Variability in bioavailability of small molecular tyrosine kinase inhibitors. Cancer Treat Rev 2015; 41: 412–422. [DOI] [PubMed] [Google Scholar]
- 24. Schwab D, Portron A, Backholer Z, Lausecker B, Kawashima K. A novel double‐tracer technique to characterize absorption, distribution, metabolism and excretion (ADME) of [14C]tofogliflozin after oral administration and concomitant intravenous microdose administration of [13C]tofogliflozin in humans. Clin Pharmacokinet 2013; 52: 463–473. [DOI] [PubMed] [Google Scholar]
- 25. Guiney WJ, Beaumont C, Thomas SR, Robertson DC, McHugh SM, Koch A, et al. Use of Entero‐Test, a simple approach for non‐invasive clinical evaluation of the biliary disposition of drugs. Br J Clin Pharmacol 2011; 72: 133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Urien S, Barré J, Morin C, Paccaly A, Montay G, Tillement JP. Docetaxel serum protein binding with high affinity to alpha 1‐acid glycoprotein. Invest New Drugs 1996; 14: 147–151. [DOI] [PubMed] [Google Scholar]
- 27. Jackson PR, Tucker GT, Woods HF. Altered plasma drug binding in cancer: role of alpha 1‐acid glycoprotein and albumin. Clin Pharmacol Ther 1982; 32: 295–302. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Linear and semi‐log (insert) mean plasma concentration time profiles of pimasertib (filled dots) and pimasertib metabolites (M445, a carboxylic acid metabolite, formed by oxidation of the propanediol moiety of pimasertib – open squares; M554, conjugate of pimasertib with phosphoethanolamine – open triangles) following oral administration of 2.6 mBq [14C]pimasertib on Day 8 (concentrations provided as ng ml−1 for pimasertib and ng eq ml−1 for pimasertib metabolites). The error bars represent the standard deviation for n = 6 patients.
Table S1 Blood, urine and faeces sampling scheme following administration of 60 mg pimasertib and 2 μg [14C]pimasertib on Day 1 and administration of 2.6 mBq [14C]pimasertib on Day 8.
Table S2 Pharmacokinetic parameters for pimasertib oral administration and [14C]pimasertib tracer dose i.v. administration on Day 1, as well as total [14C]radioactivity in plasma following administration of 2.6 mBq [14C]pimasertib p.o. on Day 8.
Table S3 Pharmacokinetic analysis of [14C]pimasertib and its major metabolites, M445 and M554.
Supplementary Methods: Bioanalytics.
Supporting info item
Supporting info item
Supporting info item
Supporting info item
Supporting info item
Supporting info item


