Abstract
Background
Community-acquired pneumonia (CAP) is a major cause of morbidity and mortality in adults even in developed countries. Several lifestyle factors and comorbidities have been linked to an increased risk, although their prevalence has not been well documented in the primary care setting. The aim of this study is to assess the incidence, risk factor and comorbid conditions distribution of CAP in adults in primary care in Spain.
Methods
Retrospective observational study in adults (>18 years-old) with CAP diagnosed and attended at primary care in Spain between 2009 and 2013, using the Computerized Database for Pharmacoepidemiological Studies in Primary Care (BIFAP).
Results
Twenty-eight thousand four hundred thirteen patient records were retrieved and analyzed. Mean age (standard deviation): 60.5 (20.3) years, 51.7 % males. Global incidence of CAP in adults was estimated at 4.63 per 1000 persons/year. CAP incidence increased progressively with age, ranging from a 1.98 at 18–20 years of age to 23.74 in patients over 90 years of age. According to sex, global CAP incidence was slightly higher in males (5.04) than females (4.26); CAP incidence from 18 to 65 year-olds up was comparable between males (range: 2.18–5.75) and females (range: 1.47–5.21), whereas from 65 years of age, CAP incidence was noticeable higher in males (range: 7.06–36.93) than in females (range: 5.43–19.62). Average prevalence of risk factors was 71.3 %, which increased with age, doubling the risk in males by the age of 75 (females 20 % vs males 40 %). From 55 years of age, at least one risk factor was identified in 85.7 % of cases: one risk factor (23.8 %), two risk factors (23.4 %), three or more risk factors (38.5 %). Major risk factors were: metabolic disease (27.4 %), cardiovascular disease (17.8 %) and diabetes (15.5 %).
Conclusions
The annual incidence of CAP in primary care adults in Spain is high, comparable between males and females up to 65 years of age, but clearly increasing in males from that age. CAP risk increases with age and doubles in males older than 75 years. The majority of CAP cases in patients over 55 years of age is associated to at least one risk factor. The main risk factors associated were metabolic disease, cardiovascular disease, and diabetes.
Electronic supplementary material
The online version of this article (doi:10.1186/s12879-016-1974-4) contains supplementary material, which is available to authorized users.
Keywords: Community-acquired pneumonia, Vaccine-preventable diseases, Risk factors, Incidence, Antibiotics, Primary care
Background
Community-acquired pneumonia (CAP) is a major cause of morbidity and mortality in adults even in developed countries [1–3]. CAP leads to high rates of hospitalization, particularly in the elderly, and belongs to the top 5 causes of death globally [4]. Depending on the geographic area analyzed, the estimated annual incidence ranges between 1.6 and 12 cases per 1000 population [5–9].
Several lifestyle factors have been associated with an increased risk of CAP including smoking, alcohol abuse, being underweight, having regular contact with children, and poor dental hygiene, among others [10–12]. Also the presence of comorbid conditions, including chronic respiratory and cardiovascular diseases, cerebrovascular disease, Parkinson’s disease, epilepsy, dementia, dysphagia, HIV or chronic renal or liver disease have been linked to an increased risk of CAP [10–12].
The burden of pneumonia is of considerable importance. However, the prevalence of different lifestyle risk factors and comorbidities in patients seeking medical assistance at primary care level because of pneumonia has not been well documented. This study aims to describe the prevalence of different lifestyle risk factors and comorbidities in patients with CAP at primary care in Spain during a 5 year period (2009–2013).
Methods
An observational retrospective study was designed to evaluate the incidence of CAP and the prevalence and distribution of risk factors and comorbidities in adults in primary care in Spain, attended between 2009 and 2013.
Data collection was performed using the Computerized Database for Pharmacoepidemiological Studies in Primary Care (BIFAP). BIFAP is a computerized database aggregating information provided by 2692 general practitioners and pediatricians working in the Spanish National Health Service. The ownership of this database is public, and its sole purpose is to enable epidemiological studies, and in particular pharmacoepidemiological studies. The information related to these patients is kept completely confidential and strictly compliant with current Spanish and European legislation. Collaboration by general practitioners in BIFAP is personal, individual and voluntary. BIFAP is sponsored by three leading Spanish medical societies in primary care: Sociedad Española de Medicina Familiar y Comunitaria (SEMFYC), Sociedad Española de Médicos de Atención Primaria (SEMERGEN) and Asociación Española de Pediatría de Atención Primaria (AEPAP). The BIFAP database includes clinical and prescription data for around 4.8 million patients.
Eligible study participants were Spanish adults 18 years of age or older, of both sexes, diagnosed of the first episode of CAP between January 2009 and December 2013. Patients had to have been recorded with the doctor for 1 year at least. Patients with previous diagnoses of pneumonia or nosocomial pneumonia were excluded.
All patients were identified when a first register of pneumonia during the study period was detected in their medical history. Patients with a potential diagnosis of pneumonia were selected through a computerized algorithm that identified them through process codes (CIAP R81), or through the occurrence of the word “pneumonia” in the free text history. Cases were included when there was a radiological diagnosis and/or where the diagnosis was reported by another professional in a medical record. Doubtful cases, which involved presumptive diagnosis not confirmed by additional tests, or those where information in the clinical history was insufficient, were excluded.
Different lifestyle risk factors and comorbidities associated to the first register of pneumonia were also retrieved and analyzed (Additional file 1). Comorbidities in BIFAP database are codified according to the Spanish version of the International Classification of Diseases, 9th Revision, Clinical Modification (Modificación Clínica Clasificación Internacional de Enfermedades; CIE-9-MC) and/or the Spanish version of the International Classification of Primary Care (CIAP-2/ICPC-2 PLUS) (Additional file 1).
Statistical analysis
Data were presented as mean (standard deviation) or frequency (percentage) as appropriate. We carried out a descriptive analysis of the first episodes of CAP, prevalence of the different lifestyle risk factors and comorbidities stratified by age and gender. The relationship was tested using a binary logistic model. We performed all the analyses using R Software, Version 3.0.2.
Results
A total of 2,332,622 adult patients (18 years of age or older) were included in the study cohort. 28,413 subjects with a mean age (standard deviation) of 60.5 (20.3) years had a first episode of pneumonia during the study period (Table 1).
Table 1.
Summary of main characteristics of the study cohort. Data are expressed as % (n)
| NEUMO-ES-RISK total cohorta
N = 28,413 |
AGE (years) | ||||||
|---|---|---|---|---|---|---|---|
| 18–25 years (N = 1038) |
25–40 years (N = 4861) |
40–55 years (N = 5557) |
55–70 years (N = 6057) |
70–85 years (N = 7484) |
>85 years (N = 3416) |
||
| Characteristics of the cohort | |||||||
| Pneumonia Type | |||||||
| Pneumonia (unspecified) | 57.9 % (16.462) | 53.7 % (557) | 57.6 % (2.799) | 59.3 % (3.297) | 60.2 % (3.645) | 56.9 % (4.262) | 55.7 % (1.902) |
| Bacterial pneumonia | 27.6 % (7.849) | 21.2 % (220) | 25.9 % (1.261) | 26.7 % (1.486) | 27.5 % (1.664) | 29.7 % (2.226) | 29.0 % (992) |
| Atypical pneumonia | 3.5 % (999) | 4.4 % (46) | 5.2 % (251) | 4.8 % (267) | 3.7 % (222) | 2.2 % (164) | 1.4 % (49) |
| Viral pneumonia | 2.8 % (801) | 3.4 % (35) | 3.8 % (183) | 3.9 % (216) | 2.8 % (171) | 1.9 % (140) | 1.6 % (56) |
| Complicated pneumonia | 6.1 % (1.727) | 17.1 % (177) | 7.1 % (345) | 4.7 % (263) | 5.2 % (312) | 6.1 % (456) | 5.1 % (174) |
| Aspirative pneumonia | 1.9 % (551) | 0.3 % (3) | 0.4 % (20) | 0.5 % (26) | 0.6 % (39) | 3.0 % (224) | 7.0 % (239) |
| Nosocomial pneumonia | 0.1 % (24) | 0.0 % (0) | 0.0 % (2) | 0.0 % (2) | 0.1 % (4) | 0.2 % (12) | 0.1 % (4) |
| Gender | |||||||
| Female | 48.3 % (13.716) | 41.4 % (430) | 49.6 % (2.411) | 50.2 % (2.790) | 48.7 % (2.949) | 42.8 % (3.203) | 56.6 % (1.933) |
| Male | 51.7 % (14.697) | 58.6 % (608) | 50.4 % (2.450) | 49.8 % (2.767) | 51.3 % (3.108) | 57.2 % (4.281) | 43.4 % (1.483) |
| Risk factors | |||||||
| Alcoholism | 2.5 % (700) | 0.0 % (0) | 0.8 % (39) | 3.6 % (199) | 4.2 % (256) | 2.5 % (185) | 0.6 % (21) |
| Tobacco | 13.0 % (3.702) | 8.0 % (83) | 13.5 % (656) | 20.9 % (1.163) | 18.3 % (1.106) | 8.3 % (621) | 2.1 % (73) |
| Anemia | 12.3 % (3.501) | 5.7 % (59) | 7.1 % (346) | 9.0 % (498) | 7.7 % (469) | 16.7 % (1.253) | 25.6 % (876) |
| Asthma | 6.5 % (1.833) | 7.8 % (81) | 4.9 % (237) | 5.0 % (277) | 6.1 % (367) | 8.2 % (615) | 7.5 % (256) |
| Bronchitis | 2.1 % (591) | 0.2 % (2) | 0.4 % (20) | 0.9 % (51) | 2.3 % (138) | 3.5 % (265) | 3.4 % (115) |
| COPD | 10.8 % (3.055) | 0.2 % (2) | 0.2 % (9) | 3.1 % (173) | 11.7 % (709) | 21.5 % (1.612) | 16.1 % (550) |
| Low weight | 2.9 % (828) | 3.6 % (37) | 2.5 % (121) | 2.4 % (136) | 2.4 % (148) | 3.6 % (272) | 3.3 % (114) |
| Cardiovascular disease | 17.8 % (5.071) | 0.5 % (5) | 1.7 % (82) | 4.3 % (238) | 15.5 % (936) | 33.0 % (2.469) | 39.3 % (1.341) |
| Cerebrovascular disease | 7.8 % (2.221) | 0.1 % (1) | 0.2 % (12) | 0.9 % (48) | 4.6 % (281) | 14.4 % (1.077) | 23.5 % (802) |
| Bipolar syndrome | 0.2 % (63) | 0.1 % (1) | 0.2 % (8) | 0.3 % (17) | 0.3 % (16) | 0.2 % (17) | 0.1 % (4) |
| Dementia | 4.3 % (1.233) | 0.0 % (0) | 0.0 % (1) | 0.0 % (2) | 0.9 % (54) | 7.2 % (539) | 18.6 % (637) |
| Psychiatric syndrome | 0.2 % (71) | 0.3 % (3) | 0.1 % (4) | 0.3 % (15) | 0.3 % (16) | 0.2 % (15) | 0.5 % (18) |
| Depression | 14.8 % (4.197) | 2.1 % (22) | 6.6 % (323) | 12.0 % (667) | 17.0 % (1.030) | 19.4 % (1.452) | 20.6 % (703) |
| Diabetes | 15.5 % (4.415) | 0.8 % (8) | 1.5 % (75) | 5.7 % (314) | 17.9 % (1.082) | 28.9 % (2.165) | 22.6 % (771) |
| Metabolic disease | 27.4 % (7.780) | 1.7 % (18) | 5.9 % (287) | 17.7 % (986) | 40.4 % (2.445) | 41.5 % (3.106) | 27.5 % (938) |
| Dysphagia | 1.5 % (425) | 0.4 % (4) | 0.6 % (30) | 0.6 % (36) | 1.5 % (88) | 2.0 % (153) | 3.3 % (114) |
| Neurologic disease | 1.3 % (362) | 0.5 % (5) | 0.5 % (22) | 0.9 % (52) | 1.7 % (100) | 1.6 % (117) | 1.9 % (66) |
| Parkinson | 1.6 % (447) | 0.0 % (0) | 0.0 % (0) | 0.1 % (3) | 0.5 % (33) | 3.4 % (258) | 4.5 % (153) |
| Epilepsy | 1.9 % (535) | 2.0 % (21) | 1.6 % (80) | 1.7 % (93) | 1.9 % (118) | 2.0 % (149) | 2.2 % (74) |
| Hepatic disease | 1.7 % (472) | 0.2 % (2) | 0.5 % (23) | 1.9 % (107) | 2.7 % (165) | 2.1 % (155) | 0.6 % (20) |
| Chronic renal disease | 0.2 % (44) | 0.0 % (0) | 0.0 % (0) | 0.0 % (1) | 0.1 % (6) | 0.3 % (21) | 0.5 % (16) |
| Rheumatologic disease | 4.7 % (1.335) | 0.6 % (6) | 0.7 % (35) | 1.9 % (104) | 4.3 % (261) | 7.8 % (582) | 10.2 % (347) |
| HIV | 1.0 % (295) | 0.2 % (2) | 1.4 % (70) | 3.5 % (196) | 0.4 % (23) | 0.1 % (4) | 0.0 % (0) |
| Poor dental hygiene | 11.8 % (3.359) | 9.1 % (94) | 10.0 % (485) | 11.5 % (639) | 14.3 % (865) | 13.6 % (1.021) | 7.5 % (255) |
| Low social status | 1.5 % (426) | 0.8 % (8) | 0.9 % (42) | 1.1 % (63) | 0.9 % (52) | 2.0 % (147) | 3.3 % (114) |
| Pneumococcal vaccination | 0.1 % (18) | 0.4 % (4) | 0.1 % (5) | 0.1 % (3) | 0.0 % (2) | 0.0 % (3) | 0.0 % (1) |
a Frequencies for categorical variables, number of patients between parenthesis
Incidence of CAP
Global incidence of CAP in adults was estimated at 4.63 per 1000 persons/year (Table 2). CAP incidence increased progressively with age, ranging from a 1.98 at 18–20 years of age to 23.74 in patients over 90 years of age (Table 2). According to gender, global CAP incidence was slightly higher in males (5.04) than females (4.26) (Table 2). CAP incidence from 18 to 65 year-olds up was comparable between males (range: 2.18–5.75) and females (range: 1.47–5.21), whereas from 65 years of age, CAP incidence was noticeable higher in males (range: 7.06–36.93) than in females (range: 5.43–19.62) (Table 2).
Table 2.
CAP incidence according to age and gender. Rates expressed per 1000 person-years
| Male | Female | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | n | p-y | Rate | Cases | n | p-y | Rate | Cases | n | p-y | Rate | |
| 18–20 years | 175 | 61,333 | 70,412.87 | 2.49 | 101 | 61,303 | 68,905.12 | 1.47 | 276 | 122,636 | 139,317.98 | 1.98 |
| 20–25 years | 433 | 79,410 | 196,125.36 | 2.21 | 329 | 89,087 | 204,046.95 | 1.61 | 762 | 168,497 | 400,172.31 | 1.90 |
| 25–30 years | 566 | 111,187 | 260,050.38 | 2.18 | 458 | 122,885 | 275,279.73 | 1.66 | 1024 | 234,072 | 535,330.11 | 1.91 |
| 30–35 years | 818 | 134,560 | 332,654.60 | 2.46 | 796 | 140,318 | 343,610.41 | 2.32 | 1614 | 274,878 | 676,265.01 | 2.39 |
| 35–40 years | 1070 | 123,355 | 336,083.56 | 3.18 | 1157 | 125,302 | 341,845.69 | 3.38 | 2227 | 248,657 | 677,929.25 | 3.29 |
| 40–45 years | 1074 | 108,836 | 306,130.49 | 3.51 | 1060 | 110,765 | 309,832.41 | 3.42 | 2134 | 219,601 | 615,962.90 | 3.46 |
| 45–50 years | 823 | 93,700 | 272,812.94 | 3.02 | 833 | 98,233 | 280,717.22 | 2.97 | 1656 | 191,933 | 553,530.15 | 2.99 |
| 50–55 years | 874 | 81,114 | 239,243.53 | 3.65 | 903 | 88,311 | 256,471.30 | 3.52 | 1777 | 169,425 | 495,714.83 | 3.58 |
| 55–60 years | 917 | 71,745 | 207,713.86 | 4.41 | 937 | 77,261 | 222,700.73 | 4.21 | 1854 | 149,006 | 430,414.59 | 4.31 |
| 60–65 years | 1097 | 64,835 | 190,729.33 | 5.75 | 1080 | 71,241 | 207,353.03 | 5.21 | 2177 | 136,076 | 398,082.36 | 5.47 |
| 65–70 years | 1098 | 48,791 | 155,627.10 | 7.06 | 935 | 54,759 | 172,088.42 | 5.43 | 2033 | 103,550 | 327,715.52 | 6.20 |
| 70–75 years | 1214 | 41,283 | 116,993.45 | 10.38 | 890 | 51,806 | 143,029.88 | 6.22 | 2104 | 93,089 | 260,023.33 | 8.09 |
| 75–80 years | 1604 | 36,855 | 109,640.33 | 14.63 | 1115 | 52,422 | 149,267.10 | 7.47 | 2719 | 89,277 | 258,907.43 | 10.50 |
| 80–85 years | 1472 | 25,189 | 75,766.96 | 19.43 | 1204 | 43,904 | 125,031.08 | 9.63 | 2676 | 69,093 | 200,798.03 | 13.33 |
| 85–90 years | 978 | 12,965 | 39,021.71 | 25.06 | 1081 | 28,978 | 83,030.03 | 13.02 | 2059 | 41,943 | 122,051.74 | 16.87 |
| 90–110 years | 514 | 4952 | 13,917.42 | 36.93 | 873 | 15,937 | 44,495.90 | 19.62 | 1387 | 20,889 | 58,413.33 | 23.74 |
| Total | 14,727 | 1,100,110 | 2,922,923.88 | 5.04 | 13.752 | 1,232,512 | 3,227,704.99 | 4.26 | 28,479 | 2,332,622 | 6,150,628.88 | 4.63 |
Risk factors for CAP
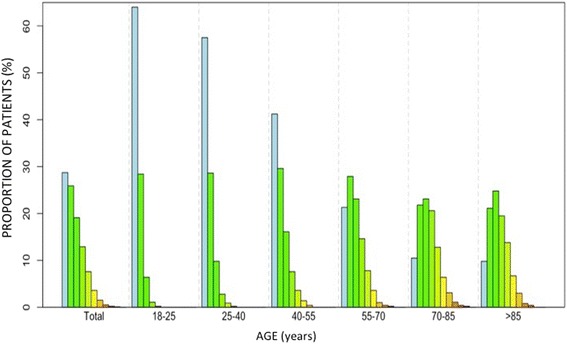
Overall, the main risk factors detected were: metabolic disease (27.4 %), cardiovascular disease (17.8 %), diabetes (15.5 %), depression (14.8 %), smoking (13.0 %), anemia (12.3 %), poor dental hygiene (11.8 %), chronic obstructive pulmonary disease (COPD) (10.8 %) and cerebrovascular disease (7.8 %) (Figs. 1 and 2).
Fig. 1.
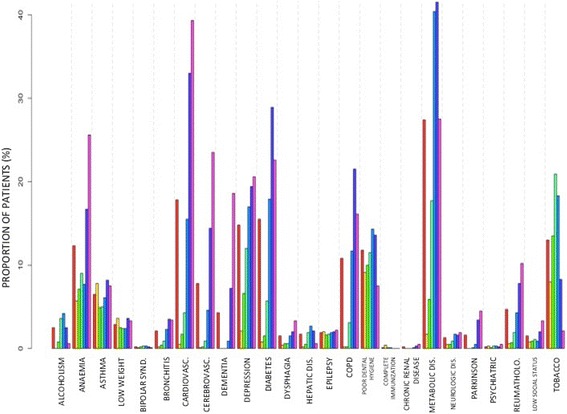
Distribution of the different lifestyle risk factors and comorbidities in patients seeking medical assistance because of pneumonia at primary care, according to age. Legend: 
Fig. 2.
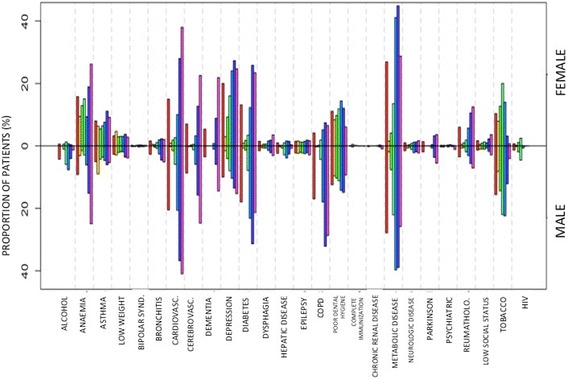
Distribution of the different lifestyle risk factors and comorbidities in patients seeking medical assistance because of pneumonia at primary care, according to gender. Legend: 
The main risk factors according to age were (Fig. 1): between 18 and 25 years: 9.1 % poor dental hygiene, 8.0 % smoking, 7.8 % asthma, 5.7 % anemia and 3.6 % low weight; between 25 and 40 years: smoking 13.5 %, 10.0 % poor dental hygiene, 7.1 % anemia, 6.6 % depression, 5.9 % metabolic disease and 4.9 % asthma; between 40 and 55 years: smoking 20.9 %, metabolic disease 17.7 %, depression 12.0 %, poor dental hygiene 11.5 %, and anemia 9 %; between 55 and 70 years: 40.4 % metabolic disease, smoking 18.3 %, 17.9 % diabetes, 17.0 % depression, 15.5 % cardiovascular disease, 14.3 %, poor dental hygiene and 11.7 % COPD; between 70 and 85 years: 41.5 % metabolic disease, 33.0 % cardiovascular disease, 28.9 % diabetes, COPD 21.5 %, 19.4 % depression, anemia 16.7 % and 14.4 % cerebrovascular disease; over 85 years: 39.3 % cardiovascular disease, 27.5 % metabolic disease, 25.6 % anemia, 23.5 % cerebrovascular disease, 22.6 % diabetes, 20.6 % depression, 18.6 % dementia and 16.1 % COPD.
The main risk factors according to gender were (Fig. 2): women: metabolic disease (26.9 %), depression (20.0 %), anemia (15.8 %) and cardiovascular disease (15.0 %); men: metabolic disease (27.8 %), cardiovascular disease (20.5 %), diabetes (17.9 %) and smoking (15.5 %). Overall, taking into account the total number of risk factors and stratifying them by age, a progressive increase with age is observed, with an exponential increase in males, which even doubles the risk from 75 years of age (Fig. 3).
Fig. 3.
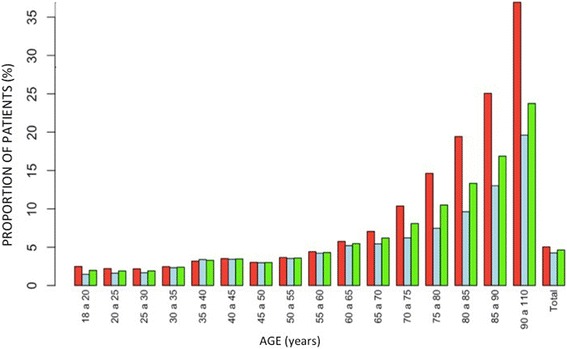
Global incidence of CAP stratified by age. Legend: 
Analyzing the number of comorbidities in terms of age, we note that less than 40 % of 18–25 year-old patients years showed any known risk factor, whereas after age 55 there is an identified risk factor in the 85.7 % of cases (one risk factor in 23.8 %, two factors in 23.4 %, three in 18.2 %, four in 11.2 %, five in 5.5 % and six in 2.3 %) (Fig. 4). The association of comorbidities showed no significant differences regarding sex in any age group.
Fig. 4.
Global prevalence of the different lifestyle risk factors and comorbidities stratified by age. Legend: 
Discussion
Our findings, based on the largest primary care population database in Spain, indicate a high incidence of CAP in primary care adults in Spain that is strongly associated with a high prevalence of multiple lifestyle risk factors and comorbidities. If we do not implement appropriate interventions, the currently high and increasing prevalence of these associated risk factors will likely lead to an even higher incidence of CAP in the aging population of Spain.
The global incidence of CAP in adults calculated in this study (4.63/1000 person-years) is coherent with the estimates from other Spanish studies, which range from 1.6 to 9 episodes per 1000 person-years [7]. According to these results, the percentage of CAP is higher in Spain compared to other European countries. As suggested by other publications, this may be associated with intrinsic differences in the structure of the health system and other factors such as heterogeneity in the entry criteria, or the possibility of care in the emergency unit, among others [13]. Furthermore, our results confirm the previous observations of higher incidence rates associated with men and older ages [14–16].
We found the highest burden of disease associated with metabolic disease, cardiovascular disease and diabetes. These findings are consistent with pooled data from observational studies which demonstrated that patients with other medical conditions such as chronic respiratory diseases, cardiovascular diseases, cerebrovascular diseases, dementia and diabetes mellitus were the most frequently observed comorbidities associated with CAP [10, 11, 16]. Up to two-thirds of patients had a chronic respiratory disease and almost half had a chronic cardiovascular disease, highlighting the need for appropriate management of these patients to reduce their risk of CAP.
Lifestyle factors such as smoking, high alcohol intake or being underweight have been associated with an increased risk of CAP [10, 11, 16], which is consistent with our findings. Smoking and excessive alcohol consumption are major health risks globally and are targets for interventions to reduce the global burden of disease. Ensuring that patients make appropriate lifestyle changes would help reduce the overall burden of CAP. Similarly, being underweight may predispose patients to CAP due to the consequences of undernutrition or underlying conditions on immune function, so assessment of the nutritional status of vulnerable patients might help identify those at increased risk of CAP.
Overall, we observed substantially increased rates of pneumonia among persons with >1 risk condition, and disease rates were especially high among those with ≥3 risk conditions. This is especially significant when noting that risk factors tend to increase over time: after age 55, we identified a risk factor in 85.7 % of cases, and risk even doubles from age 75. This phenomenon of “risk stacking”— whereby risk of disease increases with increasing numbers of risk factors —has been noted for other diseases, for example, osteoporotic hip fractures and cardiovascular events [17, 18].
One potential limitation of the study is the underestimation of CAP incidence, as doubtful cases where there was not sufficient information in the medical history, or diagnosis of presumption was made without radiological confirmation, were excluded. Another aspect to bear in mind is that not all patients are initially diagnosed in primary care. It is not uncommon for a person to go directly to the hospital without going through the general practitioner, and such cases would not be initially recorded in our database. However, patients are commonly referred to their general practitioner for follow-up, or they inform the doctor about the episode suffered during further consultation in the health center. Thus, even though some cases may initially visit the emergency room or be hospitalized, they can be classified as CAP, provided that the doctor registers the episode in the patient’s medical history.
One of the strengths of BIFAP is that it is one of the largest primary care databases available. It includes information provided by 2692 family physicians and primary care pediatricians from the National Health System, integrating information from 4,800,207 valid anonymized medical records for a total of 24,957,871 person-years of follow-up (5-year average patient tracking); including: 76,561,939 records of health problems, 414,852,056 medication records, 14,190,861 immunization records and 674,846,412 general records of patient data.
The organization of the Spanish public health system sets the primary care as the main gateway to other health services. Thus BIFAP includes a wealth of information on when, how and why patients visit primary care centers. Although the objective behind the development of this database was to facilitate pharmacoepidemiological studies, its potential is greater. With appropriate methods and after overcoming complex validation tests, BIFAP data can be used to calculate incidence and prevalence of diseases from thousands of patients, and to investigate risk factors and associated prognostic factors [19, 20]. This research is a population-based study, which could determine accurately the incidence and prevalence of risk factors of CAP in Spain, and demonstrates the utility of BIFAP as a resource to estimate the prevalence and incidence of disease.
Conclusions
The incidence of CAP in primary care adults in Spain is high, increases with age, and it is double in males as compared to females over 75 years of age. The main risk factors associated with CAP are metabolic disease, cardiovascular disease, and diabetes, all of them increasing nowadays, which could favor further increase in CAP incidence. Additional studies assessing risk stratification and a better understanding of the individual phenotypes with the greatest risk of CAP could help the development and implementation of the appropriate interventions in order to reduce the risk of infection and burden of CAP at the earliest level of medical care.
Acknowledgements
The authors would like to thank the collaboration from BIFAP team at the Spanish Medicines and Healthcare Products Regulatory Agency, and especially recognize the work from Mónica Ríos Martínez, María Consuelo Huerta Álvarez and Cristina Amil Bastardo.
NEUMOEXPERTOS group is national working group on pneumonia prevention endorsed by the Healthcare Research Insitute of Santiago de Compostela (Spain) and consisting of: F. Martinón-Torres, D. Vargas, E. Mascarós, E. Redondo, J.L. Díaz-Maroto, M. Linares-Rufo, A. Gil, J. Molina, D. Ocaña, I. Rivero-Calle.
Funding
This study has been partially sponsored by an unrestricted grant from Pfizer to the Healthcare Research Institute of Santiago de Compostela. The sponsor had no role in the design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and was ultimately responsible for the decision to submit this work for publication.
FMT’s research activities have been supported by grants from Instituto Carlos III (Intensificación de la actividad investigadora and FIS PI13/02382) from National Plan I + D + I and FEDER funds.
Availability of data and materials
Most of the data generated or analysed during this study are included in this published article [and its supplementary information files], although restrictions apply to the availability of some data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of BIFAP database.
Authors’ contributions
IRC, JPS and FMT drafted the manuscript. JPS performed the statistical analysis. All of the authors helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
FMT has received research grants and/or honoraria as a consultant/advisor and/or speaker and for conducting vaccine trials from GlaxoSmithKline, Sanofi Pasteur MSD, Merck, Sanofi Pasteur, Pfizer, Novartis, and MedImmune Inc. None declared for the rest of the authors.
ERM has received honoraria as a consultant/advisor and/or speaker, as well as grants for attending to conferences and practical courses from GlaxoSmithKline, Sanofi Pasteur MSD, Merck, Sanofi Pasteur, Pfizer and Novartis.
IRC has received grants for attending to a conference from GlaxoSmithKline.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The information contained in BIFAP is completely anonymous and includes no data that could identify patients, doctors or centers, ensuring full confidentiality. The Data Protection Agency considers that BIFAP meets the requirements of Law 14/2007 (adopted on July 3) on Biomedical Research regarding the protection of personal data and privacy. The Galician Research Ethics Committee granted permission for the study (Registration number 2014/623).
Abbreviations
- AEPAP
Asociación Española de Pediatría de Atención Primaria
- BIFAP
Computerized Database for Pharmacoepidemiological Studies in Primary Care
- CAP
Community-acquired pneumonia
- SEMERGEN
Sociedad Española de Médicos de Atención Primaria
- SEMFYC
Sociedad Española de Medicina Familiar y Comunitaria
Additional file
Different lifestyle risk factors and comorbidities associated to the first register of pneumonia. (DOCX 42 kb)
Contributor Information
I. Rivero-Calle, Email: irina667@hotmail.com
J. Pardo-Seco, Email: j.pardoseco@gmail.com
P. Aldaz, Email: pablo.aldaz.herce@cfnavarra.es
D. A. Vargas, Email: vdiegoa_@hotmail.com
E. Mascarós, Email: enmasba@sociedadgrap.com
E. Redondo, Email: redondome@madrid.es
J. L. Díaz-Maroto, Email: jdiazmarotom@semergen.es
M. Linares-Rufo, Email: manuellinares@fundacionio.org
M. J. Fierro-Alacio, Email: mjfierroalario@gmail.com
A. Gil, Email: angel.gil@urjc.es
J. Molina, Email: jmolinaparis@gmail.com
D. Ocaña, Email: ficusficus@gmail.com
Federico Martinón-Torres, Phone: +34 981 950615, Email: federico.martinon.torres@sergas.es.
on behalf of NEUMOEXPERTOS group:
F. Martinón-Torres, D. Vargas, E. Mascarós, E. Redondo, J. L. Díaz- Maroto, M. Linares-Rufo, A. Gil, J. Molina, D. Ocaña, and I. Rivero-Calle
References
- 1.Welte T, Torres A, Nathwani D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax. 2012;67:71–9. doi: 10.1136/thx.2009.129502. [DOI] [PubMed] [Google Scholar]
- 2.Blasi F, Mantero M, Santus P, Tarsia P. Understanding the burden of pneumococcal disease in adults. Clin Microbiol Infect. 2015;18(s5):7–14. doi: 10.1111/j.1469-0691.2012.03937.x. [DOI] [PubMed] [Google Scholar]
- 3.Lozano R, Naghavi M, Foreman K, Stephen L, Shibuya K, Aboyans V. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gil-Prieto R, Garcia-Garcia L, Alvaro-Meca A, Mendez C, Garcia A, de Miguel AG. The burden of hospitalisations for community-acquired pneumonia (CAP) and pneumococcal pneumonia in adults in Spain (2003–2007) Vaccine. 2011;29(3):412–6. doi: 10.1016/j.vaccine.2010.11.025. [DOI] [PubMed] [Google Scholar]
- 5.Loddenkemper R, Gibson G, Sibille Y. European lung white book. Brussels: European Respiratory Society and European Lung Foundation, The First Comprehensive Survey on Respiratory Health in Europe, ERSJ Ltd; 2003. [Google Scholar]
- 6.Rodriguez LA, Ruigomez A, Wallander MA, Johansson S. Acid-suppressive drugs and community-acquired pneumonia. Epidemiology. 2009;20(6):800–6. doi: 10.1097/EDE.0b013e3181b5f27d. [DOI] [PubMed] [Google Scholar]
- 7.Almirall J, Morato I, Riera F, Verdaguer A, Priu R, Coll P, et al. Incidence of community-acquired pneumonia and Chlamydia pneumoniae infection: a prospective multicentre study. Eur Respir J. 1993;6(1):14–8. [PubMed] [Google Scholar]
- 8.Schnoor M, Hedicke J, Dalhoff K, Raspe H, Schafer T. Approaches to estimate the population-based incidence of community acquired pneumonia. J Infect. 2007;55(3):233–9. doi: 10.1016/j.jinf.2007.04.355. [DOI] [PubMed] [Google Scholar]
- 9.Welte T, Kohnlein T. Global and local epidemiology of community-acquired pneumonia: the experience of the CAPNETZ Network. Semin Respir Crit Care Med. 2009;30(2):127–35. doi: 10.1055/s-0029-1202941. [DOI] [PubMed] [Google Scholar]
- 10.Torres A, Peetermans WE, Viegi G, Blasi F. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax. 2013;68(11):1057–65. doi: 10.1136/thoraxjnl-2013-204282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shea KM, Edelsberg J, Weycker D, Farkouh RA, Strutton DR, Pelton SI. Rates of pneumococcal disease in adults with chronic medical conditions. Open Forum Infect Dis. 2014;1(1):ofu024. doi: 10.1093/ofid/ofu024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelton SI, Shea KM, Weycker D, Farkouh RA, Strutton DR, Edelsberg J. Rethinking risk for pneumococcal disease in adults: the role of risk stacking. Open Forum Infect Dis. 2015;2(1):ofv020. doi: 10.1093/ofid/ofv020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64 Suppl 3:iii1–55. doi: 10.1136/thx.2009.121434. [DOI] [PubMed] [Google Scholar]
- 14.Gutierrez F, Masia M, Mirete C, Soldan B, Rodriguez JC, Padilla S, et al. The influence of age and gender on the population-based incidence of community-acquired pneumonia caused by different microbial pathogens. J Infect. 2006;53(3):166–74. doi: 10.1016/j.jinf.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 15.Falagas ME, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Respir Med. 2007;101(9):1845–63. doi: 10.1016/j.rmed.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 16.Vila-Corcoles A, Ochoa-Gondar O, Rodriguez-Blanco T, Raga-Luria X, Gomez-Bertomeu F. Epidemiology of community-acquired pneumonia in older adults: a population-based study. Respir Med. 2009;103(2):309–16. doi: 10.1016/j.rmed.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–73. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 18.Acharjee S, Qin J, Murphy SA, McCabe C, Cannon CP. Distribution of traditional and novel risk factors and their relation to subsequent cardiovascular events in patients with acute coronary syndromes (from the PROVE IT-TIMI 22 trial) Am J Cardiol. 2010;105(5):619–23. doi: 10.1016/j.amjcard.2009.10.042. [DOI] [PubMed] [Google Scholar]
- 19.Ruigomez A, Brauer R, Rodriguez LA, Huerta C, Requena G, Gil M, et al. Ascertainment of acute liver injury in two European primary care databases. Eur J Clin Pharmacol. 2014;70(10):1227–35. doi: 10.1007/s00228-014-1721-y. [DOI] [PubMed] [Google Scholar]
- 20.Requena G, Abbing-Karahagopian V, Huerta C, De Bruin ML, Alvarez Y, Miret M, et al. Incidence rates and trends of hip/femur fractures in five European countries: comparison using e-healthcare records databases. Calcif Tissue Int. 2014;94(6):580–9. doi: 10.1007/s00223-014-9850-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Most of the data generated or analysed during this study are included in this published article [and its supplementary information files], although restrictions apply to the availability of some data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of BIFAP database.


