Abstract
Aim:
To study the prevalence of Psychiatric disorders in cancer patients and to find out the factors associated with Psychiatric disorders in Cancer Patients.
Settings and Design:
Department of Radiotherapy, Medical College, Thiruvananthapuram, cross sectional survey design was used.
Methods and Material:
Adult patients (18 years of age and above), having a diagnosis of carcinoma were selected by consecutive sampling method.A questionnaire which included back ground data, socio economic variables, treatment variables like type of malignancy, exposure to radiation & chemotherapy prior to the evaluation and current treatment, co occurring medical illness & treatment and past & family history of psychiatric illness was used to collect data. Delirium rating scale and MINI International neuropsychiatric interview were used to assess Psychiatric disorders and delirium.
Statistical Analysis Used:
Chi square and logistics regression tests were used for analysis.
Results:
Of the 384 assessed, 160(41.7%) had psychiatric disorders. Adjustment disorders were seen in 22.6%. 10.9% of subjects had major depressive disorder. Thus a total of 33.5% of patients had a diagnosis of either anxiety or depressive disorder. Proportion of patients having delirium was 6.5%. Hypomania was seen in small (1.6%) of patients. Multivariate analysis for various parameters for psychiatric disorders showed that age, past history of chemotherapy, past history of radiotherapy, & surgical treatment of carcinomas are significant predictors of psychiatric disorders.
Conclusions:
Psychiatric disorders are seen in a significant proportion of Psychiatric patients.
Key words: Adjustment disorders, cancer, delirium, depression, mood disorders
INTRODUCTION
Cancer is a leading cause of death worldwide accounting for 7.6 million deaths (around 13% of all deaths) in 2008, and about 70% of all cancer deaths occurred in low- and middle-income countries. Deaths from cancer worldwide are projected to continue to rise to over 11 million by 2030.[1] India is no exception to this, population-based cancer registries within the National Cancer Registry Programme and outside the network has provided a picture of the cancer pattern in India based on which it is estimated that there will be about 800,000 new cancer cases in India every year. At any given point, the prevalence is likely to be three times this load that is about 2,400,000 cases in a year.[2]
The experience of having cancer has been associated with high levels of psychological stress. Galen noted a relationship between dysphoric affect and cancer long ago.[3] Correlations between neoplasia and psychological disorders were noted by numerous 18th and 19th century physicians.[4] An illness like cancer can have various psychiatric sequelae as a result of the disease itself or due to associated problems. The diagnosis of cancer itself when revealed to the patient can cause emotional reactions such as shock and disbelief, followed by anger, depression, loss, and grief.
Adjustment disorder is the most common psychiatric syndrome in cancer patients.[5] Conceptually, these are disorders with emotional and behavioral symptoms which are responses to an identifiable stressor.[6] A life-threatening illness like cancer will definitely have emotional consequences.
There have been many criticisms against the prevalence studies of psychiatric illness in cancer. Most researchers limited their focus to specific forms of a psychological disorder such as “depression,” and few included formal complete psychiatric evaluation in their designs, other investigators concentrated on the general psychological adjustment of the cancer patient, utilizing symptom, and mood measures to estimate levels of well-being rather than to measure the prevalence of disorder.
To plan interventions efficiently, it is important to gain insight into the prevalence, severity, course of the psychological sequelae, and the variables influencing them. In a state like Kerala where the incidence of cancer is on the increase, an exact estimation of the prevalence of adjustment disorders and other psychiatric illnesses is very important in planning management strategies. It is in this context that the study was planned to find the prevalence of psychiatric illnesses in cancer patients.
MATERIALS AND METHODS
This cross-sectional study was conducted at the Department of Radiotherapy, Medical College, Thiruvananthapuram, a tertiary care teaching hospital with inpatient beds. Adult patients (18 years of age and above) having a diagnosis of carcinoma consecutively admitted for 1 year during 2011 and 2012 were the subjects for the study. Patients under evaluation but not having a definite diagnosis of cancer, as well as those patients not willing to give consent, were excluded from the study. For an expected prevalence of psychiatric disorders of 20% in this population and an expected variation of 20%, the sample size was calculated to be 384.
The study questionnaire included background data; socioeconomic variables; treatment variables such as type of malignancy, exposure to radiation, and chemotherapy prior to the evaluation and current treatment; co-occurring medical illness and treatment; and past and family history of psychiatric illness. It also included following instruments which were used to assess the psychiatric morbidity:
Delirium rating scale is a 10-item clinician-administered questionnaire for assessing delirium, with scores ranging from zero to three or four.[7] With a cutoff score of ten points, sensitivity and specificity of the instrument were 0.94 and 0.82, respectively[8]
Mini-International Neuropsychiatric Interview (MINI)[9] is a structured diagnostic interview schedule for diagnosing psychiatric problems based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and International Classification of Diseases-10. Its psychometric properties have been established in primary care settings and medically ill population.[10] A translated version in Malayalam was used for diagnoses like major affective disorders and anxiety disorders.[11] As there was no translated version for adjustment disorders, the adjustment disorder module from MINI plus was translated to Malayalam by translation-retranslation method. The psychometric properties of the said scale were assessed in the outpatient wing of the Department of Psychiatry Medical College Trivandrum and was found to have good psychometric properties.[12]
RESULTS
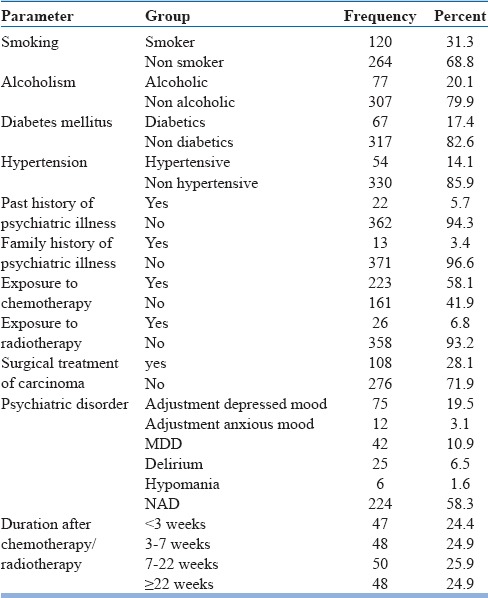
Distribution of clinical variables [Table 1] showed that 31.3% of patients were smokers and 20.1% were using alcohol. About 17.4% had diabetes and 14.1% had hypertension. Past history of psychiatric illness and family history of psychiatric illness were seen in 5.7% and 3.4%, respectively. About 58.1% of patients were on chemotherapy, 6.8% were on radiotherapy, and 28.1% had surgical interventions for carcinoma.
Table 1.
Clinical variables
Of the 384 subjects assessed, 160 (41.7%) had a psychiatric disorder in this study. Adjustment disorder as a group was seen in 22.6%. Of these, adjustment disorder with depressed mood was seen in 19.5% and adjustment disorder with anxious mood was seen in 3.1%. About 10.9% of subjects had major depressive disorder. Thus, a total of 33.5% of patients had a diagnosis of either anxiety or depressive disorder. The proportion of patients having delirium was 6.5%. Hypomania was seen in small (1.6%) of patients. In a study conducted in India,[13] 38% of cancer patients were found to have identifiable DSM-III-R anxiety or depressive disorder. Our findings are consistent with the above study.
Association between the presence of psychiatric disorders and sociodemographic factors is given in Table 2.
Table 2.
Association between psychiatric disorders and socio demographic factors
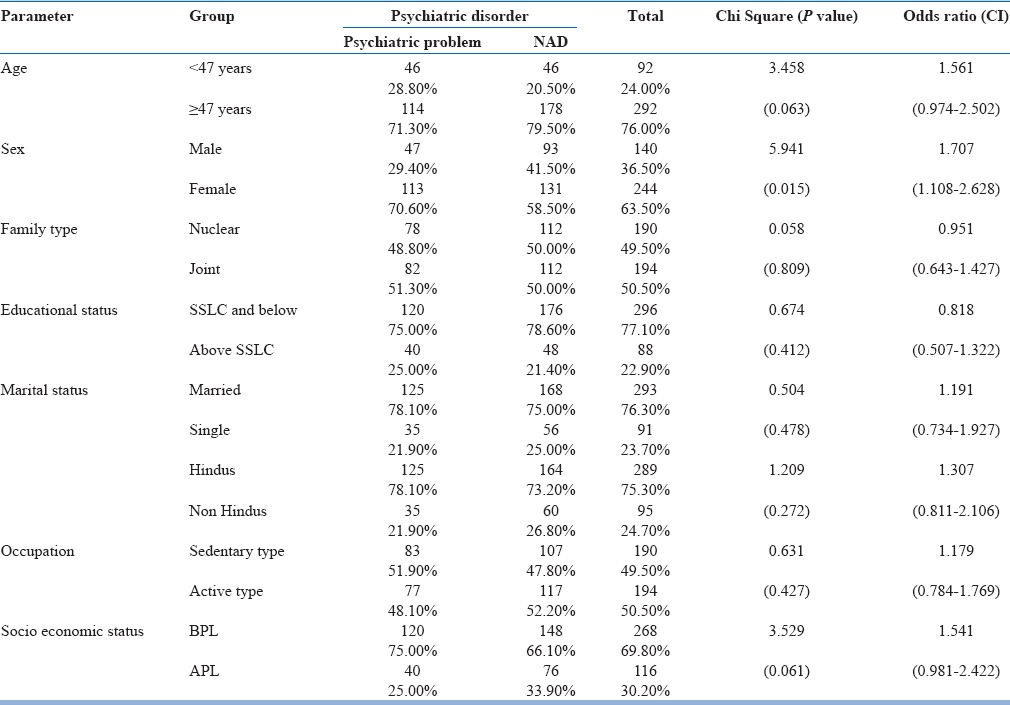
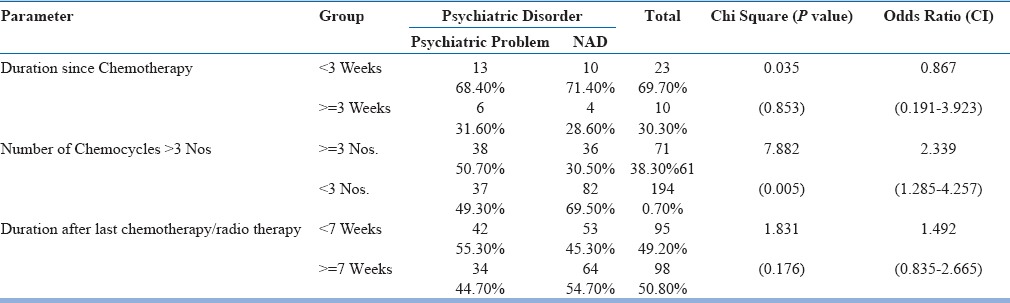
Cut-off age of 47 was taken as it represented the median value. From the study it is seen that Psychiatric disorders are more seen in females (odds ratio [OR] =1.707, confidence interval [CI] =1.108–2.628; P = 0.015). Psychiatric disorders increase with a number of chemotherapies (OR = 2.339, CI = 1.285–4.257 P = 0.005), but no such relationship was seen for the duration since last chemotherapy [Table 3].
Table 3.
Association between the presence of psychiatric disorders and chemotherapy variables
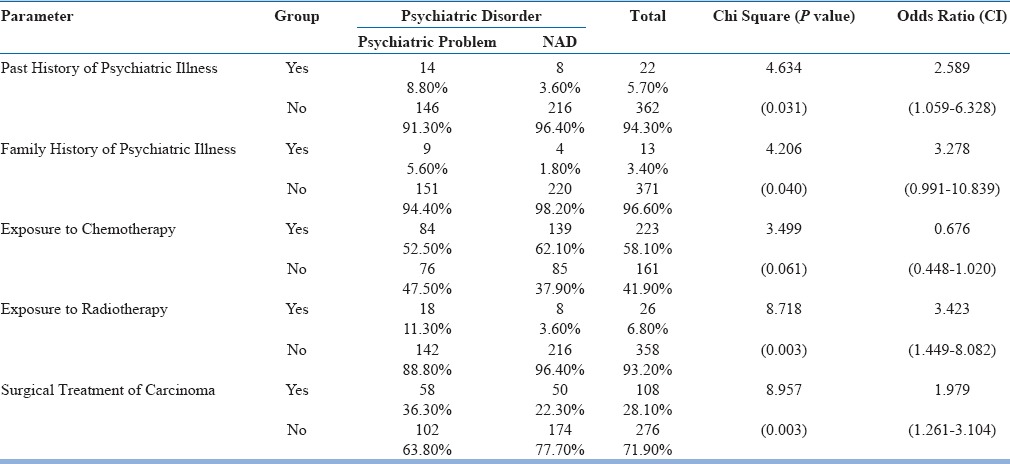
Association between psychiatric disorders and clinical and carcinoma-related variables [Table 4] shows that history of psychiatric illness (OR = 2.589, CI = 1.059–6.328 P = 0.031), family history of psychiatric illness (OR = 3.278, CI = 0.991–10.839 P = 0.040), exposure to radiotherapy (OR = 3.423 CI = 1.449–8.082: P =0.003), and surgical treatment of carcinoma (OR = 1.979 CI = 1.261–3.104 P = 0.003) were associated with psychiatric disorders, but no significant relationship is seen with exposure to chemotherapy (OR = 0.676, CI = 0.448–1.020; P = 0.061).
Table 4.
Association between psychiatric disorders and clinical and carcinoma-related variables
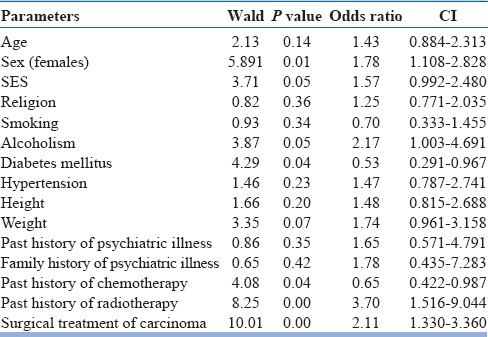
Binary logistic regression analysis for various parameters for psychiatric disorders is shown in Table 5. It is seen that female gender, history of radiotherapy, and surgical treatment of carcinomas are significant predictors of psychiatric disorders. However, history of chemotherapy was associated negatively with psychiatric disorders, may be because of the fact that chemotherapy is often chosen in the early stage of treatment. Alcoholism which was not associated with psychiatric disorders in univariate analysis became significant in multivariate analysis because the gender effect was adjusted. Thus, gender was a confounding factor in the relationship between alcoholism and psychiatric disorders. There was a negative relationship between diabetes and psychiatric disorders.
Table 5.
Binary logistic regression analysis results
DISCUSSION
In this study of 384 cancer patients admitted in the radiology ward of a teaching hospital, 160 patients (41.7%) had psychiatric disorders. Derogatis et al. had found a prevalence was 47%,[5] but in a study conducted in India by Chaturvedi et al., 38% of cancer patients had identifiable DSM-III-R anxiety or depressive disorders.[13] Our results are comparable with the results from Indian study.
Major depressive disorder was seen in 10.9% of patients. Reported prevalence of major depression varied from 0% to 38% which was explained by factors such as varying conceptualizations of depression, different criteria used to define depression, differences in methodological approaches to the measurement of depression, and different populations studied.[14] It has to be noted that prevalence of depression in general medical and primary practice populations tend to be more consistently in the 12–30% range.[15,16]
Delirium was seen in 6.5% of patients; the prevalence of delirium in cancer patients has been reported as 5–30% and is substantially higher in the terminal stage of illness.[17]
Our study sample consisted mainly of patients admitted in the ward for chemotherapy and at a less severe stage of illness, this could be the reason for comparatively lesser prevalence of depression and delirium.
The relationship between psychiatric disorders and sociodemographic factors showed that females had more chances of developing a psychiatric disorder. A study from Kerala by Pandey et al. also showed similar results.[18]
Association between psychiatric disorders and chemotherapy showed that psychiatric disorders increase with a number of chemotherapies. It could be because medications used in chemotherapy can cause neuropsychiatric sequelae. The findings such as history of psychiatric illness, family history of psychiatric illness, exposure to radiotherapy, and surgical treatment of carcinoma are associated with psychiatric disorders is a replication of previous studies.[19,20]
Multivariate analysis for various parameters for psychiatric disorders showed that age, history of chemotherapy, history of radiotherapy, and surgical treatment of carcinomas are significant predictors of psychiatric disorders.
A meta-analysis of 58 studies after 1980 showed that studies with younger patients[21] (mean age <50 years) reported significantly more depression, anxiety, and general distress than studies with older patients (mean age 50 years or over). In our study also psychiatric problems were more in younger patients (age >47 years).
The history of chemotherapy has been shown to be associated with psychiatric problems. In a study from Kerala by Pandey et al.,[18] it was shown that among patients undergoing chemotherapy, 15.38% were found to have anxiety, while 16.23% had depression.
The history of radiotherapy has been shown to be associated with psychiatric problems. In a study among patients receiving radiotherapy by Schmale et al.[20] have shown significant psychiatric problems associated with radiotherapy.
Surgical treatment of carcinomas has been associated with psychiatric problems. In studies among 160 women awaiting breast surgery, Morris et al.[22] found a 22% prevalence of depression in women who had a mastectomy for breast cancer and Maguire et al.[19] found 26% moderate or severe depression among women who had mastectomy compared with a 12% prevalence of depression in women with benign disease.
Limitations of the study
Sample consisted of patients admitted in hospital for chemotherapy and so the results may not be a true reflection of the cancer patients
As patients taking radiotherapy were not usually admitted in wards, the sample contained less number of radiotherapy cases and this might have influenced the findings
Most of the patients taking chemotherapy were at a less severe stage of illness and so the results might reflect the morbidity in patients taking chemotherapy
Duration of diagnosis of cancer to assessment time was not included as a study variable. The psychiatric morbidity could be influenced by time-dependent factors since diagnosis
Usage of opioid analgesics or psychotropic agents was not included as a variable in the study which is a limitation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v2.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10. Lyon, France: International Agency for Research on Cancer; 2010. [Last accessed on 2012 Dec 02]. Available from: http://www.globocan.iarc.fr . [Google Scholar]
- 2.Government of India. Director General of Health Services. 50 Years of Cancer Control in India. c2003. [Last updated on 2011 Feb 28, Last cited on 2012 Dec 12]. Available from: http://www.mohfw.nic.in/index1.php?lang=1&level=3&sublinkid=340&lid=193 .
- 3.Goldfarb C, Driesen J, Cole D. Psychophysiologic aspects of malignancy. Am J Psychiatry. 1967;123:1545–52. doi: 10.1176/ajp.123.12.1545. [DOI] [PubMed] [Google Scholar]
- 4.Guy R. An Essay on Scirrhus Tumors and Cancers. London: J and A Churchill; 1759. [Google Scholar]
- 5.Derogatis LR, Morrow GR, Fetting J, Penman D, Piasetsky S, Schmale AM, et al. The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751–7. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (Revised 4th Edition) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 7.Trzepacz PT, Baker RW, Greenhouse J. A symptom rating scale for delirium. Psychiatry Res. 1988;23:89–97. doi: 10.1016/0165-1781(88)90037-6. [DOI] [PubMed] [Google Scholar]
- 8.Trzepacz PT. The delirium rating scale. Its use in consultation-liaison research. Psychosomatics. 1999;40:193–204. doi: 10.1016/S0033-3182(99)71235-1. [DOI] [PubMed] [Google Scholar]
- 9.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 10.Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, et al. The Mini International Neuropsychiatric Interview (MINI).A short diagnostic structure interview: Reliability and validity according to CIDI. Eur Psychiatry. 1997;12:224–31. [Google Scholar]
- 11.Kumar CT, Dinesh N, Cherkil S, Satish S, Mathew S, Kallumpuram SV, et al. An introduction to the mini international neuropsychiatric interview (MINI) and its Malayalam version. Kerala J Psychiatry. 2010;24:41–5. [Google Scholar]
- 12.Roy GM, Vidhukumar K, Anil P. Criterion Validity of the Translated Malayalam Version of the Adjustment Disorder Module from MINI 6.0 in a Tertiary Care Centre. Paper Presented at: National Conference of Indian Association of Private Psychiatry; 12-14 November, 2011; Trivandrum. [Google Scholar]
- 13.Chaturvedi SK, Chandra P, Channabasavanna SM. Detection of anxiety and depression in cancer patients. NIMHANS J. 1994;12:141–4. [Google Scholar]
- 14.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;32:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 15.Hoeper EW, Nycz GR, Cleary PD. Estimated prevalence of RDC mental disorder in primary medical care. Int J Ment Health. 1979;8:6–15. [Google Scholar]
- 16.Houpt JL, Orleans CS, George LK. The Importance of Mental Health Services to General Health Care. Cambridge, Massachusetts: Ballinger Publishing Co.; 1979. [Google Scholar]
- 17.Fleishman S, Lesko L, Breitbart WS. Treatment of organic mental disorders in cancer patients. In: Breitbart WS, Holland JC, editors. Psychiatric Aspects of Symptom Management in Cancer Patients. Washington: American Psychiatric Press; 1993. pp. 23–47. [Google Scholar]
- 18.Pandey M, Sarita GP, Devi N, Thomas BC, Hussain BM, Krishnan R. Distress, anxiety, and depression in cancer patients undergoing chemotherapy. World J Surg Oncol. 2006;4:68. doi: 10.1186/1477-7819-4-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maguire GP, Lee EG, Bevington DJ, Küchemann CS, Crabtree RJ, Cornell CE. Psychiatric problems in the first year after mastectomy. Br Med J. 1978;1:963–5. doi: 10.1136/bmj.1.6118.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmale AH, Morrow GR, Davis A, Illies E, McNally J, Wright G, et al. Pretreatment behavioral profiles associated with subsequent psychosocial adjustment in radiation therapy patients: A prospective study. Int J Psychiatry Med. 1982;12:187–95. doi: 10.2190/w8ky-6bb2-ajwp-re27. [DOI] [PubMed] [Google Scholar]
- 21.van’t Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological sequelae of cancer diagnosis: A meta-analytical review of 58 studies after 1980. Psychosom Med. 1997;59:280–93. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Morris T, Greer HS, White P. Psychological and social adjustment to mastectomy: A two-year follow-up study. Cancer. 1977;40:2381–7. doi: 10.1002/1097-0142(197711)40:5<2381::aid-cncr2820400555>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]


