Abstract
Context and Aims:
Ureteroscopy is the definitive management for ureteric stone. Conventional ureteroscopy uses fluoroscopy guidance which has radiation exposure to patients as well as hospital staff. Ultrasound is a good radiation-free alternative for using in the urological procedure. With this background, we executed a prospective randomized trial comparing fluoroscopy-guided ureteroscopy versus ultrasound-guided ureteroscopy.
Subjects and Methods:
Patients were randomized into two groups (41 into fluoroscopy and 41 into ultrasound group after exclusion) in a single center from July 2014 to March 2015. Semi-rigid ureteroscopy was used in all cases. Ultrasound was used to place guide wire and postprocedure stents placement in ultrasound group. Patient's characteristics; intra- and post-operative parameters were compared between the two groups.
Statistical Analysis Used:
SPSS version 16.0 (Chicago, IL, USA) was used for statistical analysis. The results were presented as percentages and means (± standard deviation). The categorical/dichotomous variables were analyzed using Chi-squared test. Continuous variables were analyzed using unpaired t-test.
Results:
A total of 102 adult patients were randomized in this trial and eighty patients undergo the final analysis. Mean stone burden was 41.75 ± 13.44 (17.94–79.20 mm2). Mean operative time was 43.90 ± 12.99 (25–82 min) in fluoroscopy group versus 45.61 ± 11.62 (28–78 min) in ultrasound group. The initial success rate was 93.75% (92.30% in fluoroscopy vs. 95.12% in ultrasound group). Overall complications noted in 8.75% and most of the complications were minor in nature.
Conclusions:
Ultrasound-guided ureteroscopy is safe and effectively for ureteric stone. Fluoroscopy can be avoided during ureteroscopy for uncomplicated stone. No radiation ureteroscopy is feasible with good success and minimal complication. Larger sample size with multicentric trial needed for its greater applicability.
Key Words: Fluoroscopy, radiation, ultrasonography, ureteroscopy
INTRODUCTION
The lifetime risk of urinary stone disease varies 3–12% in the western countries.[1] Medical expulsive therapy is usually preferred for uncomplicated small and distal ureteric stones with variable success rate. However, the definitive management of ureteral stone is ureteroscopic retrieval. Ureteroscopy has a high success rate (81–94%) and can clear stone in a single procedure in most of the cases with acceptable short- and long-term complication.[1,2] Ureteroscopy is usually performed under fluoroscopy guidance which has a risk of radiation exposure. Radiation has many harmful effects to patient and hospital stuff. Prolonged radiation exposure could have malignancy potential also.[3,4] There is growing concern about radiation health hazard all over the world.[5] To cut short this radiation exposure, ultrasound is a good alternative because it is radiation free and gives a good visualization of upper tracts; it is portable and of value in pregnant women. With this background, we prospectively compared the safety, efficacy, and outcome of ureteroscopy with fluoroscopy versus ureteroscopy with real-time ultrasonography for the management of ureteral stones.
SUBJECTS AND METHODS
Study design
A total of 102 adult patients (>15 years) were randomized into the study. Twenty-two patients were excluded before ureteroscopy procedure (size >1 cm, n = 20, and spontaneous stone passage, n = 2). Patient with calculus >1 cm, solitary kidney, compromised renal function (creatinine >1.4 mg/dl) were excluded from the study. Patients were randomized with computerized random number into either group fluoroscopy guided ureteroscopy (A) versus real-time ultrasound-guided ureteroscopy (B). All the procedures were done in a single operation theater having both fluoroscopy and ultrasound facility. If the ultrasound-guided procedure was not successful, then fluoroscopy guidance was taken as per prior ethical approval. Dilation of the orifice was performed with the help of 8 Fr balloon dilator under direct vision with 22 Fr cystoscope if needed.
The following demographic parameters were collected: Age, sex, stone related data, previous treatments, urine culture, plain X-ray kidney, ureter, and bladder (KUB), ultrasound KUB, excretory urogram, intra- and post-operative data including clearance and complications in both the groups. All patients were treated according to urine culture report with antibiotic before surgery if needed. Stone size was calculated by multiplying two largest dimensions on radiological study available (plain X-ray KUB, ultrasound KUB, and excretory urogram).
Operative technique
Semi-rigid ureteroscopy (6.5/8.5 Fr, Wolf, Richard Wolf Medical Instruments Corporation, Vernon Hills, IL, USA) was performed in all patients according to the standard technique by experienced urologists. Detailed imaging has been studied in all patients before ureteroscopy. In the ultrasound group, after cystoscopy we put a 0.035” guidewire (Terumo flexible tip guide wire) with tactile sensation and confirmed the position in the pelvis with real-time ultrasound (Acuson X300 Ultrasound System, Siemens Healthcare GmbH, Federal Republic of Germany). Holmium laser (365 nm fibre, Auriga Holmium Laser System, Star Med Tec GmbH, Starnberg, Germany) was used for stone fragmentation in both the group. Fragments were removed with removal forceps. In Group A, after stone clearance, fluoroscopy (Siemens Multimobil 5E System, Siemens Healthcare GmbH, Federal Republic of Germany) guided 5/6 Fr double J stent was placed. In Group B (ultrasound guided) after stone clearance a 5/6 Fr double J stent was placed and negotiated up to pelvis which was again confirmed by ultrasound. We removed Foley catheter on day 1 postoperative period. Imaging includes X-ray KUB, renal and bladder ultrasound on postoperative day 1. Double J stent was removed after 2 weeks under sedation and antibiotic coverage. Patients were followed up regularly at 1 month and 3 months with plain X-ray KUB and ultrasound KUB for each group.
Statistical analysis
SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The results were presented as percentages and means (± standard deviation). The categorical/dichotomous variables were analyzed using Chi-squared test. Continuous variables were analyzed using unpaired t-test.

RESULTS
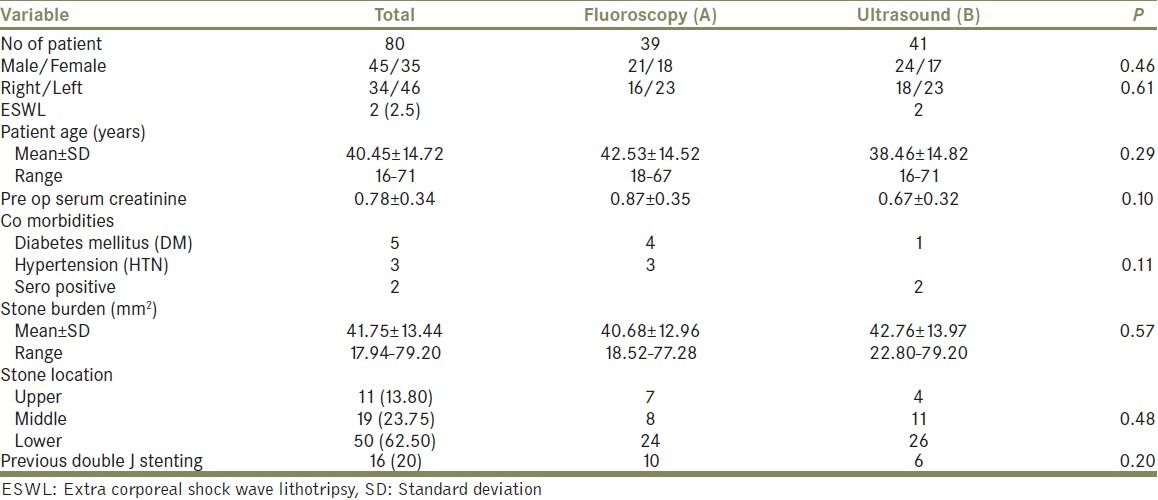
Mean age (range) of the study group was 40.45 ± 14.72 with fluoroscopy group (A) having 42.53 ± 14.52 (range 18–67) and ultrasound group (B) having 36.12 ± 11.84 (range 16–71). The mean stone burden was 41.75 ± 13.44 (17.94–79.20 mm2) with fluoroscopy group of 40.68 ± 12.96 (18.52–77.28 mm2) and ultrasound group of 42.76 ± 13.97 (22.80–79.20 mm2). History of extracorporeal shock wave lithotripsy was found in two patients (both in ultrasound group). Mean serum creatinine in the preoperative period was 0.78 ± 0.34 (fluroscopy-0.87 ± 0.35 vs. ultrasound-0.67 ± 0.32). Preoperative data of ureteroscopy procedure is depicted in Table 1.
Table 1.
Preoperative data of ureteroscopy procedure: No of patient, n (%)
Mean operative time was 43.90 ± 12.99 (25–82 min) in fluoroscopy group versus 45.61 ± 11.62 (28–78 min) in ultrasound group. Mean radiation exposure time in fluoroscopy group was 40.97 ± 22.68 (10–95 s). The initial success rate was 93.75% (75/80) of which 92.30% (36/39) in fluoroscopy versus 95.12% (39/41) in ultrasound group. Up migration of stones in the kidney occurred in two cases (both in Group A) which were managed successfully with stented shock wave lithotripsy. Operative and postoperative data is depicted in Table 2.
Table 2.
Operative and post operative data: No of patients, n (%)
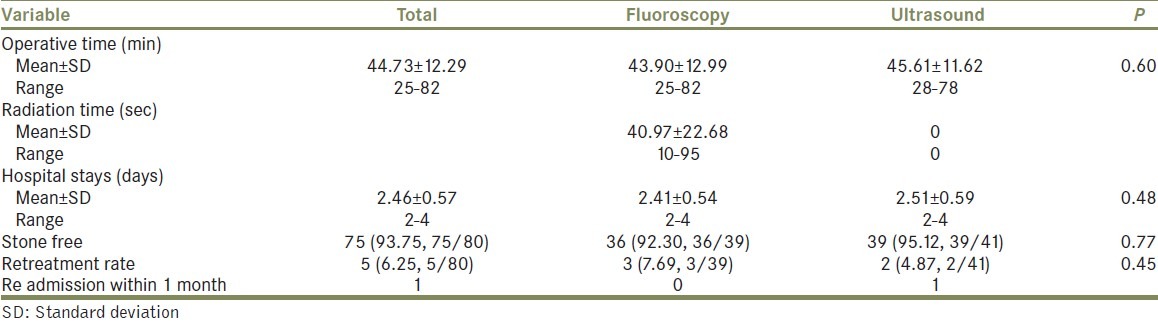
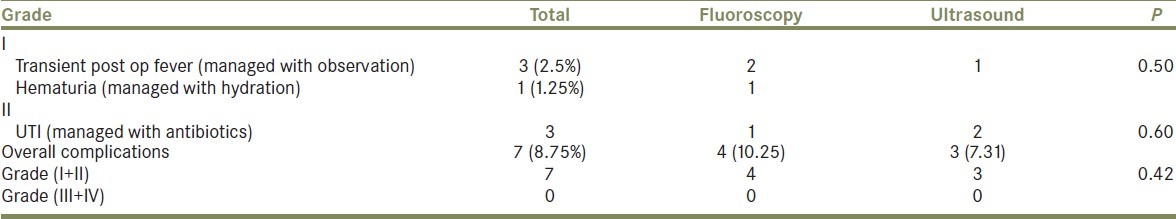
Retreatment (re-ureteroscopy) was needed in three patients over 1st month follow-up. Overall complications noted in 8.75% (7/80). Most of the complications were minor in nature (complications are described in Table 3). Minor complication includes postoperative fever (Clavien Grade I) in 3 cases which was managed conservatively, hematuria (Clavien Grade I) in 1 case which was managed with hydration. Urinary tract infection (Clavien Grade II) in two patients which was managed with antibiotics on outpatient basis. One patient required readmission for persistent fever on postoperative day 6 which was managed with double J stent removal and intravenous antibiotics. There was no Clavien Grade III/IV complication in both the group.
Table 3.
Complications according to modified Clavien Grading: No of complications, n (%)
DISCUSSION
There is no safe dose of radiation. Fluoroscopy emits a significant amount of radiation not only to the patient but also to the hospital staff. With increasing incidence of urinary tract stones disease, patient populations such as recurrent renal or ureteric stone formers may be at higher risk because of repeated exposures to ionizing radiation. The cumulative dose of radiation to patients and hospital staff may increase relatively rapidly where fluoroscopy is used. Hence, there is always some attempt to decrease the radiation dose and or to use alternate method that does not have radiation risk.
The main disadvantage of fluoroscopy is radiation hazards in comparison to ultrasound for imaging urinary tract calculus. Prolonged and cumulative radiation doses have high chances of secondary malignancy. Other than malignancy, high skin exposure led to tissue injury also.[3] Centre for Devices and Radiological Health of the Food and Drug Administration has raised concern over growing incidence of radiation-induced burn to both patients and staff.[5]
Three principle steps are recommended to decrease the radiation doses such as limiting radiation exposure time (short bursts of fluoroscopy and last image hold method), increasing distance from the radiation source and using a protective shield (lead apron and thyroid shields). Wearing lead apron to avoid radiation exposure is quite uncomfortable.
Recently, fluoroless ureteroscopy and or decreased radiation protocol has also been described.[6,7] Ureteroscopy is the conventional preferred approach for management of ureteral calculus. Ureteroscopy can be used for ureteral calculus in all location because of newer development in ureteroscopy and lasers such as holmium laser.[8] Ultrasound can be used as a substitute for this purpose. In urological procedure, ultrasound is a versatile tool and applicable to all age group including pregnant patients also due to its no radiation hazards. Ultrasound is already used in performing percutaneous nephrostomy[9] in some center and in the pregnant patient[10] for double J stent placement. However, the use of ultrasound needs special expertise in ultrasound with recent machine and high resolution.
In a study by Deters et al.[11] they achieved a success rate of 86% stone-free rate with ultrasound-guided ureteroscopy time of 45.72 min and fluoroscopy-guided ureteroscopy of 36.52 min. However, they have taken only those patients who had been stented previously. In another study by Peng et al.[12] they showed that retrograde intrarenal surgery is feasible without fluoroscopy. In that study 95.7% of stone-free rate was achieved over 1 month with minimal complication. In this study, we have achieved stone-free rate of more than 90% in both group (Fluoroscopy-92.30% vs. Ultrasound-90.24%). We did not routinely stented the patients preoperatively. Only 20% of patients had preoperative stent in situ for an average duration of 1 month where balloon dilation was not required. In another study by Peng et al.[12] using low radiation fluoroscopy, they were able to keep the total fluoroscopy time 0–35 s with excellent success and low complications rate. In another study by Scarpa et al.,[13] they performed successful rigid ureteroscopy in 15 pregnant patients with the help of ultrasound only.
We have selected the patients of ureteric stone with size <1 cm as per ethical approval. We belief larger stone (size >1 cm) can also be approached with ultrasound guidance. As impacted stone is the main cause for inability to negotiate guide wire beyond the stone, then fluoroscopy guidance also may not be successful to pass guide wire in those cases as like ultrasound. Further study may be helpful to prove this. Most of the endo urologists are familiar with fluoroscopy guided ureteroscopy which is time tested, but ultrasound may have a role in cases of ureteric stone management in the coming future. Despite this surgeon can take the help of ultrasound initially and use the fluoroscopy guidance only if guide wire could not be able to pass with ultrasound. This may significantly help the patients as well as medical staff to avoid radiation exposure without significantly increasing the operation time.
In two patients, we had difficulty in bypassing guide wire beyond the stone in the ultrasound group (both in the mid ureteric location) because of impacted stones and for the same reason fluoroscopy guidance was not taken. In these cases, we have negotiated the ureteroscopy up to the stone and fragmented and then guide wire negotiated into the pelvi calyceal system.
Fluoroless ureteroscopy has a reported complications rate of 3.7–8.0%, most of which are minor complications.[1,10] We did not have any complication of ureteric perforation intraoperatively or strictures formations over 3 months follow-up in any of the group. Re procedure rate in our study was 6.25% which was less than reported in the literature.[10]
Ultrasound-guided ureteroscopy have several advantages. There was no radiation exposure to this Group (B). Real-time ultrasound with high-resolution probe was able to guide placement of ureteric guide wire and double J stent continuously during the whole procedure. The extra technician for fluoroscopy unit was not required as surgeon or assistant can hold the ultrasound probe to guide the placement of safety wire.
Limitation of the study
Our study has some shortcomings. We tried best possible matching between the groups. We did not use computed tomography scan in the preoperative as well as postoperative follow-up period which is standard for diagnosis of ureteric calculus. The sample size is relatively small. Despite all these limitations, this study shows that ultrasound may be used safely and effectively during management of ureteric stones.
CONCLUSION
Radiation hazard can be abolished during ureteroscopy in selected cases. Ultrasound is good enough for this purpose. Ultrasound is safe, effective, and radiation-free method. However, larger sample size and multi-institutional study are required to establish its wider acceptability.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178:2418–34. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 2.Johnson DB, Pearle MS. Complications of ureteroscopy. Urol Clin North Am. 2004;31:157–71. doi: 10.1016/S0094-0143(03)00089-2. [DOI] [PubMed] [Google Scholar]
- 3.Mahesh M. Fluoroscopy: Patient radiation exposure issues. Radiographics. 2001;21:1033–45. doi: 10.1148/radiographics.21.4.g01jl271033. [DOI] [PubMed] [Google Scholar]
- 4.Wenzl TB. Increased brain cancer risk in physicians with high radiation exposure. Radiology. 2005;235:709–10. doi: 10.1148/radiol.2352041787. [DOI] [PubMed] [Google Scholar]
- 5.USFDA. Initiative to Reduce Unnecessary Radiation Exposure in Patients. February 2010. 2010. [Last accessed on 2015 Mar 25]. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/search.cfm .
- 6.Olgin G, Smith D, Alsyouf M, Arenas JL, Engebretsen S, Huang G, et al. Ureteroscopy without fluoroscopy: A feasibility study and comparison with conventional ureteroscopy. J Endourol. 2015;29:625–9. doi: 10.1089/end.2014.0237. [DOI] [PubMed] [Google Scholar]
- 7.Hsi RS, Harper JD. Fluoroless ureteroscopy: Zero-dose fluoroscopy during ureteroscopic treatment of urinary-tract calculi. J Endourol. 2013;27:432–7. doi: 10.1089/end.2012.0478. [DOI] [PubMed] [Google Scholar]
- 8.Francesca F, Scattoni V, Nava L, Pompa P, Grasso M, Rigatti P. Failures and complications of transurethral ureteroscopy in 297 cases: Conventional rigid instruments vs. small caliber semirigid ureteroscopes. Eur Urol. 1995;28:112–5. doi: 10.1159/000475032. [DOI] [PubMed] [Google Scholar]
- 9.Basiri A, Ziaee SA, Nasseh H, Kamranmanesh M, Masoudy P, Heidary F, et al. Totally ultrasonography-guided percutaneous nephrolithotomy in the flank position. J Endourol. 2008;22:1453–7. doi: 10.1089/end.2007.0391. [DOI] [PubMed] [Google Scholar]
- 10.Jarrard DJ, Gerber GS, Lyon ES. Management of acute ureteral obstruction in pregnancy utilizing ultrasound-guided placement of ureteral stents. Urology. 1993;42:263–7. doi: 10.1016/0090-4295(93)90614-g. [DOI] [PubMed] [Google Scholar]
- 11.Deters LA, Dagrosa LM, Herrick BW, Silas A, Pais VM., Jr Ultrasound guided ureteroscopy for the definitive management of ureteral stones: A randomized, controlled trial. J Urol. 2014;192:1710–3. doi: 10.1016/j.juro.2014.06.073. [DOI] [PubMed] [Google Scholar]
- 12.Peng Y, Xu B, Zhang W, Li L, Liu M, Gao X, et al. Retrograde intrarenal surgery for the treatment of renal stones: Is fluoroscopy-free technique achievable? Urolithiasis. 2015;43:265–70. doi: 10.1007/s00240-015-0760-x. [DOI] [PubMed] [Google Scholar]
- 13.Scarpa RM, De Lisa A, Usai E. Diagnosis and treatment of ureteral calculi during pregnancy with rigid ureteroscopes. J Urol. 1996;155:875–7. [PubMed] [Google Scholar]


