Abstract
Context:
Extracorporeal shockwave lithotripsy (SWL) is the first-line treatment for renal calculi in most cases. Recent technology has allowed lithotriptor machines to localize stones using fluoroscopy or ultrasound (US).
Aim:
The aim of this study is to compare stone free rates (SFR) using two techniques.
Methods:
This is a single center retrospective cohort study. We have studied 95 patients with renal calculi undergoing first SWL treatment with localization using US (48 pts) and fluoroscopy (47 pts). SFR was defined as fragments ≤2 m at 4 weeks post procedure on x-ray or US. Patient records were reviewed.
Results:
Stone size and location, age and body mass index were comparable between groups. Stones ≤7 mm had better SFR with US 86% (18/21) compared to fluoroscopy 59% (10/17) P= 0.08. Overall the US group had similar SFR to the fluoroscopy group for stones of all sizes and locations with 60% (29/48) compared to 45% (21/47)P= 0.18. Radiation exposure was the biggest difference between techniques with a mean radiation dose (mGy/cm2) in the US group of 103 (0–233) and 2113 (241–7821) in the fluoroscopy group. Radiation use in the US group was due to the use of a single shot pre- and post-procedure, this could be reduced to zero.
Conclusions:
Our data show equivalent outcomes using US compared to the traditional fluoroscopy localization technique. We would encourage departments to develop the use of US localization to reduce radiation exposure to patients.
Key Words: Lithotripsy, localization, shockwave lithotripsy, urolithiasis
INTRODUCTION
Extracorporeal shockwave lithotripsy (SWL) has been used to treat for renal calculi since the 1980s and is a well-established first line treatment.[1,2,3] Although little has changed with regards to the energy source and coupling devices, in recent years, advancement in SWL technology has seen the introduction of ultrasound (US) localization of stones. The first lithotriptor machines used fluoroscopy to localize stones and second and third generations have developed technology, which can localize with both fluoroscopy and/or US. This has provided the real-time visualization and assessment of the stone during treatment, which allows adjustment without interrupting the procedure. US is the only way to localize radiolucent stones, which would otherwise require a different treatment modality such as flexible uretorenoscopy and stone lasertripsy. An obvious benefit of US localization is the lack of ionizing radiation to the patient. It is not currently known if the localizing technique used influences stone clearance rates.
There are well-documented features, which influence stone clearance and successful treatment rates with SWL. These include stone size, composition, skin to stone distance, patient tolerance, patient positioning, shock power, and frequency. Anatomical variations affect treatment success including congenital abnormalities. Particularly for lower pole stones, the measurements of infundibular length, width, and infundibulo-pelvic angle have been well-documented as predictive factors of stone-free rates (SFR).[4,5] Good technique in delivering the treatment is crucial to good outcomes, which, of course, is operator dependent.
The evidence comparing the performance of different lithotriptor machines is often poor due to the difficulty in developing randomized control trials. Ordinarily, there will only be one lithotriptor machine for any given region and as such, well-designed trials have not been feasible. There are several nomograms to predict the outcome using first generation machines.[6,7] Nomograms on second and third generation machines are being developed.[8] Studies comparing the three generations of the lithotripter, including a study by Gerber et al., gave mixed results.[9] There are currently no direct comparisons between the different localization techniques.
Widely quoted data come from first generation machines such as the Dornier human model 3, which used fluoroscopy. They give SFRs of 72% for calyceal stones and 78% for renal pelvis stones of 5–10 mm.[7] Initial experience of US localization by Dore in a small cohort retrospective study, found the SFRs were 68.5% using the newer generation machines.[10]
Currently in our department, we have operators of both forms of imaging modalities. The department is a tertiary referral center of nearby local hospitals and serves a population of approximately 800,000. The aim of this study was to quantify the rates of successful lithotripsy treatment in patients who attended our department and to establish whether localization modality was an influencing factor.
METHODS
Patients were identified from our database and received treatments on our Sonolith I-sys Lithotripter (an electro-conductor lithotripter). In our establishment, one operator can perform US and fluoroscopic localization, the other only performs fluoroscopic localization. Both operators have many years experience with SWL.
Two consecutive cohorts of patients receiving initial treatment for renal calculi in our unit on the same lithotripsy machine from 2012 to 2013 were studied. Only the first session of SWL was studied as subsequent treatments did not necessarily use the same localization modality. Pelvi-ureteric junction and ureteric stones were excluded. Patients who did not receive the full treatment were excluded, i.e., insufficient shocks/power. All patients had radiopaque calculi and underwent and X-ray kidney, ureter, and bladder before treatment and at follow-up, 4 weeks after SWL.
The size and location of the target stone were measured. Other measurements include age, body mass index (BMI), radiation dose (mGy/cm2), and complications, which occurred. It was not possible to analyze the composition of the stones or stone fragments. The SFR was defined as no visible fragments ≤2 mm using X-ray or US at 4 weeks. Unsuccessful treatment was defined as any patient requiring further treatment (with SWL or endoscopic treatment) or follow-up for significant residual fragments >2 mm.
RESULTS
For the US group 48 patients were studied and 47 in the fluoroscopy group. Stone size was measured and in the US group average size 8.5 mm (range 4–18 mm) with median size 8 mm. The fluoroscopy group average stone size 9.3 mm (5–16 mm) median stone size 9 mm. Both groups were comparable for average age and BMI. Average age in the US and fluoroscopy groups was 59 and 58 years, respectively. Average BMI was 28 in both groups.
Overall SFR at first SWL session in the US group was 29/48 (60%), which was greater than the fluoroscopy group, 21/47 (45%). This, however, was not statistically significant, P = 0.18, confidence interval 95% using Chi-square test.
Comparing stones ≤7 mm, the US group had greater success than the fluoroscopy group at the first SWL session (SFR 85.7% compared to 58.8%, respectively). The relative risk reduction ratio is three (P = 0.08 using Fisher's exact test) using US compared to fluoroscopy [Tables 1 and 2].
Table 1.
SFR of stones by size and localization modality
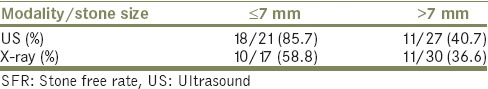
Table 2.
SFR of stones by location and localisation modality
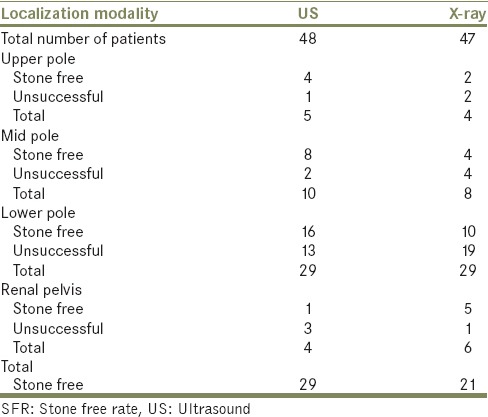
To assess complication rates, the postprocedural hospitalization rates were recorded. There were fewer re-admissions in the US group of four patients, two requiring intervention with ureteric stenting under general or regional anesthesia (Clavien Dindo Grade 3), and two managed conservatively with analgesics (Clavien Dindo Grade 2). The fluoroscopy group had eight re-admissions with three requiring intervention (Clavien Dindo Grade 3), five managed conservatively (Clavien Dindo Grade 2). No patients had serious complications.
Mean radiation dose (mGy/cm2) in the US group was 103 (0–233) and 2113 (241–7821) in the fluoroscopy group.
DISCUSSION
We believe this study to be novel and clinically relevant to the current practice for treatment of renal calculi. Our patient group was similar in demographics of age, sex, and BMI. There were comparable stone sizes in the US and fluoroscopy group with a median stone size of 8 mm and 9 mm, respectively. For current practice, this cohort is comparable with patients in the UK being treating with SWL for renal calculi. Our results have found that US localization for stones ≤7 mm achieved SFR in 85.7% compared to 58.8% using fluoroscopy localization, P = 0.08 (Fisher's exact test). Both groups had similar results for stones >7 mm.
Radiation dose between the groups was significantly higher in the fluoroscopy group as expected. This could potentially be reduced to 0 mGy/cm2 in the US group as single spot images were taken before and after for documentation purposes. Radiation exposure should always be limited due to the emerging risk of cancer associated with radiation used in a healthcare setting. This is, especially important in the group of patients who are recurrent stone formers and will have a cumulative radiation exposure over their lifetime.
The limitations of this study include the inability to assess the stone composition or use a substitute such as Hounsfield units on computed tomography scanning. Factors including the anatomy of the lower pole (infundibular length, width and infundibulopelvic angle) were not measured. BMI was used as a substitute marker for the stone to skin distance, which was not directly measured. High BMI is known to make US less reliable and further study, specifically in obese patients, would have to be done to determine whether this affects stone localization using US and the treatment outcomes.
The limitation with both localization techniques is that they are operator dependent. The operator will program the localization into the lithotriptor, decide on the frequency of adjustments during the procedure and assess the disintegration of a stone. This variability makes a direct comparison between localization techniques difficult. This study has used only one operator for US and two operators who perform fluoroscopic localization to minimize this bias.
CONCLUSIONS
Our data shows equivalence in SFR using US localization compared with traditional fluoroscopy. Coupled with the benefit of no radiation, US is the preferred modality for SWL. We would encourage departments to develop the use of this modality where possible to reduce the radiation exposure to patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Mrs. Angela King, Radiographer, Sunderland Royal Hospital.
REFERENCES
- 1.Miller NL, Lingeman JE. Management of kidney stones. BMJ. 2007;334:468–72. doi: 10.1136/bmj.39113.480185.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wen CC, Nakada SY. Treatment selection and outcomes: Renal calculi. Urol Clin North Am. 2007;34:409–19. doi: 10.1016/j.ucl.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Chaussy C, Brendel W, Schmiedt E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet. 1980;2:1265–8. doi: 10.1016/s0140-6736(80)92335-1. [DOI] [PubMed] [Google Scholar]
- 4.Ruggera L, Beltrami P, Ballario R, Cavalleri S, Cazzoletti L, Artibani W. Impact of anatomical pielocaliceal topography in the treatment of renal lower calyces stones with extracorporeal shock wave lithotripsy. Int J Urol. 2005;12:525–32. doi: 10.1111/j.1442-2042.2005.01101.x. [DOI] [PubMed] [Google Scholar]
- 5.Ghoneim IA, Ziada AM, Elkatib SE. Predictive factors of lower calyceal stone clearance after extracorporeal shockwave lithotripsy (ESWL): A focus on the infundibulopelvic anatomy. Eur Urol. 2005;48:296–302. doi: 10.1016/j.eururo.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Abdel-Khalek M, Sheir KZ, Mokhtar AA, Eraky I, Kenawy M, Bazeed M. Prediction of success rate after extracorporeal shock-wave lithotripsy of renal stones – A multivariate analysis model. Scand J Urol Nephrol. 2004;38:161–7. doi: 10.1080/00365590310022626. [DOI] [PubMed] [Google Scholar]
- 7.Kanao K, Nakashima J, Nakagawa K, Asakura H, Miyajima A, Oya M, et al. Preoperative nomograms for predicting stone-free rate after extracorporeal shock wave lithotripsy. J Urol. 2006;176(4 Pt 1):1453–6. doi: 10.1016/j.juro.2006.06.089. [DOI] [PubMed] [Google Scholar]
- 8.Wiesenthal JD, Ghiculete D, Ray AA, Honey RJ, Pace KT. A clinical nomogram to predict the successful shock wave lithotripsy of renal and ureteral calculi. J Urol. 2011;186:556–62. doi: 10.1016/j.juro.2011.03.109. [DOI] [PubMed] [Google Scholar]
- 9.Gerber R, Studer UE, Danuser H. Is newer always better? A comparative study of 3 lithotriptor generations. J Urol. 2005;173:2013–6. doi: 10.1097/01.ju.0000158042.41319.c4. [DOI] [PubMed] [Google Scholar]
- 10.Dore B, Grange PH, Aubert J. Extracorporeal hydro-electric shockwave lithotripsy (Sonolith 2000).Analysis of 137 records of a first-year experience. Acta Urol Belg. 1989;57:743–54. [PubMed] [Google Scholar]


