Abstract
The tricuspid is the lost valve and the pulmonary being the most anterior, is not visualized well on TEE; The Pulmonary valve is a semilunar valve that separates the right ventricle from the pulmonary artery. It is situated anterior and superior to the aortic valve, almost at right angle to the aortic valve and parallel to the beam of the ultrasound.
Keywords: Transesophageal echocardiography evaluation, Tricuspid and pulmonic valves, Tricuspid regurgitation
TRICUSPID VALVE
Previously considered the forgotten or lost valve, with recognition of the importance of tricuspid repair on outcomes, and the significance of tricuspid regurgitation (TR) on mortality, assessment has assumed greater significance as part of a comprehensive examination. The tricuspid valve (TV) is the largest and the most apically displaced valve. It is located between the right atrium and right ventricle. It has a valve area of 4–6 cm2. The valve is approximately 45° to the sagittal plane or diaphragm so that the margins of the valve are anterosuperior, inferior, or posterior and septal, and the cusps take their name from these attachment sites.[1]
Schematic representation of the heart valves with their spatial relationships and orientation.
The TV complex consists of three leaflets, anterior, posterior, and septal, three papillary muscles with their chordae tendineae, fibrous tricuspid annulus, and the right atrial and right ventricular (RV) myocardium. Valve function depends on the integrity and coordination of these components. The anterior leaflet is the largest, the posterior the second largest and the more inferiorly displaced with multiple scallops, and septal the smallest and the most superiorly placed. The septal leaflet arises medially directly from the tricuspid annulus above the interventricular septum. It is more apically displaced as compared to the mitral anterior leaflet. The anterior papillary muscle provides chordae to the anterior and posterior leaflets, and the posterior papillary muscle provides chordae to the posterior and septal leaflets. The septal wall supplies chordae to the anterior and septal leaflets unless there is a small septal papillary muscle. In addition, there may be accessory chordal attachments to the RV free wall and to the moderator band. The anterior papillary muscle is connected to the septal muscle by the moderator band. All of these multiple chordal attachments are affected by RV dysfunction and dilation, leading to tethering and TR [Figure 1].[2,3]
Figure 1.
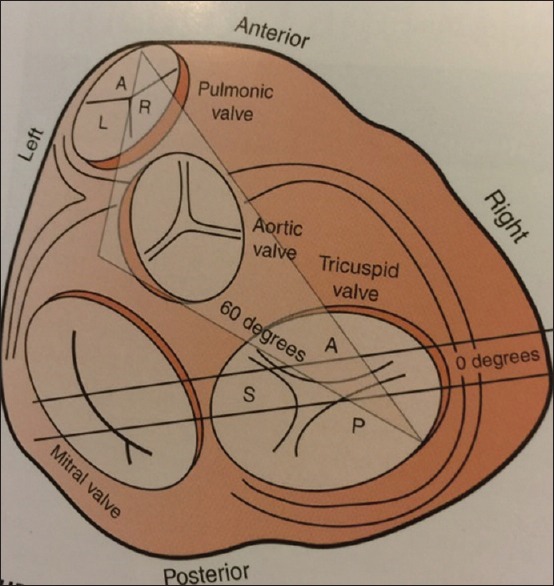
Schematic diagram of the heart that shows the spatial relationships of the valves. Note that the aortic valve plane is almost perpendicular to that of the pulmonic valve, so that when the imaging plane is along the short axis of the aortic valve (imaging at 60°, shaded triangle), the pulmonic valve is imaged in its long axis. When imaging at 0° to obtain the four-chamber view (solid straight lines), anteflexion and retroflexion will move the imaging plane anteriorly and posteriorly to allow imaging of the anterior and posterior leaflets of the tricuspid valve, respectively. (A, anterior;P, posterior; S, septal; L, left; R, right.)
The tricuspid annulus has a complex three-dimensional (3D) structure, with the posterior leaflet being the most inferior and anteroseptal part of the valve being the most superior. This gives it a unique saddle shape which has specific implications for the design and application of the annuloplasty ring.
Tomographic views
The TV can be evaluated in the following tomographic views: Midesophageal four chamber view, midesophageal RV inflow–outflow view, midesophageal modified bicaval view, transgastric short axis view, and transgastric RV inflow view.
TRICUSPID REGURGITATION
Trace or mild TR is frequently a normal finding. It is seen in 65% of the population. Pacemaker wires or catheters passing through the TV commonly cause regurgitation.[4]
Common causes of TR are congenital or acquired. Acquired TR is primary or secondary. It is due to rheumatic heart disease, degenerative disease, or carcinoid. The leaflet structure is characteristic. Rheumatic heart disease can cause thickening and fibrotic restriction of mobility leading to malcoaptation and valvular incompetence. Carcinoid disease causes fibrous deposits and thickening of leaflets with restrictive pathology. The rigid leaflets stay fixed in an open position. Tricuspid prolapse alone is rare and is usually associated with mitral valve myxomatous disease. Flail TV due to ruptured chordae can be the consequence of endocarditis, trauma, or spontaneous rupture. Vegetations on the atrial surface of the leaflets can cause destruction of the leaflets and chordae tendineae. They can also cause leaflet hypermobility from leaflet rupture, prolapsing, or flail leaflet. Right atrial myxoma can interfere with normal leaflet coaptation, leading to regurgitation. Phen-Fen and methysergide can cause thickened, fibrotic, less mobile tricuspid leaflets. These appearances are nonspecific and require historical confirmation of drug use.
Secondary TR is functional and is usually due to left-sided heart failure from myocardial or valvular causes, RV volume and pressure overload, or dilatation of cardiac chambers. RV dysfunction may be secondary to pulmonary hypertension or RV infarction.
Congenital causes are Ebstein's anomaly, where there is atrialization of the RV, septal leaflet descent >8 mm/m2 (separation of mitral and tricuspid annular plane), and TR. Marfan's syndrome causes TR by annular dilatation or leaflet prolapse.
2D assessment includes evaluation of leaflet structure, appearance, and mobility, evaluation of subvalvular apparatus, and the right atrium/right ventricle size. Leaflets are abnormal in rheumatic, degenerative disease, and in carcinoid. In rheumatic TR, there is thickening, shortening, and retraction of the leaflets and subvalvular apparatus. There is usually coexistent rheumatic involvement of the left heart valves. Degenerative TR includes the billowing valve leaflets characterized by thickening on the entire length of the leaflet, a rigid appearance, and motion restriction. Pulmonary hypertension is usually not present, and tricuspid regurgitant jet has low velocity.
Functional TR is the result of tricuspid annular dilatation caused by RV remodeling. The dilation occurs primarily along the mural portion of the tricuspid annulus, above the RV free wall. Rigid or flexible annular bands are used to restore a more normal annular size and ovoid shape thereby reducing or eliminating TR. The echocardiographic appearance of the leaflets is normal. Normal tricuspid annular diameter is 28 ± 5 mm. A diameter >40 mm (21 mm/m2) in the midesophageal four chamber view or in the transgastric RV inflow view is indicative of annular dilatation. Tethering of leaflets from papillary muscle displacement is secondary to RV dilatation. Severe RV hypertension is associated with shift of the interventricular septum toward the left ventricle, resulting in asymmetric tethering. Tethering of leaflets with tenting distance in excess of 8 mm is typically observed in secondary TR. Evaluation of tethering may be performed by measuring systolic tenting area. Tenting area >1 cm2 is associated with severe TR. Interventricular septal flattening may be observed in end diastole (RV volume overload) or in end systole (RV pressure overload). RA and inferior vena cava (IVC) dilatation is commonly observed in chronic TR.
3D assessment of the end systolic frame allows measurement of tenting area and tethering distance that may predict residual TR after repair.
Quantification by color flow Doppler
Visualization of retrograde systolic flow from the right ventricle to right atrium is the first step in diagnosis of TR. Setting the Nyquist limit at 50–60 cm/s, the jet area, vena contracta (VC) is measured. The recent guidelines do not impress upon the jet area as it can be underestimated in eccentric jets and is influenced by right atrial pressure, volume, and color gain settings.
Vena contracta
VC is the narrowest part of the color jet just above the TV. VC >0.7 is seen in severe TR. VC width ≥7 mm has a 90% sensitivity and 93–95% specificity for severe TR.
Proximal isovelocity surface area
The radius of proximal isovelocity surface area (PISA) or flow convergence zone can be used to calculate the severity of TR. With Nyquist limit set to 28 cm/s, a PISA radius >0.9 is suggestive of severe TR. Effective regurgitant orifice area ≥40 mm2 and regurgitant volume ≥45 ml characterize severe TR.
Continuous flow Doppler
Continuous wave Doppler (CWD) interrogation of TR jet assesses severity and estimates RV systolic pressure (RVSP). CWD interrogation should be performed in views where parallel alignment with the regurgitant jet is possible and should be color Doppler-guided. CWD allows a qualitative estimation of TR severity based on shape and density of the signal. The denser the envelope compared to the forward flow, the more severe the TR is. TR severity is also based on the shape of the Doppler envelope. In severe TR, a rapid equalization of right atrial and RV pressure occurs, and the envelope is triangular with an early systolic peak. In severe TR, the continuous wave spectral profile is dense. RVSP is calculated from the peak TR jet. Using the modified Bernoulli equation RVSP = 4 (TR peak velocity2) + RAP (right atrial pressure).
Pulsed wave Doppler
In the absence of tricuspid stenosis (TS) and as seen with mitral regurgitation, a severe TR will increase the protodiastolic flow. An E-wave more than 1 m/s is an indirect marker of severe TR. Pulsed wave Doppler (PWD) is also useful for the assessment of hepatic vein profile (HVP). Given the absence of valves, the hepatic flow depends on the change in RA pressures. With the probe in the transgastrric position, the probe is turned to the right until the liver is seen, then multiplaned so that the hepatic vein is linear. Doppler sample is placed in the right superior hepatic vein 1–2 cm proximal to the junction with the IVC. A typical HVP flow pattern on PWD includes a positive systolic S-wave, a smaller diastolic D-wave, and a short negative A-wave that follows atrial contraction. Systolic flow reversal in the hepatic vein is a specific marker of severe TR; its sensitivity is 80%. With severe TR, there is dilatation of the IVC, lack of respiratory variation, and reversal of systolic S-wave on HVP.
| Parameters for tricuspid severity | Mild | Moderate | Severe |
|---|---|---|---|
| Anatomy of leaflets | Normal | Normal or abnormal | Abnormal, flail, noncoaptation |
| HV/RA/RV size | Normal | Normal or dilated | Dilated |
| Jet area (cm2) | <0.5 | >0.5 | >10 or >30% of right atrial area |
| Vena contracta width (cm) | <0.2 | <0.7 | >0.7 |
| Pisa radius (cm) | 0.5 | 0.6-0.9 | >0.9 |
| TR jet by CWD | Soft parabolic | Dense, variable contour | Dense, triangular, early peak |
| HV flow profile | S>D systolic dominance | S<D | S<0 systolic reversal |
| Tricuspid inflow (cm2) | E>1 | ||
| EROA (ml) | >45 | ||
| Effective regurgitant volume (ml) | >45 |
HV: Hepatic vein, RA: Right atrium, RV: Right ventricle, TR: Tricuspid regurgitation, CWD: Continuous wave Doppler, EROA: Effective regurgitant orifice area
TRICUSPID VALVE STENOSIS
The most common cause of TS is rheumatic, especially in countries where the prevalence is high. It is associated with mitral or aortic valve involvement. Other rare causes of TS include carcinoid disease, endocarditis, endomyocardial fibrosis, lupus erythematous, right atrial myxoma, and congenital tricuspid atresia. Carcinoid valve lesions characteristically manifest as fibrous white plaques located on the valvular and mural endocardium. The valve leaflets are thickened, rigid, and reduced in area. Fibrous tissue proliferation is present on the atrial and ventricular surfaces of the valve structure. TS is mild, but the TR is moderate to severe.
2D echocardiography features are thickened and echo-dense leaflets with or without characteristic diastolic doming. In endocarditis, destruction of leaflets may cause flailing into the atrium. Mass from vegetation or tumor can cause obstruction. The right atrium and IVC are enlarged.
Color flow Doppler
Proximal flow convergence is seen on the atrial side of TV.
Doppler echocardiography normally flows velocities through this largest valve are <0.7 m/s. Velocities >1.5 m/s with transvalvular gradient >7 mmHg are suggestive of TS.
| Parameters of severity | Mild | Moderate | Severe |
|---|---|---|---|
| Two-dimensional echo leaflets | Normal | Thickened | Thickened and calcified |
| Leaflet mobility | Normal | Moderately restricted | Severe and doming |
| RA | Normal | Dilated | Severely dilated |
| TV inflow velocity (m/s) | <0.7 | >0.7 | >1.5 |
| PHT (m/s) | 190 | ||
| Pressure | <2 | 2-6 | >7 |
| gradient (mmHg) |
RA: Right atrium, TV: Tomographic view, PHT: Pressure half-time
PULMONARY VALVE DISEASE
The pulmonary valve is a semilunar valve that separates the right ventricle from the pulmonary artery. It is situated anterior and superior to the aortic valve, almost at right angle to the aortic valve and parallel to the beam of the ultrasound. The three cusps are anterior, left, and right. The cusps of the pulmonic valve are thinner and defined by their relationship to the aortic valve and are thus termed anterior or nonseptal, right and left cusps. Each of the cusps has a fibrous node at the midpoint of the free edges (similar to the nodes of Aranti in the aortic valve) as well as lunulae, which are the thin, crescent-shaped portions of the cusps that serve as the coaptive surfaces of the valve. In contrast with the aortic valve, the cusps of the pulmonic valve are supported by freestanding musculature with no direct relationship with the muscular septum; its cusps are much thinner and lack any fibrous continuity with the anterior leaflet of the TV.[5,6]
The cusps of the pulmonic valve are defined by their relationship to the aortic valve and are thus termed anterior, right and left cusps. They can also be defined by their relationship to a commissure found in the pulmonic and aortic valves and hence termed right adjacent (right facing), left adjacent (left facing), and opposite (nonfacing). The pulmonic valve, like the other three cardiac valves, is formed by endocardial folds that are supported by internal plates of dense collagenous and elastic connective tissue and are continuous with the cardiac skeleton.
Tomographic views
Midesophageal RV inflow-outflow view, midesophageal aortic valve short axis view, transgastric RV outflow view, UE ascending aorta SAX view, transgastric RV inflow–outflow view, and deep transgastric RV outflow view. From the TG two-chamber view (transducer angle of 90 to 110) turning to the right (clockwise) will result in the TG RV inflow (or RV two-chamber) view. The anterior and inferior walls of the right ventricle are imaged in addition to the papillary muscles, chordae, and TV. The proximal RVOT is also frequently seen, and slight advancement of probe may allow imaging and Doppler interrogation of PV.
Pulmonary regurgitation
Common causes include pulmonary hypertension leading to dilatation of pulmonary artery. Less common causes are Marfan's syndrome, carcinoid from restricted leaflets, endocarditis, and congenital pulmonary stenosis where surgical intervention might have occurred.
2D echocardiography reveals thickened, restricted leaflets, annular dilatation, vegetations, prolapse, and lack of coaptation.
Doppler interrogation helps with a qualitative assessment of regurgitant jet width, length, and ratio of jet width to pulmonary artery diameter. CWD of end diastolic flow velocity helps to estimate the end-diastolic gradient using the Bernoulli equation. This estimates the pulmonary artery diastolic pressure. The slope of the regurgitant jet can be used to assess severity. A pressure half-time <100 m/s may indicate severe pulmonary insufficiency.
| Parameters for Two-dimensional echo | Mild | Moderate | Severe |
|---|---|---|---|
| Leaflets | Normal | May be abnormal | Abnormal |
| RA/RV/pulmonary annulus | Normal | May be dilated | Dilated |
| Jet length by CWD (mm) | <10 | 10-20 | >20 |
| Ratio of jet width/RVOT diameter (%) | <34 | 35-74 | >75 |
| CWD signal | Soft with slow acceleration | Dense and variable | Dense, steep deceleration (PHT <100 m/s) |
RA: Right atrium, RV: Right ventricle, CWD: Continuous wave Doppler, RVOT: Right ventricular outflow tract, PHT: Pressure half-time
Pulmonary stenosis
Congenital causes are most common. Other causes are rheumatic or carcinoid disease and RV outflow tract obstruction from infundibular hypertrophy and aneurysmal membranous ventricular septum. RV hypertrophy is seen.
2D Echo - Thickened calcified leaflets with systolic doming
Spectral Doppler - Color flow Doppler reveals aliasing. CWD reveals a late-peaking dagger-shaped envelope in the RV outflow tract. Peak gradient across the valve of >36 mmHg is evidence of moderate stenosis.
| Parameters of severity | Mild | Moderate | Severe |
|---|---|---|---|
| Two-dimensional leaflet | Normal | Thickened and moderate restriction | Thickened, calcified, severe restriction |
| RV | Normal | Mild hypertrophy | Moderate hypertrophy |
| CWD peak velocity (m/s) | <3 | 3-4 | >4 |
| Peak gradient (mmHg) | <36 | >36 | >64 |
CWD: Continuous wave Doppler, RV: Right ventricle
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
TAKE HOME MESSAGES
In this review the author discusses the echocardiography of the forgotten valve – the tricuspid and the pulmonary. The significance of tricuspid regurgitation during comprehensive TEE examination is emphasised in terms of vena contracta, PISA, CWD, PWD and how hepatic vein profile assesses the right atrial pressure. Details on tricuspid stenosis, pulmonary regurgitation and pulmonary stenosis are touched upon.
REFERENCES
- 1.Feigenbaum H, Armstrong WF, Ryan T. In: Tricuspid valve. Feigenbaum's Echocardiography. 6th ed. Feigenbaum H, Armstrong WF, Ryan T, editors. Philadelphia, USA: Lippincott Williams and Wilkins; 2005. pp. 364–9. [Google Scholar]
- 2.Hahn RT, Abrahim T, Adams M, Bruce CJ, Glas KE, Lang RM, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: Recommendations from the American society of echocardiography and the society of cardiovascular anesthesiologists. J Am Soc Echocardiogr. 2013;26:921–64. doi: 10.1016/j.echo.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Mathew J, Swaminathan M, Ayoub C. Tricuspid and pulmonic valves. Clinical Manual and Review of Transesophageal Echocardiography. 2nd ed. United States: McGraw-Hill Professional Publishing; 2011. [Google Scholar]
- 4.Rogers JH, Bolling SF. The tricuspid valve: Current perspective and evolving management of tricuspid regurgitation. Circulation. 2009;119:2718–25. doi: 10.1161/CIRCULATIONAHA.108.842773. [DOI] [PubMed] [Google Scholar]
- 5.Tricuspid and Pulmonic Valves. Society of Cardiovascular Anesthesiologists. [Last accessed on 2016 Sep 01]. Available from: http://www.sca.org .
- 6.Muralidhar K, Tempe D, Chakravarthy M, Shastry N, Kapoor PM, Tewari P, et al. Practice guidelines for perioperative transesophageal echocardiography: Recommendations of the Indian association of cardiovascular thoracic anesthesiologists. Ann Card Anaesth. 2013;16:268–78. doi: 10.4103/0971-9784.119175. [DOI] [PubMed] [Google Scholar]


