Abstract
Purpose of review:
While the distinctive motor symptoms of Parkinson disease (PD) have been described for centuries, cognitive impairment has only recently been recognized as a central feature. Studies have yielded clues to the etiology and natural history of cognitive impairment in PD, but much remains unclear and effective therapies are needed.
Recent findings:
Longitudinal cohort studies demonstrate that almost all patients with PD will develop dementia if they live long enough. New CSF biomarker and genetic studies suggest that it may soon be possible to forecast and track the progression of dementia in PD. Sleep and sleep disturbance appear to be intrinsically linked with PD, although the implications for individual outcomes and opportunities for intervention are unclear. Multidisciplinary treatment approaches incorporating cognitive training may help to improve outcomes.
Summary:
We review several recent advances in understanding the pathophysiology, genetics, and management of cognitive impairment in PD.
Cognitive impairment is a disabling comorbidity for many patients with Parkinson disease (PD) and represents a major challenge for physicians, caregivers, and the health care system.
Prevalence and natural history of PD dementia: Near-universal prevalence and progression
Clinical features of cognitive impairment in PD involve a wide range of cognitive domains, including executive function, visuospatial reasoning, memory, and language function, and can include additional features including visual hallucinations, paranoia, and fluctuations in attention.1 PD is often marked primarily by visuospatial and executive deficits, in contrast to Alzheimer disease (AD), where memory impairment predominates. Cognitive impairment in PD encompasses a spectrum of severity from relatively mild symptoms to end-stage dementia. Despite the controversy surrounding the nomenclature and clinical significance of the term mild cognitive impairment (MCI), careful characterization of early symptoms is needed for both research and clinical purposes, and formal criteria for diagnosis of MCI in PD have been established.2
Overall prevalence of PD-associated dementia (PDD) is approximately 25%–30% of total PD cases, and increases dramatically with advancing age.3 While some patients with PD survive a decade or more before developing dementia, others experience cognitive impairment shortly after, or concurrent with the onset of motor symptoms, leading to the arbitrary distinction of patients who develop dementia within 1 year of parkinsonism as having dementia with Lewy bodies (DLB).4
The Sydney Multicenter Study, the longest PD cohort study to date, found that 83% of patients who survived 20 years developed dementia.5 This and other studies, including a large retrospective study of Medicare beneficiaries,3 demonstrate that patients with PD are almost universally at risk of dementia if they survive long enough. Studies are mixed when assessing the individual contributions of age, age at onset of PD, and disease duration to the risk of dementia. These mixed findings make it difficult to draw conclusions regarding the importance of factors other than the chronic accumulation of PD pathology on the development of dementia.6,7
A recent study followed 141 patients with PD with normal cognition at baseline over a period of 2–6 years, finding that nearly half of participants developed cognitive impairment within 5 years, and that 100% of individuals who developed MCI progressed to dementia within 5 years.8 Consistent with other recent studies, predictors of progression from normal cognition to cognitive impairment included male sex, higher Unified Parkinson's Disease Rating Scale motor score, and lower (poorer) baseline cognitive scores. Although comparisons of rate of cognitive decline across diseases are challenging, we note for reference that in cognitively normal patients with CSF biomarker evidence of preclinical AD, the 5-year progression rate to Clinical Dementia Rating 0.5 (very mild dementia) was between 11% and 26%.9 Further work is needed to address the relative relationships of PD-specific pathology vs other age-related neuropathology on the development of dementia in patients with PD. For example, nearly 60% of patients with PD with dementia have concurrent cortical Aβ pathology.10 Nevertheless, these data emphasize that patients with PD progress quickly from normal cognition through stages of cognitive impairment, including dementia, and that dementia in PD contributes to greater public health burden than previously recognized.
Biomarkers: An ongoing quest for molecular fingerprints
PD remains a clinical diagnosis, with only one commercially available biomarker ([123I]-ioflupane, a dopamine transporter radioligand) approved to distinguish PD from essential tremor, although the value of this biomarker compared to longitudinal follow-up with a movement disorders specialist is unclear.11 Neurologists, even experienced movement disorders specialists, are frequently inaccurate in distinguishing idiopathic PD from other parkinsonian syndromes, especially early in the disease course. Predicting the risk and timing of dementia in patients with PD is equally challenging and is complicated by the heterogeneity of molecular neuropathology observed in PDD cases when autopsy examination is used as a gold standard. While multiple studies support a direct relationship between the presence of cortical Lewy pathology and cognitive impairment,12 some patients with PDD have very few cortical Lewy bodies.12,13 Conversely, extensive cortical Lewy pathology is occasionally seen in cognitively normal patients with PD and even individuals without PD.12,14 These observations suggest that α-synuclein (αSyn) is not solely responsible for cognitive impairment in PD. Multiple studies have documented the presence of concomitant β-amyloid (Aβ) in approximately 60% of patients with PD with dementia, as well as tau pathology in a smaller subset,10 underscoring the need for accurate biomarkers to define molecular disease signatures prior to autopsy, ideally in presymptomatic or early symptomatic phases.
Several recent studies report associations between CSF biomarkers and risk of cognitive decline in PD. In approximately 300 participants from the Deprenyl and Tocopherol Antioxidative Therapy of Parkinsonism (DATATOP) study, investigators found that higher CSF αSyn levels predicted worse cognitive performance at follow-up, despite average length to follow-up of only 1.8 years.15 Another DATATOP study found that CSF levels of phospho-tau and phospho-tau/Aβ42 ratio predicted decline in cognitive tasks over approximately 4 years.16 Notably, this was the first study to show an association with CSF tau and progression of cognitive impairment in PD, building on previous reports documenting higher CSF tau levels in patients with PDD than in patients with PD without dementia and controls. Another smaller prospective study found that lower CSF Aβ 1–42 (Aβ42) and higher αSyn levels at baseline predicted cognitive decline over 2 years.17 In this study, higher baseline levels of CSF phospho-tau were associated with worsening of motor but not cognitive symptoms.
Although these findings demonstrate the potential value of CSF biomarkers for cognitive impairment in PD, there are several caveats. First, the duration of follow-up was relatively short, compared to the timeframe over which many patients with PD develop dementia, so the generalizability to the full spectrum of cognitive decline in PD is unclear. As such, these biomarkers may better reflect accelerated cognitive decline and could potentially be useful for prognostication in cases of rapid cognitive decline. Most studies have been based on clinical diagnoses and not neuropathologic criteria, which has been shown repeatedly to be the gold standard for diagnosis of neurodegenerative disease. While CSF data have the advantage of an objective molecular marker, future studies will hopefully be combined with pathology, and especially pathologic burden, to further increase our understanding of the molecular signatures of PD and PDD.
Genetics: Renewed importance of APOE; GBA variants and potential role of lysosomal dysfunction
Given the overlap in clinical symptoms and neuropathologic features among PDD, AD, and DLB, genetic association studies represent a powerful tool to identify areas of potential divergence in molecular mechanism and to highlight shared genetic risk factors that may represent common neurodegenerative pathways. A recent multicenter study of neuropathologically confirmed DLB cases reported 3 genetic loci with significant associations with the DLB phenotype, corresponding to the genes for APOE (odds ratio [OR] 2.786, 95% confidence interval [CI] 2.397–3.239), αSyn (SNCA; OR 0.754, 95% CI 0.6725–0.8468), and SCARB2 (OR 0.749, 95% CI 0.658–0.854), a lysosomal protein previously linked to PD. Another study found that the APOE ε4 allele associated with DLB regardless of the presence of Aβ pathology, suggesting that APOE may have an Aβ-independent effect on DLB and PDD pathogenesis.18 The importance of APOE was further underscored by the finding that the APOE ε4 variant was associated with poorer cognitive performance in a study of more than 1,000 patients with PD across multiple centers.19 Interestingly, the authors noted that the MAPT H1 haplotype, while associated with overall PD risk, did not predict cognitive performance in this dataset. Other recent studies have been mixed with respect to association of the MAPT H1 haplotype and rate of cognitive decline in PD.20,21
Evidence continues to point towards a role of GBA, the gene that encodes glucocerebrosidase, in the pathogenesis of PD and PDD. Loss of function mutations in GBA cause Gaucher disease, a recessive lysosomal storage disorder, and mounting data indicate that carriers of GBA mutations are at higher risk of dementia, in addition to the well-recognized increased risk of PD.22 A recent study found that mutations, as well as a common polymorphism in GBA, were associated with deficits in executive and visuospatial function in patients with PD.23 When considered in the context of a recent study that demonstrated that glucocerebrosidase activity was lower in GBA mutation carriers and that lower glucocerebrosidase activity correlated with shorter disease duration in patients with PD (i.e., more rapid progression),24 these studies strongly implicate GBA in the neurodegenerative cascade leading to dementia in PD, and underscore the need for further work to determine precisely how GBA may interact with other disease-relevant molecules to modulate neurodegeneration, possibly via changes in lysosomal biology. Ultimately, genetic screening may be clinically useful in PDD to guide the selection of disease-modifying treatments based on knowledge of an underlying pathophysiologic mechanism.
Sleep
Sleep disturbance is almost universal in PD, markedly more frequent than in the general population,25,26 with patients manifesting a range of symptoms including sleep fragmentation, excessive daytime sleepiness, and REM behavior disorder. In addition to the detrimental effects on cognitive function associated with poor sleep, growing evidence supports a proximate role for sleep disturbance in the pathophysiology of dementia. A recent meta-analysis compiled data from 16 studies that addressed sleep disturbance and cognitive function in patients with PD using objective measures including polysomnography or validated sleep questionnaires and neuropsychological testing to assess cognitive function.27 Despite methodologic variability between studies, the authors calculated that patients with PD with poor sleep performed more poorly on tests of global cognitive ability and multiple subdomains of executive function (shifting, updating, generativity, and fluid reasoning) compared to those without sleep problems.
REM behavior disorder (RBD) is recognized as a risk factor for PD, and a recent study found that RBD predicted development of dementia in a prospective study of 80 patients with PD followed over 4 years with an OR of 49.7 (95% CI 7.4–333).28 Using a novel high-sensitivity visual short-term memory task, another recent study showed that patients with RBD have the same characteristic visual memory deficit as patients with PD.29 Interestingly, the authors noted that patients with PD made one specific type of error on this task, while carriers of mutations in glucocerebrosidase (GBA), a genetic risk factor for PD, made a separate type of error on the same task. These data, along with the finding that patients with idiopathic RBD have αSyn pathology, suggest that individuals with RBD may share a specific underlying pathology with patients with PD, even prior to the development of PD symptoms, emphasizing the possibility that RBD is an attractive target phenotype for identifying individuals at risk of developing PDD and perhaps as candidates for clinical trials.
Further work is needed to address whether sleep disturbance affects aspects of cognition in PD differently than in other neurodegenerative disorders or in the general population, and whether targeted therapies can improve sleep and cognition in PD. Perhaps the most fundamental issue is to distinguish to what extent the cognitive impairment in patients with PD with sleep disorders is simply a symptom of the sleep deprivation itself, whether the underlying sleep disorder actually contributes to dementia pathology, or whether the neurodegeneration causes the sleep pathology.
Cognitive training
Effective therapies for cognitive impairment represent a critical unmet need in PD therapeutics. In a recent retrospective study utilizing Medicare data from nearly 500,000 patients with PD, dementia was the strongest predictor of nursing home placement.30 Given the societal costs of caring for patients with dementia, any intervention that improves cognition has the potential for meaningful benefit in terms of reducing cost of care and improving quality of life. Cognitive training is broadly defined to include “structured and theoretically driven teaching of strategies or guided practice on tasks that target particular cognitive domains.”31 Indeed, a multidisciplinary rehabilitation program for patients with PD that incorporated cognitive-behavioral therapy was superior when compared to general physiotherapy alone with respect to motor scores, activities of daily living, and cognition.32
One intriguing study that bridges 2 important areas in PD examined the effect of sleep on cognitive task learning. In this study, digit span backward testing (a measure of working memory) improved following a period of nocturnal sleep, but only in patients with PD taking dopaminergic medication.33 This finding has several important implications. First, working memory was once thought not to respond to training, but this and other recent studies indicate that working memory can be improved with targeted intervention in patients with PD. Second, these data suggest that sleep plays a pivotal role in cognitive function and training in PD, and that cognitive training may be more effective in patients who get sufficient quantity and quality of sleep. Finally, the divergence in working memory outcomes between medicated and nonmedicated patients with PD indicates a specific role for dopaminergic neurotransmission in sleep-dependent improvements in cognitive function. Interestingly, the authors noted that they did not observe a similar improvement in patients diagnosed with DLB, although this may be a reflection of many factors, including worse baseline cognitive scores in the DLB group, rather than a difference in underlying neurobiology.
While cognitive training has been employed for both cognitive and gait symptoms, including in PD, the clinical benefits of this approach have only recently been studied systematically. A meta-analysis of several recent studies found that cognitive training had small but significant effects on multiple domains of cognitive function often impaired in PD, including executive function, processing speed, working memory, and overall cognitive performance.31 There was substantial variability in the design, implementation, and evaluation of the trials included in this analysis, and further work will be needed to refine the optimal patient and symptom targets as well as the mode, frequency, and duration of implementation. Patients and caregivers should understand that cognitive training has not yet been proven to translate into clinically meaningful improvements in patient or caregiver quality of life. Nevertheless, these early studies demonstrate that cognitive training has a promising role in the multidisciplinary approach to treating cognitive impairment in PD. Ideally, cognitive training would be implemented in at-risk patients with PD at early stages of cognitive impairment, with the goal of preserving remaining cognitive function and maximizing adaptive compensation to enable patients to continue to work or live independently. Properly designed cost-effectiveness studies will be needed to justify additional health care expenditures required for widespread coverage by government or private payers.
PD and cognitive impairment: Five new things
Longitudinal studies show that the risk of dementia in PD increases with advancing age and that nearly all patients with PD develop dementia if they survive 20 years with the disease.
CSF biomarkers are beginning to define molecular signatures that may help to stratify risk of dementia in PD and track disease progression.
Genetic association studies have revealed links to other neurodegenerative diseases and implicate lysosomal dysfunction in the pathophysiology of PD dementia.
Sleep disturbance appears to exacerbate cognitive impairment in PD; in particular, REM behavior disorder shares an overlapping pattern of cognitive impairment with PD and increases the risk of dementia.
Cognitive training may help improve outcomes when incorporated in a multidisciplinary therapy program.
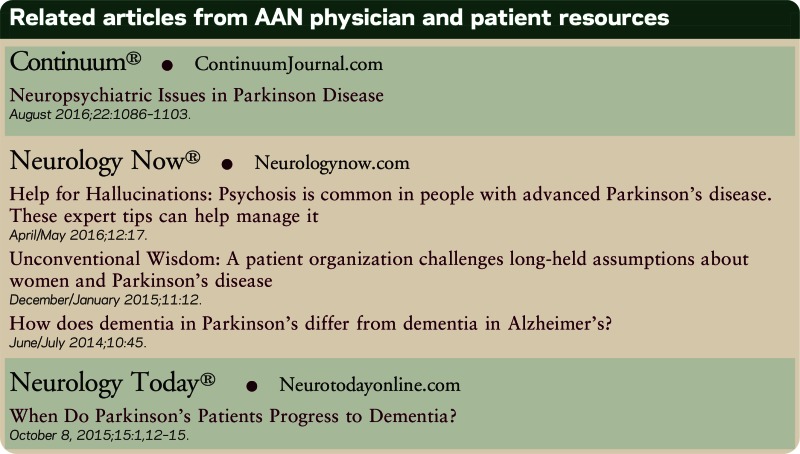
Related articles from AAN physician and patient resources
Continuum®
Neuropsychiatric Issues in Parkinson Disease
Neurology Now®
Help for Hallucinations: Psychosis is common in people with advanced Parkinson's disease. These expert tips can help manage it
Unconventional Wisdom: A patient organization challenges long-held assumptions about women and Parkinson's disease
How does dementia in Parkinson's differ from dementia in Alzheimer's?
Neurology Today®
When Do Parkinson's Patients Progress to Dementia?
AUTHOR CONTRIBUTIONS
A.A. Davis and B. Racette conducted the literature review and wrote the paper.
STUDY FUNDING
This study was supported in part by the following grants: American Academy of Neurology/American Brain Foundation Clinical Research Training Fellowship (A.A.D.), the BrightFocus Foundation (A.A.D.), K24 ES017765 (B.R.), R01ES021488 (B.R.), R01ES021488-02S1 (B.R.), R01ES025991 (B.R.), Michael J. Fox Foundation (B.R.).
DISCLOSURES
A.A. Davis received research support from the American Academy of Neurology/American Brain Foundation and the BrightFocus Foundation. B. Racette receives research support from Teva, Adamas Pharmaceuticals, Auspex Pharmaceuticals, Eisai, Allergan, Merz Pharmaceuticals GmbH, Pfizer, Civitas Therapeutics, Kyowa Hakko Kinn Pharma, AbbVie, American Parkinson Disease Association, the Michael J. Fox Foundation, and NIH; and has served as a consultant in medico-legal proceedings. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Williams-Gray CH, Evans JR, Goris A, et al. The distinct cognitive syndromes of Parkinson's disease: 5 year follow-up of the CamPaIGN cohort. Brain 2009;132:2958–2969. [DOI] [PubMed] [Google Scholar]
- 2.Litvan I, Goldman JG, Troster AI, et al. Diagnostic criteria for mild cognitive impairment in Parkinson's disease: Movement Disorder Society Task Force guidelines. Mov Disord 2012;27:349–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Willis AW, Schootman M, Kung N, Evanoff BA, Perlmutter JS, Racette BA. Predictors of survival in patients with Parkinson disease. Arch Neurol 2012;69:601–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McKeith IG, Galasko D, Kosaka K, et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the Consortium on DLB International Workshop. Neurology 1996;47:1113–1124. [DOI] [PubMed] [Google Scholar]
- 5.Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG. The Sydney Multicenter Study of Parkinson's Disease: the inevitability of dementia at 20 years. Mov Disord 2008;23:837–844. [DOI] [PubMed] [Google Scholar]
- 6.Hughes TA, Ross HF, Musa S, et al. A 10-year study of the incidence of and factors predicting dementia in Parkinson's disease. Neurology 2000;54:1596–1602. [DOI] [PubMed] [Google Scholar]
- 7.Zhu K, van Hilten JJ, Marinus J. Predictors of dementia in Parkinson's disease; findings from a 5-year prospective study using the SCOPA-COG. Parkinsonism Relat Disord 2014;20:980–985. [DOI] [PubMed] [Google Scholar]
- 8.Pigott K, Rick J, Xie SX, et al. Longitudinal study of normal cognition in Parkinson disease. Neurology 2015;85:1276–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vos SJ, Xiong C, Visser PJ, et al. Preclinical Alzheimer's disease and its outcome: a longitudinal cohort study. Lancet Neurol 2013;12:957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotzbauer PT, Cairns NJ, Campbell MC, et al. Pathologic accumulation of alpha-synuclein and Abeta in Parkinson disease patients with dementia. Arch Neurol 2012;69:1326–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perlmutter JS, Eidelberg D. To scan or not to scan: DaT is the question. Neurology 2012;78:688–689. [DOI] [PubMed] [Google Scholar]
- 12.Braak H, Rub U, Jansen Steur EN, Del Tredici K, de Vos RA. Cognitive status correlates with neuropathologic stage in Parkinson disease. Neurology 2005;64:1404–1410. [DOI] [PubMed] [Google Scholar]
- 13.Galvin JE, Pollack J, Morris JC. Clinical phenotype of Parkinson disease dementia. Neurology 2006;67:1605–1611. [DOI] [PubMed] [Google Scholar]
- 14.Hurtig HI, Trojanowski JQ, Galvin J, et al. Alpha-synuclein cortical Lewy bodies correlate with dementia in Parkinson's disease. Neurology 2000;54:1916–1921. [DOI] [PubMed] [Google Scholar]
- 15.Stewart T, Liu C, Ginghina C, et al. Cerebrospinal fluid alpha-synuclein predicts cognitive decline in Parkinson disease progression in the DATATOP cohort. Am J Pathol 2014;184:966–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu C, Cholerton B, Shi M, et al. CSF tau and tau/Abeta42 predict cognitive decline in Parkinson's disease. Parkinsonism Relat Disord 2015;21:271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall S, Surova Y, Ohrfelt A, Zetterberg H, Lindqvist D, Hansson O. CSF biomarkers and clinical progression of Parkinson disease. Neurology 2015;84:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsuang D, Leverenz JB, Lopez OL, et al. APOE epsilon4 increases risk for dementia in pure synucleinopathies. JAMA Neurol 2013;70:223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mata IF, Leverenz JB, Weintraub D, et al. APOE, MAPT, and SNCA genes and cognitive performance in Parkinson disease. JAMA Neurol 2014;71:1405–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morley JF, Xie SX, Hurtig HI, et al. Genetic influences on cognitive decline in Parkinson's disease. Mov Disord 2012;27:512–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nombela C, Rowe JB, Winder-Rhodes SE, et al. Genetic impact on cognition and brain function in newly diagnosed Parkinson's disease: ICICLE-PD study. Brain 2014;137:2743–2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alcalay RN, Caccappolo E, Mejia-Santana H, et al. Cognitive performance of GBA mutation carriers with early-onset PD: the CORE-PD study. Neurology 2012;78:1434–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mata IF, Leverenz JB, Weintraub D, et al. GBA variants are associated with a distinct pattern of cognitive deficits in Parkinson's disease. Mov Disord 2016;31:95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alcalay RN, Levy OA, Waters CC, et al. Glucocerebrosidase activity in Parkinson's disease with and without GBA mutations. Brain 2015;138:2648–2658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Larsen JP, Tandberg E. Sleep disorders in patients with Parkinson's disease: epidemiology and management. CNS Drugs 2001;15:267–275. [DOI] [PubMed] [Google Scholar]
- 26.Tandberg E, Larsen JP, Karlsen K. A community-based study of sleep disorders in patients with Parkinson's disease. Mov Disord 1998;13:895–899. [DOI] [PubMed] [Google Scholar]
- 27.Pushpanathan ME, Loftus AM, Thomas MG, Gasson N, Bucks RS. The relationship between sleep and cognition in Parkinson's disease: a meta- analysis. Sleep Med Rev 2015;26:21–32. [DOI] [PubMed] [Google Scholar]
- 28.Anang JB, Gagnon JF, Bertrand JA, et al. Predictors of dementia in Parkinson disease: a prospective cohort study. Neurology 2014;83:1253–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rolinski M, Zokaei N, Baig F, et al. Visual short-term memory deficits in REM sleep behaviour disorder mirror those in Parkinson's disease. Brain 2016;139:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Safarpour D, Thibault DP, DeSanto CL, et al. Nursing home and end-of- life care in Parkinson disease. Neurology 2015;85:413–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leung IH, Walton CC, Hallock H, Lewis SJ, Valenzuela M, Lampit A. Cognitive training in Parkinson disease: a systematic review and meta-analysis. Neurology 2015;85:1843–1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Monticone M, Ambrosini E, Laurini A, Rocca B, Foti C. In-patient multidisciplinary rehabilitation for Parkinson's disease: a randomized controlled trial. Mov Disord 2015;30:1050–1058. [DOI] [PubMed] [Google Scholar]
- 33.Scullin MK, Trotti LM, Wilson AG, Greer SA, Bliwise DL. Nocturnal sleep enhances working memory training in Parkinson's disease but not Lewy body dementia. Brain 2012;135:2789–2797. [DOI] [PMC free article] [PubMed] [Google Scholar]


