Abstract
Background
Although pediatric growth charts are recommended for weight assessment prior to age 20, many teenagers transition earlier to adult care where absolute BMI is used. This study examines concordance of weight classification in older teenagers using pediatric percentiles and adult thresholds.
Methods
BMI from 23,640 U.S. teens ages 18–19 years were classified using pediatric BMI percentile criteria for underweight (<5th), normal (5th to <85th), overweight (85th to <95th), obesity (≥95th) and severe obesity (≥120%×95th percentile) and adult BMI (kg/m2) criteria for underweight (<18.5), normal (18.5–24.9), overweight (25–29.9) and obesity: class I (30–34.9), class II (35–39.9) and class III (≥40). Concordance was examined using the Kappa statistic. Blood pressure (BP) from the same visit was classified hypertensive for BP≥140/90.
Results
The majority of visits (72.8%) occurred in adult primary care. Using pediatric/adult criteria, 3.4%/5.2% were underweight, 66.6%/58.8% normal weight, 15.7%/21.7% overweight, 14.3%/14.3% obese and 4.9%/6.0% severely/Class II–III obese, respectively. Pediatric and adult classification for underweight, normal, overweight and obesity were concordant for 90.3% (weighted Kappa 0.87 [95% confidence interval, 0.87–0.88]). For severe obesity, BMI≥120%×95th percentile showed high agreement with BMI≥35 kg/m2 (Kappa 0.89 [0.88–0.91]). Normal weight males and moderately obese females by pediatric BMI percentile criteria who were discordantly classified into higher adult weight strata had a greater proportion with hypertensive BP compared to concordantly classified counterparts.
Conclusions
Strong agreement exists between U.S. pediatric BMI percentile and adult BMI classification for older teenagers. Adult BMI classification may optimize BMI tracking and risk stratification during transition from pediatric to adult care.
Keywords: obesity, severe obesity, body mass index, adolescence, young adult
INTRODUCTION
Given the high prevalence of pediatric obesity in the United States (affecting roughly 17% of children ages 2–19 years)1, 2 and the rising prevalence of severe pediatric obesity,3, 4 increasing attention has focused on body mass index (BMI) trajectories during childhood, late adolescence and subsequent adult BMI. Adolescence has been described as an important period in the development and persistence of obesity due to a multitude of both intrinsic and extrinsic factors, such as behavioral, physiological and psychosocial changes that modulate obesity risk.5 More than 50% of obese adolescents will continue to be obese as adults,6, 7 emphasizing the importance of weight classification and tracking during the transition to adulthood.
For U.S. children and adolescents, classification of BMI is based on age-and sex-specific BMI percentiles according to the Centers for Disease Control and Prevention (CDC) growth charts where overweight is defined by BMI 85th to <95th percentile and obesity by BMI ≥95th percentile.8–10 Among adolescents, the adult criterion of BMI ≥30 kg/m2 also defines obesity even if the value is lower than the 95th BMI percentile.10 New consensus recommendations also define the threshold for severe pediatric obesity as BMI ≥120% of the 95% BMI percentile or BMI ≥35 kg/m2, whichever is lower.11 Transition to adult BMI classification occurs at age 20 years,12, 13 shifting from age- and sex-specific BMI percentiles13 to discrete BMI categories independent of age and sex. According to the World Health Organization (WHO)14 and National Heart, Lung, and Blood Institute (NHLBI)15 criteria for adults, overweight is defined by BMI 25.0–29.9 kg/m2, obesity by BMI ≥30 kg/m2, and higher order obesity classes I, II, and III by BMI 30–34.9 kg/m2, 35–39.9 kg/m2 and ≥40 kg/m2, respectively.
Multiple approaches also exist internationally for evaluating pediatric overweight and obesity, with varying definitions and age cut-offs.10, 16–18 The International Obesity Task Force provides age- and sex-specific BMI centile curves that correspond to a BMI of 25 kg/m2 and 30 kg/m2 at age 18 years17, 19 and the 2007 WHO pediatric growth reference curves achieve these same BMI levels (25 kg/m2 and 30 kg/m2) at age 19 years for +1 and +2 standard deviations16, respectively. When using the year 2000 CDC growth charts,8 the 85th BMI percentile curves cross a BMI threshold of 25 kg/m2 at an earlier age of 16½-17 years, whereas the 95th BMI percentile curves cross a BMI of 30 kg/m2 at age 17½ and 19½ years for females and males, respectively. Although CDC recommendations for adult weight classification occur at age 20 years,12 many 18–19 year olds have already transitioned to care in an adult medical home,20 where weight is classified according to adult criteria. Hence there remains a need to more clearly examine differences in weight status classification for late adolescents and relevance to clinical risk.
The goal of this study was to compare BMI classification across the four major weight categories (underweight, normal weight, overweight and obesity) and higher order obesity using U.S. pediatric BMI percentile versus adult WHO categories in a diverse real world population of older teens ages 18–19 years. The concordance of adult and pediatric weight classification methods was evaluated to determine whether they accurately represent BMI status for this age group, with examination of blood pressure (BP) findings from the same ambulatory visit to characterize clinical risk. Differences in BMI classification that influence risk stratification were investigated to determine the optimal approach for tracking of BMI and weight status during the transition to adult primary care.
METHODS
Kaiser Permanente Northern California (KPNC) is a large integrated healthcare delivery system providing care to over three million members in the Northern California region. The cohort for this study consisted of 18–19 year old KPNC teenagers who were previously examined in a population study of blood pressure and body mass index21, 22 and had follow up measurement of height and weight during 7/1/2007–12/31/2012. Body mass index was calculated as weight in kilograms divided by height in meters squared (kg/m2). Blood pressure classification was also examined based on ambulatory measurements obtained at the same visit (available in 93.7%), with a hypertensive blood pressure defined by a systolic and/or diastolic BP ≥140 mmHg or ≥90 mmHg, respectively. The Institutional Review Board at HealthPartners Institute for Education and Research approved the study with ceding of oversight authority by the KPNC Institutional Review Board. A waiver of informed consent was obtained due to the nature of the study.
To eliminate potentially erroneous values, we excluded visits with outlying height values flagged as biologically implausible by the CDC program,23 as well as height >90 inches or weight <50 pounds or >500 pounds. In addition, visits at age 18–19 years old were excluded if there was any record of pregnancy up to one year prior to the visit date based on coded diagnoses (International Classification of Diseases, 9th revision, ICD-9 V22.x and V23.x). A pediatric endocrinologist (LCG) conducted manual review of anthropometric data for individuals with (1) BMI ≥50 kg/m2, (2) high BMI values flagged by the CDC program as biologically implausible and without another confirming BMI within 5% of the measurement and (3) BMI values where another BMI was ≥20% of the measurement. A total of 357 growth charts (1.5% of the cohort) were reviewed for such cases and only 26 were excluded due to height or weight entry errors.
The CDC 2000 growth chart reference datasets were used to calculate BMI percentiles,24, 25 with classification as underweight (BMI <5th percentile), normal weight (BMI 5th to <85th percentile), overweight (BMI 85th to <95th percentile) and obese (BMI ≥95th percentile) using pediatric age- and sex-specific BMI percentile criteria.9, 10 Stratification of obesity severity according to pediatric criteria was also examined using the percentage of the 95th BMI percentile,26 with severe obesity defined by BMI ≥120% of the 95th BMI percentile.3, 26, 27 Body mass index classification using adult criteria was based on the WHO14 and NHLBI15 criteria for adults, including underweight (BMI <18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), class I obesity (BMI 30–34.9 kg/m2), class II obesity (BMI 35–39.9 kg/m2) and class III obesity (BMI ≥40 kg/m2). The term moderate obesity was used to describe those individuals with BMI ≥95th percentile and <120% of the 95th percentile or (alternatively) with class I obesity.
To characterize the concordance between pediatric BMI percentile and adult BMI classification for underweight, normal weight, overweight and obesity in this 18–19 year old cohort, we calculated the weighted Cohen’s Kappa (κ) coefficient and 95% confidence intervals overall and separately for males and females. We also examined severe obesity defined as BMI ≥120% of the 95th percentile in comparison with BMI ≥35 kg/m2 and BMI ≥40 kg/m2 using the Cohen’s Kappa statistic. Differences between groups were compared using the chi-square test and a two-sided p value criterion of <0.05 was chosen as the threshold for statistical significance. All analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
A total of 23,640 teenagers (54.3% female) ages 18–19 years old were included in this study. Overall, there were 37.5% non-Hispanic white, 9.4% black, 27.8% Hispanic, 20.6% Asian and 4.6% of other or unknown race. As shown in Table 1, 3.4% were underweight (BMI <5th percentile), 66.6% were normal weight (BMI 5th to <85th percentile), 15.7% were overweight (BMI 85th to <95th percentile) and 14.3% were obese (BMI ≥95th percentile) when pediatric BMI percentile categories were applied. Using adult BMI categories, 5.2% were underweight (BMI <18.5 kg/m2), 58.8% were normal weight (BMI 18.5–24.9 kg/m2), 21.7% were overweight (BMI 25–29.9 kg/m2), and 14.3% were obese (BMI ≥30 kg/m2). For these 18–19 year old teenagers, the majority of clinic visits where BMI was ascertained occurred in adult primary care clinics (72.8%), with only 10.2% occurring in pediatric clinics, 9.6% in gynecology clinics, 2.6% in family practice clinics and the remaining 4.8% in other departments.
Table 1.
Comparison of pediatric body mass index (BMI) percentile and adult BMI criteria for weight classification in 23,640 older teens ages 18–19 years old (column percentages are represented)
| ADULT CRITERIA for absolute BMI Classification | PEDIATRIC CRITERIA for BMI Percentile Classification | BMI PERCENTILE IN THE OBESE RANGE BMI ≥95th percentile |
||||
|---|---|---|---|---|---|---|
| Underweight <5th percentile N = 792 |
Normal weight 5th to <85th percentile N = 15,744 |
Overweight 85th to <95th percentile N = 3721 |
Obese ≥95th percentile N = 3383 |
|||
|
Underweight <18.5 kg/m2 N = 1236 |
761 (96.1%) | 475 (3.0%) § | 0 | 0 |
Moderate obesity <120% × 95th percentile N = 2225 |
Severe obesity ≥120% × 95th percentile N = 1158 |
|
Normal 18.5–24.9 kg/m2 N = 13,899 |
31 (3.9%) € | 13,868 (88.1%) | 0 | 0 | ||
|
Overweight 25–29.9 kg/m2 N = 5130 |
0 | 1401 (8.9%) * | 3532 (94.9%) | 197 (5.8%) ‡ | 197 (8.8%) ‡ | 0 |
|
Obese ≥30 kg/m2 N = 3375 |
0 | 0 | 189 (5.1%) † | 3186 (94.2%) | ||
|
ABSOLUTE BMI IN THE OBESE RANGE BMI ≥30.0 kg/m2 |
Class I obesity 30.0–34.9 kg/m2 N = 1967 |
189 (5.1%) † | 1773 (79.7%) | 5 (0.4%) | ||
|
Class II obesity 35.0–39.9 kg/m2 N = 879 |
0 | 255 (11.5%) ∆ | 624 (53.9%) | |||
|
Class III obesity ≥40 kg/m2 N = 529 |
0 | 0 | 529 (45.7%) | |||
Pediatric criteria for BMI percentile classification: 3.4%, underweight, 66.6% normal weight, 15.7% overweight, 14.3% obese.
Adult criteria for BMI classification in the cohort: 5.2%, underweight, 58.8% normal weight, 21.7% overweight, 14.3% obese.
Bolded numbers and percentages represent concordant classification based on pediatric BMI percentile and adult BMI categories
These 475 (2.0% of cohort, 38 male, 437 female) had underweight BMI values (17.6–18.4 kg/m2) and normal range BMI percentiles (5.0–12.9th percentile)
These 31 (0.1% of cohort) were all male with normal BMI values (18.5–19.0 kg/m2) and underweight BMI percentiles (2.9–4.9th, median 4.6th percentile). They included 4 with chronic/acute illness (3 with subsequently normal BMI during the ensuing 2 years and 1 with no follow-up BMI). Among the remaining 27, 10 had no follow-up BMI, 13 had normal follow-up BMI (18.5–24.9 kg/m2) and 4 had low follow-up BMI (BMI 17.7–17.9 kg/m2, all with height >70 inches and no active health issues) using adult criteria.
These 1401 (5.9% of cohort, 752 male, 649 female) had overweight BMI values (25.0–26.9 kg/m2) and normal range BMI percentiles (72.1–84.9th percentile)
These 189 (0.8% of cohort, 4 male, 185 female) had obese BMI values 30.0–31.4 kg/m2 and overweight range BMI percentiles (93.4–94.9th percentile)
These 197 (0.8% of cohort) were all male with overweight BMI values 29.0–29.9 kg/m2 and obesity range BMI percentiles (95.0–96.4th percentile)
These 255 (1.1% of the cohort, 34 male, 221 female) had BMI ranging 35.0–37.7 kg/m2.
Figure 1 shows the prevalence of low, normal and high BMI using both pediatric BMI percentile and adult BMI classification by gender. A higher percentage of males compared to females were classified as obese by pediatric BMI percentile criteria (16.8% vs 12.2%, p<0.001) and to a lesser degree by adult BMI criteria (15.0% vs 13.7%, p<0.01). For higher order obesity, where the overall proportion of teens varied depending on criteria (4.9% with BMI ≥120% of the 95th percentile, 6.0% with BMI ≥35 kg/m2, and 2.2% with BMI ≥40 kg/m2), a male predominance was seen only when using pediatric BMI percentile criteria for severe obesity (≥120% of the 95th percentile, Figure 1). For the higher order adult obesity categories (BMI ≥35 kg/m2 and ≥40 kg/m2), the proportions by gender were similar. Figure 2 examines differences in the relative prevalence of elevated BMI within each gender subgroup by race/ethnicity. The prevalence of obesity in males was highest among Hispanics followed by blacks, then whites and Asians, regardless of whether pediatric BMI percentile criteria (≥95th percentile) or adult BMI criteria (≥30 kg/m2) were used. For females, the prevalence of obesity was highest in blacks followed by Hispanics, then whites and Asians, also regardless of criteria. For higher order obesity, the prevalence rates were generally highest in Hispanics and blacks, depending on the criteria used.
Figure 1. The proportion of older teens ages 18–19 years old by body mass index (BMI) classification method.
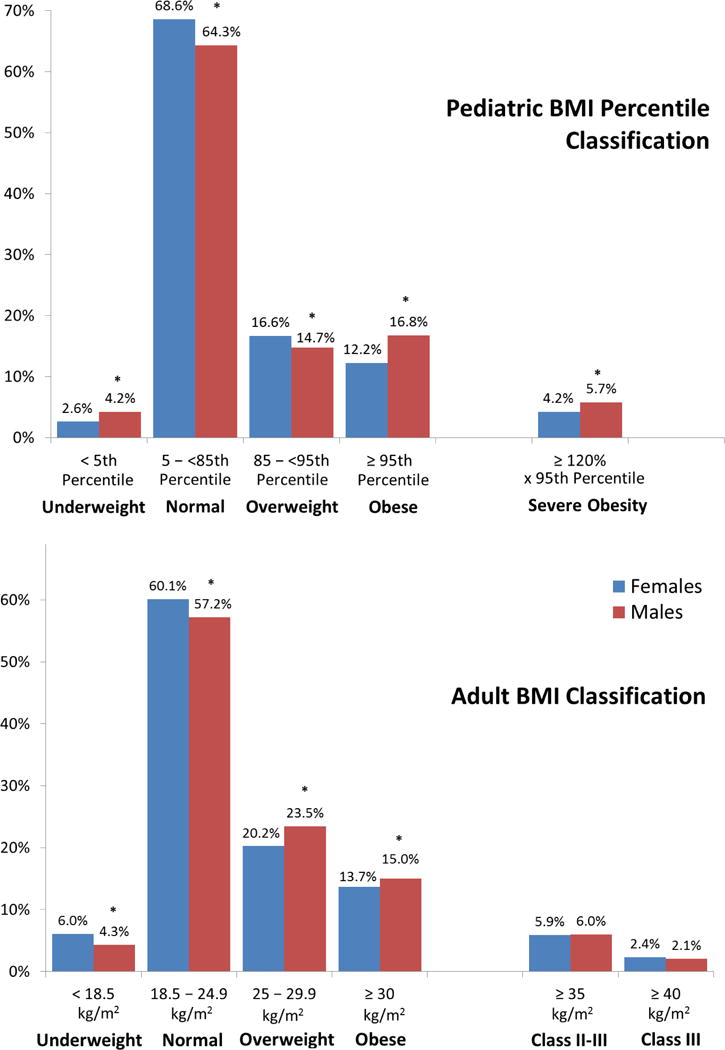
* p <0.01 for females versus males.
Figure 2. Body Mass Index (BMI) by race/ethnicity and sex in teens ages 18–19 years old.
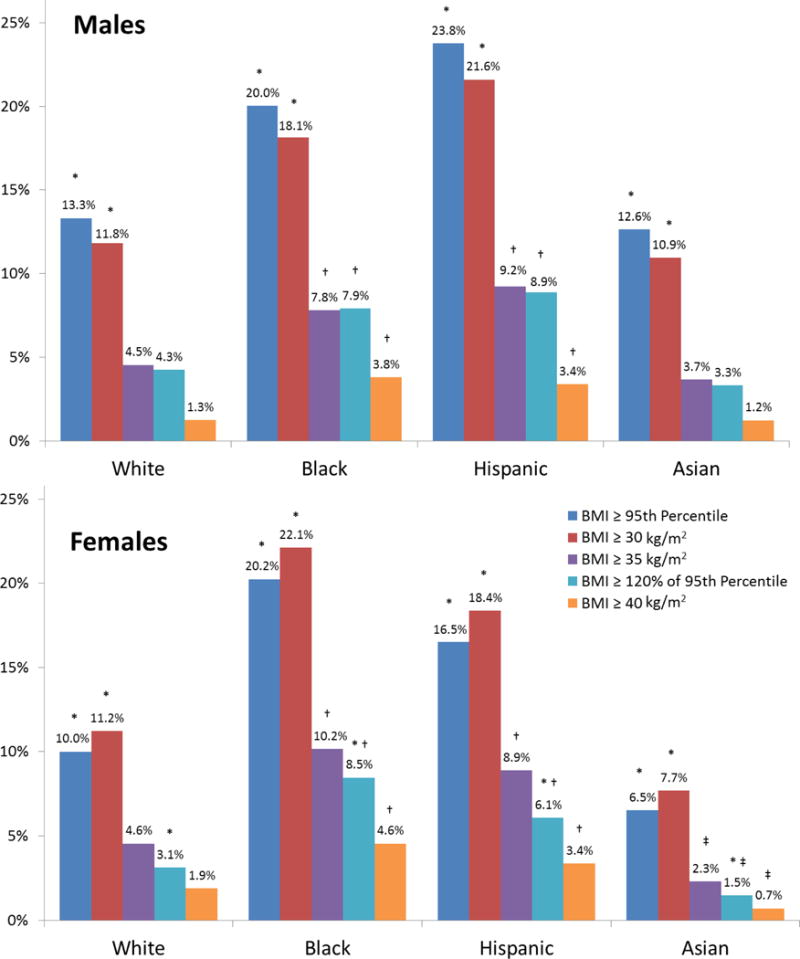
* p <0.05 compared to all other race/ethnic subgroups (white, black, Hispanic or Asian), except for comparisons between white and Asian males
† p <0.05 compared to whites and Asians
‡ p <0.05 compared to whites
Table 1 compares the weight status classification for the cohort using pediatric BMI percentile and adult BMI criteria for underweight, normal weight, overweight and obesity. Of the 18–19 year olds with BMI <5th percentile, most (96.1%) were in the underweight (BMI <18.5 kg/m2) adult category, while the remaining 3.9% (N=31) had BMI values (18.5–19.0 kg/m2) just within the adult normal range, corresponding to the 2.9th – 4.9th BMI percentile (median 4.6th percentile); all were male and mostly in good health except four with weight loss or low body weight due to illness (Table 1 footnote). Among teens in the normal (5th to <85th percentile) or overweight (85th to <95th percentile) BMI percentile range, 88.1% and 94.9%, respectively, were similarly classified based on adult criteria, although 8.9% with normal pediatric BMI percentile range had BMI values (25.0–26.9 kg/m2) just within the adult overweight range, accounting for 1401 (5.9%) of individuals. An additional 5.1% with overweight BMI percentile had BMI values just within the adult obese range (BMI 30.0–31.4 kg/m2, 97.9% female). Finally, 94.2% of those with BMI ≥95th percentile also met BMI criteria for adult obesity, while the remaining 5.8% had BMI values (29.0–29.9 kg/m2) just below the adult obesity threshold. Overall, 90.3% of the cohort was concordantly classified; an additional 5.9% were discordantly classified as overweight by adult criteria and normal weight by pediatric criteria and the remaining discordant subgroups each contributed less than 2% of the cohort (Table 1, footnote). Comparing pediatric BMI percentile and adult BMI classification across the four primary weight categories of underweight, normal, overweight and obesity, the weighted Kappa statistic was 0.87 (95% confidence interval, CI 0.87–0.88) overall and similar when stratified by gender (weighted Kappa 0.87, 95% CI 0.86–0.88 for females and 0.88, 95% CI 0.87–0.89 for males), demonstrating a high level of agreement.
Table 1 further examines the categorization of obese teenagers, comparing pediatric obesity stratification of moderate and severe obesity (based on the threshold of 120% of the 95th BMI percentile) to the adult thresholds for higher order obesity above BMI ≥30 kg/m2 designated as class I, II and III obesity. Nearly all teens with adult class I obesity had a BMI <120% of the 95th percentile and approximately 71% with class II obesity had BMI ≥120% of the 95th percentile. Among the 255 individuals with class II obesity and BMI <120% of the 95th percentile, 86.7% were female. These findings are expected given that a BMI of 120% of the 95th percentile is approximately equivalent to 35 kg/m2 and 37 kg/m2 in 18–19 year old males and females, respectively. The corresponding Kappa statistic for comparison of BMI ≥120% of the 95th percentile to a uniform threshold of BMI ≥35 kg/m2 was 0.89 (95% CI 0.88–0.91). This agreement was much lower when comparing BMI ≥120% of the 95th percentile to BMI ≥40 kg/m2 (Kappa statistic 0.62, 95% CI 0.59–0.64).
Figure 3 reports the prevalence of hypertensive BP at the index visit by gender and weight classification, including concordantly and discordantly classified subgroups. Overall, males had a higher prevalence of hypertensive BP compared to females, and across both genders, obese teens had the highest rates of hypertensive BP. An increased prevalence of hypertensive BP was evident among males with normal BMI percentile but BMI in the adult overweight range when compared to males with normal BMI by both criteria (3.3% vs. 1.6%, p<0.001). Females discordantly classified as moderately obese by pediatric criteria and class II obese by adult criteria also had a higher prevalence of hypertensive BP when compared with females concordantly classified as having moderate or Class I obesity (5.0% vs. 2.1%, p<0.02).
Figure 3. Hypertensive blood pressure (BP) by weight status in 18–19 year old teens†.
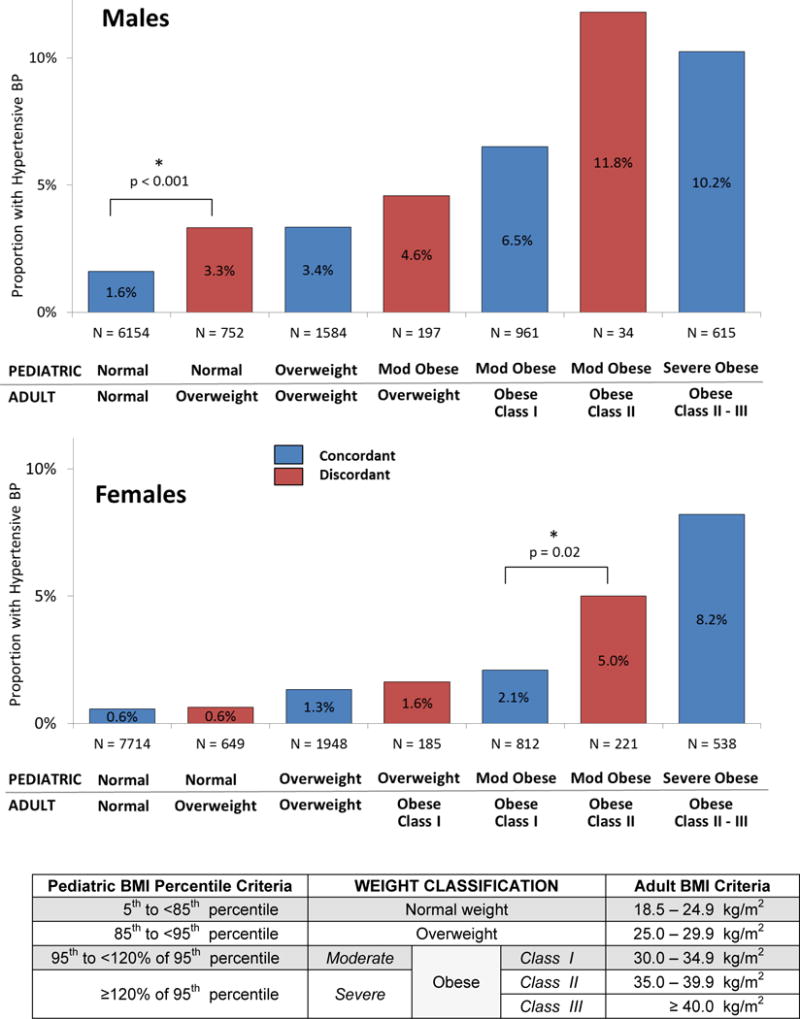
* p<0.05 comparing adjacent groups
† All adjacent groups were compared. Underweight teens (N = 1267) and those in discordant overweight/obese subcategories with N ≤ 5 (9 overweight/obese males) are not shown.
DISCUSSION
In this racially and ethnically diverse cohort of more than 20,000 U.S. teenagers age 18–19 years old, the distributions of BMI using adult WHO definitions and pediatric BMI percentile criteria were examined by gender and race/ethnicity. Overall, a high level of agreement was seen between pediatric and adult classification across the four major weight groups – underweight, normal weight, overweight and obese, with only a small proportion (less than 10%) discordantly classified due to borderline values. Among those discordantly classified into different weight groups by pediatric BMI percentile and adult BMI criteria thresholds, more than half were in the upper normal BMI percentile range with overweight BMI values of 25.0–26.9 kg/m2, where the male subgroup was found to have a higher prevalence of hypertensive BP than their normal BMI counterparts. These individuals would arguably benefit from classification as overweight for both BMI tracking and intervention.
Among obese teenagers within this older age range, a high level of agreement was also found between the pediatric BMI percentile threshold for severe obesity and the adult threshold for class II obesity, appropriately so given that a BMI of 120% of the 95th percentile for severe pediatric obesity approaches a BMI of 35 kg/m2 in males and 37 kg/m2 in females at age 18–19 years.11 Among females with moderate obesity by pediatric BMI percentile criteria, those with class II adult obesity had a significantly higher prevalence of hypertensive BP compared to those classified as having moderate or class I adult obesity. These BP findings further support use of adult BMI criteria in older teens, including a BMI threshold of 35 kg/m2 associated with a higher prevalence of hypertensive BP in females. Comprehensive data on fasting glucose, lipids and hemoglobin A1C were not obtained in the majority of patients in this study. However, the greater proportion with elevated BP (albeit limited to a single ambulatory measurement insufficient to support a formal diagnosis of hypertension without repeated BP) in teenagers discordantly classified with lower pediatric BMI percentile but higher adult BMI category supports the use of adult BMI criteria in older adolescents to identify candidates for overweight and obesity intervention.
According to the 2000 CDC growth charts for children and adolescents age 2–19 years old, the reference values for height, weight and BMI are age- and sex-dependent25 until the transition to adult BMI classification at age 20 years.12 However, the CDC growth chart upper limit of BMI 36–37 kg/m2 makes it difficult to track BMI percentile in the heaviest adolescents,28 many of whom have BMI ≥40 kg/m2 that well exceeds the 99th percentile. As such, expressing BMI as a percentage above the 95th BMI percentile enables specific BMI tracking for severely obese children and adolescents,26, 28 and has been shown in preliminary studies to be associated with clinically relevant health risk.22 However, this approach requires specialized growth charts11, 28 and is not practical in the young adult clinic setting. In the current study, 6% met criteria for class II adult obesity or higher and 2.2% met criteria for class III obesity (similar to rates reported from nationally representative data)4 with BMI values ranging as high as 78 kg/m2. In addition to existing recommendations for BMI ≥30 kg/m2 to further classify pediatric obesity and more recent recommendations for BMI ≥35 kg/m2 to define severe obesity in children and adolescents with BMI <120% of the 95th percentile (aligning with class II obesity or greater),11 our study findings support the use of discrete BMI values for classifying and tracking overweight and obesity severity in older teens with high BMI, providing a practical approach to weight assessment and management. This older adolescent age range also corresponds to an expected plateauing in linear growth,8 albeit weight and corresponding BMI may continue to increase.
In summary, in this diverse, community-based cohort of older U.S. teenagers in whom obesity and severe obesity were prevalent, a high degree of concordance was seen when classifying BMI using either pediatric BMI percentile or adult BMI criteria, with an absolute BMI threshold of 35 kg/m2 to define severe obesity. Furthermore, in a significant number of overweight at-risk older adolescents, using adult BMI criteria may better identify individuals who could benefit from closer observation and lifestyle intervention. From a real-world clinical perspective, the adult WHO/NHLBI classification criteria for BMI provides a practical approach for management of teen health for the many teenagers who have transitioned from pediatric to adult primary care.
What is already known about this subject
Body mass index (BMI) classification of weight status in the United States (U.S.) changes from pediatric BMI percentile categories to adult BMI categories at age 20 years.
Many teenagers transition at age 18 to adult medical care, where pediatric growth charts are unlikely to be used for weight classification.
Although the pediatric and adult BMI cut points roughly approach similar thresholds for overweight and obesity in older teenagers, the extent to which weight status is discordantly classified in this age group and the relationship with clinical risk stratification is unknown.
What this study adds
For 18–19 year old U.S. teenagers, a high level of agreement exists between pediatric BMI percentile and adult BMI thresholds across underweight, normal, overweight and obese categories, with less than 10% discordant; a high level of agreement also exists between pediatric severe obesity and the BMI threshold for adult class II obesity.
Normal weight males and moderately obese females by pediatric BMI percentile criteria who were discordantly classified into a higher adult weight strata had significantly higher rates of hypertensive blood pressure compared to their concordantly classified counterparts.
Adult BMI weight classification provides a practical approach for risk stratification and tracking of weight status in older teenagers, many of whom have already transitioned to adult medical care.
Acknowledgments
JL, BM, MC and LG conceived the project. MC conducted the data analyses. BM, JL and LG drafted the initial manuscript. All authors provided critical input on data analysis and interpretation, revised the manuscript for important intellectual content, and approved the final version. The authors would like to acknowledge Joel Gonzalez for his support with manuscript preparation. This study was funded by the National Heart, Lung and Blood Institute at the National Institutes of Health 1RO1HL093345 to HealthPartners Research Foundation (Patrick O’Connor, Principal Investigator) and conducted within the Cardiovascular Research Network, a consortium of research organizations affiliated with the HMO Research Network and sponsored by the National Heart Lung and Blood Institute (U19 HL91179-01).
Footnotes
DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST:
L.Greenspan has received payment for a manuscript unrelated to the current study. R.Prineas has received payment for consultancy to Health Partners, Inc. J.Lo has received grant funding from Sanofi unrelated to the current study. J.Lo, M.Chandra, L. Greenspan, M.Daley and K.Margolis have received funding from the National Institutes of Health. The remaining authors have no potential conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang YC, Gortmaker SL, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976–2006. Int J Pediatr Obes. 2011;6:12–20. doi: 10.3109/17477161003587774. [DOI] [PubMed] [Google Scholar]
- 4.Skinner AC, Skelton JA. Prevalence and Trends in Obesity and Severe Obesity Among Children in the United States, 1999–2012. JAMA Pediatr. 2014 doi: 10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- 5.Alberga AS, Sigal RJ, Goldfield G, Prud’homme D, Kenny GP. Overweight and obese teenagers: why is adolescence a critical period? Pediatr Obes. 2012;7:261–73. doi: 10.1111/j.2047-6310.2011.00046.x. [DOI] [PubMed] [Google Scholar]
- 6.Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–44. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 7.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. The American journal of clinical nutrition. 2002;76:653–8. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 8.CDC growth charts: United States. http://www.cdc.gov/growthcharts/clinical_charts.htm. Accessed January 9, 2013. [PubMed]
- 9.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. National health statistics reports. 2010:1–5. [PubMed] [Google Scholar]
- 10.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 11.Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128:1689–712. doi: 10.1161/CIR.0b013e3182a5cfb3. [DOI] [PubMed] [Google Scholar]
- 12.About BMI for Adults. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed March 27, 2013.
- 13.BMI Percentile Calculator for Child and Teen English Version. http://apps.nccd.cdc.gov/dnpabmi/. Accessed January 4, 2013.
- 14.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 15.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults–The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 16.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–94. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 18.Flegal KM, Ogden CL. Childhood Obesity: Are We All Speaking the Same Language? Adv Nutr. 2011;2:159S–66S. doi: 10.3945/an.111.000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 21.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131:e415–24. doi: 10.1542/peds.2012-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lo JC, Chandra M, Sinaiko A, et al. Severe obesity in children: prevalence, persistence and relation to hypertension. Int J Pediatr Endocrinol. 2014;2014:3. doi: 10.1186/1687-9856-2014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cut-offs to define outliers in the 2000 CDC Growth Charts. http://www.cdc.gov/nccdphp/dnpa/growthcharts/resources/BIV-cutoffs.pdf. Accessed April 26, 2012.
- 24.A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 y) http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed October 20, 2011.
- 25.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000:1–27. [PubMed] [Google Scholar]
- 26.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90:1314–20. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- 27.Koebnick C, Smith N, Coleman KJ, et al. Prevalence of extreme obesity in a multiethnic cohort of children and adolescents. J Pediatr. 2010;157:26–31 e2. doi: 10.1016/j.jpeds.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gulati AK, Kaplan DW, Daniels SR. Clinical tracking of severely obese children: a new growth chart. Pediatrics. 2012;130:1136–40. doi: 10.1542/peds.2012-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]


