Abstract
Objective
Recently, numerous studies have reported that hexokinase-2 (HK2) is aberrantly expressed in cancer, indicating that HK2 plays a pivotal role in the development and progression of cancer. However, its prognostic significance in solid tumor remains unclear. Accordingly, we performed a meta-analysis to assess the prognostic value of HK2 in solid tumor.
Methods
Eligible studies were identified using PubMed, Embase, and Web of Science databases. Pooled hazard ratios (HRs) with 95% confidence intervals (CIs) for overall survival (OS) or progression-free survival (PFS)/disease-free survival (DFS)/relapse-free survival (RFS) were estimated with random effects or fixed effects models, respectively. Subgroup analysis was also performed according to patients’ ethnicities, tumor types, detection methods, and analysis types.
Results
Data from 21 included studies with 2532 patients were summarized. HK2 overexpression was significantly associated with worse OS (pooled HR = 1.90, 95% CI = 1.51–2.38, p < 0.001) and PFS (pooled HR = 2.91, 95% CI = 2.02–4.22, p < 0.001) in solid tumor. As to a specific form of cancer, the negative effect of HK2 on OS was observed in hepatocellular carcinoma (pooled HR = 2.06, 95% CI = 1.67–2.54, p < 0.001), gastric cancer (pooled HR = 1.72, 95% CI = 1.09–2.71, p = 0.020), colorectal cancer (pooled HR = 2.89, 95% CI = 1.62–5.16, p < 0.001), but not in pancreatic cancer (pooled HR = 1.13, 95% CI = 0.28–4.66, p = 0.864). No publication bias was found in the included studies for OS (Begg’s test, p = 0.325; Egger’s test, p = 0.441).
Conclusion
In this meta-analysis, we identified that elevated HK2 expression was significantly associated with shorter OS and PFS in patients with solid tumor, but the association varies according to cancer type.
Introduction
Cancer has being the leading cause of mortality worldwide and is therefore a major public health threat. Solid tumors account for most of human cancers [1]. Currently, curative surgical resection is still the optimal therapy for primary solid tumor. However, outcome may vary in patients with the same tumor after surgery. Thus, to precisely evaluate the therapeutic effect and prognosis of patients who suffer from cancer, feasible and effective biomarkers are urgently needed.
Numerous studies have shown that cancer metabolism is closely related to cancer cell survival owing to the sharing of common signaling molecules between these two pathways [2–4]. Cancer cells prefer to convert glucose to lactic acid as the main source of energy, regardless of oxygen availability, a phenomenon designated the Warburg effect or aerobic glycolysis [5]. Aerobic glycolysis generates less ATP than oxidative phosphorylation (OXPHOS), but can rapidly provide sufficient energy and biosynthetic precursors for cellular proliferation. Therefore aerobic glycolysis has been identified as the seventh hallmark of cancer [6]. Although the glycolysis rate can be regulated by a number of metabolic enzymes in the glycolytic pathway, most studies have suggested that glycolytic flux primarily relies on upregulation of glucose transporters and hexokinase (HK) [7, 8]. Specifically, HK2 has been suggested to contribute to the increased glycolysis by catalyzing the conversion from glucose to glucose-6-phosphate in the glycolytic pathway of cancer cells [9].
Recently, overexpression of HK2 has been reported in various solid tumors, including colorectal cancer [10], hepatocellular carcinoma [11], ovarian cancer [12], and pancreatic cancer [13], indicating that HK2 plays an important role in the development and progression of cancer. However, the prognostic value of HK2 was still controversial. Many studies have shown that overexpression of HK2 is associated with poor prognosis [14–16], whereas a few studies have demonstrated the opposite results [10].
Thus, in order to clarify the prognostic significance of HK2 as a metabolic marker in various solid tumors, we performed a meta-analysis on data collected systematically.
Methods
Search Strategy
The PubMed, Embase, and Web of Science databases were used for a comprehensive literature search with the following terms and their combinations: “hexokinase-2 or HK2 or HK-2”, “cancer or carcinoma or tumor or neoplasm”, and “prognosis or prognostic or outcome or survival”. The last search was conducted on September 28, 2016. Any potential studies were manually searched for in the references.
Inclusion and Exclusion Criteria
Eligible studies met the following inclusion criteria: evaluation of patients with pathologically diagnosed solid tumors; the study contained sample size more than 20; published in English; studies aimed to explore the association between HK2 expression and prognosis; and studies with hazard ratios (HRs) and confidence intervals (CIs), which could be directly obtained or calculated with relevant data.
The exclusion criteria were as follows: studies of tumor cell lines, animal experiments, or non-solid tumors; published in a language other than English; duplicate reports and inappropriate article types, such as case reports, letters, conference papers, and reviews; studies without sufficient data for obtaining HRs and CIs.
Data Extraction and Quality Assessment
Data were extracted from the included studies by two authors (Yulin Liu and Liang Shi) independently, and a third author (Ke Wu) was responsible for reconciling disagreements. Extracted data included first author’s name, publication year, country, tumor type, sample size, tumor stage, mean age, cut-off value, and outcome. The adopted indexes for outcomes included overall survival (OS) and progression-free survival (PFS)/disease-free survival (DFS)/relapse-free survival (RFS). The quality of the included studies was assessed using the Newcastle-Ottawa Scale (case-control studies) [17]. The score ranged from 0 to 9, and studies with scores of 6 or more were regarded as high quality.
Statistical Analysis
HRs and their 95% CIs were used to assess the prognostic value of elevated HK2 expression in solid tumor. The reported statistical variables were extracted directly from the primary studies. If not given explicitly, variables were calculated using the Kaplan-Meier method or available data according to Tierney’s method [18]. Heterogeneity analysis was performed by visual observation of forest plots with the I2 statistic and Chi-squared tests [19]. I2 > 50% and/or p < 0.05 was considered representative of obviously heterogeneity, and a random effect model was applied to pool the HRs and their CIs. Otherwise, a fixed effect model was applied. Pooled HRs of greater than 1 represented poor prognosis of elevated HK2 expression, and results with p values of less than 0.05 were considered statistically significant. Subgroup analysis was further performed for interpretation of identified heterogeneity. Additionally, the consistency of pooled outcomes was examined with sensitivity analysis. Publication bias was investigated using funnel plots with Egger’s test and Begg’s test, and results with p values of less than 0.05 were considered to be indicative of significant bias. Stata 12.0 software was used for all statistical analyses in this meta-analysis.
Results
Eligible Studies
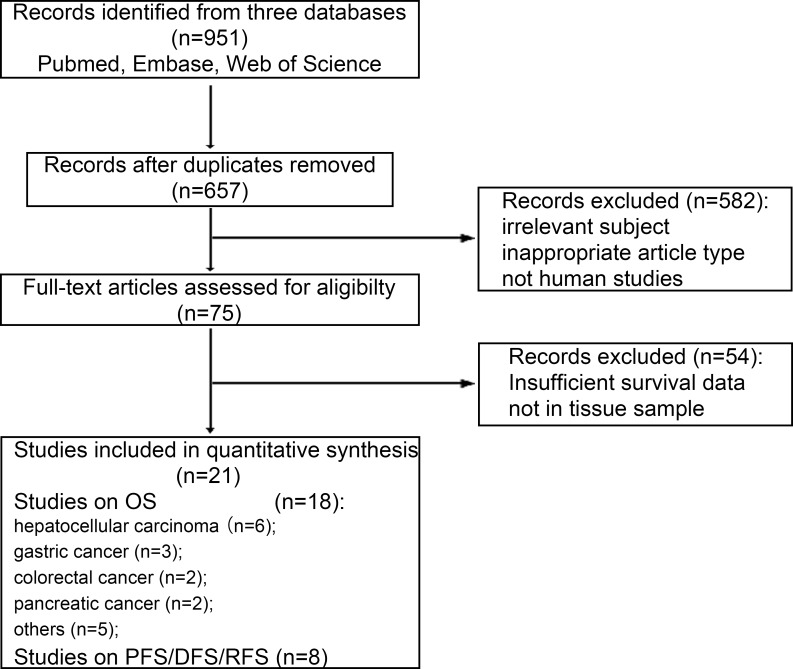
According to our defined searching strategy, a total of 951 references were identified after an initial search. After screening by titles and abstracts, 876studies were excluded on account of duplicated data, irrelevant subject, inappropriate article type, and inappropriate study type (i.e., cell and animal experiments). The 75 remaining studies for the association of HK2 overexpression with cancer prognosis were evaluated by reading the full text. Finally, 21studies consisting of 2532 cases were evaluated in this meta-analysis (Fig 1).
Fig 1. Flow diagram shows search strategy.
Characteristics of Included Studies
The main characteristics of the included studies are shown in Table 1. Twenty-one eligible studies from China, Japan, Korea, the United States of America, Canada, and Germany included patients who had been diagnosed with a variety of solid tumors, such as hepatocellular carcinoma, gastric cancer, colorectal cancer and pancreatic cancer. HK2 protein and mRNA expression in tumor tissues were detected in 18 and three studies, respectively. 18 studies provided data on OS, which including hepatocellular carcinoma (n = 6), gastric cancer (n = 3), colorectal cancer (n = 2), pancreatic cancer (n = 2) and others (n = 5). Eight studies provided data on PFS/DFS/RFS. HRs were directly extracted from 14 studies and calculated with available data or survival curves from the other seven studies. The cut-off values for positive expression of HK2 varied in these studies. In quality assessment, all of the included studies had scores ranging from 6 to 9, indicating that they were of high quality.
Table 1. The main characteristics of the included studies in the meta-analysis.
| First author | Year | Country | Tumor type | Sample size | Stage | Method | Mean age | Cut-off value | Analysis | Outcome | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhang [20] | 2016 | China | HCC | 155 | I-IV | IHC | NR | CS | univariate | OS | 7 |
| Guo [21] | 2015 | China | HCC | 120 | I-IV | RT-PCR | NR | NR | survival curves | OS | 7 |
| Gong [22] | 2012 | China | HCC | 97 | I-IV | RT-PCR | NR | 0.39% | survival curve | OS | 8 |
| Kwee [23] | 2012 | America | HCC | 157 | I-IV | IHC | NR | CS | multivariate | OS | 9 |
| Peng [14] | 2008 | China | HCC | 203 | I-IV | RT-PCR | 54.9 | ratio ≥1.5 | survival curve | OS | 8 |
| Paudyal [24] | 2008 | Japan | HCC | 31 | I-IV | IHC | NR | CS | multivariate | OS | 8 |
| Hur [25] | 2013 | Korea | GC | 152 | I-IV | IHC | 55.8±13.6 | staining≥30% | univariate | OS/DFS | 7 |
| Qiu [16] | 2011 | China | GC | 188 | I-IV | IHC | 57 | NR | multivariate | OS | 8 |
| Rho [26] | 2007 | Korea | GC | 257 | I-IV | IHC | 54.6 | staining≥10% | multivariate | OS | 9 |
| Katagiri [27] | 2016 | Japan | CRC | 195 | I-IV | IHC | 64.5 | staining≥10% | multivariate | OS | 8 |
| Ho [28] | 2016 | Canada | CRC | 60 | I-IV | IF | NR | F-Score ≥ 24.7 | univariate | OS/PFS | 7 |
| Hamabe [10] | 2014 | Japan | CRC | 104 | I-IV | IHC | NR | CS | survival curve | RFS | 8 |
| Ogawa [13] | 2015 | Japan | PC | 36 | I- III | IHC | 70 | CS | multivariate | OS/RFS | 7 |
| Lyshchik [29] | 2007 | Japan | PC | 74 | I-IV | IHC | 63.5 ± 9.2 | index≥3 | survival curve | OS | 8 |
| Sato [30] | 2013 | Japan | BC | 118 | I- III | IHC | 57 | staining≥10% | survival curve | DFS | 7 |
| Palmieri [31] | 2009 | Germany | BC | 123 | NR | IHC | 51 | NR | multivariate | OS | 8 |
| Zhang [32] | 2016 | China | NPC | 140 | I-IV | IHC | 48 | index≥3 | multivariate | OS/PFS | 9 |
| Huang [33] | 2015 | China | CCA | 132 | I-IV | IHC | 51 | staining≥25% | multivariate | PFS | 8 |
| Suh[12] | 2014 | Korea | EOC | 111 | I-IV | IHC | NR | CS | multivariate | OS/PFS | 9 |
| Tsukada [34] | 2012 | Japan | ULMS | 23 | I | IHC | 51.5 | CS | multivariate | OS | 8 |
| Wolf [15] | 2011 | Canada | GBM | 56 | NR | IHC | NR | NR | multivariate | OS | 7 |
HCC: hepatocellular carcinoma; GC: gastric cancer; CRC: colorectal cancer; PC: pancreatic cancer; BC: breast cancer; NPS: nasopharyngeal carcinoma; CCA: cervical carcinoma; EOC: epithelial ovarian carcinoma; ULMS: uterine leiomyosarcoma; GBM: glioblastoma multiforme; IHC: immunohistochemistry; RT-PCR: reverse transcription-polymerase chain reaction; IF: immunofluorescence; NR: not reported; CS: complex score combining intensity and percentage of HK2 expression.
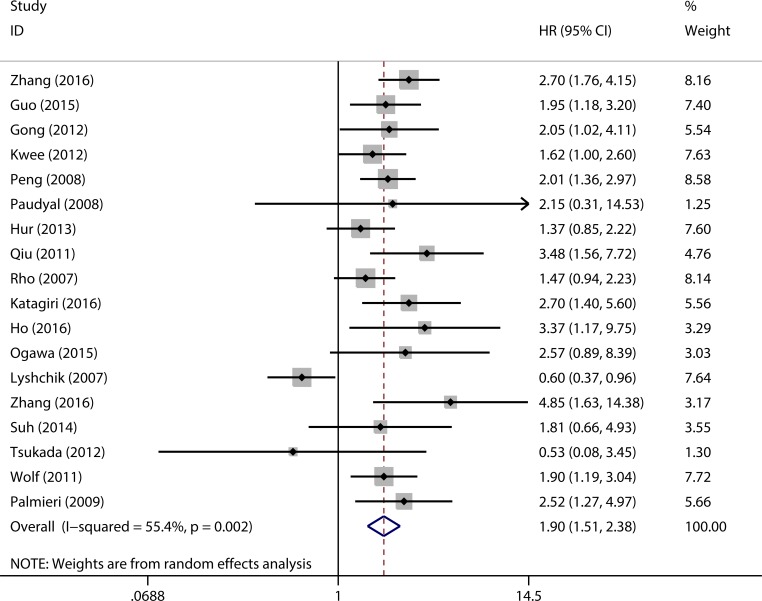
Correlation of HK2 Expression with OS and Subgroup Analysis
The combined analysis of 18 studies showed that elevated HK2 expression was associated with worse OS (pooled HR = 1.90, 95% CI = 1.51–2.38, p < 0.001) (Fig 2). Owing to moderate heterogeneity (I2 = 55.4%, p = 0.002), a random effect model was used to pool HRs.
Fig 2. Forest plots to assess the effect of elevated HK2 expression on OS in patients with various solid tumors.
In order to identify the possible sources of heterogeneity across these studies, subgroup analysis was performed according to patients’ ethnicity, tumor type, detection method, and analysis type (Table 2). Subgroup analysis by patient ethnicity showed that HK2 overexpression was significantly associated with worse OS in Asian patients (pooled HR = 1.86, 95% CI = 1.39–2.49, p < 0.001) and Caucasian patients (pooled HR = 1.97, 95% CI = 1.47–2.63, p < 0.001). The negative effect of HK2 overexpression on OS was demonstrated in patients with hepatocellular carcinoma (pooled HR = 2.06, 95% CI = 1.67–2.54, p < 0.001), gastric cancer (pooled HR = 1.72, 95% CI = 1.09–2.71, p = 0.020), colorectal cancer (pooled HR = 2.89, 95% CI = 1.62–5.16, p < 0.001) and others (pooled HR = 2.15, 95% CI = 1.44–3.21, p < 0.001), but not with pancreatic cancer (pooled HR = 1.13, 95% CI = 0.28–4.66, p = 0.864). In subgroup analysis based on detection method, overexpression of HK2 could significantly indicate poor outcome in patients with solid tumor (IHC: pooled HR = 1.85, 95% CI = 1.37–2.49, p < 0.001; RT-PCR: pooled HR = 2.00, 95% CI = 1.51–2.65, p < 0.001). Subgroup analysis by the type of analysis suggested that elevated HK2 expression was significantly associated with shorter OS using either univariate analysis (pooled HR = 1.72, 95% CI = 1.13–2.61, p = 0.011) or multivariate analysis (pooled HR = 1.99, 95% CI = 1.60–2.46, p < 0.001).
Table 2. Pooled HRs for OS according to subgroup analysis.
| Subgroup | No. of patients | No. of studies | Random-effect model | Heterogeneity | ||
|---|---|---|---|---|---|---|
| HR (95% CI) | p value | I2 (%) | p value | |||
| Overall survival | 2178 | 18 | 1.90 (1.51, 2.38) | < 0.001 | 55.4 | 0.002 |
| Ethnicity | ||||||
| Asian | 1782 | 14 | 1.86 (1.39, 2.49) | < 0.001 | 63.4 | 0.001 |
| Caucasian | 396 | 4 | 1.97 (1.47, 2.63) | < 0.001 | 0 | 0.541 |
| Tumor type | ||||||
| HCC | 763 | 6 | 2.06 (1.67, 2.54) | < 0.001 | 0 | 0.767 |
| GC | 597 | 3 | 1.72 (1.09, 2.71) | 0.020 | 52.1 | 0.124 |
| CRC | 255 | 2 | 2.89 (1.62, 5.16) | < 0.001 | 0 | 0.731 |
| PC | 110 | 2 | 1.13 (0.28, 4.66) | 0.864 | 81.7 | 0.019 |
| Others | 453 | 5 | 2.15 (1.44, 3.21) | < 0.001 | 17.6 | 0.303 |
| Detection method | ||||||
| IHC | 1698 | 14 | 1.85 (1.37, 2.49) | < 0.001 | 63.9 | 0.001 |
| RT-PCR | 420 | 3 | 2.00 (1.51, 2.65) | < 0.001 | 0 | 0.992 |
| IF | 60 | 1 | 3.37 (1.17, 9.74) | 0.024 | - | - |
| Analysis type | ||||||
| Multivariate | 1317 | 11 | 1.99 (1.60, 2.46) | < 0.001 | 4.3 | 0.402 |
| Univariate | 861 | 7 | 1.72 (1.13, 2.61) | 0.011 | 77.3 | < 0.001 |
| Lyshchik's study | ||||||
| Yes | 2178 | 18 | 1.90 (1.51, 2.38) | < 0.001 | 55.4 | 0.002 |
| No | 2104 | 17 | 2.00 (1.73, 2.32) | < 0.001 | 0 | 0.475 |
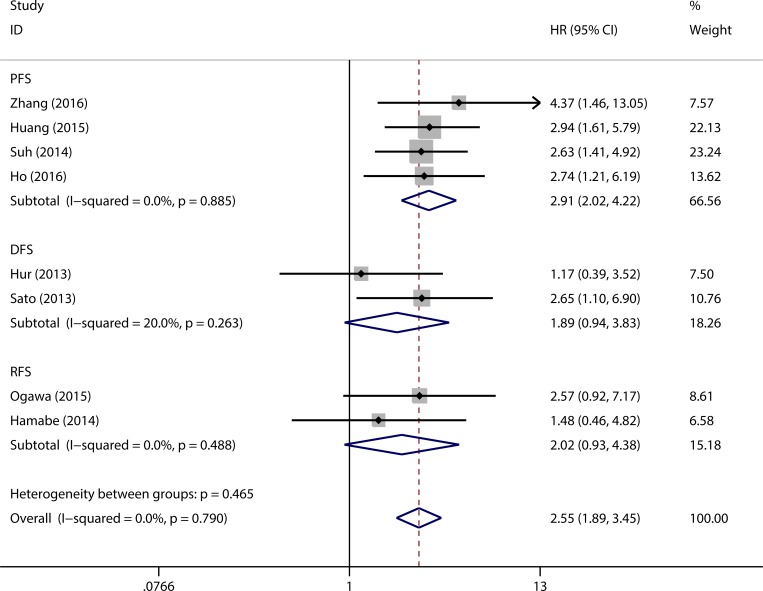
Correlation of HK2 Expression with PFS/DFS/RFS
Eight eligible studies were adopted to pool HRs for PFS/DFS/RFS. Without obvious statistical heterogeneity (I2 = 0.0%, p = 0.790), a fixed effect model was used to pool HRs. The results showed that elevated HK2 expression was associated with negative outcome in patients with solid tumor (pooled HR = 2.55, 95% CI = 1.89–3.45, p < 0.001) (Fig 3). Additionally, data were analyzed based on PFS, DFS, and RFS. Patients with elevated HK2 expression had a significantly shorter PFS (pooled HR = 2.91, 95% CI = 2.02–4.22, p < 0.001). Despite the lack of significant difference, a similar trend was observed for DFS (pooled HR = 1.89, 95% CI = 0.94–3.83, p = 0.074) and RFS (pooled HR = 2.02, 95% CI = 0.93–4.38, p = 0.076).
Fig 3. Forest plots to assess the effect of elevated HK2 expression on PFS/DFS/RFS.
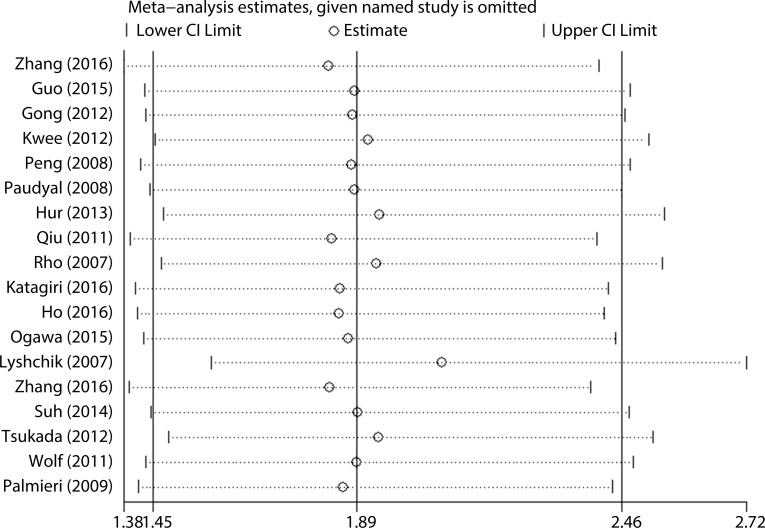
Sensitivity Analysis
Sensitivity analysis was performed by sequentially omitting individual studies with a fixed-effect model (Fig 4). No studies were found to obviously impact the result pattern. Interestingly, one study by Lyshchik et al [22] contributed the most to the observed heterogeneity. After deletion of this study, the observed heterogeneity dramatically decreased (I2 = 55.4%, p = 0.002 versus I2 = 0.0%, p = 0.475). However, the association between HK2 expression and OS was not altered when this study was included (pooled HR = 1.90, 95% CI = 1.51–2.38, p < 0.001) or excluded (pooled HR = 2.00, 95% CI = 1.73–2.32, p < 0.001).
Fig 4. Sensitivity analysis of the evaluation on the relationship between HK2 expression and OS.
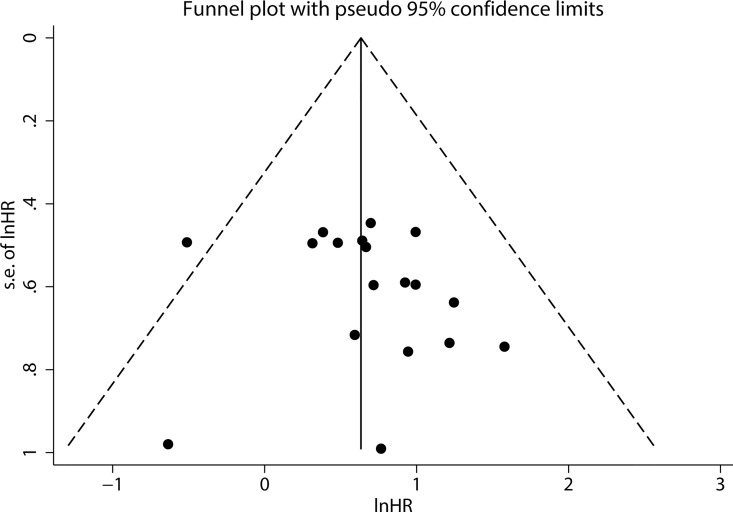
Publication Bias
Publication bias was not found by visual assessment of funnel plots (Fig 5), and this analysis was confirmed by Begg’s test (p = 0.325) and Egger’s test (p = 0.441). Because fewer than 10 eligible studies were used to pool HRs for PFS/DFS/RFS, funnel plots, Begg’s tests, and Egger’s tests were not performed and publication bias was not assessed in these analyses.
Fig 5. Funnel plots to evaluate publication bias of included studies for OS.
Discussion
In the past several decades, aerobic glycolysis has attracted increasing attention as a hallmark of cancer cells. Metabolic reprogramming furnishes cancer cells with sufficient precursor substances for rapid cell proliferation [35, 36]. As a key irreversible step in the glycolytic pathway, the phosphorylation of glucose catalyzed by HK plays a pivotal role in aerobic glycolysis. Meanwhile, HK is involved in the initiation and progression of tumor; in particular, HK2 is a critical component integrating cell viability and energy production pathways [21, 37]. The pro-survival effect of HK2 is achieved mainly through the following three mechanisms: (1) upregulation of HK2 facilitates the generation of biosynthetic precursors for cellular proliferation by increasing glycolysis rate [38]; (2) overexpression of HK2 could increase NADPH levels in the cytoplasm through the pentose phosphate pathway, contributing to protection of cells from oxidative damage [39]; and (3) HK2 can bind to mitochondria and preserve mitochondrial integrity in order to block mitochondrial death pathways [40]. Therefore, elevated expression of HK2 is critical for promoting tumor progression.
Accumulating evidence has revealed that elevated HK2 expression is associated with not only the development and progression of tumor [37, 41], but also with an unfavorable prognosis [23]. The overexpression of HK2 was positively correlated with tumor stage, differentiation and lymph node metastasis, as well as with a reduction in survival [10, 16, 21, 32].To the best of our knowledge, the present study is the first meta-analysis systematically exploring the prognostic value of elevated HK2 expression in solid tumor. In brief, our meta-analysis provided strong support that elevated HK2 expression was a significant independent indicator of poor outcome based on pooled HRs estimates. HK2 was associated with shorter OS in hepatocellular carcinoma, gastric cancer and colorectal cancer. The adverse prognostic effect of HK2 overexpression was virtually unaffected by ethnic background, analysis type and detection method. Moreover, patients with elevated HK2 expression had a significantly shorter PFS. Besides as an independent indicator of poor prognosis, combination of the expression of HK2 and other biomarkers could hold potent prognostic value in patients with solid tumor. In pancreatic cancer, although the positive expression of HK2 exhibited borderline significant prognostic value for OS, the combination of elevated expression of HK2 and PKM2 was found to be significant (P<0.05) [13]. Hamabe et al. reported that the combined evaluation of positive HK2 and negative phosphorylated pyruvate dehydrogenase (p-PDH) was associated with reduced RFS in stage II and III patients with CRC [10].[29]
Interestingly, we also found HK2 failed to predict the outcome of patients with pancreatic cancer. This discrepancy may be partly attributed to the small sample size in the individual studies [13, 29]. In addition, data from univariate analysis were adopted to estimate the prognostic role of HK2 expression in the study by Lyshchik et al [29], allowing us to ignore the effects of clinicopathological factors on the prediction efficacy of HK2. Sensitivity analysis revealed that the study by Lyshchik et al was the main source of heterogeneity. After deletion of this study, the observed heterogeneity completely disappeared. Finally, considering that pancreatic cancer remains a lather disease in spite of improvement in early diagnosis, curative surgical resection, and adjuvant therapies, multidisciplinary treatment is required for a complete cure [42]. Preoperative treatment have an effect on immunohistochemical staining patterns, which may impair the predictive efficacy of HK2 on outcome in tumor.
And yet for all that, as a key regulator of glycolysis, the expression of HK2 is likely significant for the progression and prognosis of pancreatic cancer. The dense desmoplastic region surrounding pancreatic cancer cells inhibits neovascularization, leading to the deficiency of oxygen and nutrients in tumor tissue [43, 44]. Under such stressful microenvironment, cancer cells undergo a shift in cellular metabolism from oxidative phosphorylation to glycolysis [45], as a hallmark of cancer cells. Therefore, more studies designed rationally are required to confirm that elevated HK2 expression is associated with unfavorable outcome in patients with pancreatic cancer.
In spite of the strong results of our study, there were still several limitations to our meta-analysis. First, although the study by Lyshchik et al was identified as the main source of heterogeneity, specific clinical elements that contributed to the heterogeneity were not explicit. Second, due to the use of various cut-off values in the included studies, the utility of HK2 as a prognostic biomarker was impaired in patients with solid tumor. Accordingly, it may be necessary to standardize detection methods and cut-off values. Third, because multiple factors affect prognosis, we preferred to include studies in which multivariate analysis had been performed; however, eight studies with univariate analysis only were still included for a comprehensive analysis. In general, multivariate analysis is more efficient and precise when there are multiple interacting variables in one experiment [46]. Subgroup analysis indicated that multivariate analysis also yielded more stable results. Finally, the approach for obtaining essential data to pool HRs could be a potential source of heterogeneity. The pooled HRs extracted directly from the primary studies seemed to be more reliable than those calculated with survival curves or available data. Although subgroup analysis by tumor type was conducted, the impact of HK2 on prognosis was lost in some specific forms of cancer. Hence, it is essential for more studies to enroll patients with specific forms of cancer.
In conclusion, our meta-analysis suggested that HK2 could act as an independent prognostic factor for patients with solid tumor, but the association between HK2 and prognosis varies according to cancer type. Based on the above-mentioned limitations, this conclusion should be further confirmed by additional clinical studies with larger sample sizes.
Supporting Information
(TIF)
(TIF)
(DOC)
Acknowledgments
We thank our colleagues in our laboratory for methodological support and Cactus Communications Inc. (Philadelphia, PA, USA) for proofreading this manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by the Chinese Ministry of Science and Technology (973 program, 2015CB5540007), National Natural Science Foundation of China (81472740, 81101825) and Research Fund of Public Welfare in Health Industry, Health and Family Plan Committee of China (No. 201402015). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (2014) GLOBOCAN2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Available: http://globocan.iarc.fr/Default.aspx.
- 2.Maurya AK, Vinayak M. Quercetin regresses Dalton's lymphoma growth via suppression of PI3K/AKT signaling leading to upregulation of p53 and decrease in energy metabolism. Nutr Cancer. 2015;67(2):354–63. 10.1080/01635581.2015.990574 . [DOI] [PubMed] [Google Scholar]
- 3.Domenech E, Maestre C, Esteban-Martinez L, Partida D, Pascual R, Fernandez-Miranda G, et al. AMPK and PFKFB3 mediate glycolysis and survival in response to mitophagy during mitotic arrest. Nat Cell Biol. 2015;17(10):1304–16. 10.1038/ncb3231 . [DOI] [PubMed] [Google Scholar]
- 4.Chen GQ, Tang CF, Shi XK, Lin CY, Fatima S, Pan XH, et al. Halofuginone inhibits colorectal cancer growth through suppression of Akt/mTORC1 signaling and glucose metabolism. Oncotarget. 2015;6(27):24148–62. 10.18632/oncotarget.4376 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warburg O, Wind F, Negelein E. THE METABOLISM OF TUMORS IN THE BODY. J Gen Physiol. 1927;8(6):519–30. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. 10.1016/j.cell.2011.02.013 . [DOI] [PubMed] [Google Scholar]
- 7.Rivenzon-Segal D, Boldin-Adamsky S, Seger D, Seger R, Degani H. Glycolysis and glucose transporter 1 as markers of response to hormonal therapy in breast cancer. Int J Cancer. 2003;107(2):177–82. 10.1002/ijc.11387 . [DOI] [PubMed] [Google Scholar]
- 8.Mathupala SP, Rempel A, Pedersen PL. Aberrant glycolytic metabolism of cancer cells: a remarkable coordination of genetic, transcriptional, post-translational, and mutational events that lead to a critical role for type II hexokinase. J Bioenerg Biomembr. 1997;29(4):339–43. . [DOI] [PubMed] [Google Scholar]
- 9.Mathupala SP, Ko YH, Pedersen PL. Hexokinase-2 bound to mitochondria: cancer's stygian link to the "Warburg Effect" and a pivotal target for effective therapy. Semin Cancer Biol. 2009;19(1):17–24. 10.1016/j.semcancer.2008.11.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamabe A, Yamamoto H, Konno M, Uemura M, Nishimura J, Hata T, et al. Combined evaluation of hexokinase 2 and phosphorylated pyruvate dehydrogenase-E1alpha in invasive front lesions of colorectal tumors predicts cancer metabolism and patient prognosis. Cancer Sci. 2014;105(9):1100–8. 10.1111/cas.12487 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guzman G, Chennuri R, Chan A, Rea B, Quintana A, Patel R, et al. Evidence for heightened hexokinase II immunoexpression in hepatocyte dysplasia and hepatocellular carcinoma. Dig Dis Sci. 2015;60(2):420–6. 10.1007/s10620-014-3364-3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suh DH, Kim MA, Kim H, Kim MK, Kim HS, Chung HH, et al. Association of overexpression of hexokinase II with chemoresistance in epithelial ovarian cancer. Clin Exp Med. 2014;14(3):345–53. 10.1007/s10238-013-0250-9 . [DOI] [PubMed] [Google Scholar]
- 13.Ogawa H, Nagano H, Konno M, Eguchi H, Koseki J, Kawamoto K, et al. The combination of the expression of hexokinase 2 and pyruvate kinase M2 is a prognostic marker in patients with pancreatic cancer. Mol Clin Oncol. 2015;3(3):563–71. 10.3892/mco.2015.490 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peng SY, Lai PL, Pan HW, Hsiao LP, Hsu HC. Aberrant expression of the glycolytic enzymes aldolase B and type II hexokinase in hepatocellular carcinoma are predictive markers for advanced stage, early recurrence and poor prognosis. Oncol Rep. 2008;19(4):1045–53. 10.3892/or.19.4.1045 . [DOI] [PubMed] [Google Scholar]
- 15.Wolf A, Agnihotri S, Micallef J, Mukherjee J, Sabha N, Cairns R, et al. Hexokinase 2 is a key mediator of aerobic glycolysis and promotes tumor growth in human glioblastoma multiforme. J Exp Med. 2011;208(2):313–26. 10.1084/jem.20101470 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qiu MZ, Han B, Luo HY, Zhou ZW, Wang ZQ, Wang FH, et al. Expressions of hypoxia-inducible factor-1alpha and hexokinase-II in gastric adenocarcinoma: the impact on prognosis and correlation to clinicopathologic features. Tumour Biol. 2011;32(1):159–66. 10.1007/s13277-010-0109-6 . [DOI] [PubMed] [Google Scholar]
- 17.Ottawa Hospital Research Institute. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 18.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16 10.1186/1745-6215-8-16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. 10.1002/sim.1186 . [DOI] [PubMed] [Google Scholar]
- 20.Zhang ZF, Feng XS, Chen H, Duan ZJ, Wang LX, Yang D, et al. Prognostic significance of synergistic hexokinase-2 and beta2-adrenergic receptor expression in human hepatocelluar carcinoma after curative resection. BMC Gastroenterol. 2016;16(1):57 10.1186/s12876-016-0474-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo W, Qiu Z, Wang Z, Wang Q, Tan N, Chen T, et al. MiR-199a-5p is negatively associated with malignancies and regulates glycolysis and lactate production by targeting hexokinase 2 in liver cancer. Hepatology. 2015;62(4):1132–44. 10.1002/hep.27929 . [DOI] [PubMed] [Google Scholar]
- 22.Gong L, Cui Z, Chen P, Han H, Peng J, Leng X. Reduced survival of patients with hepatocellular carcinoma expressing hexokinase II. Med Oncol. 2012;29(2):909–14. 10.1007/s12032-011-9841-z . [DOI] [PubMed] [Google Scholar]
- 23.Kwee SA, Hernandez B, Chan O, Wong L. Choline Kinase Alpha and Hexokinase-2 Protein Expression in Hepatocellular Carcinoma: Association with Survival. PloS one. 2012;7(10). 10.1371/journal.pone.0046591 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paudyal B, Paudyal P, Oriuchi N, Tsushima Y, Nakajima T, Endo K. Clinical implication of glucose transport and metabolism evaluated by 18F-FDG PET in hepatocellular carcinoma. Int J Oncol. 2008;33(5):1047–54. 10.3892/ijo_00000093 . [DOI] [PubMed] [Google Scholar]
- 25.Hur H, Xuan Y, Kim YB, Lee G, Shim W, Yun J, et al. Expression of pyruvate dehydrogenase kinase-1 in gastric cancer as a potential therapeutic target. Int J Oncol. 2013;42(1):44–54. 10.3892/ijo.2012.1687 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rho M, Kim J, Chang DJ, You ML, Hee EL, Kim MA, et al. Expression of type 2 hexokinase and mitochondria-related genes in gastric carcinoma tissues and cell lines. Anticancer Res. 2007;27(1 A):251–8. . [PubMed] [Google Scholar]
- 27.Katagiri M, Karasawa H, Takagi K, Nakayama S, Yabuuchi S, Fujishima F, et al. Hexokinase 2 in colorectal cancer: a potent prognostic factor associated with glycolysis, proliferation and migration. Histol Histopathol. 2016:11799 10.14670/hh-11-799 . [DOI] [PubMed] [Google Scholar]
- 28.Ho N, Coomber BL. Hexokinase II expression is correlated with colorectal cancer prognosis. Cancer Treatment Communications. 2016;6:11–6. 10.1016/j.ctrc.2016.02.008 . [DOI] [Google Scholar]
- 29.Lyshchik A, Higashi T, Hara T, Nakamoto Y, Fujimoto K, Doi R, et al. Expression of glucose transporter-1, hexokinase-II, proliferating cell nuclear antigen and survival of patients with pancreatic cancer. Cancer Invest. 2007;25(3):154–62. 10.1080/07357900701208931 . [DOI] [PubMed] [Google Scholar]
- 30.Sato-Tadano A, Suzuki T, Amari M, Takagi K, Miki Y, Tamaki K, et al. Hexokinase II in breast carcinoma: a potent prognostic factor associated with hypoxia-inducible factor-1alpha and Ki-67. Cancer Sci. 2013;104(10):1380–8. 10.1111/cas.12238 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmieri D, Fitzgerald D, Shreeve SM, Hua E, Bronder JL, Weil RJ, et al. Analyses of resected human brain metastases of breast cancer reveal the association between up-regulation of hexokinase 2 and poor prognosis. Mol Cancer Res. 2009;7(9):1438–45. 10.1158/1541-7786.MCR-09-0234 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang MX, Hua YJ, Wang HY, Zhou L, Mai HQ, Guo X, et al. Long-term prognostic implications and therapeutic target role of hexokinase II in patients with nasopharyngeal carcinoma. Oncotarget. 2016;7(16):21287–97. 10.18632/oncotarget.7116 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang X, Liu M, Sun H, Wang F, Xie X, Chen X, et al. HK2 is a radiation resistant and independent negative prognostic factor for patients with locally advanced cervical squamous cell carcinoma. Int J Clin Exp Pathol. 2015;8(4):4054–63. . [PMC free article] [PubMed] [Google Scholar]
- 34.Tsukada H, Muramatsu T, Miyazawa M, Iida T, Ikeda M, Shida M, et al. Long Term Prognostic Implications of Expression of Glucose Transporter-1 and Hexokinase II in Patients with Stage I Uterine Leiomyosarcoma. Acta Histochem Cytochem. 2012;45(2):147–54. 10.1267/ahc.11063 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim SO, Li CW, Xia W, Lee HH, Chang SS, Shen J, et al. EGFR Signaling Enhances Aerobic Glycolysis in Triple-Negative Breast Cancer Cells to Promote Tumor Growth and Immune Escape. Cancer Res. 2016;76(5):1284–96. 10.1158/0008-5472.can-15-2478 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qin L, Tian Y, Yu Z, Shi D, Wang J, Zhang C, et al. Targeting PDK1 with dichloroacetophenone to inhibit acute myeloid leukemia (AML) cell growth. Oncotarget. 2016;7(2):1395–407. 10.18632/oncotarget.6366 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patra K, Wang Q, Bhaskar P, Miller L, Wang Z, Wheaton W, et al. Hexokinase 2 is required for tumor initiation and maintenance and its systemic deletion is therapeutic in mouse models of cancer. Cancer cell. 2013;24(2):213–28. 10.1016/j.ccr.2013.06.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pedersen PL. Warburg, me and Hexokinase 2: Multiple discoveries of key molecular events underlying one of cancers' most common phenotypes, the "Warburg Effect", i.e., elevated glycolysis in the presence of oxygen. J Bioenerg Biomembr. 2007;39(3):211–22. 10.1007/s10863-007-9094-x . [DOI] [PubMed] [Google Scholar]
- 39.Sun L, Shukair S, Naik TJ, Moazed F, Ardehali H. Glucose phosphorylation and mitochondrial binding are required for the protective effects of hexokinases I and II. Mol Cell Biol. 2008;28(3):1007–17. 10.1128/mcb.00224-07 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pastorino JG, Hoek JB. Hexokinase II: the integration of energy metabolism and control of apoptosis. Curr Med Chem. 2003;10(16):1535–51. 10.2174/0929867033457269 . [DOI] [PubMed] [Google Scholar]
- 41.Feliciano P. Hexokinase 2 required in tumors. Nature Genetics. 2013;45(9):969 . [Google Scholar]
- 42.Alemi F, Alseidi A, Scott Helton W, Rocha FG. Multidisciplinary management of locally advanced pancreatic ductal adenocarcinoma. Curr Probl Surg. 2015;52(9):362–98. 10.1067/j.cpsurg.2015.07.003 . [DOI] [PubMed] [Google Scholar]
- 43.Feig C, Gopinathan A, Neesse A, Chan DS, Cook N, Tuveson DA. The pancreas cancer microenvironment. Clin Cancer Res. 2012;18(16):4266–76. 10.1158/1078-0432.ccr-11-3114 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koong AC, Mehta VK, Le QT, Fisher GA, Terris DJ, Brown JM, et al. Pancreatic tumors show high levels of hypoxia. Int J Radiat Oncol Biol Phys. 2000;48(4):919–22. . [DOI] [PubMed] [Google Scholar]
- 45.Vazquez A, Kamphorst JJ, Markert EK, Schug ZT, Tardito S, Gottlieb E. Cancer metabolism at a glance. J Cell Sci. 2016;129(18):3367–73. 10.1242/jcs.181016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gaddis ML. Statistical methodology: IV. Analysis of variance, analysis of covariance, and multivariate analysis of variance. Acad Emerg Med. 1998;5(3):258–65. 10.1111/j.1553-2712.1998.tb02624.x . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.