Abstract
In the last decade, there have been a number of action plans published to highlight the importance of preventing osteoporosis and related fractures. In the province of Ontario Canada, the Ministry of Health provided funding for the Ontario Osteoporosis Strategy. The goal is to reduce morbidity, mortality, and costs from osteoporosis and related fractures through an integrated and comprehensive approach aimed at health promotion and disease management. This paper describes the components of the Ontario Osteoporosis Strategy and progress on implementation efforts as of March 2009. There are five main components: health promotion; bone mineral density testing, access, and quality; postfracture care; professional education; and research and evaluation. Responsibility for implementation of the initiatives within the components is shared across a number of professional and patient organizations and academic teaching hospitals with osteoporosis researchers. The lessons learned from each phase of the development, implementation, and evaluation of the Ontario Osteoporosis Strategy provides a tremendous opportunity to inform other jurisdictions embarking on implementing similar large-scale bone health initiatives.
Keywords: Fracture prevention, Health policy, Osteoporosis, Population health
Introduction
Osteoporosis and related fractures are a major health problem among older populations, particularly in developed nations, and impose a considerable financial burden on health care systems [1, 2]. To highlight these issues for policy-makers in both Europe and the USA, action plans to improve bone health have been disseminated [2, 3]. This paper goes one step further by describing the implementation of an Osteoporosis Action Plan in the province of Ontario, Canada. While there has been a decline in the incidence of hip and wrist fractures associated with increases in bone density testing and treatment with antiresorptive medications, there remains an estimated 20,000 hip and wrist fractures each year in Ontario, Canada’s most populous province with approximately 12 million inhabitants [4]. In October 2000, the Ontario Women’s Health Council submitted to the Minister of Health and Long-Term Care the report of the Strategic Action Working Group on Osteoporosis “A Framework and Strategy for the Prevention and Management of Osteoporosis.” An Osteoporosis Action Plan Committee was established in May 2002, comprising government and external experts to develop specific, feasible recommendations for actions to advance osteoporosis prevention and care. Their recommendations outlined in the February 2003 “Osteoporosis Action Plan: An Osteoporosis Strategy for Ontario” resulted in the launching of the Ontario Osteoporosis Strategy, a population-based initiative to improve quality of care for osteoporosis in Ontario, Canada in 2005. The Ontario Osteoporosis Strategy is one of the initiatives of the Ontario Chronic Disease Prevention and Management Strategy and is funded by the Ontario Ministry of Health and Long-Term Care. The initial investment was $5 million annually (CDN) (http://ogov.newswire.ca/ontario/GPOE/2005/02/22/c6912.html?lmatch=&lang=_e.html). Details on cost-effectiveness cannot be provided because these are internal government documents and not publicly available.
The overall goal of the Ontario Osteoporosis Strategy is to reduce morbidity, mortality, and costs from osteoporosis and related fractures through an integrated and comprehensive approach aimed at health promotion and disease management. A comprehensive strategy will help raise public awareness, change the knowledge, attitudes and behaviors of both the public and health professionals and improve prevention and treatment programs. This paper describes the components of the Ontario Osteoporosis Strategy and progress on implementation efforts as of March 2009.
Overview of the Ontario Osteoporosis Strategy
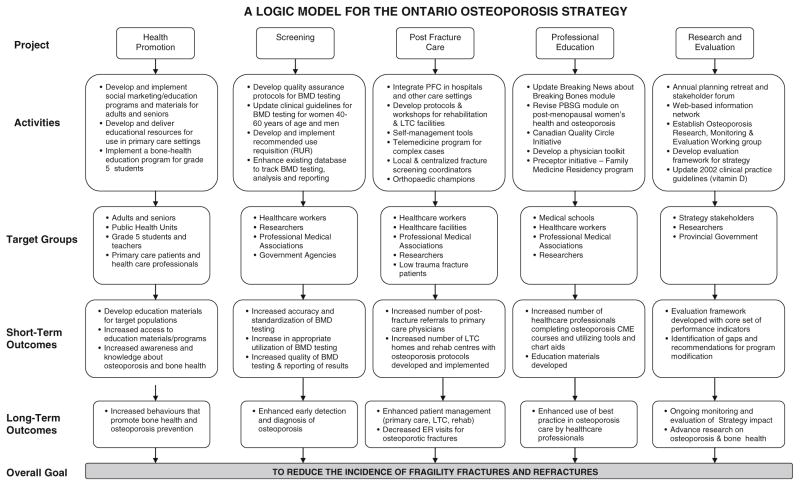
The Ontario Osteoporosis Strategy has five main components: health promotion; bone mineral density testing, access, and quality; postfracture care; professional education; and research and evaluation. The logic model (Fig. 1) provides details on the components of the strategy and short-and long-term outcomes. The website www.osteostrategy.on.ca houses materials developed to date for each component of the strategy. The Ontario Osteoporosis Strategy is centrally coordinated by the Provincial Programs: Acute Services and Chronic Disease Unit of the Ministry of Health and Long-term Care. Responsibility for implementation of the initiatives within the components is shared across a number of professional and patient organizations and academic teaching hospitals with osteoporosis researchers.
Fig. 1.
Logic model for the Ontario Osteoporosis Strategy
Component 1: health promotion
Health promotion and public education are being provided to promote bone health, reduce the risk of osteoporosis (primary prevention), and increase early detection and management. This component focuses on those at increased risk for osteoporosis: the elderly, postmenopausal women, and children and adolescents in the critical period of bone growth and development. Short-term goals for this component are to develop educational materials for target populations, increase access to educational materials and programs, and increase awareness and knowledge about osteoporosis and bone health.
Osteoporosis Canada developed the “Break Through” education program, which provides participants with interactive information about bone health and identifies strategies for reducing their risk of osteoporosis, falls and further bone loss. Resources include print media, DVDs, television advertisements and public service announcements, a website, and a virtual patient network with a toll-free number run by volunteers to provide evidence-based information on osteoporosis care and management. Patient education materials for use in the primary care setting were also developed and/or updated and disseminated to physicians. Resources are now being developed for community pharmacists. A key aspect of the health promotion component is the hiring of 13 Area Managers who are responsible for disseminating information in communities across their region by building relationships with community groups, health care providers, and institutions to increase awareness about osteoporosis and its risk factors in the community. Area Managers are typically middle/senior management level individuals with formal training in social sciences and/or health care and bring to the position considerable experience in managing and implementing programs in their communities. The Area Managers are also responsible for implementing and integrating Strategy projects within existing community/regional programs and initiatives and ensuring that care gaps are identified and addressed.
Among children and adolescents, grade 5 students (10–11 years old) in Ontario have been targeted for an educational intervention. They receive the Power4Bones program developed by the Dairy Farmers of Canada. Program materials include: complete teacher guide and weekly instructional envelopes; ID badges for online components including comics, web challenges, and public service announcement development; trivia-action based board game; and participation prizes for each student. As this was an already established program, wide-scale implementation began in January 2005. Feedback from student and teacher evaluations indicate that key learnings and behavior changes were retained by students, and the program is well received.
The Power4Bones program was developed before the Osteoporosis Strategy was implemented in response to research findings that indicated that children in Ontario were not eating well enough and were not active enough to build strong bones. The program was piloted in 2004 and implemented in 2005. Grade 5 students were targeted since they are on the cusp of a crucial bone-building and critical growth period of life (ages 11–14 for girls and 13–17 for boys) and could help facilitate developing healthy bone-building behaviors.
Component 2: bone mineral density testing, access, and quality
The short-term goals of the bone mineral density (BMD) component of the Strategy are to increase quality of BMD testing and reporting at all sites and appropriate utilization of BMD testing. In Ontario, the number of BMD tests has increased steadily from about 37,000 in 1992 to over 400,000 tests in 2001; the group most likely to have a BMD test is women between the ages of 55 and 69 years [4]. What is not known from these data is the proportion of women with a new fracture who received a BMD test. There is evidence to suggest internationally that this high-risk group is not receiving adequate osteoporosis and fracture management [5, 6]. There is strong evidence that treatment of women at high risk for fracture will decrease risk and subsequent fractures [1].
There are a number of initiatives within this component that have recently been funded by the Strategy. The Ontario Association of Radiologists is implementing a Canadian BMD Facility Accreditation Program based on one developed by the Canadian Association of Radiologists [7]. This program has been designed to evaluate personnel qualifications, equipment performance, and effectiveness of quality control measures. The program is based on a set of recommendations for optimal BMD reporting in postmenopausal women and older men. It complements the standards developed by the Canadian Panel of the International Society for Clinical Densitometry establishing the minimum requirements for acceptable performance of BMD testing in Canada. Two continuing medical education events in April and October 2007 promoted the accreditation program, and pilot testing of the program began in 2008.
To increase appropriate utilization of BMD testing, researchers from the Multidisciplinary Osteoporosis Program at Women’s College Hospital are finalizing a Recommended Use Requisition form for BMD testing. The requisition will incorporate assessment of fracture risk and a decision algorithm for referral for testing based on existing guidelines and the recently published systematic reviews on risk factors for BMD for peri-menopausal women [8] and men [9]. Another more recent initiative of the Strategy is the development of an Ontario BMD Program of which one priority is the development and implementation of a common dual xray absorptiometry (DXA) reporting system. These reports would incorporate clinical risk factors, DXA scanner identifiers (e.g., name of machine and software), provide both t-score and z-scores, an absolute fracture risk, and a statement about treatment suggestions to decrease ambiguity.
Funding has also been received in 2009 to develop a proposal for a population-based database to allow prospective analysis of the utilization and appropriateness of BMD testing across the province; currently, the only data available on BMD testing at the population level is whether or not the patient had the test.
Component 3: postfracture care
The presence of a low trauma fracture is a significant risk factor for predicting future fracture; with about 50% of all surviving men and women experiencing a subsequent fracture in 10 years [10]. Despite this, the literature summarizing the care gap from studies conducted before the Strategy showed that less than 30% of patients with fractures are subsequently diagnosed with osteoporosis, and less than half of those receive treatment [5]. Thus, secondary fracture prevention is a major focus of the Strategy with a number of interrelated initiatives designed to reduce the risk of refracture and to increase referrals to primary care physicians for assessment and treatment of osteoporosis.
Fracture clinic screening program
A province-wide Fracture Clinic Screening Program has been implemented in medium- and high-volume fracture clinics based on the Osteoporosis Exemplary Care Program developed by Bogoch et al. [11]. This program was designed to identify, investigate, and appropriately treat all orthopedic outpatients and inpatients who presented to the hospital with a fragility fracture of the wrist, shoulder, hip, or vertebra. The short-term goals were: (1) to develop awareness by hospital staff regarding the importance of identifying patients with a fragility fracture and their need for referral, evaluation, and possible treatment; (2) to increase identification and referral rates of patients with a fragility fracture; (3) to develop awareness by patients that the fracture may have been caused by an underlying bone disease; and (4) to enhance patient knowledge regarding osteoporosis and its management. The Screening Coordinators conduct an osteoporosis assessment review, provide osteoporosis education, refer low trauma fracture patients 50 years and older to their family physician for follow-up, and send a letter to the patient’s family physician recommending that the patient be assessed for osteoporosis. There are currently 19 Screening Coordinators working at 36 high- and medium-volume fracture clinics throughout Ontario.
Postfracture care initiatives for rural and remote communities
Smaller volume hospitals treat approximately 30% of low trauma fracture patients (approximately 13,400/year) across 122 hospitals. To meet the needs of these communities, the Strategy provides access to a Multidisciplinary Telehealth Osteoporosis Clinic and is testing a centralized coordinator model in a cluster randomized trial. One of the teaching hospitals with a multidisciplinary osteoporosis clinic provides osteoporosis care via videoconferencing through the Ontario Telemedicine Network to individuals in smaller communities throughout Ontario. The target population is complex osteoporosis patients, and a description of this initiative has been published [12, 13].
The Regional Osteoporosis Coordinator Knowledge Exchange Trial enrolled 36 sites and 289 patients to compare simple fall prevention advice (control) to a multifaceted osteoporosis intervention. Data collection was completed in July 2009. It will determine if a centralized coordinator who identifies patients from emergency department records, provides telephone advice, and sends a letter to their primary care physicians with evidence-based recommendations about fracture risk and osteoporosis treatment will increase the proportion of patients who receive appropriate investigation and treatment for osteoporosis in smaller communities.
Postfracture care initiatives for rehabilitation units and nursing homes
The goal of postfracture care initiatives in nursing homes and rehabilitations units is to integrate osteoporosis assessment and management into the existing services provided to patients postfracture. Conventional rehabilitation protocols frequently do not make the link between fractures and osteoporosis and therefore lack osteoporosis assessment and management interventions. To address this need, the Osteoporosis Strategy funded the Fracture Fighters Program (www.fracturefighters.ca) in 2007. Thirty-six hospitals with inpatient rehabilitation units that treated at least 40 hip fractures per year participated. Two clinical coaches (nurse and rehabilitation therapist) were identified from each unit and attended a 1-day training session which included education on osteoporosis best practices, change management strategies, and the distribution of resource materials (website, booklets, posters, audit checklists). Telephone support and an audit process were also implemented. The clinical coach was a resource person for the other health care professionals. Each site was expected to provide education about osteoporosis to fracture patients and hand out patient booklets, encourage use of calcium and vitamin D supplements, send a letter to the patient’s family physician about following up for osteoporosis, and making a referral for bone mineral density testing if available onsite.
The nursing home component of the Strategy involves working with the Long-Term Care Sector to promote and implement evidence-based osteoporosis and fracture prevention care strategies through educating staff, promoting greater awareness, and evidence-informed care decisions regarding osteoporosis, increasing fall and fracture prevention, and developing user-friendly and appropriate resources. To date, a number of dissemination strategies including webinars and written material have been developed. A survey of current practices in management of osteoporosis in the long term has recently been published [14]. A survey of both physicians’ and nurses’ beliefs and attitudes in osteoporosis and fracture care and a scoping review have been completed on interventions that reduce the risk of fractures and falls in nursing homes.
Component 4: professional education
The goal of the professional education component of the Strategy is to improve medical professionals’ utilization of clinical practice guidelines. To achieve this, the Ontario College of Family Physicians (OCFP) developed three evidence-based education modules (Male Osteoporosis, Osteoporosis and Fragility Fractures, and Post-Menopausal Women—Health Promotion and Disease Prevention) and a practice toolkit. The toolkit includes a one-page flow sheet to help family physicians assess and manage patients over age 50 at risk of osteoporosis and fracture, chart for assessment, counseling tips and references, and an algorithm for patient screening. Continuing medical education (CME)-accredited workshops led by trained peer facilitators are also currently being offered for physicians. To increase the number of healthcare professionals completing osteoporosis CME courses and utilizing tools and chart aids, the OCFP is partnering with McMaster University’s Division of e-Learning Innovation to develop e-learning content that will be disseminated through a continuing medical education portal.
Component 5: research and evaluation
An Osteoporosis Research, Monitoring and Evaluation Work Group (ORMEW) was formed in 2006 with representation from the Ministry of Health and all Strategy-funded projects. The mandate of the working group is to evaluate the impact of the Strategy in improving osteoporosis prevention and treatment in Ontario. ORMEW was responsible for developing a monitoring and evaluation framework that outlines a core set of performance indicators, data elements, data collection methodology, and protocols for reporting. The first step in this process involved systematically reviewing the literature on quality of care for osteoporosis, with particular attention to indicators and measurements that have been suggested or previously used in quality improvement initiatives [15–20]. The results of this systematic review were tabulated and summarized and distributed to an expert panel. Standard consensus methods were used to develop a core set of quality indicators based on their importance and validity. We are in the process of finalizing the indicators and their data sources.
Conclusions
The Ontario Osteoporosis Strategy is an Osteoporosis Action Plan that is being implemented at a population-based level. It is important to note that this was made possible by the endorsement and financial support of the provincial health ministry in Ontario, which recognized that osteoporosis and related fractures are a major healthcare priority. Components of this model are potentially applicable in other countries with the caveat that it would need to be tailored to the unique needs of each jurisdiction and health care system. The lessons learned from each phase of the development, implementation, and evaluation of the Ontario Osteoporosis Strategy provides a tremendous opportunity to inform other jurisdictions embarking on implementing similar large-scale bone health initiatives.
Acknowledgments
We would like to thank the Ministry of Health in Ontario for their support of the Ontario Osteoporosis Strategy. Dr. Susan Jaglal holds the Toronto Rehabilitation Institute Chair at the University of Toronto. Dr. Gillian Hawker holds the F.M. Hill Chair in Academic Women’s Medicine. Dr. Alexandra Papiaoannou holds the Eli Lilly Canada Research Chair in Osteoporosis.
Footnotes
Conflicts of interest None.
Contributor Information
S. B. Jaglal, Department of Physical Therapy, University of Toronto, 160-500 University Ave, Toronto, ON M5G 1V7, Canada
G. Hawker, Medicine and Rheumatology, Women’s College Hospital and University of Toronto, 76 Grenville St, Room 815, Toronto, ON M5S 1B2, Canada
C. Cameron, Department of Physical Therapy, University of Toronto, 160-500 University Ave, Toronto, ON M5G 1V7, Canada
J. Canavan, Negotiations and Accountability Management Division/Acute Services and Chronic Disease Unit, Ontario Ministry of Health and Long-Term Care, 1075 Bay St. Suite 601, Toronto, ON M5S 2B1, Canada
D. Beaton, Mobility Program Clinical Research Unit, Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, 30 Bond Street, Toronto, ON M5B 1WB, Canada
E. Bogoch, Mobility Program Clinical Research Unit, Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, 55 Queen St. E, Suite 800, Toronto, ON M5C 1R6, Canada
R. Jain, Ontario Osteoporosis Strategy, Osteoporosis Canada, 1090 Don Mills Rd, Suite 310, Toronto, ON M3C 3R6, Canada
A. Papaioannou, Division of Geriatrics/Department of Medicine, McMaster University, 563 Sanatorium Rd, Building 74, Hamilton, ON L9C 7N4, Canada
References
- 1.Curtis JR, Adachi JD, Saag KG. Bridging the osteoporosis quality chasm. J Bone Min Res. 2009;24:3–7. doi: 10.1359/jbmr.081116. [DOI] [PubMed] [Google Scholar]
- 2.Compston J. Action plan for the prevention of osteoporotic fractures in the European Community. Osteoporos Int. 2004;15:259–262. doi: 10.1007/s00198-004-1605-6. [DOI] [PubMed] [Google Scholar]
- 3.Raisz LG, Elderkin AL, Schargorodski L, Hart T, Waldman C, King T, Noonan AS. A call to action: developing and implementing a national action plan to improve bone health. Osteoporos Int. 2009;20:1805–1806. doi: 10.1007/s00198-009-1041-8. [DOI] [PubMed] [Google Scholar]
- 4.Jaglal SB, Weller I, Mamdami M, Hawker G, Kreder H, Jaakkimainen L, Adachi R. Population trends in bone density testing, treatment and hip and wrist fracture rates: are the hip fracture projections wrong? JBMR. 2005;20(6):898–905. doi: 10.1359/JBMR.041231. [DOI] [PubMed] [Google Scholar]
- 5.Giangregorio L, Papaioannou A, Crraney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006;35:293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Papaioannou A, Kennedy CC, Ioannidis G, Gao Y, Sawka AM, Goltzman D, Tenenhouse A, Pickard L, Olszynski WP, Davison KS, Kaiser S, Josse RG, Kreiger N, Hanley DA, Prior JC, Brown JP, Anastassiades T, Adachi JD CaMos Research Group. The osteoporosis care gap in men with fragility fractures: the Canadian Multicentre Osteoporosis Study. Osteoporos Int. 2008;19(4):581–587. doi: 10.1007/s00198-007-0483-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siminoski K, Leslie WD, Frame H, Hodsman A, Josse RG, Khan A, Lentle BC, Levesque J, Lyons DJ, Tarulli G, Brown J. Recommendations for bone mineral density reporting in Canada. Can Assoc Rad J. 2005;56:178–188. [PubMed] [Google Scholar]
- 8.Waugh EJ, Lam MA, Hawker GA, McGowan J, Papaioannou A, Cheung AM, Hodsman AB, Leslie WD, Siminoski K, Jamal SA, Perimenopause BMD Guidelines Subcommittee of Osteoporosis Canada. Risk factors for low bone mass in healthy 40–60 year old women: a systematic review of the literature. Osteoporos Int. 2009;20(1):1–21. doi: 10.1007/s00198-008-0643-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papaioannou A, Kennedy CC, Cranney A, Hawker G, Brown JP, Kaiser SM, Leslie WD, O’Brien CJM, Sawka AM, Khan A, Siminoski K, Tarulli G, Webster D, McGowan J, Adachi JD. Risk factors for low BMD in healthy men age 50 years or older: a systematic review. Osteopor Int. 2009;20(4):507–518. doi: 10.1007/s00198-008-0720-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007;297(4):387–394. doi: 10.1001/jama.297.4.387. [DOI] [PubMed] [Google Scholar]
- 11.Bogoch ER, Elliot-Gibson V, Beaton DE, Jamal SA, Josse RG, Murray TM. Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. J Bone Joint Surg Am. 2006;88(1):25–34. doi: 10.2106/JBJS.E.00198. [DOI] [PubMed] [Google Scholar]
- 12.Dickson L, Cameron C, Hawker G, Ratansi A, Radziunas I, Bansod V, Jaglal S. Development of a multidisciplinary osteoporosis telehealth program. Telemed e-Health. 2008;14(5):473–478. doi: 10.1089/tmj.2007.0079. [DOI] [PubMed] [Google Scholar]
- 13.Jaglal SB, Hawker G, Bansod V, Salbach NM, Zwarenstein M, Carroll J, Brooks D, Cameron C, Bogoch E, Jaakkimainen L, Kreder H. A demonstration project of a multi-component educational intervention to improve integrated post-fracture osteoporosis care in five rural communities in Ontario, Canada. Osteoporos Int. 2009;20(2):265–274. doi: 10.1007/s00198-008-0654-7. [DOI] [PubMed] [Google Scholar]
- 14.Giangregorio LM, Jantzi M, Papaioannou A, Hirdes J, Maxwell CJ, Poss JW. Osteoporosis management among residents living in long-term care. Osteoporos Int. 2009;20(9):1471–1478. doi: 10.1007/s00198-009-0837-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ACOVE Quality Indicators. Ann Intern Med. 2001;135:653–667. doi: 10.7326/0003-4819-135-8_part_2-200110161-00004. [DOI] [PubMed] [Google Scholar]
- 16.Grossman JM, MacLean CH. Quality indicators for the management of osteoporosis in vulnerable elders. Ann Intern Med. 2001;135:722–730. doi: 10.7326/0003-4819-135-8_part_2-200110161-00011. [DOI] [PubMed] [Google Scholar]
- 17.McKinley ED, Thompson JW, Briefer-French J, Wilcox LS, Weisman CS, Andrews WC. Performance indicators in women’s health: incorporating women’s health in the health plan employer data and information set (HEDIS) Women’s Health Issues. 2001;2(1):46–58. doi: 10.1016/s1049-3867(01)00120-7. [DOI] [PubMed] [Google Scholar]
- 18.National Committee for Quality Assurance (NCQA) Health plan employer data and information set. Vol. 2, technical specifications. National Committee for Quality Assurance (NCQA); Washington DC: 2005. HEDIS 2006; p. 350. [Google Scholar]
- 19.National Quality Forum. [accessed October 29, 2009]; www.qualityforum.org.
- 20.Rubenstein LZ, Powers CM, MacLean CH. Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders. Ann Intern Med. 2001;135:686–693. doi: 10.7326/0003-4819-135-8_part_2-200110161-00007. [DOI] [PubMed] [Google Scholar]