Abstract
Objective
To explore the perceptions of patients who have sustained a fragility fracture regarding their future fracture risk and the beliefs underlying their perceptions.
Methods
Patients with fragility fracture participated in a telephone interview. Quantitative and qualitative methods were used to characterize patient characteristics and perspectives of future fracture risk. Content analysis of qualitative statements was independently performed by three investigators to identify common themes and contrasting statements, and the findings were discussed to ensure consensus.
Results
Consistent themes were identified among participant responses irrespective of whether they responded “yes”, “no” or “unsure” when asked whether they were at increased fracture risk: (1) patients’ perception of risk was influenced by whether or not they believed they had osteoporosis, which may be altered by interaction with health care providers; (2) patients’ had their own perceptions of their bone health; (3) patients’ attributed their risk to their own actions or “carefulness”; and (4) patients’ had specific beliefs about their fracture and determinants of fracture risk.
Conclusion
Patients who experience fragility fractures develop perceptions about future fracture risk that are influenced by interactions with health care providers, as well as beliefs about their fracture and beliefs that they can modify their risk.
Practice implications
Health care providers should discuss strategies for fracture prevention with all patients after fragility fracture to ensure that patients understand that participation in preventative behaviours can modify their risk.
Keywords: Osteoporosis, Fracture, Perception of risk
1. Introduction
Osteoporosis is a disease characterized by compromised bone strength and an increased risk of fragility fracture. A fragility fracture is a fracture that occurs with minimal trauma, such as a fall from a standing height or less [1]. Fragility fractures can reduce quality of life, increase fear of falling, and often result in impaired mobility and a loss of independence [2–4]. Effective therapeutic options for fracture prevention are available [1]. For example, the relative risk of fracture associated with bisphosphonate use compared with placebo in women with osteoporosis is 0.47 (95% confidence intervals 0.26–0.79) for hip fractures, 0.52 (0.42–0.66) for radiographic vertebral fractures and 0.70 (0.59–0.82) for all clinical fractures [5]. Therefore, it is essential that individuals who experience fragility fracture be aware that they are at increased risk for a subsequent fracture and be made aware of available osteoporosis management options, including bone mineral density testing, pharmacological therapies and non-pharmacological prevention strategies [6]. However, individuals over the age of 40 years with fragility fracture are not receiving appropriate osteoporosis management [7,8]. It is unknown whether poor management of fragility fractures is due to physicians not treating the condition or due to patients not perceiving themselves at risk and being willing to accept treatment.
Individuals who suffer a fragility fracture need to be aware of the link between their fractures and osteoporosis, so that they can actively participate in fracture prevention strategies, such as adequate nutrition, exercise and pharmaceutical management, if necessary [9]. In-depth interviews reveal that many patients with fragility fracture had not associated their fracture with bone fragility. Instead they attributed their fractures to external factors, such as a fall, or slipping on ice [10–12]. With a chronic disease such as osteoporosis, patient self-management is an important element in effective long-term management, especially with self-care issues such as adequate calcium and vitamin D intakes, fall prevention and exercise [13]. The chronic care model, in which patient self-management is one of the six components, has been shown to be associated with reduced health care costs and less use of health care services [14]. Adherence to osteoporosis therapies is poor, and the reasons for poor adherence to therapies are not well understood [15]. It has been suggested that perceived susceptibility may influence acceptance of osteoporosis therapy [9]. Therefore, it is essential that patients understand that having a fragility fracture increases their risk for subsequent fractures, and that preventative action may be necessary.
Although previous studies have evaluated osteoporosis risk perceptions among peri- and postmenopausal women, it is not known whether patients with fragility fracture understand that they are at increased risk of future fracture, regardless of whether they have osteoporosis based a on bone mineral density test [10,11,16]. Further, no study has specifically explored the perspectives of fragility fracture patients who do and do not perceive themselves to be at risk of fracture, and the beliefs underlying those perceptions. The purpose of the current study was to explore the fragility fracture patient’s perceptions of future fracture risk.
2. Methods
2.1. Study sample
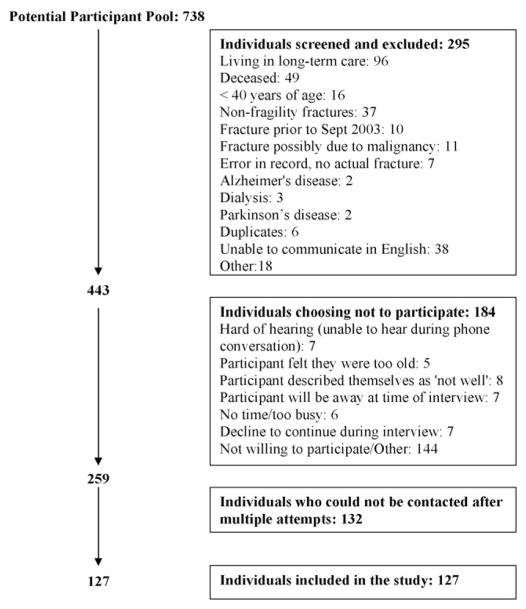
Males and females who were treated for a fragility fracture by orthopaedic surgeons at two major teaching hospital fracture clinics were recruited to participate. Fractures had to occur at the radius, humerus, femur, rib, tibia (in females only), pelvis or vertebrae to be considered a possible osteoporotic fragility fracture [17]. All patients who had sustained a fracture at specified sites were identified by orthopaedic surgeons’ records. Letters were sent to patients from their physicians requesting their participation in the study. All patients received a follow-up telephone call to confirm whether they were interested in participating. Participants were considered eligible for inclusion in the study if they were 40 years of age or older and if they had experienced a fragility fracture within 24 months of the interview date. Interviews were conducted from September 2005 to June 2006. Exclusion criteria were as follows: fractures of the hands, feet, skull, clavicle, ankle or the tibia in males; fracture due to malignancy; non-fragility fractures; not living in the community; not able to communicate in English; on dialysis; unable to complete interview due to memory loss, dementia, other medical reasons and fracture >2 years prior to avoid problems with recall (Fig. 1). Patients were also asked to describe the incident in which the fracture occurred to verify whether the fracture was a fragility fracture. A fracture occurring in any event that was not a fall from standing height or similar non-traumatic event was reviewed by at least three physicians among the research team and a decision was made whether to include or exclude the fracture. The study received approval by the Hamilton Health Sciences Research Ethics Board and the St. Joseph’s Healthcare Research Ethics Board.
Fig. 1.
Flow diagram of participant recruitment and inclusion/exclusion.
2.2. Design
This was a descriptive study that used qualitative and quantitative methods for data collection. A telephone interview was conducted with individuals who agreed to participate using a survey instrument developed and pilot-tested for this study by the research team. Interview data were gathered using a Computer Assisted Telephone Interviewing (CATI) system. Each interview was performed by one of two interviewers who were trained to use prompts to probe for responses. The aim of the process was to improve the richness of data collected and reduce the amount of missing data. All responses were directly entered into a computer database during the interview, and questions appeared sequentially so that the interview could not continue until a response was entered for each question. The interview contained structured questions about the following: socio-demographic information; prescription medication use in the past year (including treatments for osteoporosis, calcium and vitamin D supplementation); medical and fracture history; family history of osteoporosis; and participation in osteoporosis preventative activities (e.g. exercise, intake of calcium rich foods, fall prevention). Participants’ perceptions of risk were determined by asking “Do you think that breaking your [insert fracture site] means that you are at increased risk for breaking a bone in the future?” and “Do you think your fracture was related to osteoporosis?” Open-ended questioning was used to discern why the patients did or did not perceive themselves to be at risk of future fracture. The patients’ qualitative comments about their perceptions of risk were also recorded using the CATI system.
2.3. Analyses
Three members of the research team independently analyzed the complete set of patients’ qualitative statements. A content analysis approach was used to extract recurrent themes across interviews. Data were coded and like elements were extracted from the text into broad groupings. Common themes and contrasting statements were identified and then discussed to ensure there was consensus [18]. Data from quantitative analyses were used to categorize participants as having either: less than 3 osteoporosis risk factors, or 3 or more osteoporosis risk factors, to determine if statements were different among patients with fewer than 3 compared to those with 3 or more risk factors. The following risk factors were chosen based on previous research [1] and consensus among the research team regarding clinical factors that increase risk of future fractures: age greater than 65 years, family history of hip, wrist or spine fracture, self-reported osteoporosis diagnosis, 3 or more falls in the past year, oral glucocorticoid use (past or current), or premature menopause. In addition, participants were characterized based on self-reported osteoporosis diagnosis (yes/no/unsure) to determine if statements or emerging themes were different among participants with and without a diagnosis. The Health Behaviour Change Model was used to guide the analysis and interpretation of results [19]. Descriptive statistics for demographic and clinical participant characteristics are presented as mean (standard deviation [S.D.]) for continuous variables or count (percent) for categorical variables. These analyses were performed with SPSS (version 14).
3. Results
3.1. Sample
The response rate for the telephone interview was 29% (Fig. 1) with 127 participants responding. The mean (S.D.) age of the entire cohort approached (N = 738) was 71.8 years (16.3), where 73.3% were female. Demographic characteristics of the 127 participants are listed in Table 1. A history of a previous fracture after the age of 40 years was reported by 51 (40%) participants, including 16 wrist, 2 hip, 2 pelvis, 2 spine, 6 humerus, 6 ankle and 25 fractures reported at other sites. A diagnosis of osteoporosis was reported in 56 (44%) participants. Among those with an osteoporosis diagnosis, 45 (80%) were diagnosed before the index fracture. Use of at least one medication, not including supplements, for osteoporosis was reported in 54 (43%) respondents. Current and past use of oral corticosteroids was reported in 4 (3%) and 17 (13%) participants, respectively, current and past use of inhaled corticosteroids was reported in 1 (1%) and 2 (2%) participants, and 2 (2%) participants reported past use of corticosteroids but were unsure whether they were oral or inhaled.
Table 1.
Participant characteristics.
| Total number of participants | 127 |
| Age in years (S.D.) | 67.5 (12.7) |
| Number of females: n (%) | 106 (82) |
| Menopausal status (females): n (%) | |
| Pre-menopausal | 4 (3.1) |
| Peri-menopausal | 3 (2.3) |
| Post-menopausal | 95 (74.8) |
| Unsure | 3 (2.3) |
| Site of index fracture: n (%) | |
| Wrist | 72 (56.7) |
| Hip | 26 (20.5) |
| Other femur fracture | 10 (7.9) |
| Humerus | 5 (3.9) |
| Spine | 1 (0.8) |
| Pelvis | 1 (0.8) |
| Elbow | 12 (9.4) |
| Cause of fracture: n (%) | |
| Fall from standing height | 75 (59.1) |
| Twisting | 3 (2.4) |
| Slipping on ice | 37 (29.1) |
| Ice skating | 3 (2.4) |
| Re-fracture | 1 (0.8) |
| Fall from standing height while running | 2 (1.6) |
| Hit it on something | 2 (1.6) |
| Unsure | 1 (0.8) |
| Spontaneous | 3 (2.4) |
| Average time post-fracture in months (S.D.) | 11.2 (6.3) |
| History of previous fracture: n (%) | 51 (40.2) |
| Family history of fracture: n (%) | 28 (21.7) |
| Self-reported height loss: n (%) | 67 (51.9) |
| At least one fall in the past yeara: n (%) | 103 (81.1) |
| 3 or more falls in the past year: n (%) | 13 (10.1) |
| Use assistive aid for mobility (cane, crutches, walker, wheelchair): n (%) | 45 (35.4) |
| 4 or more prescription medications: n (%) | 53 (41.1) |
| Mean number of prescription medications: Mean (S.D.) | 3.7 (3.3) |
| Marital status: n (%) | |
| Single | 7 (5.4) |
| Married | 67 (52.8) |
| Widowed | 34 (26.4) |
| Divorced/Separated | 19 (14.7) |
| Living arrangements: n (%) | |
| Live alone | 45 (34.9) |
| Live with others | 82 (64.6) |
If the respondent’s fracture was due to a fall, this fall was included in the total.
3.2. Respondent assessment of future fracture risk
The responses regarding future fracture risk in this sample of respondents who had suffered a fragility fracture could be separated into three groups: 43.3% of individuals who perceived themselves to be at increased risk of future fracture, a similar percentage did not believe they were at risk of future fracture, and the remaining 15% were unsure (Table 2). Respondents’ qualitative responses revealed that even among those that responded with a definite “yes” or “no”, when asked whether why they were at increased risk of future fracture there was some uncertainty. For example, one respondent who indicated that she thought she was at risk noted,
“Well this is the first bone I have ever broken and maybe I am at risk because of my age.”
Table 2.
Perceptions of osteoporosis and fracture risk among individuals who have had a fragility fracture (n = 127).
| Response: number of respondents (%)
|
|||
|---|---|---|---|
| Yes | No | Unsure | |
| Do you think that breaking your (insert fracture site) means that you are at increased risk of breaking a bone in the future? | 55 (43.3) | 53 (41.7) | 19 (15%) |
| Do you think your fracture was related to osteoporosis? | 22 (17.3) | 68 (53.5) | 37 (29.1) |
| Have you ever been told that you have osteoporosis? | 56 (44.1) | 67 (52.8) | 4 (3.1) |
3.3. Themes
Qualitative responses revealed four consistent themes across participants who responded “yes”, “no” or “unsure” when asked whether they were at increased fracture risk (Table 3): (1) patients’ perception of risk was influenced by interactions with health care providers, independent of whether or not they believed they had osteoporosis; (2) patients’ had their own perceptions of bone health, often influenced by bone density testing; (3) patients’ attributed their risk to their own actions or “carefulness”; and (4) patients’ had specific beliefs about the fracture and the determinants of fracture risk. Patient qualitative responses and the associated themes are presented in Table 3, and are discussed in the subsections below.
Table 3.
Factors that influence fragility fracture patients’ perceptions of risk.
| Factors resulting in a perceptions of increased risk | Factors resulting in no increased perception of risk | Factors resulting in uncertainty about risk | |
|---|---|---|---|
| Belief they have a diagnosis of osteoporosis |
|
|
|
| Perceptions of own bone health |
|
|
|
| Carefulness: belief that they can modify their own fracture risk |
|
|
|
| Beliefs or awareness about cause and effect |
|
|
|
3.3.1. Theme 1: communication with health care providers about fracture risk
An overwhelming number of respondents who perceived themselves at risk of future fracture or were unsure, indicated that they thought they might be at risk because they had been given a clinical diagnosis of osteoporosis/osteopenia or told that they are at risk of fracture (Tables 3 and 4). In contrast, a number of respondents reported that communication with their physicians or other health care providers led them to believe they were not at risk of fracture, for example one patient noted:
“. . .doctor says my bones are very good and the break should never have happened.”
Table 4.
Perceptions of fracture risk among individuals who have had a fragility fracture who have or have not been given an osteoporosis diagnosis (n = 127).
| Do you think that breaking your (insert bone site) means that you are at increased risk of breaking a bone in the future? n (%)
|
|||
|---|---|---|---|
| No | Yes | Unsure | |
| Have you ever been told that you have osteoporosis? n (%) | |||
| No | 45 (35) | 8 (6) | 12 (9) |
| Yes | 14 (11) | 41 (33) | 7 (6) |
Communication with health care providers may not have sufficiently clarified fracture risk for some participants. For example, one participant reported being on an osteoporosis medication, but was not sure about her risk for future fractures (Table 3). In other words, when interpreting the data, it was evident that patients referred to a discussion with a health care provider when providing a reason for their perception of risk, and that discussion included the use of the term osteoporosis or some reference to whether the patient was at risk of fragility fractures. Table 5 illustrates that perceptions of risk were similar among those with 3 or more osteoporosis risk factors compared to those with less than three risk factors, suggesting that patients may not understand multiplicative nature of risk or that health care providers have difficulty conveying information about risk to patients. The data did not demonstrate that patients understood the concept that simply having a fragility fracture put them at increased risk of future fracture.
Table 5.
Perceptions of fracture risk among individuals who have had a fragility fracture who do or do not have 3 or more risk factors (n = 127).
| Do you think that breaking your (insert bone site) means that you are at increased risk of breaking a bone in the future? n (%)
|
|||
|---|---|---|---|
| No | Yes | Unsure | |
| Three or more risk factors | |||
| No | 42 (33) | 42 (33) | 16 (13) |
| Yes | 11 (9) | 13 (10) | 3 (2) |
3.3.2. Theme 2: patient perceptions about bone health
Many respondents mentioned their beliefs about bone health. A number of participants who indicated that they thought they were at increased risk of future fracture attributed the risk to having weak or brittle bones, often referring specifically to bone density results. Several respondents did not think they were at risk of fracture and attributed this to the fact that they had normal bone density. Many patients’ risk perceptions equated good bone density with no risk or low bone density with high risk, when in fact a determination of future fracture risk should consider clinical risk factors in addition to bone density. Providing an interpretation of future fracture risk based on bone density alone may have misled some patients to believe that they were not at risk. The first two themes are related, in that perceptions of risk were influenced by the information provided by health care providers—either a clinical diagnosis of osteoporosis and increased fracture risk or a discussion of bone density results. However, an important distinction was made between the two themes during the interpretation of the data; it became clear that some patients were simply told they did or did not have osteoporosis or increased fracture risk, and other patients’ risk was put in the context of their bone density results. The link between the two themes is that that no matter how the presence or absence of fracture risk was communicated (e.g. using a clinical diagnosis, a statement of fracture risk or through bone density results), in some instances the patients’ communication with health care providers facilitated an appropriate risk perception, and in other cases it did not.
3.3.3. Theme 3: carefulness—belief that they can modify their own fracture risk
Across all three groups (yes, no, unsure) there were respondents who attributed their risk, or lack thereof, to their own actions. During the interpretation of the data, it was evident that the word “careful” was used frequently by respondents, but was linked to different risk perceptions: some respondents reported that they did not perceive themselves to be at increased risk because they were being a lot more careful, while others reported that they did think they were at risk and were likely to break a bone if they were not more careful. Another respondent was unsure of her future fracture risk, saying:
“ . . .really do not know. I will need to be more careful.”
The patients, whether they felt susceptible to fractures or not, felt that carefulness was linked to fracture risk, suggesting that patients perceived fracture risk to be modifiable by their own actions. Consistent with this interpretation, some respondents who did not perceive themselves to be at risk attributed this to preventative actions, such as being more physically active or using an assistive device. Taken together, the data suggest that patients believe that their actions are linked to future fracture risk.
3.3.4. Theme 4: beliefs about the cause of fracture and future fracture risk
Many respondents who did not perceive themselves to be at increased risk of future fracture reported that this was their first fracture, or that the incident that caused the fracture was an accident, and would not happen again. The words “first time”, “first break”, and “freak/fluke accident” were repeated often among patient responses as a reason they were not at increased risk of future fracture, and also appeared among those who were unsure about their risk of future fracture. In contrast, several participants who said that they did perceive themselves at risk attributed their future fracture risk to osteoporosis risk factors, such as age, prednisone use, or prior or subsequent fractures. The cause and effect theme is somewhat of a cross-cutting theme; it links the three themes described above in that all reflect different factors or “causes” related to fracture risk, namely having osteoporosis, having low bone density, being careful, participating in preventative actions, or having osteoporosis risk factors. Patients seem to understand that certain factors influence fracture risk, and they define their own personal level of risk by the presence or absence of those factors. Therefore, patients for whom the “causes” are present attribute their fracture to the “causes”, and patients for whom the “causes” are absent suggest that the fracture should not have happened.
3.4. Beliefs about fracture risk among those with and without a diagnosis of osteoporosis
Participants were characterized based on self-reported osteoporosis diagnosis (yes/no/unsure) to determine if statements or emerging themes were different among participants with and without a diagnosis. Content analyses revealed that there were distinct differences in responses between the groups, and that certain themes were more evident in one group than another. Individuals who did not have an osteoporosis diagnosis often reported that they were not at risk of fracture because this was their first break, it was an accident, their doctor told them their bones are fine, or they were going to be more careful. In contrast, those with an osteoporosis diagnosis reported that they thought they were at risk because they had osteoporosis, they had broken bones before, or because their doctor had told them their bones were weak.
4. Discussion and conclusion
4.1. Discussion
The current study reveals that perceptions of future fracture risk vary among individuals who have suffered a fragility fracture, and appeared to be related to: (a) the patient’s beliefs about whether they have osteoporosis or their beliefs about the health of their bones, information that is often influenced by interactions with health care providers; (b) beliefs about whether they could modify their risk (e.g. by being careful); or (c) their beliefs about the causes of fracture or risk factors related to fracture risk. Consistent with the Health Belief Model [19], the threat of a future fracture seemed to be linked to perceived susceptibility to osteoporosis, health beliefs and health behaviours.
Communication with a health care provider was often provided as a reason why patients did or did not perceive themselves to be at increased risk for fracture. The associations made by patients between an osteoporosis diagnosis and their perceptions of fracture risk are encouraging, indicating that patients who have been diagnosed with osteoporosis understand the link between osteoporosis and future fractures. However, a number of respondents had been told by their physicians that they were not at risk, which is concerning since all respondents had sustained a fragility fracture, and a fragility fracture is an independent predictor of future fractures, even among individuals who do not have low bone density [6]. It is possible that patients did not understand whether they were at risk. A recent study revealed that the agreement between self-report and actual bone density results was poor, indicating that patients may not understand when results are conveyed to them [20]. It is also possible that many patients were not assessed for osteoporosis and therefore the fact that they may be at increased risk of fracture was not communicated to them; a recent systematic review of observational studies demonstrated that there is a gap between the occurrence of a fragility fracture and appropriate osteoporosis diagnosis and management, in that many patients are not being assessed and treated [7].
When qualitative responses from those with and without an osteoporosis diagnosis were analysed separately, it became evident that those with a diagnosis seemed to link their diagnosis with their risk for future fractures, whereas those without a diagnosis often stated that they were not at greater risk of future fractures, referring to their fracture as their first break, or to indicate that their fracture was the result of an accident. Patient responses about risk perceptions did not appear to differ among those with greater than three risk factors compared to those with less than three risk factors, suggesting that it is the diagnosis rather than the presence of risk factors that influences patient perceptions about susceptibility to fractures. We recently published data demonstrating that the odds of a fragility fracture patient perceiving themselves at increased risk for fracture were higher for those that reported a diagnosis of osteoporosis (OR 22.91 [95%CI 7.45; 70.44]), but the odds decreased with increasing age (0.95 [0.91; 0.99]) [21]. If many fragility fracture patients do not perceive themselves to be susceptible to future fracture, they may not accept or pursue strategies for fracture prevention, either pharmacological or non-pharmacological [19]. A recent study demonstrated that perceived susceptibility to fracture was related to current use of an antiresorptive medication [9]. Similarly, having a previous bone density test or diagnosis of osteoporosis were the only factors associated with active consideration of or current use of osteoporosis medication in hip fracture patients [22]. The current study reveals that communication with health care providers has an important influence on risk perceptions among fragility fracture patients. Therefore, it is necessary to address patient–physician communication to enhance perceived susceptibility to future fracture if we are to facilitate patient acceptance of intervention and self-management.
Many of the patients referred to their bone density results when speaking about their perceptions of risk, indicating that patients or their health care providers emphasize bone density as a major contributor to fracture risk. A recent study demonstrated that bone density information was associated with perceived susceptibility and acceptance of pharmacological and non-pharmacological management among women 50–65 years of age [23]. Using bone mineral density measured via dual-energy X-ray absorptiometry is currently the gold standard for the diagnosis of osteoporosis [24]. More recently, an absolute fracture risk model has been developed that includes bone density as well as clinical risk factors such as age, gender, history of fragility fracture and use of glucocorticoids when classifying fracture risk [25,26], however it is likely that many health care providers still focus on bone density results as the sole criterion for classifying fracture risk. When bone density is used to determine future fracture risk, patients are classified as normal, osteopenic or osteoporotic based on bone density alone, and only those in the osteoporotic range are considered to be at risk [27]. The new absolute fracture risk model conveys fracture risk as a 10-year probability of any type of osteoporotic fracture, and it is based on economic modeling that incorporated hip fracture risk in the US population in the calculation of cost-effective treatment thresholds [28]. According to the absolute fracture risk model, a history of fragility fracture and age have an additive effect on 10-year fracture risk by independent of bone density, so it is possible to be at high risk of future fracture even though bone density is not in the osteoporotic range. Using bone density as the sole criterion for determining fracture risk misleads physicians and patients that those that are in the osteopenic range are not risk of fractures, when in fact a large proportion of fractures occur among individuals whose bone density is in the osteopenic range [29]. Therefore, in many cases of fragility fracture a diagnosis of increased fracture risk or initiation of osteoporosis management should occur even though the patient’s bone density is not in the osteoporotic range. A key message from our study is that the health care provider’s interpretation of and communication of bone density results to the patient influences risk perceptions. It has been suggested that creating an idea of certainty about medical evidence or test results that are uncertain should be avoided to achieve good communication between health care providers and patients, and that it may be beneficial to acknowledge the uncertainties present in medical evidence [30]. For example, bone density results may be presented as a precise way to predict outcome and provide a false sense of certainty about fracture risk. Therefore, communicating the message that having a fragility fracture increases future fracture risk independent of bone density, and then providing information about risk in the context of the patient’s situation and risk factors (e.g. 10 year fracture risk) may be a better way of communicating perceived susceptibility among fragility fracture patients, and therefore facilitating decision-making regarding treatment recommendations.
Many respondents across the perceived risk categories spoke about being more “careful”; it is interesting that fragility fracture patients focused more on physical action that they thought they could take to reduce falls or accidents rather than taking medications to decrease fracture risk. It would be of interest to evaluate what steps, if any, these patients are actually taking to be “more careful” as part of their activities of daily living, or whether they received recommendations for preventing falls from their family physician. Fall prevention strategies such as home hazard risk assessment or exercise have been demonstrated to reduce falls [31]. However, it is unknown whether interventions of this nature would be accepted by fragility fracture patients. Similar to our findings, a study evaluating perceived susceptibility to osteoporosis among community-dwelling women over the age of 40 who had not been diagnosed with osteoporosis demonstrated that the majority of women perceive their risk to be lower than other women their age, and they attributed their lower risk primarily to their own preventative behaviours, such as calcium supplementation or exercise [32]. A number of individuals reported that they did not believe they were at risk of future fracture because this was the first time they had broken a bone, and the fracture was an “accident”. This finding is of great concern given that all of the respondents had a fragility fracture, which is an independent risk factor for future fractures [6]. Previous reports of patient perceptions of fracture support our finding that individuals who suffer fragility fractures attribute their fractures to external causes rather than to bone fragility [10,11]. In fact, for some patients the belief that their fracture was an accident was so strong that even subsequent fractures were attributed to external situations rather than bone fragility [10,11]. Patients’ beliefs about cause and effect was a cross-cutting theme; factors such as bone density, the presence of osteoporosis risk factors and being careful were perceived as potential “causes” of fracture, and perceptions about personal fracture risk appeared to be defined by the presence or absence of these factors. Interestingly, having a history of fragility fracture did not appear as a strong mediator of perceived susceptibility to future fractures. A study exploring the experience of hip fracture among elderly individuals revealed that patients perceive the problem of a fracture differently; some patients have a mechanistic perspective, in that they view the fall as the mechanism for their fracture, and the repair of the fracture returns them to their previous health status, whereas others view the fracture as part of a disease or illness, where treatment of the fracture does not reduce their susceptibility to future disease-related outcomes [33]. The current study is consistent with these findings, in that it reveals that although patients have a general understanding of some of the factors that influence fracture risk, their perceptions about the causes of their fracture appear to be the primary determinants of whether they believe themselves to be at increased risk of future fracture. Other studies of older women’s perceptions of osteoporosis reveal that women develop models and images of osteoporosis and what it means to be at risk, and that risk perceptions influence behaviour [12,34]; women who perceived that they were susceptible to osteoporosis were fearful of fractures and reduced their physical activity, and knowledge of low bone density reinforced the fear and uncertainty about participating in physical activity [34]. Therefore, when communicating risk to fragility fracture patients it is essential to consider differences in patient perceptions of fracture risk and reinforce appropriate preventative behaviours in the context of the patient’s model of osteoporosis and fracture susceptibility.
The current study has a few limitations. Among the potential pool of participants, 42% chose not to participate and 30% could not be contacted to determine if they were eligible. The refusal to participate may in itself be a statement on patients’ perception of osteoporosis risk; it is possible that patients who do not perceive themselves at risk would not perceive a study on osteoporosis to be personally relevant. We acknowledge that this is a potential source of responder bias. We conducted a descriptive study using both qualitative and quantitative data rather than an exclusively qualitative study [18,35]. Therefore, we did not employ conventional qualitative methods, such as in-depth one on one interviews (with a small sample) or iterative data analysis (when identifying themes) however our approach allowed us to analyze qualitative data from 127 respondents classified by their fracture risk response and so generate results less likely to be found within a smaller sample of interviewees. Further, we interviewed participants at one time point and so we are unable to comment on changes in perception of risk over time. We did not have bone density data to confirm whether all participants have osteoporosis. However, having a fragility fracture is a predictor of future fractures independent of bone density [6]. We report history of prior fracture after the age of 40, but we did not ascertain whether prior fractures were also fragility fractures. The proportion of respondents reporting a diagnosis of osteoporosis is relatively high compared to previous reports of the proportion of fragility fracture patients diagnosed with osteoporosis after fracture [7,8], suggesting that we may have over-represented individuals with diagnosed osteoporosis. However, even among our sample there were a substantial number of individuals who did not make the link between their fragility fracture and osteoporosis. Inclusion of a more representative sample may have actually increased the strength of our findings. Finally, individuals living in long-term care were excluded, and patients who had a hip fracture or were male were under-represented.
4.2. Conclusions
In summary, perceptions of future fracture risk vary substantially among individuals who have suffered a fragility fracture, and were related to the patient’s beliefs about whether they could modify their own risk and their beliefs about the causes of fracture or risk factors related to fracture risk. Patient beliefs seemed to be influenced by interactions with health care providers. Future research should investigate how to influence perceived susceptibility and health beliefs among fragility fracture patients to enhance the adoption of preventative action. Many patients referred to actions they could take to reduce their fracture risk, particularly being more careful; future research should evaluate the feasibility of implementing fall prevention programs after fragility fracture. Finally, the recurrent references to information provided by health care providers indicates that it is crucial for health care providers to deliver the message that having a fragility fracture increases the risk for future fracture independent of bone mineral density. Communication about fracture risk should include a comprehensive risk assessment that discusses risk in the context of each patient’s risk factors and considers that patients view the problem of fracture and future fracture risk differently.
4.3. Practice implications
The current study reveals that it is necessary for health care providers to ensure that fragility fracture patients understand that having a fragility fracture results in an increased risk of future fractures. Further, although some patients may already be taking steps to reduce fracture risk, health care providers should discuss strategies for fracture prevention with all patients after fragility fracture to ensure that patients understand that participation in preventative behaviours can modify their risk.
Acknowledgments
The authors would like to acknowledge financial support from The Drummond Foundation. This project was part of the “Fracture? Think Osteoporosis!” initiative at Hamilton Health Sciences. We would like to thank the orthopaedic surgeons at the Henderson Hospital and St. Joseph’s Healthcare for their assistance: Dr. Mitchell Winemaker, Dr. David Wismer, Dr. Nigel Colterjohn, Dr. Brett Dunlop, Dr. Jaydeep Moro and Dr. Arthur Porte as well as their invaluable administrative stuff. We also acknowledge the assistance of Madeline Nixon, Jennifer Ranford, Ruth McCallum, and Katherine Gaebel in the recruitment, screening and interviewing of study participants. A. Cranney had a research salary award from the Canadian Institutes of Health Research. J.D. Adachi holds the Alliance for Better Bone Health Chair in Rheumatology, funded by the Alliance of Procter & Gamble and Sanofi Aventis.
Financial Support: The Drummond Foundation.
References
- 1.Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ. 2002;167:S1–34. [PMC free article] [PubMed] [Google Scholar]
- 2.Petrella RJ, Payne M, Myers A, Overend T, Chesworth B. Physical function and fear of falling after hip fracture rehabilitation in the elderly. Am J Phys Med Rehabil. 2000;79:154–60. doi: 10.1097/00002060-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Adachi JD, Loannidis G, Berger C, Joseph L, Papaioannou A, Pickard L, Papadimitropoulos EA, Hopman W, Poliquin S, Prior JC, Hanley DA, Olszynski WP, Anastassiades T, Brown JP, Murray T, Jackson SA, Tenenhouse A. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int. 2001;12:903–8. doi: 10.1007/s001980170017. [DOI] [PubMed] [Google Scholar]
- 4.Papaioannou A, Watts NB, Kendler DL, Yuen CK, Adachi JD, Ferko N. Diagnosis and management of vertebral fractures in elderly adults. Am J Med. 2002;113:220–8. doi: 10.1016/s0002-9343(02)01190-7. [DOI] [PubMed] [Google Scholar]
- 5.Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR. Fracture risk reduction with alendronate in women with osteoporosis: the fracture intervention trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85:4118–24. doi: 10.1210/jcem.85.11.6953. [DOI] [PubMed] [Google Scholar]
- 6.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–82. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 7.Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD. Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum. 2006;35:293–305. doi: 10.1016/j.semarthrit.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Papaioannou A, Giangregorio L, Kvern B, Boulos P, Ioannidis G, Adachi JD. The osteoporosis care gap in Canada. BMC Musculoskelet Disord. 2004;5:11. doi: 10.1186/1471-2474-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cline RR, Farley JF, Hansen RA, Schommer JC. Osteoporosis beliefs and anti-resorptive medication use. Maturitas. 2005;50:196–208. doi: 10.1016/j.maturitas.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Meadows LM, Mrkonjic LA, Lagendyk LE, Petersen KM. After the fall: women’s views of fractures in relation to bone health at midlife. Women Health. 2004;39:47–62. doi: 10.1300/J013v39n02_04. [DOI] [PubMed] [Google Scholar]
- 11.Meadows LM, Mrkonjic LA. Breaking—bad news: women’s experiences of fractures at midlife. Can J Public Health. 2003;94:427–30. doi: 10.1007/BF03405079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reventlow S, Bang H. Brittle bones: ageing or threat of disease exploring women’s cultural models of osteoporosis. Scand J Public Health. 2006;34:320–6. doi: 10.1080/14034940500327869. [DOI] [PubMed] [Google Scholar]
- 13.Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119:239–43. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model. Part 2 J Am Med Assoc. 2002;288:1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 15.Silverman S. Adherence to medications for the treatment of osteoporosis. Rheum Dis Clin North Am. 2006;32:721–31. doi: 10.1016/j.rdc.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Hsieh C, Novielli KD, Diamond JJ, Cheruva D. Health beliefs and attitudes toward the prevention of osteoporosis in older women. Menopause. 2001;8:372–6. doi: 10.1097/00042192-200109000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Kanis JA, Oden A, Johnell O, Jonsson B, De Laet C, Dawson A. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int. 2001;12:417–27. doi: 10.1007/s001980170112. [DOI] [PubMed] [Google Scholar]
- 18.Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, CA: Sage; 2002. Qualitative analysis and interpretation; pp. 431–534. [Google Scholar]
- 19.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15:175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 20.Cadarette SM, Beaton DE, Gignac MA, Jaglal SB, Dickson L, Hawker GA. Minimal error in self-report of having had dxa, but self-report of its results was poor. J Clin Epidemiol. 2007;60:1306–11. doi: 10.1016/j.jclinepi.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Giangregorio L, Papaioannou A, Thabane L, Debeer J, Cranney A, Dolovich L, Adili A, Adachi JD. Do patients perceive a link between a fragility fracture and osteoporosis? BMC Musculoskelet Disord. 2008;9:38. doi: 10.1186/1471-2474-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mauck KF, Cuddihy MT, Trousdale RT, Pond GR, Pankratz VS, Melton LJ., III The decision to accept treatment for osteoporosis following hip fracture: exploring the woman’s perspective using a stage-of-change model. Osteoporos Int. 2002;13:560–4. doi: 10.1007/s001980200073. [DOI] [PubMed] [Google Scholar]
- 23.Sedlak CA, Doheny MO, Estok PJ, Zeller RA, Winchell J. DXA, health beliefs, and osteoporosis prevention behaviors. J Aging Health. 2007;19:742–56. doi: 10.1177/0898264307304303. [DOI] [PubMed] [Google Scholar]
- 24.Hellekson KL. NIH releases statement on osteoporosis prevention, diagnosis, and therapy. Am Fam Phys. 2002;66:161–2. [PubMed] [Google Scholar]
- 25.Siminoski K, Leslie WD, Frame H, Hodsman A, Josse RG, Khan A, Lentle BC, Levesque J, Lyons DJ, Tarulli G, Brown JP. Recommendations for bone mineral density reporting in Canada. Can Assoc Radiol J. 2005;56:178–88. [PubMed] [Google Scholar]
- 26.Dawson-Hughes B, Tosteson AN, Melton LJ, III, Baim S, Favus MJ, Khosla S, Lindsay RL. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int. 2008;19:449–58. doi: 10.1007/s00198-008-0559-5. [DOI] [PubMed] [Google Scholar]
- 27.Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech. Rep. Ser. 1994;843:1–129. [PubMed] [Google Scholar]
- 28.Tosteson AN, Melton LJ, III, Dawson-Hughes B, Baim S, Favus MJ, Khosla S, Lindsay RL. Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int. 2008;19:437–47. doi: 10.1007/s00198-007-0550-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE, Berger ML. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164:1108–12. doi: 10.1001/archinte.164.10.1108. [DOI] [PubMed] [Google Scholar]
- 30.Griffiths F, Green E, Tsouroufli M. The nature of medical evidence and its inherent uncertainty for the clinical consultation: qualitative study. Br Med J. 2005;330:511. doi: 10.1136/bmj.38336.482720.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003:CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 32.Gerend MA, Erchull MJ, Aiken LS, Maner JK. Reasons and risk: factors underlying women’s perceptions of susceptibility to osteoporosis. Maturitas. 2006;55:227–37. doi: 10.1016/j.maturitas.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 33.Borkan JM, Quirk M, Sullivan M. Finding meaning after the fall: injury narratives from elderly hip fracture patients. Soc Sci Med. 1991;33:947–57. doi: 10.1016/0277-9536(91)90265-e. [DOI] [PubMed] [Google Scholar]
- 34.Reventlow SD. Perceived risk of osteoporosis: restricted physical activities? Qualitative interview study with women in their sixties. Scand J Prim Health Care. 2007;25:160–5. doi: 10.1080/02813430701305668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Creswell J. Qualitative inquiry and research design: choosing among five traditions. Sage; Thousand Oaks, CA: 1998. [Google Scholar]