Abstract
Introduction
Pervasive refusal syndrome (PRS) describes children with social withdrawal who become unable to walk, eat, or care for themselves. This case report examines whether an integrative medicine approach is useful for treating PRS.
Case Presentation
A seven-year-old girl with symptoms most consistent with PRS and depression was admitted to a pediatric ward in Germany that integrates conventional pediatric and psychosomatic care with anthroposophic medicine. She was integrated into the structured activities of the ward and received massages, movement therapy, and color light therapy. Her parents were fully integrated into her care. After four weeks, she talked again, showed increased appetite, and supported herself when moved passively. She made a full recovery within four weeks after hospital discharge.
Discussion
Integration of parents and an integrative medicine approach providing a variety of comforting sensory experiences was helpful for this patient with PRS.
INTRODUCTION
Pervasive refusal syndrome (PRS) describes children with dramatic social withdrawal who refuse or are unable to walk, eat, or care for themselves, typically refusing any help.1 The etiology has been discussed as a sensitivity-stressor spectrum of traumatic experiences.2 A multidisciplinary, structured, inpatient psychiatric approach that provides persistent, realistic optimism and restricted parent visits has been recommended.3,4 There is documentation of one child being treated on a general pediatric ward with full integration of parents into her care5 and one child treated at home.6 Complementary and alternative medicine approaches seem to have a place in child psychiatry,7 but there are no reports detailing their use in PRS.
CASE PRESENTATION
Presenting Concerns
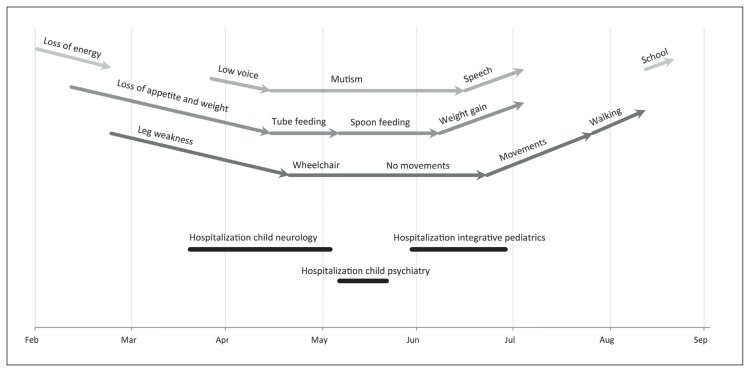
A seven-year-old white girl presented with unclear loss of energy and diffuse headaches. Her symptoms worsened during the next four weeks with the addition of loss of appetite. After a viral infection of the upper respiratory tract, she began to experience generalized weakness of the limbs, with increasing gait difficulties (Figure 1).
Figure 1.
Timeline.
In her medical history, the patient had colic in early infancy and Stage 1 Lyme borreliosis at age 5 years. Typical child development milestones were met. During preschool she had difficulties detaching from her mother and complained about frequent abdominal pain. The family physician described her as an intelligent, almost overly alert, sensitive, and anxious child. Her weight fluctuated at or above the third percentile for age. She began primary school at age six full of enthusiasm and was well performing and well integrated. A few months into the first school year, she seemed increasingly exhausted, eagerly awaiting each weekend and not wanting to return to school after holidays. The girl lived with her parents and a younger brother. Both parents had been feeling overworked the previous year; the mother had been near burnout and taken time off work.
During a 6-week hospitalization for diagnostic work-up at a pediatric neurology center, the girl became wheelchair bound, refused to eat, and lost further weight, requiring feeding by nasogastric tube. Her speech became slow and poorly pronounced, and she whimpered and cried for hours every day. She was transferred to a child psychiatric ward, where she received diagnoses of moderate depression, mixed dissociative disorder, and separation anxiety. Treatment with haloperidol was started. Her parents interrupted the hospitalization and medication after 16 days because they did not agree with the restricted twice-weekly visits and a pharmaceutical treatment approach. She was then admitted to a general pediatric ward with an integrative medicine approach at the Filderklinik in Stuttgart, Germany, on referral from the family physician.
At physical examination, the girl did not speak but appeared alert and smiled as a positive response to questions. Sitting in a wheelchair with her head hanging to the side, no active movements occurred. There was no spasticity, posturing, or negativism. Muscle tendon reflexes were present and symmetric. Babinski sign was absent. She whimpered even in response to light touch. Findings from examination of the heart, lungs, and abdomen were normal. The child’s body mass index was 11.4 kg/m2 (below the third percentile).
Extensive diagnostic evaluations for infectious, metabolic, neoplastic, and endocrine causes of her neurologic symptoms were carried out during the initial neurologic hospitalization. All the following parameters were found to be normal: cerebrospinal fluid analyzed for cells, chemistry panel, Borrelia burgdorferi serologic analysis, polymerase chain reaction for Herpes simplex and picornavirus; complete blood cell count; electrolytes; liver function tests; thyroid function tests; vitamin B12 levels; cortisol levels; screening tests for metabolic diseases; copper elimination tests for Wilson disease; and antibodies for gluten intolerance. In addition, magnetic resonance imaging of the head and spine and electroencephalography had normal results. Lively muscle tendon reflexes excluded Guillain-Barré syndrome. No intelligence test was performed.
The working diagnosis on arrival to our service was PRS because her withdrawal affected eating, mobilization, speech, and school attendance and required hospitalization, and because she would react negatively to encouragement and praise.3,8 Crying and whimpering were atypical for PRS, and depression was considered as an additional diagnosis. Depression could not, however, explain the level of somatic impairment in the absence of depressive stupor, agitation, diurnal variation, or psychomotor retardation.2 Separation anxiety seemed present but could not explain the extent of the symptoms. Although she had illness gains in the form of paternal attention, her condition fit less with conversion disorder, which more typically affects one organ system at a time; additionally, neurologic inconsistencies that are diagnostic of conversion muscle weakness were missing.9 A psychotic disorder with predominantly negative symptoms was ruled out because she was always adequate in visual contact and her sense of reality was intact. Although mutism can be part of catatonia, she had none of the motor signs of this condition.10 It should be noted, however, that some catatonia experts consider PRS a misnomer for catatonia.11
Therapeutic Intervention and Treatment
The hospital setting was a pediatric ward that integrates conventional care with anthroposophic medicine.12 The team included physicians, nurses, special educators, and therapists, offering specialized movement therapy,13 rhythmic massage,14 art therapies, and color light therapy.15 Specific nursing techniques included massages and compresses. Medications in low homeopathic dilutions were used in addition to conventional medications. Elements of Waldorf special education were integrated into the ward routines.16 A pediatrician experienced in child psychiatry and a senior pediatric neurologist were involved in this patient’s care.
The parents were told that, as a sensitive and anxious child, their daughter seemed to have “pulled back” because she had too quickly exhausted her energy with her alert and active approach toward an increasingly demanding environment. The therapy goal was recovery through comforting sensory and whole-body experiences, with initial acceptance of her regression.
We allowed the mother to be present throughout the hospilization to let the girl feel secure, accepting potential reinforcement of the mother-child attachment. An initial four-week stay was agreed to by the parents. All therapies would at least be tried; there was an understanding that a nasogastric tube would be placed if she lost further weight.
The girl was integrated into joint meals with patients, parents, and staff; joint morning and evening gatherings of all children in a circle; and a daily play group for preschool children. She would sit in her wheelchair rather than play, but from her eye expressions she appeared increasingly engaged. She was spoon-fed, progressing gradually from pureed to solid food and eventually a regular diet. A special educator played to her on a harp and read her stories.
The patient received daily gentle abdominal massages with mallow oil (Malva arborea), and rhythmic massage of the legs with ointment containing pallasites, a mineral. She had twice-weekly oil-dispersion baths with gold-rose blossom oil and, toward the end, evening mustard footbaths.
In movement therapy (eurythmy therapy), movements were first shown by the therapist and connected to short stories. Later the therapist would move the girl’s arms and legs; during Week 4 the patient began giving active support during arm movements.
Color light therapy sessions involved sitting five to eight minutes in front of different metal-colored glasses (manganese-violet, iron-blue, red-gold, and cobalt-blue).
Only one family therapy session took place with both parents.
Anthroposophic medications were administered as follows:
Before admission and continued until hospital Day 9: Bryophyllum 50% trituration, Bryophyllum argento cultum Rh D3 (D denotes decimal dilution, ie, D2 = 1:102, D3 = 1:103, etc), and Gentiana Magenglobuli D4.
From hospital Day 9 onward: “Aufbaukalk 1, Weleda” (containing Apatit D5, Cucurbita pepo D2); “Aufbaukalk 2, Weleda” (containing Conchae, Quercus D3); and Levisticum D4.
Started between hospital Days 12 and 21: Siderit D6; Argentum metallicum praeparatum D20; Apis D4/Levisticum D3; and Berberis D2/Quarz D19.
Apis/Levisticum and Berberis/Quarz were manufactured by Wala Heilmittel GmbH, Bad Boll, Germany; all other medications were manufactured by Weleda AG, Schwäbisch Gmünd, Germany.
Follow-up and Outcomes
During the course of 4 weeks, the girl began to talk again. Her appetite increased, although she gained only 900 g of weight (still below the third percentile). At the end of the hospitalization, she gave support when moved passively and began moving while asleep. On discharge, she expressed a desire to not be seen in her wheelchair. After discharge, she gradually started walking and within a month made an almost full recovery (except for a stiff walk). A scheduled subsequent hospitalization was no longer needed. A year later, eating habits, weight, body movements, and strength were normal, and she was interacting actively with friends. She now attends a small class in a different school to provide a more socially protected learning environment; she has no academic difficulties.
The parents read the final report and gave signed informed consent for its publication. The mother said of their daughter, “The worst thing was not having a diagnosis for a long time. At the Filderklinik she wanted to avoid being again fed by nasogastric tube and therefore decided to eat. This became her first step toward recovery. In the months preceding her illness, it seemed as if her ambitions were outpacing her energy; this exhausted her. Today she has fully recovered but is less in a hurry to achieve things.”
DISCUSSION
PRS and depression appeared the most likely diagnoses in this sensitive, high-achieving girl. Within the spectrum of resistance, withdrawal and regression were dominant rather than refusal.17 Recovery was exceptionally fast,18 probably helped by absence of severe trauma or family dysfunction, as well as the maintained level of cooperation with the patient, and the therapeutic approach.
We think that the pleasurable atmosphere of a general pediatric ward, body and sensory stimulation therapies, as well as a developed structure of group activities were the main “therapeutic agent.”19 Full parental integration seemed important too. It is unclear whether enmeshed mother-child relationships in PRS are primary or secondary to the child becoming ill.3 Our concept worked similarly well for two additional children with PRS who presented to our clinic.
Anthroposophic medicine is an integrative treatment system based on a holistic understanding of humans and nature that considers a close interconnection between body, mind, and spirit in its therapeutic approach.12,20 Anthroposophic medicine is integrated with conventional medicine in hospitals and medical practices and is most prevalent in central Europe.12 It is practiced by physicians, therapists, and nurses and is used across a range of medical specialties. A Health-Technology Assessment Report and a 2011 update identified 265 clinical studies on the efficacy and effectiveness of anthroposophic medicine.21–23
The integrative treatment approach with anthroposophic medicine seemed helpful in this case, but separating out how the specific therapies contributed to the overall progress is not feasible. Medications play a limited role in treatment of PRS. Because anthroposophic medications were used simultaneously with various other therapies, their benefit cannot be determined for this single case.
By describing therapeutic concept, setting, and all interventions, a whole-systems research approach was taken.24 A limitation of this report is that no intelligence test was performed, because the girl’s intelligence was perceived as above average. Another limitation is that replication requires a multidisciplinary approach and a team with psychiatric experience that few general pediatric departments can offer. Other methods than those used here could be considered to provide comforting sensory stimulation, such as Snoezelen multisensory stimulation therapy.25
CONCLUSION
An integrative medicine approach with various complementary therapies focused on comforting and sensory stimulation, were helpful in this case of PRS and depression.
Equal
When the disease is stronger than the patient, the physician will not be able to help at all. When the strength of the patient is greater than the strength of the disease, he does not need a physician at all. But when both are equal, then one needs a physician who will support the patient’s strength and help him against the disease.
— Abu Bakr Muhammad Ibn Zakariya al Razi, 854–925, Persian polymath, physician, alchemist, and philosopher
Acknowledgments
Dr Sally Hargreaves (Imperial College London) and Dr Kavitha Kolappa (Harvard Medical School) provided helpful comments on the manuscript.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Lask B, Britten C, Kroll L, Magagna J, Tranter M. Children with pervasive refusal. Arch Dis Child. 1991 Jul;66(7):866–9. doi: 10.1136/adc.66.7.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nunn KP, Lask B, Owen I. Pervasive refusal syndrome (PRS) 21 years on: a re-conceptualisation and a renaming. Eur Child Adolesc Psychiatry. 2014 Mar;23(3):163–72. doi: 10.1007/s00787-013-0433-7. [DOI] [PubMed] [Google Scholar]
- 3.Jaspers T, Hanssen GM, van der Valk JA, Hanekom JH, van Well GT, Schieveld JN. Pervasive refusal syndrome as part of the refusal-withdrawal-regression spectrum: critical review of the literature illustrated by a case report. Eur Child Adolesc Psychiatry. 2009 Nov;18(11):645–51. doi: 10.1007/s00787-009-0027-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nunn KP, Thompson SL, Moore SG, English M, Burke EA, Byrne N. Managing pervasive refusal syndrome: strategies of hope. Clin Child Psychol Psychiatry. 1998 Apr;3(2):229–49. doi: 10.1177/1359104598032007. [DOI] [Google Scholar]
- 5.Edwards H, Done A. Caring for Sophie. A child with pervasive refusal syndrome. Paediatr Nurs. 2004 Jun;16(5):39–42. doi: 10.7748/paed2004.06.16.5.39.c927. [DOI] [PubMed] [Google Scholar]
- 6.Wright B, Beverley D. Pervasive refusal syndrome. Clin Child Psychol Psychiatry. 2012 Apr;17(2):221–8. doi: 10.1177/1359104511403680. [DOI] [PubMed] [Google Scholar]
- 7.Simkin DR, Popper CW. Overview of integrative medicine in child and adolescent psychiatry. Child Adolesc Psychiatr Clin N Am. 2013 Jul;22(3):375–80. v. doi: 10.1016/j.chc.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Thompson SL, Nunn KP. The pervasive refusal syndrome: the RAHC experience. Clin Child Psychol Psychiatry. 1997 Jan;2(1):145–65. doi: 10.1177/1359104597021010. [DOI] [Google Scholar]
- 9.Stone J, Warlow C, Sharpe M. The symptom of functional weakness: a controlled study of 107 patients. Brain. 2010 May;133(Pt 5):1537–51. doi: 10.1093/brain/awq068. [DOI] [PubMed] [Google Scholar]
- 10.Fink M, Taylor MA. The catatonia syndrome: forgotten but not gone. Arch Gen Psychiatry. 2009 Nov;66(11):1173–7. doi: 10.1001/archgenpsychiatry.2009.141. [DOI] [PubMed] [Google Scholar]
- 11.Dhossche D, Kellner CH. Pervasive refusal syndrome: a misnomer for catatonia. Asian J Psychiatr. 2015 Dec;18:113. doi: 10.1016/j.ajp.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Kienle GS, Albonico HU, Baars E, Hamre HJ, Zimmermann P, Kiene H. Anthroposophic medicine: an integrative medical system originating in Europe. Glob Adv Health Med. 2013 Nov;2(6):20–31. doi: 10.7453/gahmj.2012.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kienle GS, Hampton Schwab J, Murphy JB, et al. Eurythmy therapy in anxiety. Altern Ther Health Med. 2011 Jul-Aug;17(4):56–63. [PubMed] [Google Scholar]
- 14.Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H. Rhythmical massage therapy in chronic disease: a 4-year prospective cohort study. J Altern Complement Med. 2007 Jul-Aug;13(6):635–42. doi: 10.1089/acm.2006.6345. [DOI] [PubMed] [Google Scholar]
- 15.Altmaier M. [Metallfarblichttherapie: Zur Forschung und Entwicklung einer neuen Therapie auf anthroposophischer Grundlage]. Frankfurt am Main, Germany: Info 3 Verlag; 2010. Jun 1, [Google Scholar]
- 16.Sobo EJ. Salutogenic education? Movement and whole child health in a Waldorf (Steiner) school. Med Anthropol Q. 2015 Jun;29(2):137–56. doi: 10.1111/maq.12140. [DOI] [PubMed] [Google Scholar]
- 17.Jans T, Ball J, Preiss M, Haberhausen M, Warnke A, Renner TJ. Pervasive refusal syndrome. Three German cases provide further illustration. Z Kinder Jugendpsychiatr Psychother. 2011 Sep;39(5):351–8. doi: 10.1024/1422-4917/a000128. [DOI] [PubMed] [Google Scholar]
- 18.Guirguis S, Reid C, Rao S, Grahame V, Kaplan C. Follow-up study of four cases of pervasive refusal syndrome. Eur Child Adolesc Psychiatry. 2011 May;20(5):271–4. doi: 10.1007/s00787-011-0169-1. [DOI] [PubMed] [Google Scholar]
- 19.Green J, Burke M. The ward as a therapeutic agent. In: Green J, Jacobs B, editors. In-patient child psychiatry: modern practice, research and the future. Hove, East Sussex, United Kingdom: Routledge; 1998. pp. 93–109. [Google Scholar]
- 20.Heusser P. [Anthroposophische Medizin und Wissenschaft: Beiträge zu einer integrativen medizinischen Anthropologie]. Stuttgart, Germany: Schattauer; 2011. [Google Scholar]
- 21.Kienle GS, Kiene H, Albonico HU. Anthroposophic medicine: effectiveness, utility, costs, safety. Stuttgart, Germany: Schattauer; 2006. [Google Scholar]
- 22.Kienle GS, Glockmann A, Grugel R, Hamre HJ, Kiene H. [Clinical research on anthroposophic medicine: update of a health technology assessment report and status quo]. Forsch Komplementmed. 2011;18(5):269–82. doi: 10.1159/000331812. [Article in German] [DOI] [PubMed] [Google Scholar]
- 23.Hamre HJ, Kiene H, Ziegler R, et al. Overview of the publications from the Anthroposophic Medicine Outcomes Study (AMOS): a whole system evaluation study. Glob Adv Health Med. 2014 Jan;3(1):54–70. doi: 10.7453/gahmj.2013.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boon H, Macpherson H, Fleishman S, et al. Evaluating complex healthcare systems: a critique of four approaches. Evid Based Complement Alternat Med. 2007 Sep;4(3):279–85. doi: 10.1093/ecam/nel079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hotz GA, Castelblanco A, Lara IM, Weiss AD, Duncan R, Kuluz JW. Snoezelen: a controlled multi-sensory stimulation therapy for children recovering from severe brain injury. Brain Inj. 2006 Jul;20(8):879–88. doi: 10.1080/02699050600832635. [DOI] [PubMed] [Google Scholar]