Abstract
The End of Life Option Act in California, effective June 9, 2016, permits physicians to prescribe lethal medication to patients confirmed to be terminally ill and capable of independently making and carrying out a decision to ingest deadly medication. Medicine has traditionally excluded the provision of deadly medication from proper practice. Physicians reasonably may hold to that limit. However, honoring a repeated request from a capable, terminally ill patient to receive life-ending medication still can be considered to be a moral and permissible approach to relieve suffering. A physician choosing to expand his/her role within this narrowly defined context allows the patient to assume authority for a deeply personal decision that may belong to the patient more than to anyone else.
INTRODUCTION
This article details an ethical rationale for the physician prescribing life-ending medications for capable, terminally ill patients who will then decide for themselves whether to end their lives this way. It also provides guidance for the physician who wonders whether this service should be offered within the context of an agreement to work collaboratively as physicians. More than one ethical approach may be used to examine this clinical situation. This particular analysis is offered to promote a moral understanding among physicians practicing together within the Southern California Permanente Medical Group (SCPMG). The approach includes those who appreciate the actions permitted in the End of Life Option Act (EOLOA) as useful to Kaiser Permanente (KP) patients and those who may hold an opposing opinion. Physicians who have not yet decided which approach to consider appropriate may benefit from this discussion.
Legislative Highlights
The state of Oregon implemented the Death with Dignity Act in 1997,1 adopting a process for “Physician Aid-In-Dying.” Although commonly referred to as “Physician-Assisted Suicide,” many patients were satisfied with receiving the medication without taking it. Numerous attempts to repeal the Act failed. In 2006, the US Supreme Court ruled in favor of Oregon, upholding the law.2
KP Northwest adopted procedures to comply with the Oregon law to include participation by physicians within Northwest Permanente.
In California, skilled lobbying efforts, high-profile cases, significant voter support, and precedents from other states led to the proposal of the EOLOA.3 Initially the California Medical Association (CMA) opposed the legislation, relying on a position statement held since 1987. After a poll and discussion, the CMA changed its position to “neutral” in May 2015.4 Despite eloquent objections by some physicians reluctant to be placed in a role proscribed by traditional values and after withdrawal of CMA opposition, the EOLOA was signed into law in 2015 and implemented on June 9, 2016.
The CMA position change and the enacted law are at odds with the current American Medical Association position (see Sidebar: American Medical Association Opinion 2.211—Physician-Assisted Suicide), leaving California physicians in a quandary about existing and potential roles.
Since the passage of the law, discussions have included attempts to reverse the EOLOA through referendum or other political processes. A referendum attempt failed for lack of signatures in January 2016.
The California End of Life Option Act
The EOLOA3 details circumstances under which physicians in California, including those within SCPMG, may legally provide life-ending medications to terminally ill patients. KP has remained neutral on the subject of the EOLOA. After passage of the law, a KP Southern California task force formed to organize efforts to comply with the EOLOA. The task force asked the physician CoDirector of the KP Southern California Bioethics Program to provide an ethical analysis for SCPMG physicians. This article shares that analysis (see Sidebar: Ethical Analysis Summary).
Within the context of the law, a terminally ill patient with access to adequate palliative care, who is capable of making this decision without coercion or impairment from psychiatric illness, may express a persistent wish to consciously ingest, under his/her own power, a physician-prescribed, life-ending medication. That medication allows the dying patient to determine the time and nature of death rather than leaving it to the course of illness.
Provisions of the EOLOA include that the patient must
be age 18 years or older; capable of making “medical” decisions as assessed by an attending and consulting physician; and, if needed, as assessed by either a psychologist or a psychiatrist
have a disease that within reasonable medical judgment, and confirmed by a consulting physician, will result in death within 6 months
be able to make an affirmative, conscious, and physical act to self-administer and ingest the aid-in-dying medication
make two oral requests to an attending physician, separated by at least 15 days and associated with a completed, written request
be a California resident.
American Medical Association Opinion 2.211—Physician-Assisted Suicide1.
Physician-assisted suicide occurs when a physician facilitates a patient’s death by providing the necessary means and/or information to enable the patient to perform the life-ending act (eg, the physician provides sleeping pills and information about the lethal dose, while aware that the patient may commit suicide).
It is understandable, though tragic, that some patients in extreme duress—such as those suffering from a terminal, painful, debilitating illness—may come to decide that death is preferable to life. However, allowing physicians to participate in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks.
Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life. Patients should not be abandoned once it is determined that cure is impossible. Multidisciplinary interventions should be sought including specialty consultation, hospice care, pastoral support, family counseling, and other modalities. Patients near the end of life must continue to receive emotional support, comfort care, adequate pain control, respect for patient autonomy, and good communication. (I, IV)
Issued June 1994
Opinion 2.211: physician-assisted suicide [Internet]. Chicago, IL: American Medical Association; 1994 Jun [cited 2016 Feb 28]. Available from: www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion2211.page.
Once the medications have been secured by the patient, s/he assumes moral authority over whether to take them. California is, to some degree, relieved of the moral implications of disallowing patients to take their lives in this manner and assumes some responsibility to confirm that the process does not result in harm. The EOLOA can be considered to be a legal device necessary in the context of the current California law that allows patients to receive controlled substances only through a physician’s prescription. Although individual physician participation in this act is optional, this legal situation requires physician participation for the Act to be operationalized.
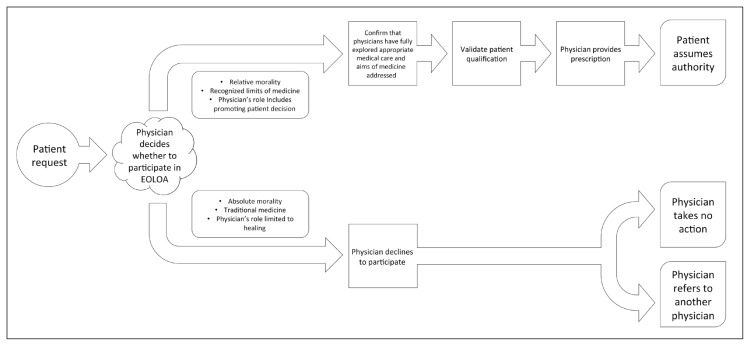
Practically, the participating physician takes three steps (Figure 1):
Figure 1.
Flow chart of process for physician involvement in the EOLOA.
EOLOA = End of Life Option Act.
confirm appropriate medical care has been fully explored and the aims of medicine have been addressed
validate that a patient is qualified to receive the medication under the EOLOA and within the exercise of a physician’s best medical judgment
provide the prescription to the patient.
AN ETHICAL RATIONALE
Some believe that any step a physician takes toward providing any patient with lethal medication violates traditional prohibitions against offering lethal or poisonous medication.5,6 This view holds that the physician acting in such a role is either engaging in or is complicit in an immoral act—or at least not practicing medicine in the traditional role of medicine as a healing profession. In this traditional framework, the prescription of life-ending medication could be seen as eroding the credibility and fabric of a social understanding of the practice of medicine. Some may consider that such a serious change might undermine the pillars on which the profession of medicine is founded and damage related provisions for professional conduct. Physicians holding this view may understandably regard those who prescribe life-ending medication as unprofessional and fear that the prescription of aid-in-dying drugs will destroy patient trust in the physician’s commitment to cure.
Ethical Analysis Summary.
Some physicians within California will choose to participate in the End of Life Option Act (EOLOA). They will feel they are doing the right thing when they prescribe life-ending medications for capable, terminally ill patients who will then decide for themselves whether to end their lives this way. Other physicians may feel uncomfortable participating, believing that prescribing lethal medication may be immoral or outside the proper practice of medicine. Undecided physicians may suspend judgment, waiting to be convinced by a particular patient with a terminal illness making an understandable request.
The arguments offered in this article are intended to help physicians make their own decision and to appreciate the decisions of other physicians. Although a physician may disagree with another’s position, tolerance is important. Tolerance fosters mutual respect, enhances working relationships, and provides for the broader understanding that physicians who care deeply about their patients on this particular issue may not agree.
Physicians who value traditional medicine: For these physicians prescribing fatal doses of medication to patients is just wrong; it is contrary to the proper practice of medicine as handed down through millennia. Medicine is about healing; ending life can never be considered healing. There must be some absolute moral standard on which medicine is founded. Just as physicians should not participate in torture or the execution of criminals, physicians also should not participate in suicide or encourage patients to kill themselves. Physicians should focus solely on providing sufficient palliative and hospice resources to the terminally ill to reduce the likelihood of such requests.
Physicians for whom the morality of this specific end-of-life decision is relative and not absolute: These physicians feel that, when there is no way to heal the dying patient, the best approach is to allow the patient to decide this issue. When the Hippocratic Oath was written, a dying patient might have received assistance from nonphysicians to obtain life-ending preparations. The traditional practice of medicine did not prevent patients from obtaining these drugs; it only disallowed physicians from providing them. Well-intended modern laws restrict independent patient access to lethal medications without a physician’s prescription. The patient may understandably view a physician’s refusal to prescribe these medications as being unfairly obstructive. The EOLOA allows a physician to honor a dying patient’s request to obtain a life-ending prescription. Although prescribing lethal doses of medication violates the tenets of traditional medicine, it is considered reasonable with the safeguards of the EOLOA. The physician prescribes the drugs, allowing the patient to assume authority for this personal decision. In addition, the physician provides comfort to the patient, giving him/her a measure of control over an uncontrollable illness, and confirming that a moral community accepts the patient’s decision. Although many concerns of the dying can be adequately addressed by palliative or hospice care, these have limits with regard to the ability to restore lost autonomy, to promote personal dignity, to make life sufficiently enjoyable, and to lessen a patient’s sense of burden on loved ones.
Thus, the act of prescribing a fatal dose of medication is not within the traditional practice of medicine. Physicians may reasonably hold to that limit. However, delivery of life-ending medications to the terminally ill can still be considered an approach to relieve suffering that is both moral and permissible.
Physicians who choose to participate in the provisions of the EOLOA also uphold key notions of professional responsibility. Particularly important in this view is the practical realization of the worth and centrality of individual human values in every aspect of medical professional activity. For these physicians, it follows that a sensitive and empathic response that honors individual beliefs, dignity, and perceived suffering may, in some contexts, understandably result in the prescription of life-ending medication. The physician fulfills a patient’s request, giving the patient a measure of control over an uncontrollable illness, and confirming that a moral community accepts the patient’s decision. This view holds further that patients will trust physicians additionally to facilitate a more comfortable end, while addressing perhaps the greatest suffering—physical, emotional, existential—that patients experience.
Although one physician within SCPMG may not accept another’s position on this compelling issue, tolerance by physicians of the plurality of opinions and the different social roles of medical professionals that result remains deeply important. Tolerance fosters mutual respect, enhances working relationships, and provides for a broader understanding that physicians who care deeply about their patients may not agree on this particular issue. This ethical analysis is offered to promote understanding among SCPMG physicians and with it, a commitment to professional values that continue to inspire patient trust and appreciation.
EMPIRIC BASIS FOR THE END OF LIFE OPTION ACT
For those patients whose underlying disease has no cure, physicians offer treatment for suffering: the palliation of symptoms. The growth of the specialty of palliative medicine over the last decades is a testimony to the complexity of this treatment. Despite appropriate palliation, some patients facing death will still request life-ending medication. The reasons for this request have been categorized in various ways as seen by those engaged in this activity who poll their particular patient populations. See Sidebar: Euthanasia Research for examples and extracts from one Web site promoting the discussion of euthanasia.
THE MORAL BASIS
Although palliation of symptoms may not be enough for some terminally ill patients to want to continue life, this fact does not oblige physicians to provide the means by which a patient might end it. On what moral basis, then, can physicians participate in the validation of a patient’s request for life-ending medications, confirm the patient’s access to palliative care, and in the proper situation prescribe deadly medication?
From the Hippocratic Corpus comes a direction to know when medicine can no longer be helpful and to know when to step away.7 This is stated succinctly in the following:
First I will define what I conceive medicine to be. In general terms, it is to do away with the sufferings of the sick, to lessen the violence of their diseases, and to refuse to treat those who are overmastered by their diseases, realizing that in such cases medicine is powerless.7
In modern understanding of the above, physicians continue to offer relief of suffering to those overmastered by disease while ceasing attempts that predictably will be ineffective at treating the underlying illness. However, in the context of the time in which the Hippocratic Corpus was conceived, the patient, family or persons other than physicians might morally and reasonably seek provisions towards an expedited death through herbal drugs. The Greeks had the knowledge to quickly effectuate a death as evidenced by the death of Socrates, a contemporary of Hippocrates.
Euthanasia Research1.
The Oregon Department of Human Services explained in its March 9, 2006 “Eighth Annual Report on Oregon’s Death with Dignity Act”:
“The most frequently reported concerns included a decreasing ability to participate in activities that make life enjoyable (89%), loss of dignity (89%), and losing autonomy (79%) …”
From: Pearlman RA, Starks H. Chapter 6. Why do people seek physician-assisted death? In: Quill TE, Battin MP. Physician-assisted dying: the case for palliative care and patient choice. Baltimore, MD: Johns Hopkins University Press; 2004. p 91–101:
“Motivating Factor
-
Illness-related experiences
- Feeling weak, tired, and uncomfortable 24 (69%)
- Loss of function 23 (66%)
- Pain or unacceptable side effects of pain medication 14 (40%)
-
Threats to sense of self
- Loss of sense of self 22 (63%)
- Desire for control 21 (60%)
- Long-standing beliefs in favor of hastened death 5 (14%)
-
Fears about the future
- Fears about future quality of life and dying 21 (60%)
- Negative past experiences with dying 17 (49%)
- Fear of being a burden on others 3 (9%).”
From: Ganzini L, Harvath TA, Jackson A, Goy ER, Miller LL, Delorit MA. Experiences of Oregon nurses and social workers with hospice patients who requested assistance with suicide. N Engl J Med 2002 Aug 22;347(8):582–8. DOI: http://dx.doi.org/10.1056/NEJMsa020562:
“According to the hospice nurses, the most important reasons for requesting assistance with suicide, among patients who received prescriptions for lethal medications, were a desire to control the circumstances of death, a desire to die at home, the belief that continuing to live was pointless, and being ready to die. Depression and other psychiatric disorders, lack of social support, and concern about being a financial drain were, according to nurses, relatively unimportant …
Hospice social workers reported that the desire to control the circumstances of death, the wish to die at home, loss of independence or fear of such loss, and loss of dignity or fear of such loss were the most important reasons for requesting prescriptions for lethal medications; the median score for all these reasons was 5 on the 1-to-5 scale. They ranked lack of social support and depression as the least important reasons; the median score for both was 1 …”
Why do patients request physician-assisted death (aka physician-assisted suicide)? [Internet]. Santa Monica, CA: ProCon.org; 2008 Jun 10 [cited 2016 Feb 5]. Available from: http://euthanasia.procon.org/view.answers.php?questionID=000199.
Suicide was not uncommon in ancient Greece. Plato and the stoic, Zeno, described the appropriateness of suicide under certain conditions and perhaps the cowardliness of it under others.8 Hippocrates held the view that physicians should not be associated with this controversial practice and clearly and unequivocally placed it outside the limit of the proper practice of medicine.8
Ironically, after hundreds of years of concerned moral and religious argument, the medicalization of suicide transferred some of this controversy into an arena perhaps least equipped to deal with it. The physician’s role, circumscribed by traditional prohibitions, was limited to describing and attempting to reverse underlying psychiatric self-destructive motivation. The traditional practice of medicine had no ability to endorse euthanasia or to facilitate suicide. Over time, the involvement of the medical profession may have promoted an inappropriate generalization that all those seeking to kill themselves were mentally ill and its corollary that treatment of underlying mental illness might be the most satisfactory approach for suicidal inclination.
TRADITIONAL MEDICINE AND MODERN BALANCE
The traditional understanding of the proper practice of medicine has been that medicine offers therapeutics through which a process of “healing” or “making whole again” may take place. This is stated eloquently by Edmund Pellegrino9p40:
Medicine must be concerned with the “good” of the patient. As David Thomasma and I have emphasized elsewhere, the patient’s good is a compound notion. It is not synonymous with the patient’s medical good. Healing means “to make whole again.” Therefore, ascertaining and enhancing all four realms of the patient’s good are involved in healing—the patient’s biomedical good, his own conception of the good for him as an individual, his good as a member of the human species (ie, the good for humans), and his good as a spiritual being (ie, the good for the soul). The concept of wholeness, together with its asymptotic attainment through relationships between, and among, persons is the specific end of medicine. It is not an end proper to any of the sciences basic to medicine. But without a concept of healing, medicine as such does not exist.
For some patients, the traditional practice of medicine has limitations. In these uncommon situations, there is no healing that can be accomplished medically, no healing that can be appreciated by the patient, no social understanding of healing, and no spiritual understanding of healing.
Without a concept of healing, the traditional practice of medicine ceases to exist. A physician’s determination that the patient has been overmastered by disease and is beyond healing may be the most difficult of the three steps described above that operationalize the EOLOA. Although there is an ongoing role for the medical profession to palliate symptoms, once a patient finds existence within a threat of imminent and unavoidable death to lack meaning, palliation of symptoms cannot return a patient to an acceptable state. At that juncture, although the patient may derive some benefit from palliative therapeutics, those therapeutics can not be understood summarily as “healing.”
In the very distant past, physicians encountering this situation might have stepped aside, leaving patients and families to decide how to proceed, including the possibility of suicide. In the current scenario, with implementation of the EOLOA, the participating physician must detail that for an individual patient, no medical concept of healing, and no promotion of “good” in its compound notion, is understandable by the physician or by the patient. This “diagnosis” that confirms that the patient is “overmastered by disease” and unable to heal or be healed signals the limits of traditional medicine. This stage marks the point where moral authority for a decision regarding dying under this law may be assumed by the patient.
Physicians have elaborated professional values that might guide this expanded role. The relief of suffering has been discussed extensively in the literature.10 Another professional value is that of humanism. As described by Pellegrino, “Humanism encompasses a spirit of sincere concern for the centrality of human values in every aspect of professional activity. This concern focuses on respect for the freedom, dignity, worth, and belief systems of the individual person, and it implies a sensitive, nonhumiliating, and empathetic way of helping with some problem or need.”9p88 Respect for the individual person may not require ceding to the individual patient authority to ingest deadly medication. The “humane” action, although commonly described as offering life-ending medication, cannot be determined from such an analysis. However, in humanism’s explicit call to respect individual freedom and beliefs, some physicians find justification to expand a role for physicians in the specified context of continued patient suffering, in the absence of a known process for healing, and for an individual who repeatedly requests life-ending medication.
The EOLOA details a process intended to protect vulnerable patients and, simultaneously, to preserve the integrity of individual physician moral decision making. The EOLOA mandates that each physician be allowed to decide whether participation for that physician is ethically acceptable and to be protected from social or professional consequences of that assessment. Both physician and patient are permitted to participate in the legal process or to decline involvement. Although the physician and patient are both granted legal permission to engage in this action, each must also grant permission to the other for the process to move forward. Although permissions are essential to procedure, this approach is morally unsatisfying in that permission cannot make a morally wrong act right. The hope is that in areas of moral uncertainty and lack of clear social guidance, vetted agreements by those involved will provide safeguards against abuse.
When a physician first receives a request from a patient for life-ending medication, the physician should explore the request in sufficient detail to determine whether the request is valid. To confirm the diagnosis and prognosis, additional opinions may be required. The physician should confirm the patient’s understanding of current medical care to ensure that the request does not come as a result of end-of-life treatment that can be improved. Maximizing the palliation of symptoms including pain, incontinence, and nausea may make the patient more comfortable. In addition, improving issues of independence, autonomy, spiritual distress, and dignity may be essential for some patients.
The physician must confirm that the patient has decision-making capacity, free from the coercive influence of others, and can self-administer and ingest the medication. The patient must be emotionally and psychologically prepared. Over time, the physician reassesses a judgment by the patient that current and foreseeable life lacks meaning. Once the physician has confirmed the validity of the request, the physician delivers the prescription to the pharmacy. The patient then receives the drugs from the pharmacy and assumes the moral authority to choose whether to take the medication.
Today, previously open avenues to obtain optimal deadly drugs without a physician’s prescription are largely closed to patients. Only physicians licensed within the state of California may place optimal lethal prescriptions within legal reach of the California patient. Advising terminally ill patients requesting lethal medication to find nonprescription means to their death remains irresponsible practically and socially.
Once a capable patient has been determined to be terminally ill, no interest of the state or claim of the medical profession, religion, or any other individual overrides a patient’s request to own a decision whether to take life-ending medication. In the past, state laws intended to protect patients from unsafe prescriptions have placed physicians in the position of denying patients this option.
With the EOLOA, physicians may opt out of a position that obstructs a dying patient’s request to assume moral authority for this decision. To do so, such a physician must violate traditional medical prohibitions against the prescription of deadly medications as detailed above. A diagnosis of terminal illness signals the time that for the patient seeking aid in dying, a physician can consider validating such a patient request. After validation, the participating physician then may decide to act in a role expanded beyond traditional medicine to include the prescription of medications to assist in dying.
CONCLUSION
Thus, the act of prescribing a fatal dose of medication is not within the traditional practice of medicine. Physicians reasonably may hold to that limit. However, honoring a repeated request from a capable, terminally ill patient to receive life-ending medication still can be considered to be a moral and permissible approach to relieve suffering. A physician choosing to expand his/her role within this narrowly defined context allows the patient to assume authority for a deeply personal decision that may belong to the patient more than to anyone else.
Friend
I have come to believe that a content life is one that gracefully carries death on its shoulder as a friend and not a feared adversary.
— The Least of These Brethren: A Doctor’s Story of Hope and Miracles on an Inner-City AIDS Ward. Daniel J Baxter, MD, American author and physician
Acknowledgment
Special thanks are offered to the Medical Bioethics Directors of the Bioethics Program of Kaiser Permanente Southern California for the collegial discussions relevant to this issue. Additionally acknowledged are the written suggestions of David Lerman, PhD; Mark J Bliton, PhD; Felicia Cohn, PhD; Craig Nelson, PhD, CLS; Paula Goodman-Crews, MSW, LSCW; and Linda Washburn, RN. Mason Shaner is acknowledged for assistance with Figure 1.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.The Oregon Death with Dignity Act. ORS 127.800-127.897 (1997 Oct 27).
- 2.Gonzales v Oregon. 546 US 243 (2006 Jan 17).
- 3.California Assembly Bill No. 15. AB-15 End of life. Ch. 1, Part 1.85, Sect. 443 (2015 Oct 5).
- 4.California Medical Association removes opposition to physician aid in dying bill [Internet] Sacramento, CA: California Medical Association; 2015. May 20, [cited 2016 Apr 22]. Available from: www.cmanet.org/news/press-detail/?article=california-medical-association-removes. [Google Scholar]
- 5.The oath. Vol. 147. Cambridge, MA: Loeb Classical Library, Harvard University Press; 1923. Hippocrates of Cos; pp. 298–9. p LCL. [DOI] [Google Scholar]
- 6.Pellegrino ED. Some things ought never be done: moral absolutes in clinical ethics. Theor Med Bioeth. 2005;26(6):469–86. doi: 10.1007/s11017-005-2201-2. [DOI] [PubMed] [Google Scholar]
- 7.Hippocrates The art Loeb edition of the Hippocratic corpus IIJones WHS.London, Great Britain: William Heinemann Ltd; 1923. 192 [Google Scholar]
- 8.Edelstein L. In: Ancient medicine: selected papers of Ludwig Edelstein. Temkin O, Temkin CL, editors. Baltimore, MD: The Johns Hopkins University Press; 1967. Oct 1, pp. 14–9. [Google Scholar]
- 9.Pellegrino ED. In: The philosophy of medicine reborn: a Pellegrino reader. Engelhardt HT Jr, Jotterand F, editors. Notre Dame, IN: University of Notre Dame; 2008. p. 40. [Google Scholar]
- 10.Quill TE. Physicians should “assist in suicide” when it is appropriate. J Law Med Ethics. 2012 Spring;40(1):57–65. doi: 10.1111/j.1748-720x.2012.00646.x. [DOI] [PubMed] [Google Scholar]