Abstract
Despite the prevalence of zygomaticomaxillary complex (ZMC) fractures, there is no consensus regarding the best approach to management. The aim of this study is to determine differences in ZMC fracture treatment among various surgical specialties. A survey was conducted regarding treatment of patients with different ZMC fractures that included a minimally displaced fracture (Case 1), a displaced fracture without diplopia (Case 2), a displaced fracture with diplopia (Case 3), and a complex comminuted fracture (Case 4). The survey was distributed to members of plastic surgery, oral maxillofacial surgery, and otolaryngology societies. The rates of surgical treatment, exploration of the orbital floor, and plating three or more buttresses were analyzed among the specialties. A total of 173 surgeons participated (46 plastic and reconstructive surgeons, 25 oral and maxillofacial surgeons, and 102 otolaryngologists). In Case 1, a significantly higher percentage of plastic surgeons recommend an operation (p < 0.01) compared with other specialties. More than 90% of surgeons would perform an operation on Case 2. Plastic surgeons explored the orbital floor (p < 0.01) and also fixated three or more buttresses more frequently (p < 0.01). More than 93% of surgeons would operate on Case 3, with plastic surgeons having the greatest proportion who fixed three or more buttresses (p < 0.01). In Case 4, there was no difference in treatment patterns between specialties. Across the specialties, more fixation was placed by surgeons with fewer years in practice (<10 years). Conclusion There is no consensus on standard treatment of ZMC fractures, as made evident by the survey. Significant variability in fracture type warrants an individualized approach to management. A thorough review on ZMC fracture management is provided.
Keywords: orbital fractures, zygomatic fractures, facial injuries
The prominence of the zygomaticomaxillary complex (ZMC) convexity along the anterolateral portions of the face makes it vulnerable to traumatic injury. While there is debate as to what part of the facial skeleton is most commonly injured, ZMC fractures comprise up to 40% of facial fractures.1 2 Common etiologies include motor vehicle accidents, assault, falls, and sports-related injuries.1 3 The complex three-dimensional aspect of the zygoma contributes both to facial aesthetics and function. It forms the malar eminence, providing cheek projection, and the lateral and inferior portions of the orbit. Reestablishing preinjury form is the goal of all ZMC fracture treatments, regardless of the approach utilized.
As surgical technique and technology have improved through the past century, management opinions have evolved.4 5 6 7 Standard treatment mostly involves internal fixation with plates and screws, but there is much debate regarding what qualifies as adequate fixation. Three-point fixation for treatment of ZMC fractures is traditionally recommended; however, there are varying opinions on what is truly necessary for adequate reconstruction.6 8 9 10 11
Despite the prevalence of ZMC fractures, there is no consensus in the literature concerning the best approach to management and when repair is indicated. The aim of this study is to survey surgeons among the specialties of plastic and reconstructive surgery (PRS), oral and maxillofacial surgery (OMFS), and otolaryngology (ENT) to look for practice patterns and potential differences in approach to treatment of ZMC fractures. We also provide an extensive literature review on the treatment of these injuries.
Methods
Study Design
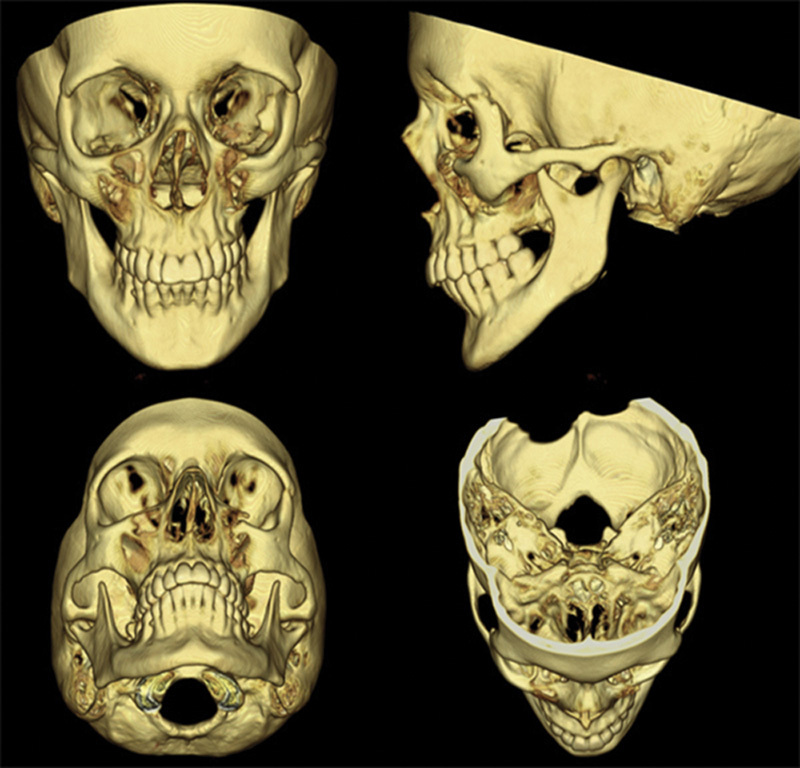
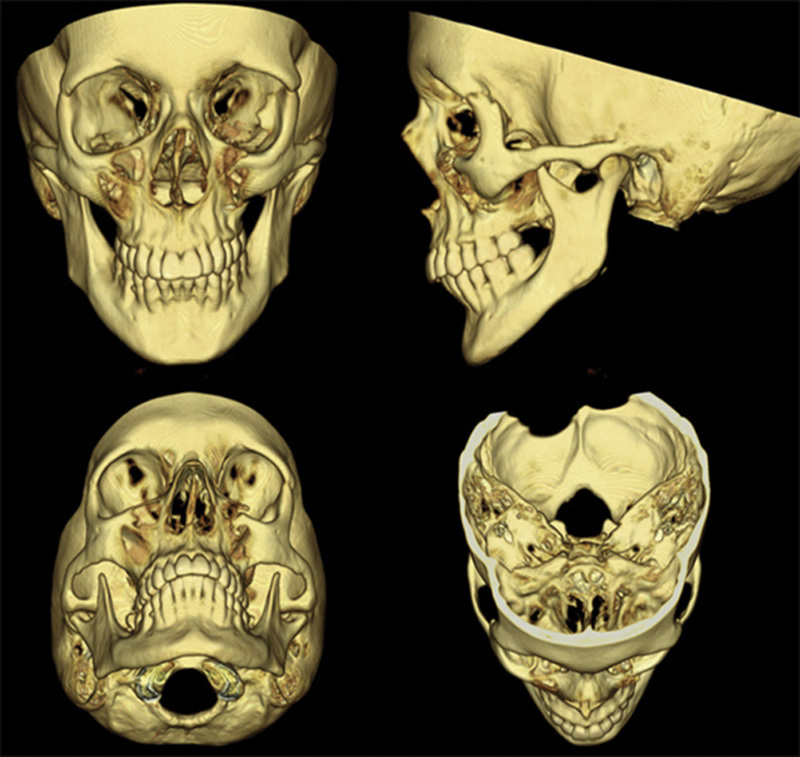
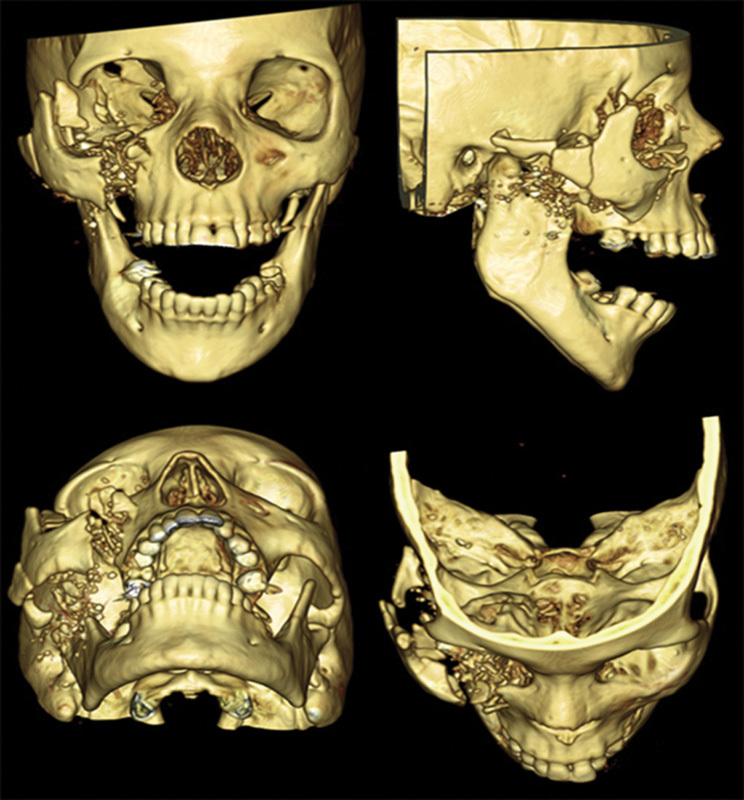
After institutional review board approval, a survey was constructed using REDCap (Research Electronic Data Capture) through Washington University in St. Louis School of Medicine. The survey consisted of questions regarding treatment of four different ZMC fractures in skeletally mature patients. The injury patterns included that of a minimally displaced fracture (Fig. 1), a displaced fracture without diplopia (Fig. 2), a displaced fracture with diplopia (Fig. 3), and a highly comminuted fracture (Fig. 4). The survey questions are detailed in Fig. 5. The survey was then distributed to members of various PRS, OMFS, and ENT societies including the American Society of Maxillofacial Surgeons, the American Association of Oral and Maxillofacial Surgeons, and the American Academy of Facial Plastic and Reconstructive Surgery. Responses were recorded by the REDCap system. Data were collected regarding surgical specialty, practice type, years in practice, multiple soft-tissue approaches (two or more), points of fixation (three or more), and exploration of the orbital floor. In addition, we included details regarding upper and lower eyelid approaches and which buttresses were fixated. A programming code run in MatLab version R2012b (Natick, MA) was employed to calculate results of Fisher exact tests to compare proportions between the surgical specialties including post hoc testing of significant results.12 All other statistical analyses were performed using IBM SPSS version 22 (Armonk, NY). For all comparisons, a p-value of less than 0.01 was considered statistically significant. The Holm-Bonferroni adjustment for multiple testing was then applied to each family of comparisons.
Fig. 1.

Case 1.
Fig. 2.
Case 2.
Fig. 3.
Case 3.
Fig. 4.
Case 4.
Fig. 5.
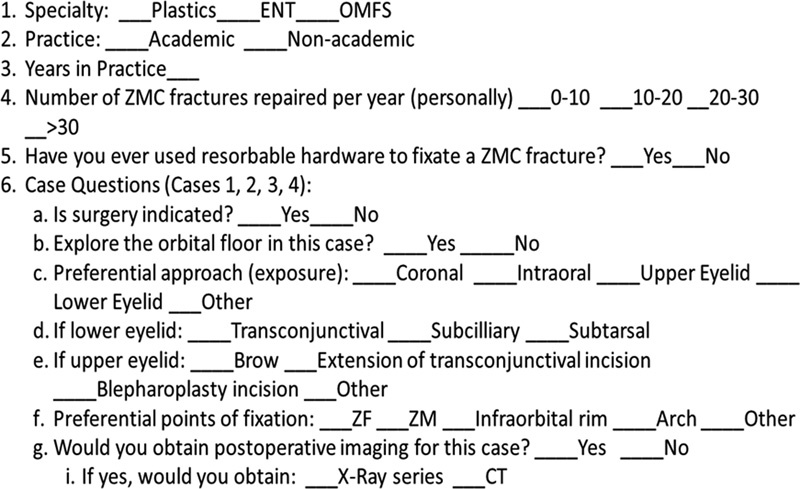
Survey questions.
Results
A total of 173 surgeons participated in this survey (102 ENT, 25 OMFS, and 46 PRS). Practice type, years in practice, number of ZMC fractures repaired in a year, and use of resorbable hardware are shown in Table 1. Experience using resorbable hardware to fixate ZMC fractures is equivalent among all specialties (p = 0.54). No difference in treatment was found based on surgical volume (defined as less than or greater than ten cases per year). OMFS respondents had the greatest average years of experience compared with the other two specialties (p = 0.007).
Table 1. Demographics of survey participants.
| ENT | OMFS | PRS | p-Value | |
|---|---|---|---|---|
| Participants | 102 | 26 | 46 | |
| Academic | 50 (49%) | 17 (65%) | 35 (76%) | 0.006 |
| Years in practice | ||||
| 1–10 | 50 (54%) | 8 (32%) | 19 (45%) | 0.007 |
| 11–20 | 20 (22%) | 4 (16%) | 11 (26%) | |
| 21–30 | 21 (23%) | 7 (28%) | 8 (19%) | |
| > 30 | 1 (1%) | 6 (24%) | 4 (10%) | |
| ZMC fractures repaired per year | 0.004 | |||
| 1–10 | 67 (66%) | 8 (31%) | 18 (39%) | |
| 11–20 | 21 (21%) | 11 (42%) | 18 (39%) | |
| 21–30 | 6 (6%) | 2 (8%) | 2 (4%) | |
| > 30 | 8 (8%) | 5 (20%) | 8 (17%) | |
| Use of resorbable hardware | 35 (34%) | 10 (39%) | 12 (26%) | p = 0.539 |
Abbreviations: ENT, otolaryngologists; OMFS, oral and maxillofacial surgeons; PRS, plastic and reconstructive surgeons; ZMC, zygomaticomaxillary complex.
Case-Specific Variables
Case 1: Minimally Displaced Fracture
A higher proportion of plastic surgeons (p < 0.007) recommended surgical repair (22 vs. 6% of ENT, 0% of OMFS) (Table 2). Of those who would operate, a significantly higher percentage of plastic surgeons would also explore the orbital floor (p < 0.01). The decision to either utilize two or more approaches or fixate three or more buttresses was equivalent between the specialties (PRS and ENT). Both ENT and PRS preferred the intraoral, lower eyelid, and upper eyelid approach to this patient. Both ENT and PRS agreed that some combination of zygomaticofrontal (ZF), zygomaticomaxillary (ZM), and infraorbital rim fixation was indicated. Among the treating surgeons, 50% of PRS and 17% of ENT would perform a postoperative computed tomographic (CT) scan (Fig. 6).
Table 2. Core ZMC treatment principles.
| Surgery indicated? | ENT | OMFS | PRS | p-Value |
|---|---|---|---|---|
| Total responses | 102 (%) | 26 (%) | 46 (%) | |
| Case 1 | 6 (5) | 0 (0) | 10 (21) | 0.003 |
| Case 2 | 95 (93) | 25 (96) | 42 (91) | 0.419 |
| Case 3 | 102 (100) | 26 (100) | 43 (93) | 0.038 |
| Case 4 | 101 (99) | 26 (100) | 45 (97) | 0.658 |
| Explore orbital floor | ||||
| Case 1 | N/A | N/A | N/A | N/A |
| Case 2 | 37 (38) | 8 (32) | 31 (73) | <0.001 |
| Case 3 | 98 (96) | 24 (92) | 39 (90) | 0.337 |
| Case 4 | 100 (99) | 26 (100) | 44 (97) | 0.656 |
| Fixate three or more buttresses | ||||
| Case 1 | 1 (16) | 0 (0) | 5 (50) | 0.307 |
| Case 2 | 42 (44) | 10 (40) | 33 (78) | <0.001 |
| Case 3 | 58 (56) | 14 (53) | 37 (86) | 0.001 |
| Case 4 | 92 (91) | 25 (96) | 43 (95) | 0.633 |
| Utilize two or more approaches | ||||
| Case 1 | 4 (66) | 0 (0) | 7 (70) | 0.999 |
| Case 2 | 79 (83) | 19 (76) | 39 (92) | 0.132 |
| Case 3 | 88 (86) | 22 (84) | 41 (95) | 0.210 |
| Case 4 | 95 (94) | 24 (92) | 44 (97) | 0.570 |
Abbreviations: ENT, otolaryngologists; N/A, not available; OMFS, oral and maxillofacial surgeons; PRS, plastic and reconstructive surgeons; ZMC, zygomaticomaxillary complex.
Fig. 6.
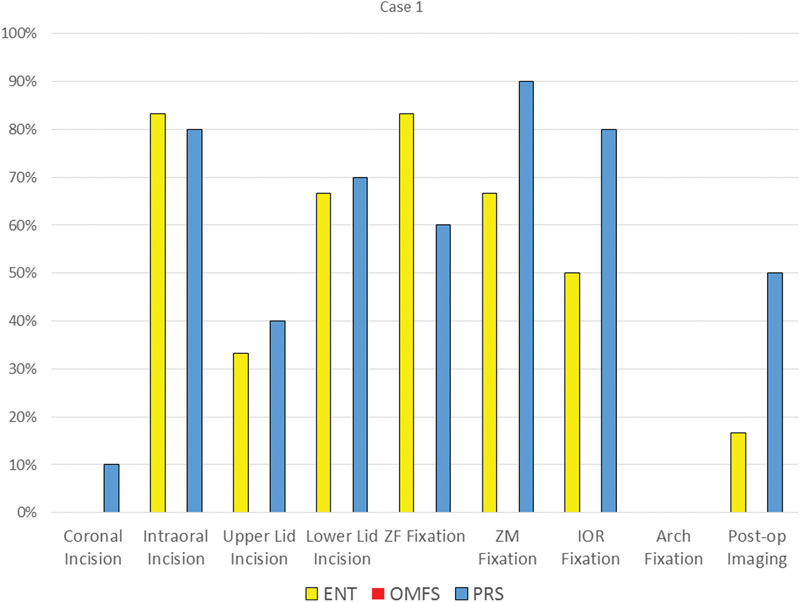
Treatment details for Case 1 (minimally displaced).
Case 2: Displaced Fracture without Diplopia
More than 90% of surgeons would treat Case 2 (93% ENT, 96% OMFS, and 91% PRS; Table 2). The most favored approach is through an intraoral incision by all specialties (ENT 74%, OMFS 77%, and PRS 84.5%); however, very few used this as their only approach. The decision to obtain postoperative imaging was favored by plastic (37%) and oral surgeons (65%). Post hoc testing revealed that more PRS surgeons would explore the orbital floor when compared against the other two specialties (p < 0.001). In addition, post hoc testing demonstrated that more PRS surgeons would fixate three or more buttresses when compared against the other two specialties (p ≤ 0.009; Fig. 7).
Fig. 7.
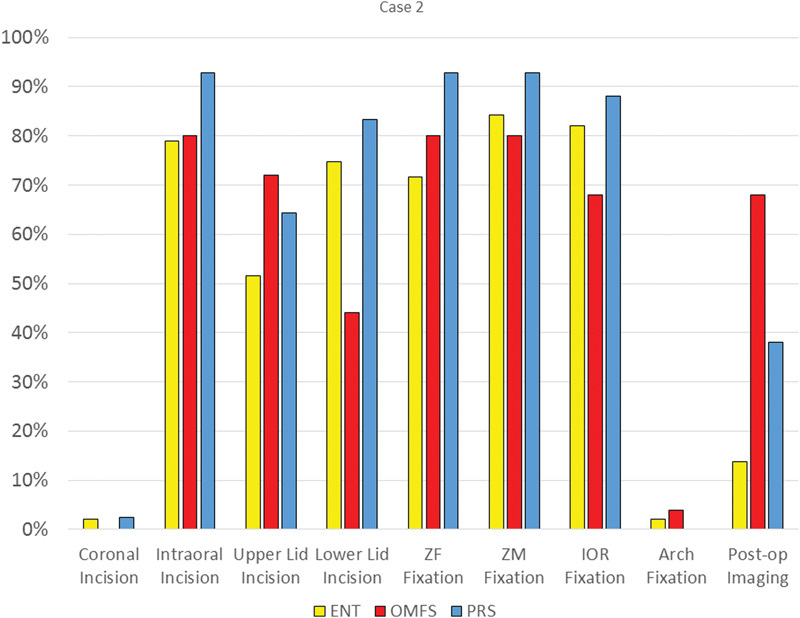
Treatment details for Case 2 (displaced without diplopia).
Case 3: Displaced Fracture with Diplopia
For Case 3, 100% ENT, 100% OMFS, and 93.5% PRS would pursue an operation (Table 2). All the specialties strongly favor multiple approaches with use of a lower eyelid incision in combination with upper eyelid and intraoral approaches. More than 90% of surgeons explored the orbital floor, and postoperative imaging was preferred by most plastic (53%) and oral (85%) surgeons. There were significant differences between specialties regarding fixation (p = 0.001); post hoc testing revealed that the PRS group was more likely to use three or more fixation points than the other specialties. There was also a (nonstatistically significant) tendency of surgeons with less than 10 years of experience to fixate three or more buttresses, regardless of specialty (p = 0.021; Fig. 8).
Fig. 8.
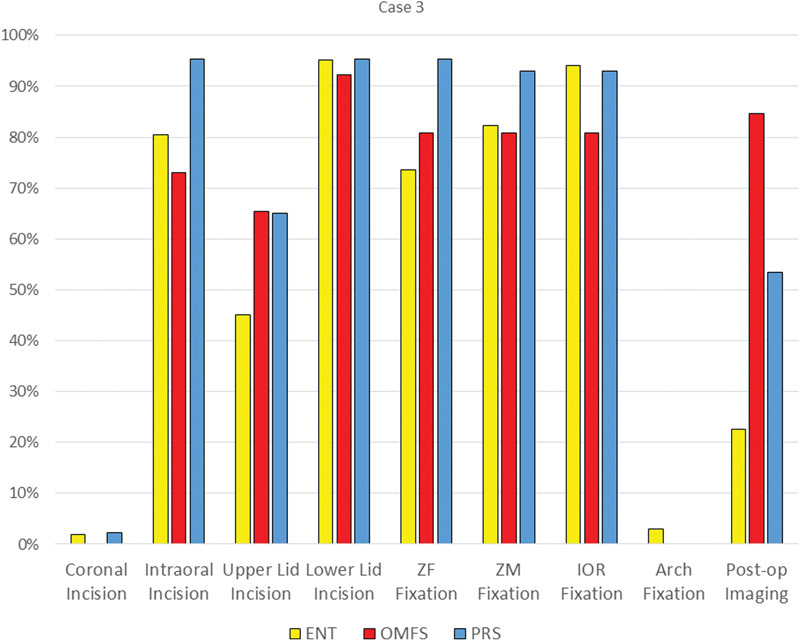
Treatment details for Case 3 (displaced with diplopia).
Case 4: Highly Comminuted Fracture
In case 4, 99% of survey respondents would recommend surgical treatment. The proportion that would explore the orbital floor and fixate three or more buttresses or utilize two or more approaches was statistically equivalent among all three specialties (Table 2). Surgeons with less than 10 years of experience were more likely to fixate three or more buttresses (p = 0.001). In this more complex fracture pattern, 63% would use a coronal incision (64% ENT, 58% OMFS, and 63% PRS). Furthermore, multiple fixation points were selected: ZF, ZM, infraorbital rim, and arch. A majority of respondents from all three specialties would obtain postoperative imaging (Fig. 9).
Fig. 9.
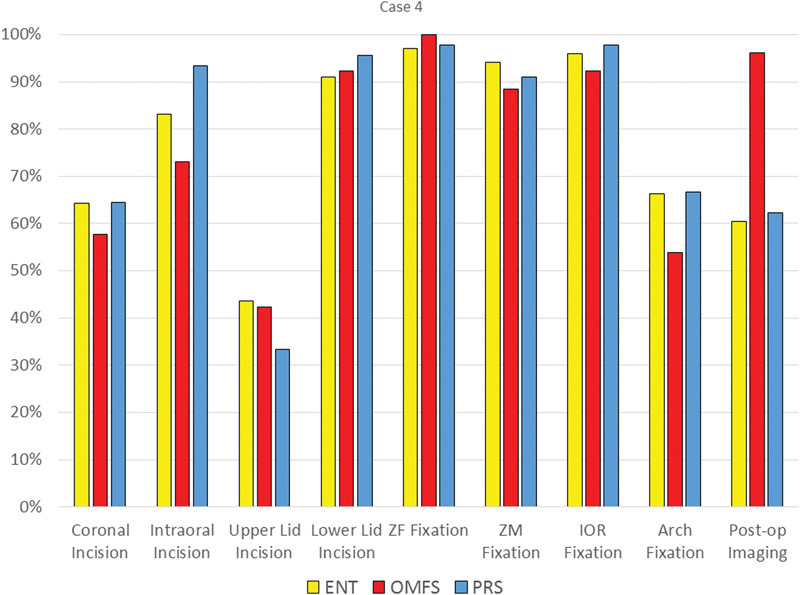
Treatment details for Case 4 (comminuted).
Incision Selection for Upper and Lower Eyelid Approach
After combining the upper eyelid approach responses for all four cases, PRS (71%) favored the lateral extension of the upper blepharoplasty incision compared with ENT (55%) and OMFS (32%; p < 0.01). For lower eyelid approaches, the transconjunctival incision was most favored by ENT (81%) compared with OMFS (67%) and PRS (60%). PRS (27%) selected the subtarsal incision significantly more than ENT (5%) or OMFS (15%; p < 0.01). There was no significant difference in preference for the subciliary incision between the three specialties (Fig. 10).
Fig. 10.
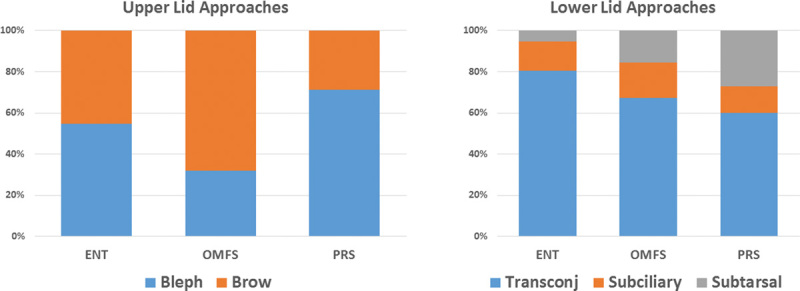
Incision selection for upper and lower eyelid approach.
Discussion
Currently, there is no consensus on ZMC fracture treatment regarding indications for surgery and the technique used. Our study demonstrates that there are significant variations within and between specialties in the treatment of ZMC fracture, confirming that management does not necessarily follow a clear standard.
Most surgeons agree that conservative treatment of ZMC fractures is appropriate in situations with no displacement of the fracture segments. If this treatment option is chosen, patients should be placed on a soft, non-chew diet for approximately 2 to 6 weeks, with close monitoring for displacement.13 If the ZMC fracture is displaced and/or the patient has enophthalmos, operative reduction and fixation is indicated. Surgical methods of ZMC fracture fixation have evolved over the years, beginning with wires for osteosynthesis.4 5 However, wire osteosynthesis is not as effective as plating systems in maintaining reduction of ZMC fractures.14 Traditional teaching recommends three-point fixation for ZMC fractures, based on biomechanical studies.15 16 However, an algorithm proposed by Ellis and Kittidumkerng recommends a step-wise process in the treatment of ZMC fractures.6 This philosophy is also reinforced by textbooks used by surgical trainees.4 17 18 19
Alternative approaches to ZMC fractures observe soft-tissue preservation and advocate a “less-is-more” approach.10 20 Ellis and Perez updated their original algorithm that advocates a sequential approach to avoid unnecessary surgical procedures that can potentially cause iatrogenic deformities.21 The goal is to achieve skeletal fixation while minimizing soft-tissue morbidity such as lower cheek descent and ectropion.6 7 The number of soft-tissue approaches and required buttresses to fixate varies depending on the type of fracture and opinion of the surgeon.22 23 24 Typically, the more comminuted high-energy ZMC fractures require wider exposure and greater fixation.7 The results of our survey confirmed this.
Different areas of the facial skeleton involved in the ZMC fracture are accessed using various approaches. The infraorbital rim and orbital floor are exposed through the lower eyelid utilizing a subtarsal, transconjunctival, or subciliary incision. The ZF suture is accessed using an upper blepharoplasty or lateral brow incision. Utilizing an intraoral approach in the gingivolabial sulcus, the ZM buttress can be reached. Some literature advocates using the intraoral approach to address the infraorbital rim, obviating the need for an eyelid incision.25 The various soft-tissue approaches are not without potential morbidity.26 A brow incision can lead to noticeable scarring. Lower eyelid exposures can result in entropion or ectropion.27 28 29 In addition, inadequate resuspension during closure results in ptosis of the malar region.30 The coronal approach is used to treat severe ZMC fractures and provides exposure to the zygomatic arch and lateral orbital rim. Potential complications include facial nerve injury, temporal fat pad injury, alopecia, and scalp necrosis.31
The challenge in ZMC fracture treatment is to balance suitable bone fixation against the potential sequelae of numerous soft-tissue approaches. No oral maxillofacial surgeons elected to operate on the minimally displaced fracture in Case 1. There was a small percentage of ENT and plastic surgeons who elected to do so and used a variety of soft-tissue approaches. An upper blepharoplasty incision was the preferred technique to approach the ZF suture among the responding surgeons. All three groups used a transconjunctival incision as their favored approach through the lower eyelid. If indicated, we prefer to access the superolateral and infraorbital rim using incisions that are concealed: upper eyelid incision and a transconjunctival approach with lateral canthotomy and inferior cantholysis. Treatment of ZMC fractures should be managed like a facial aesthetic operation and thought should be given to assess if skin incisions are necessary.
Fixation highly depends on fracture type and can include immobilizing any combination of the following five sites: ZF suture, inferior orbital rim, zygomaticosphenoid suture, ZM buttress, and zygomatic arch. While it seems obvious that stability increases with more points of fixation, this may not be necessary for all fractures. There is disagreement as to which of these four points provides the best stability when fixated is seen throughout the literature. Ellis and Kittidumkerng demonstrated that with proper reduction and stabilization of the fracture, there were no differences in the presence of postreduction displacement related to the number of fixation plates used.6 Rohner et al advocate placing a plate on the ZS suture in addition to two other points after their cadaveric biomechanical studies revealed improved structural strength compared with that of four-point fixation.32 Alternatively, one plate fixation on the ZM buttress is increasing in popularity, if the other fracture sites are reduced and stable.21 33 Hwang also demonstrated good results with one plate on the superolateral orbital rim through a lateral brow incision in 14 patients.34 Single-plate fixation is typically limited to noncomminuted ZMC fractures without ocular symptoms. ZMC fracture treatment should be tailored on a patient-by-patient basis. Every fracture is different, and these variances warrant numerous combinations of approaches and fixation methods. It appears that the surveyed population would commonly employ approaches through the mouth and eyelid for treatment of a ZMC fracture. The coronal approach was favored when the fracture was complex, requiring fixation of the zygomatic arch. It appears that the three-point fixation rule holds true for the majority of responding plastic surgeons, regardless of fracture severity. Both ENT and OMFS specialties were less inclined to fixate as many points in less comminuted or displaced fractures. The difference in opinion may be due to specialty-specific literature and surgical training.
The objective of bone fixation in ZMC fractures is to maintain reduction for both functional and aesthetic concerns. Biomechanical studies have attempted to delineate forces acting on the ZMC and how they could potentially affect fixation techniques.35 36 37 While the masseter is the main muscle causing ZMC displacement, there is debate on the extent that it truly impacts postoperative outcome. Dal Santo et al demonstrated a significant reduction in ipsilateral masseteric force with a ZMC fracture that lasts 4 to 6 weeks.38 In addition, exposure using an intraoral approach elevates masseteric attachments from the zygoma that may also influence muscle function. Postreduction asymmetry is reported in the range of 10 to 13%.6 39 This malar asymmetry is more likely due to imprecise reduction than fracture instability.
The use of absorbable plates has been advocated for fixation of ZMC fractures.40 41 Our study demonstrated that some surgeons from all specialties have used bioresorbable plates to treat ZMC fractures. Potential benefits include the absence of long-term issues with plate palpability or infection; however, biomechanical studies have demonstrated that they are not as strong as their titanium counterparts.32 42
In fractures of the ZMC, the orbital floor is always involved; however, it may not always be necessary to explore and reconstruct. Opinion varies on when treatment is indicated, and studies have developed criteria to address this question. Traditional teaching states that fracture involving greater than 50% of the orbital floor or defects measuring 1 to 2 cm2 should be explored and repaired.43 44 45 46 47 Tahernia et al determined that a change in orbital volume of 20% results in a perceptible deformity, and the 50% rule may be too conservative.44 They advise to explore and reconstruct the orbital floor with 1 cm or more of inferolateral displacement of the ZMC, as this results in an orbital volume change of 20%. Shape and position of the inferior rectus muscle has been found to be the most predictive indicator for enophthalmos.48 The usual shape of this muscle is elliptical. Rounding of the inferior rectus muscle and lying mainly within the maxillary sinus on coronal CT view indicate an increase in orbital volume, resulting in symptomatic enophthalmos.49 50 In our survey, we found that most surgeons, regardless of specialty, would explore the orbital floor in a displaced fracture, with increasing rates of exploration seen if the patient has symptomatic diplopia. Advocates of intraoperative exploration describe that the floor defect may appear small on preoperative imaging. However, after reduction of the ZMC fracture, the floor defect can be exacerbated. Our belief is that the orbital floor defect is more likely to decrease than increase after reduction of the ZMC fracture. To ensure that no critical structures are entrapped upon reduction, forced duction testing can be performed.
Postoperative imaging is commonly acquired, as indicated by our survey. We obtain a postoperative CT scan after orbital fracture reconstruction to evaluate placement of the orbital implant. Otherwise, we use an occipitomental (Waters) view X-ray film to assess reduction after ZMC repair. Intraoperative imaging is now becoming more prevalent in the treatment of ZMC fractures. Proponents indicate that they are simple to perform and help avoid secondary procedures by identifying inadequate reduction before leaving the initial operation.51 52 53 In addition to intraoperative imaging, intraoperative navigation has been used successfully in complex orbital and ZMC fractures where normal anatomy has been greatly disrupted or in bilateral injuries where there is no “normal” side for comparison.54 55 56 57
The main limitation of this study lies within the nature of the survey itself, which by necessity limited surgeons in their responses. The most commonly used approaches and fixation points were addressed in the questionnaire. Some surgeons may use approaches or techniques not addressed in our survey. The survey also represents the opinions of a small cohort of surgeons, and may in fact not be an accurate representation of contemporary practice. Although the number of respondents was quite low, there were enough responses for subanalysis comparisons. In addition, we did not address outcomes in this survey. We are unable to determine which approach resulted in better treatment outcomes.
Our practice is to only explore the orbit in patients with diplopia or CT findings showing abnormal shape and position of the inferior rectus, or if, after reduction, entrapment is encountered. In the case of minimally displaced fractures, we prefer a less invasive approach in which only necessary areas are fixated. For example, a lower eyelid incision can be avoided by using an intraoral incision for both infraorbital rim and ZM fixation.
For multiple reasons, our survey indicates that there is no consensus on the standard treatment of ZMC fractures among PRS, ENT, and OMFS surgeons, which is contrary to a recent study by Susarla et al.58 However, they excluded ENT from their analysis. For some surgeons, managing ZMC fractures can be confusing, as there are many options and opinions on treatment. Significant variability in fracture type, fixation method, and approach warrant a step-wise treatment plan. Textbooks from each of the three specialties4 17 18 19 advocate for three-point fixation, but also advocate for an individualized approach to ZMC fractures. Plastic surgery CME articles demonstrate similar thinking to that of the textbooks, in which these fractures should be treated on an individual basis, with three-point fixation not always being necessary.13 59 Our preferred approach is to use the algorithm established by Ellis and Perez.21 We use this sequential approach to treat ZMC fractures, so soft-tissue disruption is limited.
Acknowledgments
Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and Children's Discovery Institute. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
References
- 1.Bogusiak K, Arkuszewski P. Characteristics and epidemiology of zygomaticomaxillary complex fractures. J Craniofac Surg. 2010;21(4):1018–1023. doi: 10.1097/scs.0b013e3181e62e47. [DOI] [PubMed] [Google Scholar]
- 2.Marinho R O, Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral Maxillofac Surg Clin North Am. 2013;25(4):617–636. doi: 10.1016/j.coms.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 3.Ellis E III, el-Attar A, Moos K F. An analysis of 2,067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg. 1985;43(6):417–428. doi: 10.1016/s0278-2391(85)80049-5. [DOI] [PubMed] [Google Scholar]
- 4.Fonseca R J, Barber H D, Powers M P, Frost D E. Saint Louis, MO: Elsevier Health Sciences; 2013. Oral and Maxillofacial Trauma; pp. 354–450. [Google Scholar]
- 5.Rowe N, Killey H. Baltimore, MD: Williams & Wilkins; 1955. Fractures of the Facial Skeleton; pp. 205–451. [Google Scholar]
- 6.Ellis E III Kittidumkerng W Analysis of treatment for isolated zygomaticomaxillary complex fractures J Oral Maxillofac Surg 1996544386–400., discussion 400–401 [DOI] [PubMed] [Google Scholar]
- 7.Czerwinski M Martin M Lee C Quantitative comparison of open reduction and internal fixation versus the Gillies method in the treatment of orbitozygomatic complex fractures Plast Reconstr Surg 200511571848–1854., discussion 1855–1857 [DOI] [PubMed] [Google Scholar]
- 8.Choi K Y, Ryu D W, Yang J D, Chung H Y, Cho B C. Feasibility of 4-point fixation using the preauricular approach in a zygomaticomaxillary complex fracture. J Craniofac Surg. 2013;24(2):557–562. doi: 10.1097/SCS.0b013e3182700d23. [DOI] [PubMed] [Google Scholar]
- 9.Champy M, Lodde J P, Kahn J L, Kielwasser P. Attempt at systematization in the treatment of isolated fractures of the zygomatic bone: techniques and results. J Otolaryngol. 1986;15(1):39–43. [PubMed] [Google Scholar]
- 10.Fujioka M, Yamanoto T, Miyazato O, Nishimura G. Stability of one-plate fixation for zygomatic bone fracture. Plast Reconstr Surg. 2002;109(2):817–818. doi: 10.1097/00006534-200202000-00068. [DOI] [PubMed] [Google Scholar]
- 11.Holmes K D, Matthews B L. Three-point alignment of zygoma fractures with miniplate fixation. Arch Otolaryngol Head Neck Surg. 1989;115(8):961–963. doi: 10.1001/archotol.1989.01860320071021. [DOI] [PubMed] [Google Scholar]
- 12.Cardillo G My Fisher: The definitive function for the Fisher's exact and conditional test for any RxC matrix. 2010 Available at: http://www.mathworks.com/matlabcentral/fileexchange/26883. Accessed January 5, 2016
- 13.Ellstrom C L, Evans G R. Evidence-based medicine: zygoma fractures. Plast Reconstr Surg. 2013;132(6):1649–1657. doi: 10.1097/PRS.0b013e3182a80819. [DOI] [PubMed] [Google Scholar]
- 14.Rohrich R J, Watumull D. Comparison of rigid plate versus wire fixation in the management of zygoma fractures: a long-term follow-up clinical study. Plast Reconstr Surg. 1995;96(3):570–575. doi: 10.1097/00006534-199509000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Rinehart G C Marsh J L Hemmer K M Bresina S Internal fixation of malar fractures: an experimental biophysical study Plast Reconstr Surg 198984121–25., discussion 26–28 [PubMed] [Google Scholar]
- 16.Davidson J, Nickerson D, Nickerson B. Zygomatic fractures: comparison of methods of internal fixation. Plast Reconstr Surg. 1990;86(1):25–32. [PubMed] [Google Scholar]
- 17.Rodriguez E D, Losee J E, Neligan P C. New York: Elsevier Health Sciences; 2012. Plastic Surgery: Volume 3: Craniofacial, Head and Neck Surgery, Pediatric Plastic Surgery, 3rd ed; pp. 49–88. [Google Scholar]
- 18.Thorne C H. Philadelphia, PA: Wolters Kluwer Health; 2013. Grabb and Smith's Plastic Surgery, 7th ed; pp. 311–326. [Google Scholar]
- 19.Papel I D. New York: Thieme; 2009. Facial Plastic and Reconstructive Surgery, 3rd ed; pp. 945–976. [Google Scholar]
- 20.Meslemani D, Kellman R M. Zygomaticomaxillary complex fractures. Arch Facial Plast Surg. 2012;14(1):62–66. doi: 10.1001/archfacial.2011.1415. [DOI] [PubMed] [Google Scholar]
- 21.Ellis E III, Perez D. An algorithm for the treatment of isolated zygomatico-orbital fractures. J Oral Maxillofac Surg. 2014;72(10):1975–1983. doi: 10.1016/j.joms.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Langsdon P R, Knipe T A, Whatley W S, Costello T H. Transconjunctival approach to the zygomatico-frontal limb of orbitozygomatic complex fractures. Facial Plast Surg. 2005;21(3):171–175. doi: 10.1055/s-2005-922855. [DOI] [PubMed] [Google Scholar]
- 23.Rohrich R J, Janis J E, Adams W P Jr. Subciliary versus subtarsal approaches to orbitozygomatic fractures. Plast Reconstr Surg. 2003;111(5):1708–1714. doi: 10.1097/01.PRS.0000054209.18400.4E. [DOI] [PubMed] [Google Scholar]
- 24.Yonehara Y, Hirabayashi S, Tachi M, Ishii H. Treatment of zygomatic fractures without inferior orbital rim fixation. J Craniofac Surg. 2005;16(3):481–485. doi: 10.1097/01.scs.0000157308.39420.74. [DOI] [PubMed] [Google Scholar]
- 25.de Souza Carvalho A C, Pereira C C, Queiroz T P, Magro-Filho O. Intraoral approach to zygomatic fracture: modified technique for infraorbital rim fixation. J Craniofac Surg. 2012;23(2):537–538. doi: 10.1097/SCS.0b013e3182418ea6. [DOI] [PubMed] [Google Scholar]
- 26.Manson P N, Clark N, Robertson B, Crawley W A. Comprehensive management of pan-facial fractures. J Craniomaxillofac Trauma. 1995;1(1):43–56. [PubMed] [Google Scholar]
- 27.Ridgway E B, Chen C, Lee B T. Acquired entropion associated with the transconjunctival incision for facial fracture management. J Craniofac Surg. 2009;20(5):1412–1415. doi: 10.1097/SCS.0b013e3181aee3ee. [DOI] [PubMed] [Google Scholar]
- 28.Ridgway E B, Chen C, Colakoglu S, Gautam S, Lee B T. The incidence of lower eyelid malposition after facial fracture repair: a retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg. 2009;124(5):1578–1586. doi: 10.1097/PRS.0b013e3181babb3d. [DOI] [PubMed] [Google Scholar]
- 29.Raschke G F, Rieger U M, Bader R D. et al. The zygomaticomaxillary complex fracture - an anthropometric appraisal of surgical outcomes. J Craniomaxillofac Surg. 2013;41(4):331–337. doi: 10.1016/j.jcms.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Lee E I, Mohan K, Koshy J C, Hollier L H Jr. Optimizing the surgical management of zygomaticomaxillary complex fractures. Semin Plast Surg. 2010;24(4):389–397. doi: 10.1055/s-0030-1269768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alvi A, Carrau R L. The bicoronal flap approach in craniofacial trauma. J Craniomaxillofac Trauma. 1996;2(2):40–55. [PubMed] [Google Scholar]
- 32.Rohner D Tay A Meng C S Hutmacher D W Hammer B The sphenozygomatic suture as a key site for osteosynthesis of the orbitozygomatic complex in panfacial fractures: a biomechanical study in human cadavers based on clinical practice Plast Reconstr Surg 200211061463–1471., discussion 1472–1475 [DOI] [PubMed] [Google Scholar]
- 33.Kim J H, Lee J H, Hong S M, Park C H. The effectiveness of 1-point fixation for zygomaticomaxillary complex fractures. Arch Otolaryngol Head Neck Surg. 2012;138(9):828–832. doi: 10.1001/archoto.2012.1815. [DOI] [PubMed] [Google Scholar]
- 34.Hwang K. One-point fixation of tripod fractures of zygoma through a lateral brow incision. J Craniofac Surg. 2010;21(4):1042–1044. doi: 10.1097/SCS.0b013e3181e48607. [DOI] [PubMed] [Google Scholar]
- 35.O'Hara D E DelVecchio D A Bartlett S P Whitaker L A The role of microfixation in malar fractures: a quantitative biophysical study Plast Reconstr Surg 1996972345–350., discussion 351–353 [DOI] [PubMed] [Google Scholar]
- 36.Deveci M, Eski M, Gurses S, Yucesoy C A, Selmanpakoglu N, Akkas N. Biomechanical analysis of the rigid fixation of zygoma fractures: an experimental study. J Craniofac Surg. 2004;15(4):595–602. doi: 10.1097/00001665-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Hanemann M Jr, Simmons O, Jain S, Baratta R, Guerra A B, Metzinger S E. A comparison of combinations of titanium and resorbable plating systems for repair of isolated zygomatic fractures in the adult: a quantitative biomechanical study. Ann Plast Surg. 2005;54(4):402–408. doi: 10.1097/01.sap.0000151484.59846.62. [DOI] [PubMed] [Google Scholar]
- 38.Dal Santo F, Ellis E III, Throckmorton G S. The effects of zygomatic complex fracture on masseteric muscle force. J Oral Maxillofac Surg. 1992;50(8):791–799. doi: 10.1016/0278-2391(92)90267-4. [DOI] [PubMed] [Google Scholar]
- 39.Zingg M, Laedrach K, Chen J. et al. Classification and treatment of zygomatic fractures: a review of 1,025 cases. J Oral Maxillofac Surg. 1992;50(8):778–790. doi: 10.1016/0278-2391(92)90266-3. [DOI] [PubMed] [Google Scholar]
- 40.Eppley B L. Zygomaticomaxillary fracture repair with resorbable plates and screws. J Craniofac Surg. 2000;11(4):377–385. doi: 10.1097/00001665-200011040-00019. [DOI] [PubMed] [Google Scholar]
- 41.Singh V, Sharma B, Bhagol A. Evaluating the applicability of a biodegradable osteosynthesis plating system in the management of zygomatico-maxillary complex fractures. Otolaryngol Head Neck Surg. 2011;145(6):924–929. doi: 10.1177/0194599811421750. [DOI] [PubMed] [Google Scholar]
- 42.Kang I G, Jung J H, Kim S T, Choi J Y, Sykes J M. Comparison of titanium and biodegradable plates for treating midfacial fractures. J Oral Maxillofac Surg. 2014;72(4):7620–7.62E6. doi: 10.1016/j.joms.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 43.Yab K, Tajima S, Ohba S. Displacements of eyeball in orbital blowout fractures. Plast Reconstr Surg. 1997;100(6):1409–1417. doi: 10.1097/00006534-199711000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Tahernia A, Erdmann D, Follmar K, Mukundan S, Grimes J, Marcus J R. Clinical implications of orbital volume change in the management of isolated and zygomaticomaxillary complex-associated orbital floor injuries. Plast Reconstr Surg. 2009;123(3):968–975. doi: 10.1097/PRS.0b013e318199f486. [DOI] [PubMed] [Google Scholar]
- 45.Hawes M J, Dortzbach R K. Surgery on orbital floor fractures. Influence of time of repair and fracture size. Ophthalmology. 1983;90(9):1066–1070. doi: 10.1016/s0161-6420(83)80049-9. [DOI] [PubMed] [Google Scholar]
- 46.Gart M S, Gosain A K. Evidence-based medicine: orbital floor fractures. Plast Reconstr Surg. 2014;134(6):1345–1355. doi: 10.1097/PRS.0000000000000719. [DOI] [PubMed] [Google Scholar]
- 47.Christensen B J, Zaid W. Inaugural survey on practice patterns of orbital floor fractures for American oral and maxillofacial surgeons. J Oral Maxillofac Surg. 2016;74(1):105–122. doi: 10.1016/j.joms.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 48.Schouman T, Courvoisier D S, Van Issum C, Terzic A, Scolozzi P. Can systematic computed tomographic scan assessment predict treatment decision in pure orbital floor blowout fractures? J Oral Maxillofac Surg. 2012;70(7):1627–1632. doi: 10.1016/j.joms.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 49.Chiasson G, Matic D B. Muscle shape as a predictor of traumatic enophthalmos. Craniomaxillofac Trauma Reconstr. 2010;3(3):125–130. doi: 10.1055/s-0030-1262954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Banerjee A, Moore C C, Tse R, Matic D. Rounding of the inferior rectus muscle as an indication of orbital floor fracture with periorbital disruption. J Otolaryngol. 2007;36(3):175–180. [PubMed] [Google Scholar]
- 51.Heiland M, Schulze D, Blake F, Schmelzle R. Intraoperative imaging of zygomaticomaxillary complex fractures using a 3D C-arm system. Int J Oral Maxillofac Surg. 2005;34(4):369–375. doi: 10.1016/j.ijom.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 52.Wilde F, Lorenz K, Ebner A-K, Krauss O, Mascha F, Schramm A. Intraoperative imaging with a 3D C-arm system after zygomatico-orbital complex fracture reduction. J Oral Maxillofac Surg. 2013;71(5):894–910. doi: 10.1016/j.joms.2012.10.031. [DOI] [PubMed] [Google Scholar]
- 53.Stanley R B Jr. Use of intraoperative computed tomography during repair of orbitozygomatic fractures. Arch Facial Plast Surg. 1999;1(1):19–24. doi: 10.1001/archfaci.1.1.19. [DOI] [PubMed] [Google Scholar]
- 54.Gellrich N C, Schramm A, Hammer B. et al. Computer-assisted secondary reconstruction of unilateral posttraumatic orbital deformity. Plast Reconstr Surg. 2002;110(6):1417–1429. doi: 10.1097/01.PRS.0000029807.35391.E5. [DOI] [PubMed] [Google Scholar]
- 55.Bell R B, Markiewicz M R. Computer-assisted planning, stereolithographic modeling, and intraoperative navigation for complex orbital reconstruction: a descriptive study in a preliminary cohort. J Oral Maxillofac Surg. 2009;67(12):2559–2570. doi: 10.1016/j.joms.2009.07.098. [DOI] [PubMed] [Google Scholar]
- 56.Markiewicz M R, Dierks E J, Potter B E, Bell R B. Reliability of intraoperative navigation in restoring normal orbital dimensions. J Oral Maxillofac Surg. 2011;69(11):2833–2840. doi: 10.1016/j.joms.2010.12.043. [DOI] [PubMed] [Google Scholar]
- 57.Wilde F, Schramm A. Intraoperative imaging in orbital and midface reconstruction. Facial Plast Surg. 2014;30(5):545–553. doi: 10.1055/s-0034-1393700. [DOI] [PubMed] [Google Scholar]
- 58.Susarla S M, Mundinger G S, O'Brien-Coon D. et al. Does training background influence decision-making in the management of zygomaticomaxillary complex fractures? J Oral Maxillofac Surg. 2016;74(5):995–1012. doi: 10.1016/j.joms.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 59.Evans B G Evans G R MOC-PSSM CME article: zygomatic fractures Plast Reconstr Surg 2008121(1, Suppl):1–11. [DOI] [PubMed] [Google Scholar]


