Abstract
Despite national guidelines for regular physical activity, most adolescents are not physically active. Schools serve an estimated 60 million youth and provide an educational environment to meet the current physical activity guidelines. The obesity epidemic and chronic disease comorbidities associated with physical inactivity are not likely to be reversed without a strong contribution from local schools. This article describes how a structured peer-mentoring method provides a feasible, flexible, and tailored means to meet the current guidelines for best practice in a school setting. Structured peer mentoring using trained high school mentors to support behavior change in younger peers is an innovative method to meeting the School Health Guidelines to Promote Healthy Eating and Physical Activity. Through structured peer mentoring, adolescents are provided consistent social support in a caring and personalized manner. This support builds skills and competencies enhancing self-efficacy to sustain a lifetime of physical activity behavior.
Keywords: exercise, mentoring, obesity, best practices/practice guidelines, health education, school nursing
Despite national guidelines for regular physical activity, most adolescents are not physically active (Centers for Disease Control and Prevention [CDC], 2011). Current guidelines and scientific evidence for best practices to prevent obesity and obesity comorbidities such as heart disease, cancers, and diabetes recommend at least 60 min of moderate to vigorous daily physical activity (CDC, 2011; Institute of Medicine, 2012). A review of 50 studies focused on youth concluded that regular physical activity improves academic achievement, academic behavior, and cognitive skills including concentration and memory (CDC, 2010). Despite these health and academic benefits, recent data suggest that only 27% of high school students reported 60 min of daily physical activity every day during the past week, while 14% reported no physical activity in the past week, and less than half (48%) of high school students attend any physical education classes in the average week (CDC, 2010, 2013). These data indicate that most adolescents are not meeting the recommended daily physical activity guidelines. With one in three school-aged youth currently overweight or obese (Ogden, Carroll, Kit, & Flegal, 2014), obesity prevention through improving physical activity is a top priority (American Academy of Pediatrics, 2006; U.S. Department of Health and Human Services [USDHHS], 2008).
Schools serve an estimated 60 million youth and provide a critical setting to build the foundation of skills needed to help youth meet the current physical activity guidelines (U.S. Department of Education, National Center for Education Statistics, 2015). Most children attend either public or private schools and spend the majority of their waking hours in school settings. At the same time, schools are facing increasing demands on instructional time for core subject areas to improve standardized test scores (Corcoran & Silander, 2009; Farbman, 2015; Fleischman & Heppen, 2009). As a result, physical education classes, recess, and activity breaks are frequently reduced or eliminated during the school day. In 2006, only 2% of high schools provided daily physical education for students in all grades (Lee, Burgeson, Fulton, & Spain, 2007). As recently as 2013, only 20% of 12th-grade students attended daily physical education classes, far below recommendations (CDC, 2013).
Most schools rely on health education and/or physical education programs delivered by teachers to provide the skills and motivation for adolescents to engage in physical activity. In general, these school-based programs have not resulted in sustainable behavior change. Consequently, school nurses and other health professionals serving school-aged youth frequently seek alternative solutions to promote behavior change and impact health outcomes. The purpose of this article is to describe a structured peer-mentoring method to impact physical activity behavior change among adolescents. Structured peer mentoring using trained high school mentors to lead and support the behavior change in younger peers is a responsive and tailored method to meeting the School Health Guidelines to Promote Healthy Eating and Physical Activity.
Literature Review
During adolescence, teenagers spend less time with family members and more time with peers. The powerful influence that peers have on role modeling and supporting behaviors of others in their peer group is well recognized (Karcher, 2009; Substance Abuse and Mental Health Services Administration [SAMHSA], 2014). Adolescents tend to view their own peers as being more credible, having a better understanding of the concerns of young people, have a sense of responsibility to their friendship group, and are more likely to model the behaviors of peers than adults (DuBois & Karcher, 2014; Karcher, 2009; Smith, 2011).
Peer-mentoring programs have been utilized to strengthen interpersonal connectedness between adolescents, their friends, and schools (Karcher, 2012). Peer mentoring further strengthens connectedness to oneself both now and in the future (Karcher, 2012). Feeling a sense of connected to others can be best understood as what one does and does not care about such as friendship groups and school friendship networks. Peer mentors build and strengthen social networks while enhancing school connectedness for adolescents.
Social networks are links between people that provide social support (Keller & Blakeslee, 2014). Social networks among peers provide emotional, informational, and appraisal support that creates a sense of psychological safety within the peer group, resulting in higher motivation to change behavior and sustain behavioral change. Learning, behavior self-efficacy, and behavior change are facilitated when people have a sense of psychological safety or the perception that attempts to change behavior can occur without fear or embarrassment (Heaney & Israel, 2008). For adolescents, advantages of peer mentoring include enhanced learning and behavioral change support resulting from the perceived social support and psychological safety promoted by peer-to-peer mentoring.
Structured Peer Mentoring to Support Physical Activity
Recent developments in program-based peer mentoring have resulted in the emergence of structured mentoring programs to promote behavior change (Karcher & Hansen, 2014). Structured peer mentoring programs are goal directed and skill building (Karcher & Hansen, 2014). Strengths of structured peer-mentoring programs are that the mentee learns behaviors from the role modeling, personalized support for behavior change, and guidance provided from peer mentors (Hamilton & Hamilton, 1992). In structured peer mentoring, a clearly defined curriculum is delivered on a regular schedule. Structured peer mentoring retains the social support and developmental benefits of peer mentoring while adding behaviorally focused instruction.
There are numerous advantages to the use of peer mentors in structured mentoring programs promoting physical activity among adolescents. Peer mentors empower teens by the strengthened social network and social support to plan, regulate, and evaluate their personal activity plan, thus building self-efficacy to engage in regular activity. Peer mentors can focus on unique healthy lifestyle challenges to engaging in regular physical activity such as a lack of organized sports and recreational facilities prevalent in many low-resource areas. Peer mentors provide personal support and guidance to these overcoming environmental, social, and psychological barriers, leading to improved adherence to physical activity and increased peer resources to sustain physical activity. Serving as role models, peer mentors improve their own lifestyle behaviors, providing a dual effect of the intervention (SAMHSA, 2014; Smith & Holloman, 2013).
Through structured peer mentoring, physical activity behavior as a social norm is strengthened by connectedness with others who care about being physically active. Outcome expectations or the perceived value one has about engaging in physical activity is enhanced by engagement with one’s mentor and peer social group or network. Because teenagers prefer informal sharing of information among friends and peer groups, receiving structured physical activity and exercise information from those closer in age via structured peer mentoring capitalizes on this innate preference during the adolescent years. For adolescents lacking exercise self-efficacy, the social support, guidance, and role modeling provided through structured peer mentoring and the broader friendship social networks resulting from mentoring groups strengthens their personal beliefs about their own capacity to begin and ultimately sustain daily physical activity and exercise.
Health educators and school-based health education programs have used Social Cognitive Theory (SCT) to develop robust programs leading to behavioral change among individuals. Two of the most important lessons that SCT stresses in structured peer mentoring are that age-appropriate cognitive development allows for self-reflection and an awareness of what others are thinking (Noam, Malti, & Karcher, 2014). SCT also recognizes that human behavior is shaped by a dynamic interaction between the individual and the environmental influences (McAlister, Perry, & Parcel, 2008). Broadly speaking, structured peer mentoring to support physical activity addresses SCT key constructs of psychosocial determinants, self-regulation, and environmental determinants affecting individual behavior change. Psychosocial determinants include outcome expectancies and exercise self-efficacy. Outcome expectations correspond to social norms and are a function of a social outcome or how a person will feel about them if they exercise or do not exercise (McAlister et al., 2008).
Self-regulation includes goal setting, self-monitoring, overcoming barriers, time management, self-reward, and social support. For mentors and mentees, establishing, experiencing, and strengthening important relationships through the mentoring process and program helps develop stronger social skills, build exercise self-efficacy, and overcome perceived barriers by personalized empathy, praise, and attention (Karcher, 2012). Through personal praise and support from a mentor, mentees set more realistic goals, self-monitoring plans, and time management plans to engage in physical activity. Social perspective taking common during adolescence, one of collaboration and acting out of shared needs and concerns for “us,” helps to strengthen interpersonal negotiation strategies that help mentees achieve realistic goal setting, self-regulation strategies, and time management skills (Selman & Schultz, 1990). Social perspective taking further strengthens the ongoing structured peer-mentoring relationships (Karcher, 2012).
Structured peer mentoring provides mentees with opportunities to interact with others outside their immediate peer group or neighborhood. By using peer mentors from the same local community, personal plans to overcome barriers and challenges such as the lack of exercise equipment at home, the lack of recreational facilities, or taking advantage of opportunities present while at school are jointly developed. These personal plans are useful for sustaining goal-directed physical activity behavior change. In addition, through peer mentoring, engaging in physical activity may be a form of interpersonal connectedness with peer mentors, groups, and friendship networks while at school or in the community that leads to sustainability of the behavior over time.
Although SCT recognizes how the external environment shapes behavior, emphasis is also placed on how the individual’s personal ability to alter environments to suit purposes they devise for themselves such as altering environments to engage in physical activity (McAlister et al., 2008).
External environments are one’s home, neighborhood, and school. Students actively seek and create supportive environments that provide opportunities for physical activity. Structured peer-mentoring programs empower youth by providing them with resources missing from their neighborhoods and communities (Deutsch, Lawrence, & Henneberger, 2014) SCT has been used extensively for determinants of physical activity and was used to guide the development of our proposed method (see Figure 1) to impact physical activity behavior change (Hortz & Petosa, 2006; Plotnikoff, Costigan, Karunamuni, & Lubans, 2013).
Figure 1.
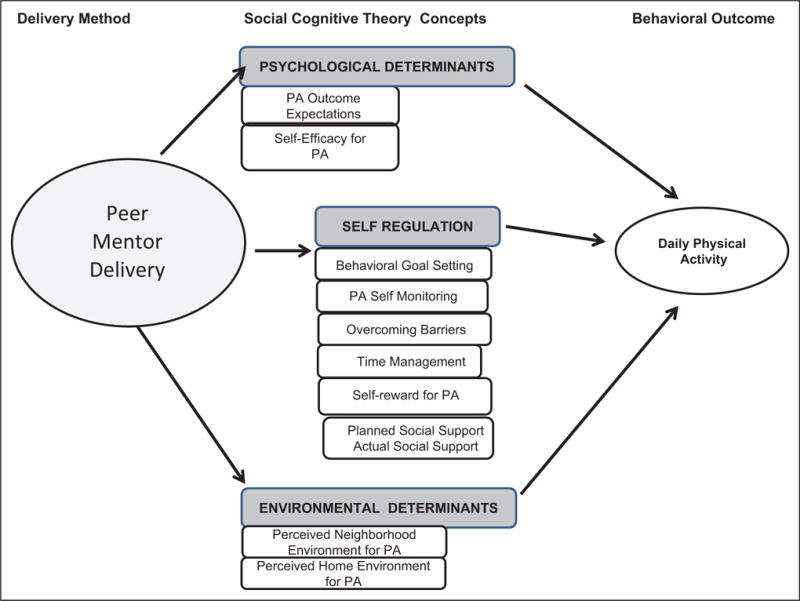
Structured peer-mentoring method with social cognitive theory concepts to impact physical activity.
A School-Based Structured Peer-Mentoring Method
Developed in collaboration with school partners and stakeholders in rural underresourced and underserved communities, our structured peer-mentoring method to promote physical activity was developed and tested over the course of six intervention studies completed over the past 15 years (see Table 1). Funded primarily by the National Institutes of Health and the Centers for Disease Control and Prevention, the authors conducted two studies testing the feasibility, acceptability, and outcomes resulting from training peer mentors to deliver a school-based health curriculum to youth and four studies to develop and refine a physical activity curriculum.
Table 1.
Preliminary Studies for Structured Peer-Mentoring Method for Physical Activity.
| Authors (year) |
Sample, Setting, Design | Variables of Interest | Key Results |
|---|---|---|---|
| Smith (2011) |
n = 72 children n = 35 peer mentors 8-session curriculum School-based (after-school) Pretest–posttest design Attention control and intervention group comparisons |
Physical Activity (PA) Attitudes Self-Efficacy toward PA Perceived support for PA Intention to be PA Body mass index (BMI) percentile |
Mentor Group: Mean change in BMI %—0.38. Improved: Attitudes toward PA (+0.29) Self-efficacy toward PA (+1.50) Perceived support to be PA (+0.74). Peer mentors delivering curriculum is feasible. Attention control: Mean change in BMI% was +0.07. Mean decreases in variables of interest |
| Smith and Holloman (2013) |
n = 160 children n = 32 peer mentors 8-session curriculum School-based randomized controlled trial (RCT) 8-session curriculum School-based comparison group was teacher led Pretest–posttest design |
Dietary behaviors PA behaviors Blood pressure (BP) BMI Mediators: nutritional knowledge, attitudes, perceived support, self-efficacy, intentions |
Mentor group: Increased PA behavior (p = .04). Marginal decrease in BMI (p = .06) Medium effect size (ES): Current Eating Behavior (ES = .57). Improved diastolic BP (ES = .56). Perceived Support (ES = .60). Teacher group. No improved behavioral or health outcomes Other comparisons: High retention rates (92%) Greater number of sessions attended resulted in better outcomes |
| Hortz et al. (2009) |
n = 15 Appalachian high schools with 602 9th graders and 422 12th graders included Needs Assessment to compare to current physical activity guidelines. Descriptive, cross-sectional study |
PA behavior over the past 7 days | Only 13.9% engaged in vigorous PA at least 3 days/week. Only 37% engaged in moderate PA at least 5 days/week. For students meeting current guidelines, 14% did so through organized sports and 12% used physical education classes |
| Winters and Petosa (2001) | n = 143 students in Appalachian high schools. Two group RCT, pretest and posttest design | Frequency of PA Self-regulation of PA Social situation for PA PA outcome expectations PA self-efficacy |
10-session dose led to best outcomes. Teacher retention rate was 100%. Program increased self-regulation. Comparisons: Intervention group increased PA from 1.29 days/week to 2.35 days/week (p < .01). Comparison group PA decreased from pretest to posttest (p = .05) |
| Hortz and Petosa (2008) | n = 363 students in two rural Appalachian high schools; two group-controlled, 10-session intervention trial with pretest and posttest design | Rates of moderate and vigorous physical exercise Gender comparisons Self-regulation Social situation |
At baseline, rate of exercise was low in both the groups. Nearly all students did not meet recommended daily exercise requirements. Intervention group: Increased moderate PA by 2.05 days/week (p = .025). Intervention increased self-regulation skills and social situation. Control group: 10% decrease in daily exercise. Other comparisons: No gender differences, regardless of group |
| Stevens and Petosa (2006) | n = 4 Appalachian high schools with 422 participating students; nonequivalent comparison group design (3 intervention school/1 comparison school). Nine-session PA curriculum. Eligible students were those who did not engage in sports or sports teams | Rates of weekly PA (moderate and vigorous) Self-regulation Social Support |
Teacher noncompliance with intervention protocols led to the loss of 26 participants. Intervention: Explained greater portion of variance at two of the three intervention schools. Intervention was partially effective at impacting moderate PA supporting need for 10 sessions. Regression models explained 24–78% of variance within intervention schools. Self-regulation and social support mediated changes in PA. No changes in vigorous PA found |
These six studies revealed that SCT and specifically self-regulation, social support, and behavioral self-efficacy variables are strongly related to moderate and vigorous physical activity (Hortz & Petosa, 2008; Winters & Petosa, 2001). The use of trained peer mentors lead to physical activity behavior change and better health outcomes in mentees, compared to the same curriculum being delivered to classroom teachers (Smith, 2011; Smith & Holloman, 2013). Mentored groups achieved improved blood pressure and body mass index outcomes, compared to teacher-led groups (Smith, 2011). The structured peer-mentoring method increased self-regulation of physical activity, and a 10-lesson dose led to the greatest improvement in moderate and vigorous daily physical activity, compared to a shorter eight-session delivery (Stevens & Petosa, 2006). Reinforcement activities via homework assignments provide weekly consistency of skills and focus on the application and refinement of self-regulation skills applied to the initiation and maintenance of physical activity.
Implementing a Structured Peer-Mentoring Program
Based on our experience, we offer the following general steps to consider when establishing a structured peer-mentoring program (see Figure 2). The first step is to secure a health behavior change curriculum. The curriculum should have clear behavioral objectives and provide concise information to support motivation to change physical activity. The curriculum should employ behavioral strategies and skills deemed valuable to personal health behavior change. Planned educational activities should be designed to take advantage of the strengths of peer mentoring. Specifically, activities should emphasize social interaction, personal tailoring, and continuous review of personal progress during the behavior change progress.
Figure 2.
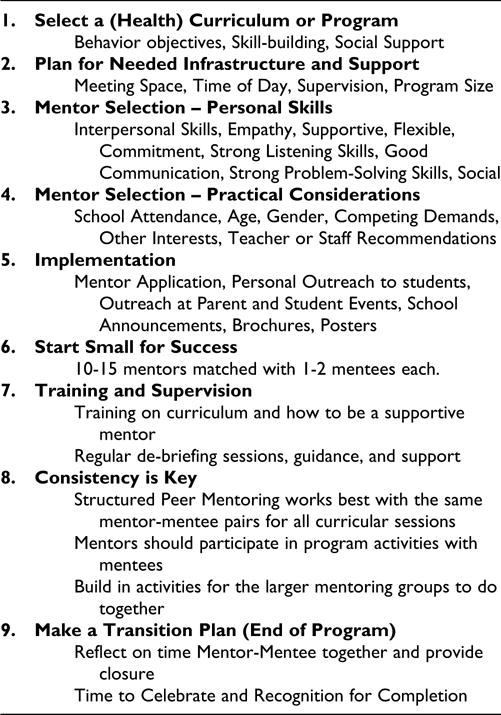
Steps to implement a school-based structured peer-mentoring program.
The next step is to consider school infrastructure and support. Meeting space and time of day are important. Support staff will be needed, such as a school coordinator, liaison, and administrative helpers. The projected size of the program and budgetary decisions need to be considered early on. Schools should plan for the projected number of peer mentors and mentees. One driving force that impacts these early decisions is transportation. Peer mentors and mentees must be able to get to and from the school for sessions or meetings. Transportation issues that result in missed meetings can be hurtful to the mentor–mentee relationship and problematic for achieving program goals. To overcome these concerns, many schools incorporate the mentoring program into the regular school day during study hall periods, lunch periods, or a regular class period such as a health class.
Because peer mentors work directly with mentees, there are certain characteristics that will help them thrive in the mentor role. Important traits for peer mentors include strong interpersonal skills, strength of character, empathy of others, supportive and flexible, commit to projects and people, skilled in making friends, good communication, strong listening skills, strong problem-solving skills, and has fun with others in structured and unstructured settings (Karcher, 2012). The best peer mentors may not be those who are already the “high achievers” or those who are most successful in school.
It might be beneficial to seek out possible peer mentors as students who are high-quality students who have less competing interests or outside obligations that might embrace the opportunity to participate as a mentor and benefit from the experience. Many successful peer mentors have been those who receive average or passing grades but regularly attend school. Consistent attendance in school indicates a consistent presence in and connectedness to school; students who regularly attend school might be better equipped to build stronger relationships with their mentees (Karcher, 2012).
Other factors to consider are age and year in school. Ideally, a peer mentor should be about 2 years older than their assigned mentee. This gap is considered important for maintaining boundaries in the relationship (Karcher, 2012). We have found that, due to competing demands and school adjustment concerns, 10th and 11th graders typically make ideal peer mentors for mentoring programs taking place during the academic year.
In order to build trust and positive relationships with their mentees, most prospective peer mentors are typically outgoing and social. They are often described by others as having a positive outlook, wanting to help others, and empathic. It would also be important to seek possible peer mentors who feel a strong sense of connectedness to their friends and school. One indicator of connectedness to one’s schools is overall performance in school.
How you recruit peer mentors will depend on the size and scope of your program. It is best to start small with 10–15 peer mentors matched with one to two mentees each. As with any newly implemented program, expect some glitches along the way so starting small will facilitate a smoother program implementation. Some suggestions for recruitment include information sharing at parent orientation events, brochures and posters in school, school announcements, in-class announcements, and personal outreach to targeted students. A key component of peer mentor recruitment is to have each prospective peer mentor complete a Mentor Application. The Mentor Application should include contact information, preferred mentoring day and time, preferred gender match, what is unique about them, why they want to be a mentor, their hobbies and interests, activities they like to do, favorite subjects in school, and their least favorite subjects in school. In addition, you may ask for a reference from a teacher, coach, or counselor as part of the application. This application may be used as a tool to match program participants to mentors as well as screen potential mentors for selection.
Training and supervision are critical components of peer mentoring. Training begins with prematch activities but continues during the program at regular meetings with mentors, such as brief debriefing sessions as well as guidance and support during mentoring sessions. To be effective peer mentors, teens need training on how to be supporting mentors as well as curriculum content training. Peer mentor training should be structured to cover important program responsibilities and how to build and sustain an effective mentoring relationship with a mentee. To assure program effectiveness, the main role of peer mentors is to consistently attend all program sessions and actively participate in program activities with their assigned mentees. These critical responsibilities build the trusting relationship that is necessary for successful peer mentoring program delivery. Other mentor program responsibilities include informing program staff if unable to attend a session (in advance), staying on task, being respectful, modeling behaviors, focusing on the mentee by giving the mentee their full attention during the sessions, helping mentee complete program activities, and report on activities or provide feedback during debriefing sessions.
Peer mentors should also be trained on whom to seek out for assistance during and after any session for help and guidance. Important mentoring topics to discuss during mentor training include what is mentoring; how to be a good listener, how to handle crises or the unexpected, how to break the ice, and getting their mentee to share; building trust; offering praise and reinforcement; offering constructive criticism; conflict resolution; problem-solving steps; and transition of the mentoring relationship or saying good-bye (Karcher, 2012).
Once mentoring training is completed, peer mentors should be trained on the school’s specific physical activity program and its delivery. To strengthen program fidelity, peer mentors should be provided detailed and structured outlines of each lesson or session’s activities including instructions, materials needed, and time allocated to complete the activity. In addition, a brief meeting with the peer mentors prior to each lesson or session to problem solve or answer any questions about the planned activities is essential. We have found that a brief 10- to 15-min debriefing meeting at the conclusion of each mentoring session for program staff to meet with the peer mentors is beneficial. During these debriefing sessions, the peer mentors may share program delivery challenges, share program delivery successes, offer suggestions for improvement, and provide guidance and support to other peer mentors. The debriefing meetings may be a time when program staff may log any community service credit or provide any incentive payment (if provided).
Peer mentors should be supportive of other peer mentors. As part of a budding social network, many mentoring groups meet in a large school space together, such as a gymnasium or a cafeteria. Seeing the presence of other mentoring groups offers a sense of security to both peer mentors and mentees. Having all mentoring groups meet in the same large space also facilitates guidance and supervision by program staff. We have found that in a large school space, it is best to ask mentor–mentee triads/dyads to work together and at a distance from other groups while remaining visible to other groups. Larger groupings may lead to distractions among all within the room and hinder implementation of the program as well as program fidelity.
Peer mentors or mentees may not be able to attend every session; a plan to handle absenteeism of both mentors and mentees should be drafted. If a peer mentor is absent, you may place their assigned mentees with other mentors for the session. If a peer mentor’s assigned mentees are absent, you can ask the mentor to assist other mentoring groups or be a program assistant or lead mentor for the session. As program assistant or lead mentor, they would help all groups or program staff in facilitating program delivery. Strategies to enhance program attendance include offering a refreshments; planning activities that span several sessions; and integrating activities from other curricula such as health, science, or math. Since many students seek community service opportunities, many schools now require a requisite number of community service hours for graduation. Offering community service hours to peer mentors should be considered. Community service hours strengthen college applications, job applications, and professional resumes. Often students who served as mentors are recruited based on the professional development and leadership experience gained from mentoring others.
Finally, a transition plan should be established. We have found that how the structured mentoring ends is critical. The transition plan should provide both the peer mentors and the mentees an opportunity to reflect on their relationship and walk away with positive feelings and memories. This phase should provide closure and opportunities for learning for both parties (Karcher, 2012). Many programs build in an end of program Celebration Session to allow for closure.
Implications for the School Nurse
Considering all causes of morbidity and mortality in the United States, modifiable behaviors are the leading cause of comorbidities of Americans. Two behaviors, physical inactivity and unhealthy eating, are largely responsible for the rapid rise in and prevalence of overweight and obesity among our school-age youth. In addition to substantial well-documented health disparities, overweight and obese youth have a higher prevalence of school problems including poor social skills, poor academic performance, and mental health concerns such as anxiety, depression, and suicide attempts (Carey, Singh, Brown, & Wilkinson, 2015; Serrano-Gonzalez, McConnel, Bokhary, Oden, & Lopez, 2015). Sedentary behaviors, specifically increased screen time, have been shown to have detrimental effects on the cognitive outcomes of youth such as language skills, memory, and spatial cognition (Carson et al., 2015). With increasing demands placed on today’s schools, the school nurse’s role has evolved to encompass the responsibility for teaching much of the health and physical education curriculum once completed by traditional teachers. School nurses assume this role often while serving several schools within district or locale. Consequently, others within the school community such as health coaches, health assistants, and administrative support are often taught and led by school nurses to address many health needs with the schools.
Older teens as trained peer health mentors may be a feasible and resourceful approach that school nurses may adapt to meet the needs of their schools. In addition, a structured peer-mentoring approach to curricular delivery overcomes several barriers to behavioral change and has many innate benefits to both the mentors and the mentees. In focusing on physical activity behaviors, our experience of working in underresourced areas suggests that many students will not have access to traditional exercise and fitness facilities characteristic of many urban and suburban settings. Lack of transportation and distance to facilities are barriers. Therefore, forms of activity that can readily be done in school, neighborhood, and home environments are best achieved through friendship networks and peer groups cultivated through peer mentoring. With peer mentors, engaging in physical activity may be a form of interpersonal connectedness to peer mentors, groups, and friendship networks that leads to sustainability of the behavior over time. Although the behavioral focus of our method is physical activity behavior, school nurses may establish a structured peer-mentoring program to address other health-related topics of importance to their individual school or school district.
Conclusion
The structured peer-mentoring method described in this article provides a promising approach that provides flexibility while at the same time the rigors of an evidence-based and sound theoretical foundation to better engage adolescents in physical activity. Through peer mentoring, adolescents are provided intense social support in a caring and personalized manner. This support builds self-efficacy, competence, and skills needed to develop, maintain, and sustain a lifetime of physical activity behavior.
Acknowledgments
Funding
The author(s) disclosed the following financial support for the research, authorship, and/or publication of this article: The method reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number R01HD080866. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Biographies
Laureen H. Smith, PhD, RN, is an associate professor at College of Nursing at The Ohio State University.
Rick L. Petosa, PhD, is a professor at College of Education and Human Ecology at The Ohio State University.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Academy of Pediatrics. Active healthy living: Prevention of childhood obesity through increased physical activity. Washington, DC: Author; 2006. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Perry CL, Parcel GS. How individuals, environments, and health behaviors interact: Social cognitive theory. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA: Jossey-Bass; 2008. pp. 153–178. [Google Scholar]
- Carey FR, Singh GK, Brown HS, Wilkinson AV. Educational outcomes associated with childhood obesity in the United States: Cross-sectional results from the 2011–2012 National Survey of Children’s Health. International Journal of Behavior, Nutrition, and Physical Activity. 2015;12:S3. doi: 10.1186/1479-5868-12-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson V, Kuzik N, Hunter S, Wiebe SA, Spence JC, Friedman A, Hinkley T. Systematic review of sedentary behavior and cognitive development in early childhood. Preventive Medicine. 2015;78:115–122. doi: 10.1016/j.ypmed.2015.07.016. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The association between school-based physical activity, including physical education, and academic performance. Atlanta, GA: US Department of Health and Human Services; 2010. [Google Scholar]
- Centers for Disease Control and Prevention. School health guidelines to promote healthy eating and physical activity. MMWR 2011. 2011;60:1–77. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States, 2013. MMWR 2014. 2013;63:1–149. [Google Scholar]
- Corcoran T, Silander M. Instruction in high schools: The evidence and the challenge. Future Child. 2009;19:157–183. doi: 10.1353/foc.0.0026. [DOI] [PubMed] [Google Scholar]
- Deutsch NL, Lawrence EC, Henneberger AK. In: Handbook of youth mentoring. DuBois DL, Karcher MJ, editors. Thousand Oaks, CA: Sage; 2014. pp. 175–188. [Google Scholar]
- DuBois DL, Karcher ML. Handbook of youth mentoring. 2nd. Thousand Oaks, CA: Sage; 2014. [Google Scholar]
- Farbman DA. The case for improving and expanding time in school: A review of key research and practice. Boston, MA: National Center on Time and Learning; 2015. [Google Scholar]
- Fleischman S, Heppen L. Improving low-performing high schools: Searching for evidence of promise. Future Child. 2009;19:105–133. doi: 10.1353/foc.0.0021. [DOI] [PubMed] [Google Scholar]
- Hamilton SF, Hamilton MA. Mentoring programs: Promise and paradox. Phi Delta Kappan. 1992;73:546–550. [Google Scholar]
- Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4th. San Francisco, CA: Jossey-Bass; 2008. pp. 189–210. [Google Scholar]
- Hortz BV, Petosa RL. Impact of the “Planning to be Active” leisure time physical exercise program on rural high school students. Journal of Adolescent Health. 2006;39:530–535. doi: 10.1016/j.jadohealth.2006.03.015. [DOI] [PubMed] [Google Scholar]
- Hortz BV, Petosa RL. Social cognitive theory variables mediation of moderate exercise. American Journal of Health Behavior. 2008;32:305–314. doi: 10.5555/ajhb.2008.32.3.305. [DOI] [PubMed] [Google Scholar]
- Hortz B, Stevens E, Holden B, Petosa R. Rates of physical activity among Appalachian adolescents in Ohio. Journal of Rural Health. 2009;25:58–61. doi: 10.1111/j.1748-0361.2009.00199.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Fitness measures and health outcomes in youth. Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- Karcher MJ. The effects of developmental mentoring and high school mentors’ attendance on their younger mentees’ self-esteem, social skills, and connectedness. Psychology School. 2005;42:65–77. [Google Scholar]
- Karcher MJ. The cross-age mentoring program for children with adolescent mentors: Program manual. San Antonio, TX: Developmental Press; 2012. [Google Scholar]
- Karcher MJ, Hansen K. Mentoring activities and interactions. In: DuBois DL, Karcher MJ, editors. Handbook of youth mentoring. Thousand Oaks, CA: Sage; 2014. pp. 63–82. [Google Scholar]
- Keller TE, Blakeslee JE. Social networks and mentoring. In: DuBois DL, Karcher MJ, editors. Handbook of youth mentoring. Thousand Oaks, CA: Sage; 2014. pp. 129–142. [Google Scholar]
- Lee SM, Burgeson CR, Fulton JE, Spain CG. Physical education and physical activity: Results from the school health policies and programs study 2006. Journal of School Health. 2007;77:435–463. doi: 10.1111/j.1746-1561.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- Noam GG, Malti TK, Karcher MJ. Mentoring relationships in developmental perspective. In: DuBois DL, Karcher MJ, editors. Handbook of youth mentoring. Thousand Oaks, CA: Sage; 2014. pp. 99–116. [Google Scholar]
- Ogden CL, Carroll MD, Kit BL, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. Journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petosa RL, Smith LH. Peer mentoring for health behavior change: A systematic review. American Journal of Health Education. 2014;45:351–357. [Google Scholar]
- Plotnikoff RC, Costigan SA, Karunamuni N, Lubans DR. Social cognitive theories used to explain physical activity behavior in adolescents: A systematic review and meta-analysis. Preventive Medicine. 2013;56:245–253. doi: 10.1016/j.ypmed.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Selman R, Schultz LH. Making a friend in youth: Developmental theory and their pair therapy. Chicago, IL: Chicago Press; 1990. [Google Scholar]
- Serrano-Gonzalez M, McConnel C, Bokhary M, Oden J, Lopez X. Association of non-high density lipoprotein cholesterol with psychosocial dysfunction in children and adolescents with obesity. Childhood Obesity. 2015;5:647–649. doi: 10.1089/chi.2015.0043. [DOI] [PubMed] [Google Scholar]
- Smith LH. Piloting the use of teen mentors to promote a healthy diet and physical activity among children in Appalachia. Journal for Specialists in Pediatric Nursing. 2011;16:16–26. doi: 10.1111/j.1744-6155.2010.00264.x. [DOI] [PubMed] [Google Scholar]
- Smith LH, Holloman C. Comparing the effects of teen mentors to adult teachers on child lifestyle behaviors and health outcomes in Appalachia. Journal of School Nursing. 2013;29:386–396. doi: 10.1177/1059840512472708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens E, Petosa RL. Evaluation of a social cognitive theory-based adolescent physical activity intervention: Plan for exercise, plan for health. Columbus: The Ohio State University; 2006. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Registry of Evidence-based Programs and Practice. Washington, DC: Author; 2014. (Cross-Age Mentoring Program (CAMP) for Children with Adolescent Mentors). [Google Scholar]
- U.S. Department of Education, National Center for Education Statistics. Digest of Education Statistics: 2013(NCES2015-011), Chapter 1. Washington, DC: National Center for Education Statistics; 2015. [Google Scholar]
- U.S. Department of Health and Human Services. Physical activity guidelines for Americans. Washington, DC: Author; 2008. [Google Scholar]
- Winters ER, Petosa RL. Test of a social cognitive theory-based educational treatment to increase the frequency of voluntary moderate and vigorous physical exercise among adolescent school students. Columbus: The Ohio State University; 2001. [Google Scholar]


