Abstract
Background
South Africa has one of the highest burdens of latent tuberculosis infection (LTBI) in high-risk populations such as young children, adolescents, household contacts of TB cases, people living with HIV, gold miners and health care workers, but little is known about the burden of LTBI in its general population.
Methods
Using a community-based survey with random sampling, we examined the burden of LTBI in an urban township of Johannesburg and investigated factors associated with LTBI. The outcome of LTBI was based on TST positivity, with a TST considered positive if the induration was ≥5 mm in people living with HIV or ≥10 mm in those with unknown or HIV negative status. We used bivariate and multivariable logistic regression to identify factors associated with LTBI
Results
The overall prevalence of LTBI was 34.3 (95 % CI 30.0, 38.8 %), the annual risk of infection among children age 0–14 years was 3.1 % (95 % CI 2.1, 5.2). LTBI was not associated with HIV status. In multivariable logistic regression analysis, LTBI was associated with age (OR = 1.03 for every year increase in age, 95 % CI = 1.01–1.05), male gender (OR = 2.70, 95 % CI = 1.55–4.70), marital status (OR = 2.00, 95 % CI = 1.31–3.54), and higher socio-economic status (OR = 2.11, 95 % CI = 1.04–4.31).
Conclusions
The prevalence of LTBI and the annual risk of infection with M. tuberculosis is high in urban populations, especially in men, but independent of HIV infection status. This study suggests that LTBI may be associated with higher SES, in contrast to the well-established association between TB disease and poverty.
Keywords: South Africa, LTBI, Prevalence, ARI, Risk factors, Urban population
Background
Tuberculosis (TB) remains a significant public health problem worldwide with an estimated 9.6 million cases and 1.5 million deaths in 2014 [1]. In 2014, South Africa had the second highest burden of TB in the African region and was ranked sixth among the 22 countries classified by the World Health Organization (WHO) as high TB burden countries [1]. More South Africans died of TB, predominantly HIV-associated TB, than any other disease [2]. These statistics suggest that the current TB control strategy is unable to control the TB epidemic in South Africa, which is fueled by both progression from LTBI to active disease, in large part due to HIV co-infection, and ongoing transmission of Mycobacterium tuberculosis (M. tuberculosis) [3].
Globally, about 2.6 billion people are infected with M. tuberculosis, representing a large reservoir of people at risk of progression to active TB disease [1, 4–7]. About 5–10 % of people with LTBI progress to active TB disease in their lifetime, the majority within 2 years of infection [8]. Those at highest risk of progression to active TB disease are young children and immunocompromised individuals [7, 9, 10]. To date, studies of the burden of LTBI in South Africa have mainly focused on high-risk populations such as young children, adolescents, household contacts of TB cases, people living with HIV, gold miners and health care workers [11–16]. These studies observed LTBI prevalence ranging from 26 % up to 89 %. The only community-based study, performed in an urban township of Cape Town, observed a very high (88.0 %) LTBI prevalence rate, but the study was limited to healthy HIV-negative individuals [17].
The goal of this study was to describe the burden of LTBI in a representative sample of all residents of an urban South Africa township and determine factors associated with LTBI.
Methods
Study site and Study population
The study was conducted in Diepsloot, a densely populated, urban township located in northern Johannesburg, South Africa. The community covers an area of 12 km2 and has an estimated population of 136,289, corresponding to a very high population density of 11,357 people/km2 [18]. The area is typical of urban South African townships, consisting of informal settlements with a mix of high-density shacks and government-subsidized brick houses. According to the 2006 Johannesburg Poverty and Livelihoods Study, Diepsloot is one of the poorest urban informal settlements in Johannesburg [19].
The analysis represents a sub-study of a large community-based household health survey conducted between May 2013 to March 2014 using a random sampling framework. Geographic coordinates were generated from an aerial map of the 13 digital geo-referenced extensions of the township. The township extensions are designated areas (neighbourhoods) within the township. Geographic coordinates were randomly selected within each extension and the number of coordinates per extension was proportional to the population density of the extension. The randomly selected coordinates were then located by the study team using a hand-held geographic positioning system (GPS) device (eTrex 10, Garmin). The household nearest to but within 30 m of each randomly selected geographic coordinate was eligible for study participation. If multiple households were equidistant from the geo-coordinate, households within the same distance were numbered, and then the survey team randomly selected one household using a random number generator. Following this method, survey teams approached 2006 households. Households, where no-one could be found home despite up to five repeat visits, were considered missing and not replaced.
At the time of the home visit, the exact latitude and longitude coordinates of the house were geocoded. When the household member agreed for the household to participate in the survey, all household members were enumerated. one of the enumerated adult (≥15 years) household members was randomly selected for study participation using the Kish grid method [20]. To be an eligible household member, each adult had to sleep in the household at least 1 night per week. This procedure was implemented to avoid the selection bias that would have occurred had the adult household member at home at the time of the survey been systematically selected for study participation. If the adult household member selected for study participation was not home, then the survey team made up to 4 attempts before the household member was considered unreachable. Selected adults who could not be reached were not replaced. All childhood household members were invited to participate in a health assessment if the selected adult household member consented for their study participation. If a child <15 was not in the household at the time the selected adult participant was interviewed, no return home visits were made for the child.
Using a structured questionnaire in English, Sesotho or IsiZulu, data on socio-demographics and household characteristics, education and employment, history of TB or contact with TB, and alcohol and smoking habits were collected from all adult participants. A health assessment was performed in all adult and child participants. Weight and height were measured, and blood was collected for haemoglobin and HIV testing by a trained lay HIV counsellor. Participants were assessed for symptoms of active TB and a tuberculin skin test (TST) was placed by a trained nurse. A quantity of 0.1 ml (5TU) of purified protein derivative (PPD) (Aplisol and Tubersol) was injected in the fore arm; the size of induration was read 48 to 72 h later. Because of a high rate of adverse events in HIV negative individuals, including blistering and ulceration, the ethics committee overseeing the study recommended in October 2014 to restrict the placement of TST to HIV positive individuals.
Study variables
The outcome of LTBI was based on TST positivity, with a TST considered positive if the induration was ≥5 mm in people living with HIV or ≥10 mm in those with unknown or HIV negative status [21].
Individual covariates included age (<15, 15–24, 25–34, 35–44 or ≥45 years); sex (male or female), HIV status (positive or negative), Body Mass Index (BMI; underweight/normal if BMI ≤18.5–24.9 kg/m2, overweight if BMI 25–29.9 kg/m2, or obese if BMI ≥30 kg/m2) presence of anaemia (with anaemia defined as haemoglobin value below 13.0 g/dl for men, <12.0 g/dl for women and children aged 12 to15 years, <11.0 g/dl or children under 5 years, or <11.5 g/dl for children aged 5 to12 years; all down-adjusted by 0.65 g/dl because of altitude), [22] education (primary or less vs. secondary or higher); marital status (living with partner or not living with a partner); employment status (unemployed or employed); household contact with TB (yes or no); smoking status (ever or never), and alcohol consumption (yes or no).
The household-level covariates included were household socioeconomic status (SES), household ventilation and household exposure to smoking. Household SES was calculated as a composite index developed by factor analysis based on household ownership of durable goods (car, motorcycle, bicycle, refrigerator, television, radio, and mobile phone), house ownership, source of drinking water, and type of toilet facilities [23, 24]. Household SES indices were categorized into tertiles of highest, median and lowest household SES. Household ventilation was defined based on the frequency household members sleep with the window open (always, only when warm enough, never, no windows in the house), household exposure to secondary smoking as (yes or no).
We created 20 neighbourhoods from the 13 extensions by further subdividing 5 largest extensions of Diepsloot township. Neighbourhood-level factors included neighbourhood SES which was obtained by summarizing household SES by 20 neighbourhood, population density defined as the number of people per square kilometre (low, medium or high) and household density defined as the number of households per square kilometre (low, medium or high). Population and household density data were retrieved from the 2011 South African census as disseminated by Statistics South Africa (STATSSA) using the SuperCROSS software [18].
Statistical analysis
LTBI prevalence was calculated by dividing the number of participants with a positive TST by the total number of participants with a TST results and 95 % confidence intervals (95 % CI) were estimated. Annual risk of infection (ARI) with M. tuberculosis in children age 0 to 14 years was calculated using the formula ARI = 1 − (1 − P)1/a; where P is the observed prevalence of LTBI, and a the mean age of participating children [25, 26].
We opted for a multilevel (hierarchical) structure of our data with individuals and households (first level) nested into 20 township neighbourhoods (second level). We calculated the intraclass correlation coefficient (ICC) to assess the magnitude of variability due to the covariates at the neighbourhood level in order to determine whether multilevel logistic models were appropriate [27–29]. The ICC was calculated by fitting a “null model” using the Stata command “gllamm” within the generalized linear latent and mixed methods framework, for binary response outcome [30].
We used bivariate and multivariable logistic regression to identify factors associated with LTBI. Starting from a full model with all potential predictors, we employed a stepwise backward elimination approach removing the least significant factor one at a time until all remaining factors were significant. We repeated the model building procedures using stepwise forward selection to check whether this yielded the same final model. Associations between predictors and LTBI are summarized in odds ratio (OR) along with 95 % CIs. A p-value of <0.05 was considered statistically significant. Data analysis was conducted using Stata version 13.1 (Stata Corp, College Station, TX).
Results
Study participants
Of the 2006 randomly selected households, 1620 could be enumerated. Of the 1620 randomly selected adults, 1581 (97.6 %) could be contacted and 1230 agreed to participate (Fig. 1). In addition, 169 children living in the same household as the participating adult were enrolled. TST was offered to 626 participants (all participants until October 2014, only HIV positive individuals thereafter). Of these, 144 refused and TST was not placed in 23. Of the 459 participants in whom a TST was placed, TST was read in 446 (97 %), the remaining 13 could not be traced within 48–72 h of TST placement.
Fig. 1.
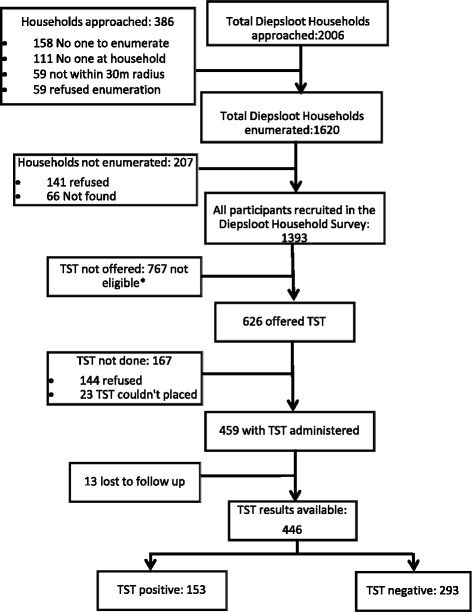
Flow chart of study participants. *These participants were not eligible for TST according to SA National TB guidelines
Among the 446 participants with TST result, mean age was 35 years, 11 % were 0 to 15 years of age, 17 % were 15 to 24 years, 33 % were 25 to 34 years, 18 % were 35 to 34 years and 21 % were 45 years or older (Table 1). Sixty percent were female, 44 % were married or living with a partner, two thirds (67 %) were unemployed and the majority (72 %) had at least some secondary education. Self-report of smoking (26 %) and alcohol use (37 %) was relatively low. Overall, 18 % of the 446 participants with TST result were HIV positive, 35 % were anaemic, 23 % were underweight and 27 % obese. Only 6 % of participants reported a history of contact with a TB case. Almost all (93.4 %) participants either lived in a house without windows or never slept with windows open and 20 % were exposed to household secondary smoking.
Table 1.
Characteristics of 446 participants with positive and negative TST results
| Characteristics | TST Positive N (row %) |
TST Negative N (row %) |
Total N (column %) |
|
|---|---|---|---|---|
| Age in Years median (IQR) | 35 (27–45) | 29 (22–38) | 32 (23–41) | |
| Age group | 0–14 | 9 (18.7) | 39 (81.3) | 48 (10.8) |
| 15–24 | 20 (26.3) | 56 (73.7) | 76 (17.0) | |
| 25–34 | 45 (30.6) | 102 (69.4)_ | 147 (33.0) | |
| 35–44 | 37 (45.1) | 45 (54.9) | 82 (18.4) | |
| ≥45 | 42 (45.2) | 51 (54.8) | 93 (20.8) | |
| Sex | Female | 86 (32.2) | 181 (67.8) | 267 (60.4) |
| Male | 65 (37.1) | 110 (62.9) | 175 (39.6) | |
| HIV status | Positive | 23 (32.9) | 47 (67.1) | 70 (18.1) |
| Negative | 115 (36.3) | 202 (63.7) | 317 (81.9) | |
| BMI (kg/m2) median (IQR) | 25 (21–29) | 23 (20–29) | 24 (20–29) | |
| BMI categories | Normal/underweight | 70 (34.8) | 131 (65.2) | 201 (49.9) |
| Overweight | 39 (41.5) | 55 (58.5) | 94 (23.3) | |
| Obese | 37 (34.3) | 71 (65.7) | 108 (26.8) | |
| Anaemia | Anaemic | 51 (32.3) | 107 (67.7) | 158 (35.4) |
| Non-anaemic | 102 (35.4) | 186 (64.6) | 288 (64.6) | |
| Education level | ≤ Primary | 44 (40.0) | 66 (60.0) | 110 (28.1) |
| ≥ Secondary | 100 (35.4) | 181 (64.6) | 281 (71.9) | |
| Employment status | Unemployed | 96 (36.8) | 165 (63.2) | 261 (66.6) |
| Employed | 48 (36.6) | 83 (63.4) | 131 (33.4) | |
| Marital status | Not living with a partner | 34 (29.6) | 81 (70.4) | 115 (61.6) |
| Living with a partner | 75 (44.4) | 94 (55.6) | 169 (38.4) | |
| Household contact with TB | Yes | 14 (58.3) | 10 (41.7) | 24 (6.2) |
| No | 129 (35.3) | 236 ((64.7) | 365 (93.8) | |
| Smoking | No | 101 (35.0) | 188 (65.0) | 289 (73.7) |
| Yes | 43 (41.8) | 60 (58.2) | 103 (26.3) | |
| Alcohol consumption | No | 87 (35.2) | 160 (64.8) | 247 (62.7) |
| Yes | 57 (38.8) | 90 (61.2) | 147 (37.3) | |
| Household ventilation | Always/Only when warm | 13 (50.0) | 13 (50.0) | 26 (6.6) |
| (sleep with window open) | Never/No windows | 131 (35.6) | 237 (64.4) | 368 (93.4) |
| Household SES | Low | 43 (29.9) | 101 (70.1) | 144 (34.0) |
| Medium | 50 (33.8) | 98 (66.2) | 148 (35.0) | |
| High | 51 (38.9) | 80 (61.1) | 131 (31.0) | |
| Household exposure to | No | 115 (36.4) | 200 (63.6) | 315 (79.9) |
| secondary smoking | Yes | 29 (36.7) | 50 (63.3) | 79 (20.1) |
| Household number of | <3 | 102 (31.3) | 224 (68.7) | 326 (73.1) |
| rooms | ≥3 | 51 (42.5) | 69 (57.5) | 120 (26.9) |
| Household density | Low (<300/km2) | 53 (34.0) | 103 (66.0) | 156 (35.0) |
| Medium (300–600/km2) | 56 (38.9) | 88 (61.1) | 144 (32.3) | |
| High (>600/km2) | 44 (30.1) | 102 (69.9) | 146 (32.7) |
Distribution of TST results, LTBI Prevalence and Annual Risk of infection
The frequency distributions of the indurations are shown in Fig. 2. Using HIV-specific definitions for LTBI, the overall prevalence of LTBI was 34 % [95 % CI, 30–39 %]. LTBI prevalence increased with age, from 19 % in the 0–14 age group to 45 % in the 45 and older age group (p = 0.002), was higher in women (37 %) than men (32 %) (p = 0.273), but similar in HIV positive (36 %) and HIV negative (32 %) participants (p = 0.553) (Table 2). Based on changes in TST prevalence with age among children age 0 to 15 years, the ARI was estimated at 3.1 % (95 % CI: 2.1–5.2).
Fig. 2.
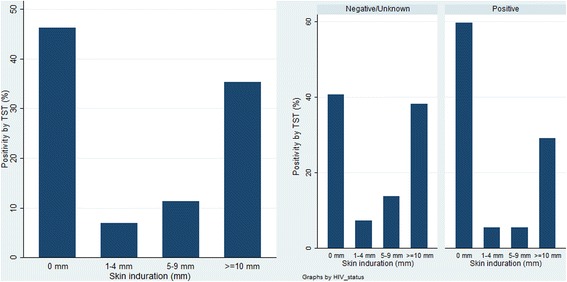
Distribution of TST induration diameter among the study participants and by HIV status
Table 2.
Estimated prevalence of infection by age, sex, and HIV status
| Characteristics | Mean age Years |
Prevalence, % % (95 % CI) |
p-value |
|---|---|---|---|
| Overall | 32.2 | 34.3 (30.0–38.8) | |
| Age group years | |||
| 0–14 | 6.2 | 18.8 (10.0–32.5) | 0.002 |
| 15–24 | 20.7 | 26.3 (17.6–37.4) | |
| 25–34 | 29.5 | 30.6 (23.7–38.8) | |
| 35–44 | 39.1 | 45.1 (34.6–56.1) | |
| 45+ | 53.4 | 45.2 (35.3–55.4) | |
| Sex | |||
| Male | 33.3 | 37.1 (30.3–44.8) | 0.273 |
| Female | 31.8 | 32.1 (26.7–37.9) | |
| HIV status | |||
| Positive | 38.1 | 32.4 (22.5–44.2) | 0.553 |
| Negative | 32.7 | 36.1 (31.0–41.5) | |
Factors associated with LTBI at individual and household level
In univariable logistic regression, age showed a strong association with LTBI with increasing odds of LTBI for every year increase in age (OR = 1.17, 95 % CI = 1.08–1.26) (Table 3). Other variables associated with LTBI were marital status, with individuals living with a partner being twice as likely to have LTBI compared with those living without a partner (OR = 2.00, 95 % CI: 1.06–3.80); history of household contact with TB, with those reporting such history being twice as likely to have LTBI compared with those not in household contact with a TB case (OR = 2.33, 95 % CI: 1.03–5.28); and number of room in the house, with people living in dwellings with 3 or more rooms being more likely to have LTBI compared to people living in dwellings with less than 3 rooms (OR = 1.62, 95 % CI: 1.05–2.50). People of the highest tertile of SES were 1.5 times more likely to have LTBI, but the 95 % CI crossed 1 (95 % CI 0.91–2.47). In multivariable logistic regression, age (OR = 1.03, 95 % CI = 1.01–1.05), gender (OR = 1.77, 95 % CI = 1.10–2.86), marital status (OR = 2.00, 95 % CI = 1.13–3.54) and living in a household that belong s to the highest tertile SES of the community (OR 2.11, 95 % CI 1.04–4.31) were independently associated with a diagnosis of LTBI.
Table 3.
Logistic regression analysis of risk factors associated with LTBI
| Characteristics | Unadjusted odds ratio (95 % CI) | Adjusted odds ratio (95 % CI) | |
|---|---|---|---|
| Individual-level characteristics | |||
| Age in years | 1.17 (1.08–1.26) | 1.03 (1.01–1.05) | |
| Sex | Female | 1.00 | 1.00 |
| Male | 1.25 (0.84–1.86) | 2.70 (1.55–4.70) | |
| HIV status | Negative | 1.00 | |
| Positive | 0.85 (0.49–1.46) | ||
| BMI categories | Normal/Underweight | 1.00 | |
| Overweight | 1.33 (0.80–2.19) | ||
| Obese | 0.97 (0.60–1.59) | ||
| Anaemia | Non-anaemic | 1.00 | |
| Anaemic | 0.87 (0.58–1.31) | ||
| Education level | ≤ Primary | 1.00 | |
| ≥ Secondary | 0.83 (0.53–1.30) | ||
| Employment status | Unemployed | 1.00 | |
| Employed | 0.99 (0.64–1.54) | ||
| Marital status | Not living with a partner | 1.00 | 1.00 |
| Living with a partner | 1.90 (1.50–3.14) | 2.00 (1.13–3.54) | |
| Household contact with TB | No | 1.00 | 1.00 |
| Yes | 2.33 (1.03–5.28) | 2.27 (0.76–6.82) | |
| Smoking | No | 1.00 | |
| Yes | 1.33 (0.84–2.11) | ||
| Alcohol consumption | No | 1.00 | |
| Yes | 1.16 (0.76–1.78) | ||
| Household- and neighbourhood-level characteristics | |||
| Household exposure to | No | 1.00 | |
| secondary smoking | Yes | 1.01 (0.61–1.69) | |
| Household number of | <3 | 1.00 | |
| rooms | ≥3 | 1.62 (1.05–2.50) | |
| Household ventilation | Always/Only when warm | 1.00 | |
| (sleep with window open) | Never/No windows | 1.37 (0.29–6.53) | |
| Household SES | Low | 1.00 | 1.00 |
| Medium | 1.20 (0.73–1.96) | 1.73 (0.85–3.52) | |
| High | 1.50 (0.91–2.47) | 2.11 (1.04–4.31) | |
| Household density | Low (<300/km2) | 1.00 | |
| Medium (300–600/km2) | 1.24 (0.77–1.98) | ||
| High (>600/km2) | 0.84 (0.52–1.36) | ||
Factors associated with LTBI at neighbourhood level
None of the neighbourhood level factors were associated with LTBI. The multilevel “null” model showed that ICC was 0.01032 (p = 0.4005), meaning that only 1 % of the variance in LTBI was explained by differences in neighbourhood factors.
Discussion
The burden of LTBI in this urban informal settlement community of northern Johannesburg, South Africa, was high with an overall prevalence of 34.3 % and an annual risk of infection of 3.1 %. Risk factors independently associated with LTBI prevalence were older age, male gender, living with a partner, and high SES.
While the LTBI burden observed was high, the 34.3 % prevalence was lower than that the LTBI burden that has been observed in the few prior population-based studies previously performed in urban townships. In a Peruvian shantytown and a Ugandan urban population, the LTBI prevalence was higher, with half of all residents were living with LTBI (52 %; 95 % CI: 48–57 in Peru and 49 %; 95 % CI: 44–55 in Uganda) [31, 32]. A study of 8 South African urban communities however showed that LTBI prevalence among household contacts can be highly variable between communities in the same region, as they documented a range of LTBI prevalence from 24 to 77 % [33]. The ARI in our study fell within the range of ARI estimates from prior South African studies (2.8–5.8 %) [15, 34]. Taking together, these results suggest that the LTBI prevalence in urban settlements is high, but shows substantial variation.
Exposure to a household TB case is well established risk factor for LTBI [31, 35, 36], resulting in a large proportion of LTBI among children and young adults being due to household exposure to TB [37]. In our study, exposure to a household TB case was not significantly associated with LTBI. This may be due to relatively small sample size of children under 12 years of age in our study population. The increasing prevalence of LTBI with age reflects the cumulative exposure to TB through social interaction in high TB burden settings [38–42] and is consistent with findings of other LTBI studies in urban populations [15–17, 32, 33]. Data on the association between male gender and increased LTBI prevalence are conflicting. A higher LTBI prevalence among males was also observed in a rural area of Ethiopia [43] and a Peruvian peri-urban shantytown [31] but not in an urban population in Ugandan [32] nor in prior South Africa studies [16, 33, 44]. Being male was a strong predictor of LTBI on our study. Recent evidence suggests that social mixing and interaction vary significant by age and gender [45]. The higher rate of LTBI in urban males we observed may be due to the high risk of TB transmission in social gathering places, such as informal alcohol drinking establishments (shebeens) [39, 46], which are more frequented by men than women.
HIV infection was common (18 %) but not associated with LTBI prevalence in this population. Other LTBI prevalence studies in high HIV burden settings have reported similar observations [32, 47]. The lack of association between HIV and LTBI may be due poor sensitivity of TST in HIV-infected individuals [48], however we addressed this by decreasing the TST cut-off to 5 mm [49]. In addition, some other risk factors such as smoking and exposure to household secondary smoking [50, 51] were not associated with LTBI prevalence in our study. The smoking and exposure to secondary smoking have been found to be associated with increased odds of LTBI in low incidence settings [52, 53]. However, studies conducted in Africa have reported conflicting results [32, 33, 44–55]. Our findings are similar to results observed in studies conducted in Uganda, Zambia and South Africa [32, 33].
TB disease has clearly been established a as disease of poverty [56, 57]. It is therefore surprising that we observed a higher LTBI prevalence among people with higher household SES. An association of higher SES rather than lower SES associated with higher LTBI prevalence was also observed in a study in Zambia [47], and in a population-based multicentre study in China [58]. Another study in South Africa found employment not unemployment (which is one of the indicators for lower SES) was associated with higher LTBI prevalence [54]. Taken together, these findings suggest that SES may have a differential effect on the risk of LTBI acquisition and risk of progression from infection to active TB disease. Boccia et al suggested that “it is possible that, especially in urban settings, higher SEP is associated with housing characteristics that reduce ventilation and life-styles that increase social mixing and therefore the likelihood of contact between cases and susceptible people. We could not find an association between ventilation and LTBI, and higher SES was not associated with poorer ventilation in our sample. Given that we did not assess use of public transportation or social mixing [39, 59, 60] in our study we could not assess whether these factors can explain the observation of higher LTBI prevalence in people of higher SES within urban settlements. These hypotheses thus warrant further in-depth investigations.
Our study had many strengths, including the population-based design with geographically weighted random sampling of the general population, including people living with and without HIV and both adults and children, and a standardized approach to define SES tertiles. Our study does have some limitations. First, the cross-sectional nature of the study does not allow for establishment of temporality or causality between LTBI and associated factors. Second, small variability at the neighbourhood level may have been due to the sparsity of level 2 clusters with only 20 neighbourhoods (level 2 clusters), smaller than recommendation of 50 level 2 clusters [61]. Thus, fitting a multilevel logistic regression model was thus not indicated for the analysis of our data. Third, even though some of well-known risk factors such occupation, crowding, and ventilation were not measured, the proxy measures of these factors were not associated with LTBI. BCG vaccination status, which can reduce the specificity of TST, was also not documented [62, 63]. Fourth, the ethics committee restricted the placement of TST only to HIV positive individuals and children under 5 years old in October 2014. However, changes regarding with restriction of TST to HIV positive individuals is negligible since only 16 participants were included in the study after the restriction was introduced. Excluding these 16 participants does not change the results. We therefore feel confident that change (imposed by the ethics committee) did not affect the results. Furthermore, the sample size was relatively small, especially for children under 12 years of age since we did not made more attempts to find this group of participants if they were not at home during interview of the adult participants. Finally, as 19 % of the targeted household were not enrolled due to failure to find someone at home despite multiple attempts or refusal to participate, our aim to enrol a representative sample of the population may not have been fully achieved.
Conclusion
The prevalence of LTBI and the annual risk of infection with M. tuberculosis is high in urban populations, especially in men, but independent of HIV infection status The unexpected association between higher LTBI and higher household SES suggest that the differential association between SES as risk factors for acquisition of TB infection and progression from LTBI to active disease is not yet fully understood. A better understanding of individual, household and community-level risk factors for LTBI will be important for the development of efficient, targeted LTBI interventions in high TB burden settings.
Acknowledgments
We are grateful to the inhabitants of Diepsloot for their participation, the survey teams (study nurses, lay HIV counsellors, drivers and interns), Clinical HIV Research Unit (CHRU) and the Witkoppen Health and Welfare Centre research team for their contributions. We also like to thank Diepsloot Community Advisory Forum, the ward counsellor’s office for their contributions during the community engagement process and the City of Johannesburg’s Geographic Information Systems Department for providing digital geographic data of Diepsloot.
Funding
Research reported in this publication was funded by the United States Agency for International Development (USAID) under award number AID-674-A-12-00033. The content is solely the responsibility of the authors and does not necessarily represent the official views of USAID. Support for Jabulani R Ncayiyana was provided by Fogarty International Center AIDS International Training and Research Program (AITRP) and South Africa National Research Foundation (NRF) Freestanding Doctoral Scholarship for Studies Abroad (Grant no. 88866).
Availability of data and materials
The datasets generated during and/or analysed during the parent study are not publically available due to data sharing agreement restrictions in place. Readers may contact Dr. Annelies van Rie for further clarification.
Authors’ contribution
JB, AvR, CH, SS, NW and IS designed the overall study and supervised implementation with additional support from JN. JN and AvR conceptualized the research idea, JN performed the statistical analysis, under the supervision of AvR, and the manuscript was written by JN, under the supervision of AvR, and reviewed by DW, EM, ME, AP, CH, SS, NW, JB and IS. All authors read and approved the final manuscript.
Authors’ information
Jabulani R. Ncayiyana, PhD and Lecturer, Division of Epidemiology and Biostatistics, School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, South Africa.
Jean Bassett, MBChB and Director, Witkoppen Health and Welfare Centre, South Africa.
Nora West, MPH and Project Manager, Witkoppen Health and Welfare Centre, South Africa.
Daniel Westreich, PhD and Associate Professor, Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, USA.
Eustatius Musenge, PhD and Senior Lecturer, Division of Epidemiology and Biostatistics, School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, South Africa.
Michael Emch, PhD and Professor, Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, USA.
Audrey Pettifor, PhD and Associate Professor, Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, USA.
Colleen F. Hanrahan, PhD and Assistant Scientist, Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, USA.
Sheree R. Schwartz, PhD and Assistant Scientist, Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, USA.
Ian Sanne, MBChB, MMed, PhD and Director, Clinical HIV Research Unit, Department of Medicine, University of the Witwatersrand, South Africa.
Annelies van Rie, MD, PhD and Professor, Department of Epidemiology and Social Medicine, Faculty of Medicine and Health Sciences, University of Antwerp, Belgium.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
An ethical clearance was obtained from the University of North Carolina at Chapel Hill Institutional Review Board (Study no.:15-2340) and University of the Witwatersrand’s Humans Research Ethics Committee (Medical) (Clearance certificate no.: M130204). Written consent was obtained from all adult participants, written parental consent and assent was obtained from all participating children age 7-17 years old.
Abbreviations
- 95 % CI
95 % confidence interval
- ARI
Annual risk of infection
- BCG
Bacillus Calmette–Guérin
- GPS
Geographic positioning system
- HIV
Human immunodeficiency virus
- ICC
Intraclass correlation coefficient
- LTBI
Latent tuberculosis infection
- OR
Odds ratio
- PPD
Purified protein derivative
- SES
Socioeconomic status
- TB
Tuberculosis
- TST
Tuberculin skin test
Contributor Information
Jabulani R. Ncayiyana, Email: Jabulani.Ncayiyana@wits.ac.za
Jean Bassett, Email: jeanb@witkoppen.co.za.
Nora West, Email: noraswest@gmail.com.
Daniel Westreich, westreic@email.unc.edu.
Eustasius Musenge, Email: eustasius.musenge@wits.ac.za.
Michael Emch, Email: emch@unc.edu.
Audrey Pettifor, apettif@email.unc.edu.
Colleen F. Hanrahan, Email: chanrah1@jhmi.edu
Sheree R. Schwartz, Email: sschwartz@jhu.edu
Ian Sanne, Email: isanne@witshealth.co.za.
Annelies van Rie, Email: annelies.vanrie@uantwerpen.be.
References
- 1.World Health Organization (WHO). Global tuberculosis report 2015. Geneva: World Health Organization; 2015.
- 2.Statistics South Africa (STATSSA). Mortality and causes of death in South Africa, 2013: Findings from death notification. Statistical Release P0309.3. Pretoria: Statistics South Africa; 2014.
- 3.Wood R, Lawn SD, Johnstone-Robertson S, Bekker LG. Tuberculosis control has failed in South Africa: time to reappraise strategy. S Afr Med J. 2011;101:111–114. doi: 10.7196/SAMJ.4587. [DOI] [PubMed] [Google Scholar]
- 4.Diel R, Loddenkemper R, Zellweger J-P, Sotgiu G, D’Ambrosio L, Centis R, van der Werf MJ, Dara M, Detjen A, Gondrie P. Old ideas to innovate tuberculosis control: preventive treatment to achieve elimination. Eur Respir J. 2013;42(3):785–801. doi: 10.1183/09031936.00205512. [DOI] [PubMed] [Google Scholar]
- 5.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. J Am Med Assoc. 1999;282(7):677–686. doi: 10.1001/jama.282.7.677. [DOI] [PubMed] [Google Scholar]
- 6.Zumla A, Raviglione M, Hafner R, Fordham von Reyn C. Tuberculosis. N Engl J Med. 2013;368(8):745–755. doi: 10.1056/NEJMra1200894. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO). Guidelines on the management of latent tuberculosis infection. Geneva: World Health Organization; 2015. [PubMed]
- 8.Centers for Disease Control Prevention (CDC). Latent tuberculosis infection: a guide for primary health care providers. Atlanta: Centers for Disease Control Prevention; 2013.
- 9.Dye C, Glaziou P, Floyd K, Raviglione M. Prospects for tuberculosis elimination. Annu Rev Public Health. 2013;34:271–286. doi: 10.1146/annurev-publhealth-031912-114431. [DOI] [PubMed] [Google Scholar]
- 10.Kasprowicz VO, Churchyard G, Lawn SD, Squire SB, Lalvani A. Diagnosing latent tuberculosis in high-risk individuals: rising to the challenge in high-burden areas. J Infect Dis. 2011;204(suppl 4):S1168–S1178. doi: 10.1093/infdis/jir449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Middelkoop K, Bekker L-G, Liang H, Aquino LD, Sebastian E, Myer L, Wood R. Force of tuberculosis infection among adolescents in a high HIV and TB prevalence community: a cross-sectional observation study. BMC Infect Dis. 2011;11(1):156. doi: 10.1186/1471-2334-11-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hanifa Y, Grant A, Lewis J, Corbett E, Fielding K, Churchyard G. Prevalence of latent tuberculosis infection among gold miners in South Africa. Int J Tuberc Lung Dis. 2009;13(1):39–46. [PubMed] [Google Scholar]
- 13.Van Rie A, McCarthy K, Scott L, Dow A, Venter W, Stevens W. Prevalence, risk factors and risk perception of tuberculosis infection among medical students and healthcare workers in Johannesburg, South Africa. S Afr Med J. 2013;103(11):853–857. doi: 10.7196/samj.7092. [DOI] [PubMed] [Google Scholar]
- 14.Shah M, Kasambira TS, Adrian PV, Madhi SA, Martinson NA. Longitudinal analysis of QuantiFERON-TB Gold In-Tube in children with adult household tuberculosis contact in South Africa: a prospective cohort study. PLoS One. 2011;6(10):e26787. doi: 10.1371/journal.pone.0026787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Middelkoop K, Bekker L-G, Myer L, Dawson R, Wood R. Rates of tuberculosis transmission to children and adolescents in a community with a high prevalence of HIV infection among adults. Clin Infect Dis. 2008;47(3):349–355. doi: 10.1086/589750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahomed H, Hawkridge T, Verver S, Geiter L, Hatherill M, Abrahams DA, Ehrlich R, Hanekom WA, Hussey GD, Team SAS Predictive factors for latent tuberculosis infection among adolescents in a high-burden area in South Africa. Int J Tuberc Lung Dis. 2011;15(3):331–336. [PubMed] [Google Scholar]
- 17.Wood R, Liang H, Wu H, Middelkoop K, Oni T, Rangaka MX, Wilkinson RJ, Bekker L-G, Lawn SD. Changing prevalence of TB infection with increasing age in high TB burden townships in South Africa. Int J Tuberc Lung Dis. 2010;14(4):406. [PMC free article] [PubMed] [Google Scholar]
- 18.Statistics South Africa (STATSSA). Census 2011; Interactive data in SuperCROSS. Pretoria: Statistics South Africa; 2011.
- 19.De Wet T, Patel L, Korth M, Forrester C. Johannesburg poverty and livelihoods study. Johannesburg: Centre for Social Development in Africa, University of Johannesburg; 2008. [Google Scholar]
- 20.Kish L. A procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44(247):380–387. doi: 10.1080/01621459.1949.10483314. [DOI] [Google Scholar]
- 21.South Africa Department of Health. National Tuberculosis Management Guidelines 2014. Pretoria: Department of Health; 2014.
- 22.Cook JD, Boy E, Flowers C, del Carmen Daroca M. The influence of high-altitude living on body iron. Blood. 2005;106(4):1441–1446. doi: 10.1182/blood-2004-12-4782. [DOI] [PubMed] [Google Scholar]
- 23.Myer L, Ehrlich RI, Susser ES. Social epidemiology in South Africa. Epidemiol Rev. 2004;26(1):112–123. doi: 10.1093/epirev/mxh004. [DOI] [PubMed] [Google Scholar]
- 24.Booysen FR. Using demographic and health surveys to measure poverty–an application to South Africa. J Stud Econ Econometrics. 2002;26(3):53–70. [Google Scholar]
- 25.Rieder H. Annual risk of infection with Mycobacterium tuberculosis. Eur Respir J. 2005;25(1):181–185. doi: 10.1183/09031936.04.00103804. [DOI] [PubMed] [Google Scholar]
- 26.Rieder H. Methodological issues in the estimation of the tuberculosis problem from tuberculin surveys. Tuber Lung Dis. 1995;76(2):114–121. doi: 10.1016/0962-8479(95)90552-9. [DOI] [PubMed] [Google Scholar]
- 27.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21(1):171–192. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 28.Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–449. doi: 10.1136/jech.2004.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: interpreting neighbourhood differences and the effect of neighbourhood characteristics on individual health. J Epidemiol Community Health. 2005;59(12):1022–1029. doi: 10.1136/jech.2004.028035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rabe-Hesketh S, Skrondal A, Pickles A. GLLAMM manual. Berkeley: University of California; 2004. [Google Scholar]
- 31.Martinez L, Arman A, Haveman N, Lundgren A, Cabrera L, Evans CA, Pelly TF, Saito M, Callacondo D, Oberhelman R. Changes in tuberculin skin test positivity over 20 years in periurban shantytowns in Lima, Peru. Am J Trop Med Hyg. 2013;89(3):507–515. doi: 10.4269/ajtmh.13-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kizza FN, List J, Nkwata AK, Okwera A, Ezeamama AE, Whalen CC, Sekandi JN. Prevalence of latent tuberculosis infection and associated risk factors in an urban African setting. BMC Infect Dis. 2015;15(1):165. doi: 10.1186/s12879-015-0904-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shanaube K, Hargreaves J, Fielding K, Schaap A, Lawrence K-A, et al. Risk factors associated with positive QuantiFERON-TB gold in-tube and tuberculin skin tests results in Zambia and South Africa. PLoS One. 2011;6(4):e18206. doi: 10.1371/journal.pone.0018206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kritzinger FE, Den Boon S, Verver S, Enarson DA, Lombard CJ, Borgdorff MW, Gie RP, Beyers N. No decrease in annual risk of tuberculosis infection in endemic area in Cape Town, South Africa. Trop Med Int Health. 2009;14(2):136–142. doi: 10.1111/j.1365-3156.2008.02213.x. [DOI] [PubMed] [Google Scholar]
- 35.Lienhardt C, Fielding K, Sillah J, Tunkara A, Donkor S, Manneh K, Warndorff D, McAdam KP, Bennett S. Risk factors for tuberculosis infection in sub-Saharan Africa: a contact study in The Gambia. Am J Respir Crit Care Med. 2003;168(4):448–455. doi: 10.1164/rccm.200212-1483OC. [DOI] [PubMed] [Google Scholar]
- 36.Gustafson P, Lisse I, Gomes V, Vieira CS, Lienhardt C, Nauclér A, Jensen H, Aaby P. Risk factors for positive tuberculin skin test in Guinea-Bissau. Epidemiology. 2007;18(3):340–347. doi: 10.1097/01.ede.0000259987.46912.2b. [DOI] [PubMed] [Google Scholar]
- 37.Zelner JL, Murray MB, Becerra MC, Galea J, Lecca L, Calderon R, Yataco R, Contreras C, Zhang Z, Grenfell BT, et al. Age-specific risks of tuberculosis infection from household and community exposures and opportunities for interventions in a high-burden setting. Am J Epidemiol. 2014;180(8):853–861. doi: 10.1093/aje/kwu192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Middelkoop K, Bekker L-G, Morrow C, Lee N, Wood R. Decreasing household contribution to TB transmission with age: a retrospective geographic analysis of young people in a South African township. BMC Infect Dis. 2014;14(1):221. doi: 10.1186/1471-2334-14-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wood R, Racow K, Bekker L-G, Morrow C, Middelkoop K, Mark D, Lawn SD. Indoor social networks in a South African township: potential contribution of location to tuberculosis transmission. PLoS One. 2012;7(6):e39246. doi: 10.1371/journal.pone.0039246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnstone-Robertson SP, Mark D, Morrow C, Middelkoop K, Chiswell M, Aquino LD, Bekker L-G, Wood R. Social mixing patterns within a South African township community: implications for respiratory disease transmission and control. Am J Epidemiol. 2011;174(11):1246–55. doi: 10.1093/aje/kwr251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wood R, Johnstone-Robertson S, Uys P, Hargrove J, Middelkoop K, Lawn SD, Bekker L-G. Tuberculosis transmission to young children in a South African community: modeling household and community infection risks. Clin Infect Dis. 2010;51(4):401–408. doi: 10.1086/655129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andrews JR, Morrow C, Walensky RP, Wood R. Integrating social contact and environmental data in evaluating tuberculosis transmission in a South African township. J Infect Dis. 2014;210(4):597–603. doi: 10.1093/infdis/jiu138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Legesse M, Ameni G, Mamo G, Medhin G, Bjune G, Abebe F. Community-based cross-sectional survey of latent tuberculosis infection in Afar pastoralists, Ethiopia, using QuantiFERON-TB Gold In-Tube and tuberculin skin test. BMC Infect Dis. 2011;11(1):89. doi: 10.1186/1471-2334-11-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.den Boon S, van Lill SWP, Borgdorff MW, Verver S, Bateman ED, Lombard CJ, Enarson DA, Beyers N. Association between smoking and tuberculosis infection: a population survey in a high tuberculosis incidence area. Thorax. 2005;60(7):555–557. doi: 10.1136/thx.2004.030924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dodd PJ, Looker C, Plumb ID, Bond V, Schaap A, Shanaube K, Muyoyeta M, Vynnycky E, Godfrey-Faussett P, Corbett EL, et al. Age- and sex-specific social contact patterns and incidence of mycobacterium tuberculosis infection. Am J Epidemiol. 2016;183(2):156–166. doi: 10.1093/aje/kwv160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Uys P, Marais BJ, Johnstone-Robertson S, Hargrove J, Wood R. Transmission elasticity in communities hyperendemic for tuberculosis. Clin Infect Dis. 2011;52(12):1399–1404. doi: 10.1093/cid/cir229. [DOI] [PubMed] [Google Scholar]
- 47.Boccia D, Hargreaves J, Ayles H, Fielding K, Simwinga M, Godfrey-Faussett P. Tuberculosis infection in Zambia: the association with relative wealth. Am J Trop Med Hyg. 2009;80(6):1004–1011. [PMC free article] [PubMed] [Google Scholar]
- 48.Pai M, Kalantri S, Dheda K. New tools and emerging technologies for the diagnosis of tuberculosis: Part I. Latent tuberculosis. Expert Rev Mol Diagn. 2006;6(3):413–422. doi: 10.1586/14737159.6.3.413. [DOI] [PubMed] [Google Scholar]
- 49.Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents. MMWR Recomm Rep. 2009;58(RR-4):1–207. [PubMed] [Google Scholar]
- 50.Lindsay RP, Shin SS, Garfein RS, Rusch ML, Novotny TE. The Association between active and passive smoking and latent tuberculosis infection in adults and children in the united states: results from NHANES. PLoS One. 2014;9(3):e93137. doi: 10.1371/journal.pone.0093137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Patra J, Bhatia M, Suraweera W, Morris SK, Patra C, Gupta PC, Jha P. Exposure to second-hand smoke and the risk of tuberculosis in children and adults: a systematic review and meta-analysis of 18 observational studies. PLoS Med. 2015;12(6):e1001835. doi: 10.1371/journal.pmed.1001835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen C, Zhu T, Wang Z, Peng H, Kong W, Zhou Y, Shao Y, Zhu L, Lu W. High latent TB infection rate and associated risk factors in the Eastern China of low TB incidence. PLoS One. 2015;10(10):e0141511. doi: 10.1371/journal.pone.0141511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Horne DJ, Campo M, Ortiz JR, Oren E, Arentz M, Crothers K, Narita M. Association between smoking and latent tuberculosis in the US population: an analysis of the National Health and Nutrition Examination Survey. PLoS One. 2012;7(11):e49050. doi: 10.1371/journal.pone.0049050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.den Boon S, Verver S, Marais BJ, Enarson DA, Lombard CJ, Bateman ED, Irusen E, Jithoo A, Gie RP, Borgdorff MW, et al. Association between passive smoking and infection with Mycobacterium tuberculosis in children. Pediatrics. 2007;119(4):734–739. doi: 10.1542/peds.2006-1796. [DOI] [PubMed] [Google Scholar]
- 55.Oni T, Gideon HP, Bangani N, Tsekela R, Seldon R, Wood K, Wilkinson KA, Goliath RT, Ottenhoff TH, Wilkinson RJ. Smoking, BCG and employment and the risk of tuberculosis infection in HIV-infected persons in South Africa. PLoS One. 2012;7(10):e47072. doi: 10.1371/journal.pone.0047072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68(12):2240–2246. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 57.Narasimhan P, Wood J, MacIntyre CR, Mathai D. Risk factors for tuberculosis. Pulm Med. 2013;2013:11. doi: 10.1155/2013/828939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gao LLW, Bai L, Wang X, Xu J, Catanzaro A, Cárdenas V, Li X, Yang Y, JDu J, et al. Latent tuberculosis infection in rural China: baseline results of a population-based, multicentre, prospective cohort study. Lancet Infect Dis. 2015;15:310–319. doi: 10.1016/S1473-3099(14)71085-0. [DOI] [PubMed] [Google Scholar]
- 59.Feske ML, Teeter LD, Musser JM, Graviss EA. Giving TB wheels: Public transportation as a risk factor for tuberculosis transmission. Tuberculosis. 2011;91(Supplement 1(0)):S16–S23. doi: 10.1016/j.tube.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 60.Zamudio C, Krapp F, Choi HW, Shah L, Ciampi A, Gotuzzo E, Heymann J, Seas C, Brewer TF. Public transportation and tuberculosis transmission in a high incidence setting. PLoS One. 2015;10(2):e0115230. doi: 10.1371/journal.pone.0115230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bell BA, Ferron JM, Kromrey JD. Cluster size in multilevel models: the impact of sparse data structures on point and interval estimates in two-level models. JSM Proceedings, Section on Survey Research Methods. Alexandria, VA: American Statistical Association. 2008:1122–1129.
- 62.Farhat M, Greenaway C, Pai M, Menzies D. False-positive tuberculin skin tests: what is the absolute effect of BCG and non-tuberculous mycobacteria?[Review Article] Int J Tuberc Lung Dis. 2006;10(11):1192–1204. [PubMed] [Google Scholar]
- 63.Tissot F, Zanetti G, Francioli P, Zellweger J-P, Zysset F. Influence of bacille Calmette-Guérin vaccination on size of tuberculin skin test reaction: to what size? Clin Infect Dis. 2005;40(2):211–217. doi: 10.1086/426434. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the parent study are not publically available due to data sharing agreement restrictions in place. Readers may contact Dr. Annelies van Rie for further clarification.


