When the draft sequence of the human genome was published in February 2001, Nature and Science featured human faces on their covers. As striking as these images were, they could be seen as more art than science, because systematic genome-wide sequencing had yet to be applied to individuals for medical purposes. What a difference a decade makes. Real faces are now appearing that demonstrate the medical value of comprehensive genome sequencing.
Researchers with NIH’s Undiagnosed Diseases Program recently identified a genetic cause for a rare and debilitating vascular disorder that had baffled the medical field and evaded diagnosis. The discovery was spurred by the cases of Louise Benge and Paula Allen, two middle-aged sisters from Kentucky who had calcification of the large blood vessels and joints in their hands and feet, in the absence of any effect on coronary arteries. Thanks to genomic analyses (just published in the New England Journal of Medicine), they now know that their severe leg and joint pain stems from a a mutation in NT5E, which encodes a protein that converts AMP to adenosine. Better understanding of the disease mechanism will help to guide development of treatments for such patients, as well as illuminate metabolic pathways involved in calcification.
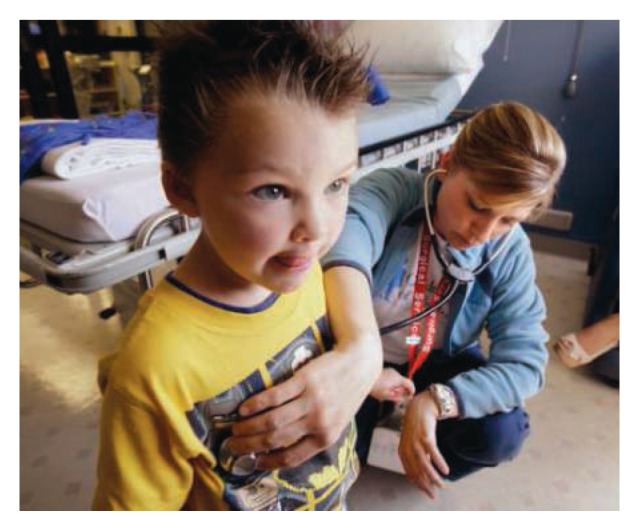
An even more impressive story of the revolution that genomic analysis is bringing to the clinic relates to Nic Volker (shown above), a 6-year-old Wisconsin boy who developed inflammatory bowel disease shortly before his second birthday. Multiple intestinal fistulas occurred, making it impossible for him to eat normally. Despite numerous tests and more than 100 surgeries, doctors remained at loss for a diagnosis and the little boy grew sicker. Then, researchers at the Medical College of Wisconsin carried out whole-exome sequencing, examining the protein-coding regions of every gene in Nic’s genome. They identified a mutation in his XIAP gene. XIAP mutations were not previously associated with bowel symptoms, but had been linked to a severe blood disorder that is curable through bone marrow transplantation. The medical team raised the possibility of a transplant, which would not have been considered without a firm diagnosis. It was performed in July 2010, using stem cells from the cord blood of a matched, healthy donor. Seven months later, Nic appears to be on the road to recovery. While he is still on immunosuppressants, doctors report the new stem cells are stably engrafted, blood counts are good, and there’s been no return of bowel disease (http://journals.lww.com/geneticsinmedicine/Documents/GIM200819_Revised.pdf). More important to Nic, he can finally eat solid foods!
These cases, and others that are now appearing in the literature, document that we stand at a significant juncture—the once-hypothetical medical benefits of individual genome sequencing are beginning to be realized in the clinic. This transition will require hard work and ingenuity; in fact, it’s one of the many reasons that NIH plans to create a National Center for Advancing Translational Sciences. My hope is that when the day arrives to celebrate the 20th anniversary of the original human genome publications, we will be able to look at a world filled with the faces of people whose health has been improved by the sequencing of their genomes.


