Abstract
Given the yearly challenge of seasonal influenza and the potential catastrophic consequences of future pandemics, the need for intensive basic and clinical influenza research is unquestionable. Although the fruits of decades of research have enabled dramatic improvements in our ability to prevent and treat influenza, many fundamental questions remain, including those related to the complex factors associated with host switching and transmission of influenza viruses. Recent public concern over two H5N1 influenza manuscripts that studied the transmissibility of influenza viruses has triggered intense discussion on dual-use research and the way forward.
Influenza A virus is an ancient and persistent threat to individual and global health (Fig. 1). Seasonal influenza (which occurs annually, usually in winter) kills ~500,000 people globally and up to 50,000 people in the United States each year. Influenza viruses have animal reservoirs, especially in birds and pigs. They can undergo extensive genetic changes and even jump species, sometimes resulting in a virus to which humans may be highly vulnerable. Such an event can lead to a global health disaster; global influenza pandemics have occurred only three times in this past century. A prime example is the 1918 influenza pandemic, which killed between 50 and 100 million people worldwide and caused enormous social and economic disruption. Influenza A viruses circulate widely and are constantly evolving toward pandemic capability, as seen again in 1957, 1968, and 2009 (1). There is thus a clear danger of future pandemics.
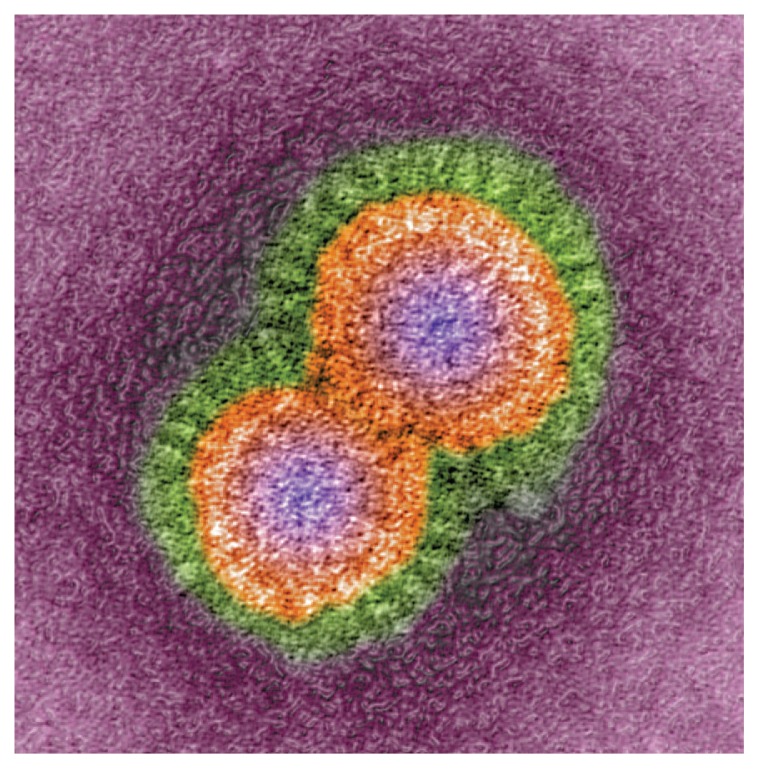
Fig. 1.
H5N1 avian influenza virus particles, colored transmission electron micrograph. Magnification: ×670,000 when printed 10 cm wide.
Over the last decade, a highly pathogenic avian influenza virus (genus A; subtype H5N1) has emerged among chickens (2). Rarely, the virus has spread to humans, usually individuals with heavy exposure to infected birds. Since 2003, ~600 confirmed cases have occurred in humans in more than a dozen countries. Nearly 60% of these reported cases have resulted in death (3). Because it has been impossible thus far to completely eliminate the virus from chicken flocks or from wild birds or to prevent transmission to mammals, there is a persistent danger that H5N1 viruses [which have continually mutated and evolved (2)] will eventually become more easily transmissible to and among humans. Because humans are not specifically immune to H5N1 influenza, this scenario would have the makings of a potentially devastating pandemic.
One of the goals of pandemic influenza research is to recognize and anticipate how viruses are evolving in the wild toward a phenotype that is dangerous to humans, thereby staying one step ahead of potential pandemics. In this regard, compelling research questions relevant to global health and pandemic preparedness include determining whether highly pathogenic viruses, such as H5N1, have the ability to mutate and/or reassort with another influenza virus to become readily transmissible by the airborne route among humans. If so, (i) what is the likelihood that such mutations or reassortments will happen in nature? (ii) Is there a genetic signature of such a virus that might be helpful in surveillance? (iii) Would such a virus be highly pathogenic for humans? And (iv), would such a virus be sensitive to currently available antiviral drugs and vaccines, or would new ones be necessary? In response to these and related questions, the National Institutes of Health (NIH) has intensified the research we conduct and support on pandemic influenza. Much of this research is specifically focused on developing improved countermeasures, including a “universal” influenza vaccine that would protect people from multiple influenza subtypes. In complementary research, NIH-supported scientists study the factors involved in the pathogenesis and transmissibility of H5N1 and other influenza viruses to nonhuman mammals (mice, guinea pigs, ferrets, and nonhuman primates) to identify potential clues to the determinants of the same properties in humans.
Within this context, global attention has been paid recently to two NIH-funded studies of H5N1 transmissibility and pathogenesis in ferrets. In those studies, H5N1 viruses were made transmissible via respiratory droplets among ferrets by engineering the virus; well-described and published protocols including reverse genetics, reassortment, and passaging of viruses in mammals were used. Manuscripts describing the studies (4, 5) have generated an unprecedented degree of discussion, concern, and disagreement among scientists, as well as the public, regarding whether the experiments should have been performed in the first place and whether they should be published in their entirety. Major sources of concern have been that the results might be used by bioterrorists to harm the public or that the virus might accidentally escape and cause a pandemic.
Research on H5N1 viruses, including the experiments reported in these two papers (4, 5), is comparable to that which has been conducted over decades with other seasonal and pandemic influenza viruses in ferrets and other animal models. The use of the ferret as an animal model for influenza transmissibility dates back to the 1930s, as ferrets are easily infected with influenza and sneeze when infected, which is useful for studying the airborne route needed for sustained human-to-human transmission. Understanding the virus characteristics associated with enhanced transmissibility—even in an imperfect animal model, such as the ferret—can benefit surveillance for naturally evolving wild viruses if they continually mutate toward a “genomic signature” that could be recognized as potentially predictive of a certain phenotype. Given the complexities of viral transmission, a virus’s ability to adapt to a host species, pathogenesis (a virus’s ability to cause disease), and the interrelation among these factors, which are likely to be unique to each influenza virus, any particular genomic signature will not necessarily predict how a given virus will act. Nonetheless, studies such as these provide incremental knowledge that the scientific community can build upon. A more in-depth understanding of the genetic evolution of influenza viruses should positively affect our ability to recognize and respond to influenza outbreaks.
However, whenever one deliberately manipulates a virus or a microbe, it is always possible, at least theoretically, that the research results could be used by bioterrorists to intentionally cause harm, or that an accidental release of a pathogen from a laboratory could inadvertently cause harm. Such research is referred to as “dual-use research,” as the research potentially has both positive and negative applications. A particular subset of dual-use research is referred to as “dual-use research of concern” or DURC. DURC is defined as life sciences research that, on the basis of current understanding, can be reasonably anticipated to provide knowledge, information, products, or technologies that can be directly misapplied to pose a significant threat with broad potential consequences to public health and safety, agricultural crops and other plants, animals, the environment, materiel, or national security (6). If a particular experiment is identified as DURC, that designation does not inherently mean that such research should be prohibited or not widely published. However, it does call for us to balance carefully the benefit of the research to public health, the biosafety and biosecurity conditions under which the research is conducted, and the potential risk that the knowledge gained from such research may fall into the hands of individuals with ill intent. Research that could enhance the transmissibility of H5N1 viruses clearly is DURC.
In this regard, the question of whether to publish the two H5N1 studies in ferrets has been intensively discussed by an independent federal advisory committee known as the National Science Advisory Board for Biosecurity (NSABB) (7, 8). On the basis of their recommendations and other evaluations, the U.S. government agreed that the research is important for the public health and should be published. However, important lessons were learned along the way and, appropriately, triggered an examination of our approach concerning the conduct, oversight, and communication of DURC. In this regard, the U.S. government announced on 29 March 2012 the U.S. Government Policy for Oversight of Life Sciences Dual Use Research of Concern (6). This policy document outlines, for federal departments and agencies that conduct or fund life sciences research, steps to determine whether projects fall under the definition of DURC, to assess the risks and benefits of these projects, to review them regularly, and to develop risk mitigation plans. In the process of weighing the potential risks and benefits of publishing these two manuscripts (4, 5), it also became clear that, when possible, it is critical to identify research with DURC potential before the initiation of the project and, certainly, before the results are submitted for publication. Such monitoring in the case of NIH-funded research requires the concerted effort of all involved, including scientists applying for or in receipt of NIH funding and NIH program officials. Additional guidelines will be needed as well to assist biosafety committees in evaluating DURC at the institutions where the research is conducted.
Furthermore, as a result of the public discussion of these two manuscripts, major gaps in our knowledge of influenza became painfully obvious. For example, there was considerable scientific debate about how well data from the ferret model can be extrapolated to understand influenza virus transmission and pathogenesis in humans. An H5N1 virus strictly adapted for ferret transmissibility may not be entirely relevant to humans. Moreover, although it is likely that the officially reported 60% case-fatality rate for human H5N1 influenza is artificially high (because nonfatal cases are less likely to be reported), there are limited surveillance data on which to base a more accurate estimate. NIH has begun a dialogue with the influenza research community about addressing these and other questions and will initiate a more strategic approach to defining the research gaps that must be addressed in order to responsibly move the field forward. In addition to identifying research gaps, the discussion of these manuscripts underscores the important practical issues of implementing rapid turnaround time between virus isolation and sequencing to provide real-time surveillance.
Finally, despite the importance of performing influenza research that may have DURC potential, this recent experience has underscored the fact that civil society needs to be involved in the dialogue early on. Clearly, research should be conducted and published only if the potential benefits to society outweigh the risks to national security and the potential harm to society. The risk/benefit calculation for certain experiments and their communication is not always obvious, and the current experience reflected considerable disagreement even in the scientific community. The ultimate goal of the new U.S. government-wide DURC policy is to ensure that the conduct and communication of research in this area remain transparent and open and that the risk/ benefit balance of such research clearly tips toward benefitting society. The public, which has a stake in the risks and the benefits of such research, deserves a rational and transparent explanation of how decisions are made. It is hoped that the upcoming dialogue related to the new DURC policy will be productive. A social contract among the scientific community, policy-makers, and the general public that builds trust is essential for success of this process.
References
- 1.Morens DM, Taubenberger JK, Fauci AS. N Engl J Med. 2009;361:225. doi: 10.1056/NEJMp0904819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan Y, et al. Proc Natl Acad Sci USA. 2004;101:8156. [Google Scholar]
- 3.World Health Organization (WHO) Cumulative number of confirmed human cases of avian influenza A (H5N1) reported to WHO. 2012. www.who.int/influenza/human_animal_interface/H5N1_cumulative_table_archives/en/index.html.
- 4.Herfst S, et al. Science. 2012;336:1534. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imai M, et al. Nature. 2012 doi: 10.1038/nature10831. [DOI] [Google Scholar]
- 6.US Government Policy for Oversight of Life Sciences Dual Use Research of Concern. 2012. http://oba.od.nih.gov/oba/biosecurity/PDF/United_States_Government_Policy_for_Oversight_of_DURC_FINAL_version_032812.pdf.
- 7.NIH press statement on the NSABB review of H5N1 research. 2011. www.nih.gov/news/health/dec2011/od-20.htm.
- 8.NSABB. Findings and Recommendations. 2012. http://oba.od.nih.gov/oba/biosecurity/PDF/03302012_NSABB_Recommendations.pdf.