Abstract
Objectives:
Typical rehabilitation programs following total hip arthroplasty and total knee arthroplasty include joint range of motion and muscle-strengthening exercises. Balance and balance exercises following total hip arthroplasty and total knee arthroplasty have not received much attention. The purpose of this study was to determine whether an intervention of balance exercises added to a typical rehabilitation program positively affects patients’ balance.
Methods:
A total of 63 patients were provided with outpatient physical therapy at their home. Patients were randomly assigned to either typical (n = 33) or balance (n = 30) exercise group. The typical group completed seven typical surgery-specific joint range of motion and muscle-strengthening exercises, while the balance group completed the typical exercises plus three balance exercises. After 5 weeks of administering the rehabilitation program, patients’ balance was assessed on a force plate using 95% ellipse area of the center of pressure amplitude.
Results:
Patients in the balance group demonstrated significant reduction in the 95% ellipse area for the anterior and posterior lean standing conditions (p < 0.01).
Conclusion:
Balance exercises added to the typical outpatient physical therapy program resulted in significantly greater improvements in balance for participants with total hip arthroplasty or total knee arthroplasty, compared to the typical exercise program alone. Physical therapists might consider the use of balance exercises to improve balance in individuals in the acute post-operative phase following total hip arthroplasty or total knee arthroplasty.
Keywords: Total hip arthroplasty, total knee arthroplasty, balance exercises, force plate, 95% ellipse area
Introduction
Balance while standing requires the integration of different components such as (1) the sensory systems, (2) the central nervous system and (3) the motor system.1 The sensory and motor systems provide input through the mechanoreceptors in joint capsules, ligaments, tendons, muscles and from cutaneous receptors.2 The integrity of joints, ligaments, tendons and muscles play an important role in providing proprioceptive feedback to maintain balance.3 Although the effects of hip osteoarthritis (OA) on hip joint proprioception are unclear, knee OA has been reported to result in impairment of proprioception in the knee joint.3 In addition, joint replacement may prevent further deterioration in proprioception but it may not improve proprioception in either hip4 or knee joints.5
Balance studies in individuals with knee OA have reported that these patients have significantly reduced balance ability.6,7 Also, a study on balance assessed in elderly male individuals (69 ± 4 years) with hip OA reported reduced balance ability in these individuals.8 But a study on balance in a relatively younger age group of individuals (56 ± 5 years) with hip OA reported no change in their balance ability.9 However, the primary reason to undergo total hip arthroplasty (THA) or total knee arthroplasty (TKA) as a result of hip or knee OA is to reduce pain and stiffness, and to improve joint range of motion (ROM), muscle strength and physical function10,11 while little emphasis is placed on improving balance.12
Studies on standing balance in individuals following THA have reported conflicting results. Wykman and Goldie13 reported significant improvement in standing balance assessed using stabilometry and sway patterns in individuals after 6 and 12 months following THA compared to pre-surgery measures. In contrast, Ellison et al.14 reported no significant difference in standing balance, measured with the Berg Balance Scale (BBS), between individuals following THA and a group of age- and gender-matched healthy subjects. Nallegowda et al.15 also reported no significant difference in standing balance, as assessed using the sensory organization test following THA as compared to age- and gender-matched subjects. Trudelle-Jackson et al.16 reported a significant impairment in the standing balance ability of individuals even 12 months after THA surgery.
Studies on standing balance in individuals following TKA have also reported contradictory results. While Swanik et al.17 reported mild improvements in standing balance in subjects following TKA, McChesney and Woollacott18 reported no change. Swanik et al.17 tested 20 subjects about 1.5 months prior to TKA and again at least 6 months after surgery. Balance was assessed using a computerized platform capable of tilting side-to-side and front-to-back. The authors reported that subjects were able to stand on an unstable platform with less postural deviation after TKA as compared to postural deviations pre-surgery. McChesney and Woollacott18 assessed balance of 22 elderly subjects over the age of 70 years who were divided into age- and gender-matched groups; one group had undergone TKA and the other group did not. No significant differences were reported in the anterior and lateral center of pressure (CoP) amplitude between the two groups. Both investigators used two-legged standing tests and did not attempt to distinguish between surgical and non-surgical sides.
Impairment in balance has been associated with increased incidence of falls and has been reported in individuals after THA or TKA surgery.1,19,20 The cost of falling is high to the individual in terms of both physical and psychological trauma,20 as well as the financial burden to the health care system.20 For these reasons, it is important to examine interventions that can prevent these falls by improving balance in individuals following THA or TKA surgery. Aside from reporting continued impairment of balance in individuals after THA or TKA, Trudelle-Jackson et al.16 and Gage et al.21 both suggested incorporating balance exercises to improve balance in individuals following surgery without actually using balance exercises in their studies. An intervention of balance exercises added to individuals’ home exercise programs could provide a high benefit for a relatively low cost. The first step, however, is to determine whether several simple balance exercises added to a typical home exercise program can produce a meaningful positive effect.
The purpose of the study was to determine whether an intervention of balance exercises added to a typical rehabilitation program for individuals following THA or TKA positively affects the CoP measure on a force platform during two-limb and one-limb standing conditions.
Methods
A randomized controlled trial was performed in London-Middlesex County, Ontario, Canada, between April 2006 and April 2009. Participants for the study were recruited from a large outpatient home physical therapy provider. Participants were seen individually at their place of residence by a physical therapist on the first or second day after hospital discharge, typically 7–10 days following their surgery. At their first post-operative home visit, qualified individuals were randomly assigned to a typical group or to a balance group using a coin-toss method. Head was allocated to typical group and tail was allocated to balance group. Participants were asked to flip the coin and the outcome decided their group allocation. The physical therapists started administering intervention to the participants on the same day after the baseline assessments and group allocation were completed. The intervention program was administered for a period of 5 weeks. At the end of 5 weeks, follow-up assessments were completed within 3–6 days in a biomechanics laboratory at an academic center. At the beginning of the study, the physical therapists visited one patient for the first as well as the follow-up visits together to ensure that similar and consistent information was conveyed to all participants with respect to instructions during assessment on outcome measures and also during implementation of the intervention. The two physical therapists who participated in the study had 3–4 years experience in working with patients with THA and TKA and had routinely used the self-reported outcome measures and physical measures for assessments. Ethical approval for the study was obtained from the Research Ethics Board for Health Sciences Research Involving Human Subjects, and all participants provided written consent prior to participation in the study.
Participants
Participants in this study were a sample of convenience of consecutive individuals referred to a large outpatient provider of home physical therapy after either THA or TKA. Charts of all referred individuals were reviewed to determine their eligibility for participation in the study with respect to the operated joint, any surgery-related complications and other health conditions. Individuals who met the inclusion/exclusion criteria were advised of the study. The inclusion criteria for the study participants were that they had unilateral THA or TKA as a result of hip or knee joint OA and were advised by their surgeon to weight bear as tolerated following surgery. Individuals with revision of THA or TKA or those who had been advised to remain non-weight bearing or partial weight bearing on the operated leg were excluded. Individuals with neurological conditions such as hemiplegia, peripheral neuropathy, vestibular disorders and Parkinson’s disease that might affect their balance and those who were considered unable to communicate or follow instructions were also excluded from the study. As advised by the surgeons, all participants were taking blood thinners for prevention of blood clots and pain medication as needed following surgery. The THA and TKA surgery on the participants was performed by different surgeons, and the information on the surgical technique used was not available in the participants’ charts.
Intervention
Intervention was started on the first post-operative home visit following baseline assessment. Participants in the typical group completed joint ROM and muscle-strengthening exercises and participants in the balance group completed joint ROM, muscle-strengthening and additional balance exercises (Appendix 1). Thereafter, participants were visited by their physical therapist once or twice per week until 5 weeks. Overall, participants received 4–6 home visits during the 5 weeks they were seen for home visits. All participants also received routine education about safety and fall prevention, transfers and limb positioning. All participants were provided with exercise sheets that included written and photographed instructions for each prescribed exercise, an exercise compliance table and a contact phone number for their physical therapist.
Participants were advised to complete 10 repetitions of each exercise 3 times a day and to keep a record on the compliance table. Typical joint ROM and muscle-strengthening exercises were completed only on the operated leg. Each participant was taught exercises in a sequence that the physical therapists considered most advisable—beginning with the simpler and progressing to more demanding exercises. Exercise execution and repetitions were reviewed by the physical therapist at each home visit. All participants were able to perform all exercises by the second visit and all completed the 5-week intervention period.
Outcome measures
Baseline assessments were completed using two self-reported outcome measures—the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Activities-specific Balance Confidence (ABC) scale—and two physical measures—the BBS and the Timed Up and Go (TUG) test. While the self-reported outcome measure WOMAC has 24 items and is used to assess pain, stiffness and physical function in patients with hip and knee OA,22 the ABC has 16 items and is used to assess the level of patients’ balance confidence while performing specific activities.23 The BBS is a 14-item therapist-administered physical measure to assess balance in the elderly,24 and the TUG is a test of functional mobility completed using a single chair and a 3-m walkway.25
At the end of 5 weeks of intervention, follow-up assessments were completed by the primary investigator (one of the two participating physical therapists) within 3–6 days in a biomechanics laboratory at an academic center. Follow-up assessments also included the two self-reported and physical measures, as well as a force-plate measure. All participants who completed the force-plate measures also completed the self-reported and physical measures. Participants in the typical group and the balance group were found to be similar on the self-reported (WOMAC—typical = 36 ± 11, balance = 37 ± 11; ABC—typical = 37 ± 19, balance = 36 ± 24) and the physical measures (BBS—typical = 37 ± 10, balance = 34 ± 7; TUG—typical = 32 ± 17, balance = 48 ± 26) at baseline assessments. Also, participants with THA and TKA were found to be similar on the self-reported and physical measures at baseline, as well as follow-up assessments, and the results of these self-reported and physical measures are already published by our research group.26 The data that were gathered on the force-plate measure on the sample population of the study already published by our research group has been presented in this study. The authors thought it appropriate and desirable to separate the force-plate data set because (1) the data from the force-plate measure was extensive, (2) to give accurate and balanced presentation of the analyses to the reader, (3) to foster ease in absorption of the data by the reader and to avoid confusion and (4) to enhance the scientific understanding of the analyses for the research question that is being addressed.
Force platform
Balance was assessed using an AMTI (Advanced Mechanical Technology Inc., Newton, MA, USA) stationary 51 cm × 46 cm steel force plate with implanted strain gauges, an amplifier and a computer with Biosoft software (Advanced Mechanical Technology Inc.) which computed the CoP excursion area while the subject stood on the force plate.
Previous studies have utilized CoP amplitude, which is the total distance traveled in the medial–lateral and anterior–posterior directions to describe CoP patterns during balance assessments.8,9 For the purposes of this study, the 95% ellipse area of the CoP amplitude in medial–lateral and anterior–posterior directions was used as the CoP measure and was calculated in cm2, using the Biosoft software. The 95% ellipse area covers 95% of the data points of the CoP amplitude in the medial–lateral and anterior–posterior direction, which according to Lee and Park27 provides good information about postural stability in anterior–posterior and medial–lateral directions, and is not biased by outliers. Swanenburg et al.28 have reported a good reliability of 95% ellipse area of the CoP using AMTI force plate to assess balance on two-legged stance in elderly patients.
After 5 weeks of participation in the home exercise program, standing balance was assessed by the primary investigator using the force plate in the biomechanics laboratory. Participants were comfortably dressed in shirt and pants and were bare foot during the tests. Before the balance tests, participants were comfortably seated on a chair placed behind the force plate while the testing procedure was demonstrated and reviewed. Participants were encouraged to ask any questions related to the procedure and report any fatigue they experience during the testing.
A walker was positioned immediately in front of the force plate for safety purposes. The participants were instructed to use the arms of the chair to stand up and place their feet on the pre-marked foot impressions on the force plate, the right foot on the right-side impression and the left foot on the left-side impression. For the one-legged standing conditions, the participants were asked to bend the knee and lift the non-testing leg. Participants were asked to use the walker to achieve balance before each test (Figure 1). Once the participants obtained balance, they were asked to release the walker and stand in the test position for 10 s during the data-capture interval. They were advised to use the walker in case they lost their balance. For safety reasons and to enhance the participant’s confidence, another physical therapist was present by the participant’s side to guard against any major loss of balance and potential fall. The 10-s data collection period began when the participant said “Now,” indicating that they believed they had established balance.
Figure 1.

Participant in two-limb standing position on the force plate for balance testing.
The balance testing comprised five test conditions performed with the participant’s eyes open. The five test conditions were as follows: (1) two-limb stance, (2) two-limb anterior lean stance, (3) two-limb posterior lean stance, (4) operated single-limb stance and (5) non-operated single-limb stance. Testing started with two-limb standing conditions where the participants were instructed to place weight equally on both feet, followed by the one-limb conditions. For the anterior and posterior lean stance, participants were instructed to lean anteriorly or posteriorly as far as they could comfortably maintain the position. Two repetitions of each test were completed, with a 10-s rest interval between repetitions during which the patient remained standing and used the walker for support as needed. Demonstration of the balance tests on the force plate was provided to the participants by the primary investigator prior to balance testing. No trial training was given to the participants to avoid any learning effect.
Statistical analyses
A two-way analysis of variance (ANOVA) tests were used to compare the two surgical groups (THA and TKA) by the two exercise groups (typical and balance) on age, height, mass, foot length and foot width. Two-way ANOVA tests were also used to examine the 95% ellipse area for each of the test conditions on the two surgical groups (THA and TKA) by two exercise groups (typical and balance). An average of the scores of the two repetitions for each test condition was used as the final score of 95% ellipse area for that condition. All statistical tests were completed using STATISTICA,29 and as five separate ANOVAs were done for the five test conditions, the α-level was corrected to 0.01 to denote statistical significance.
A priori power analysis using data from the previous study with subjects with TKA indicated that a sample of 20 participants in each group would have a power of 0.80 to detect a difference of five standard deviations between groups on the BBS at a significance level of 0.05.30 Patients with THA and TKA were pooled together to provide an adequate sample size in this study.
Results
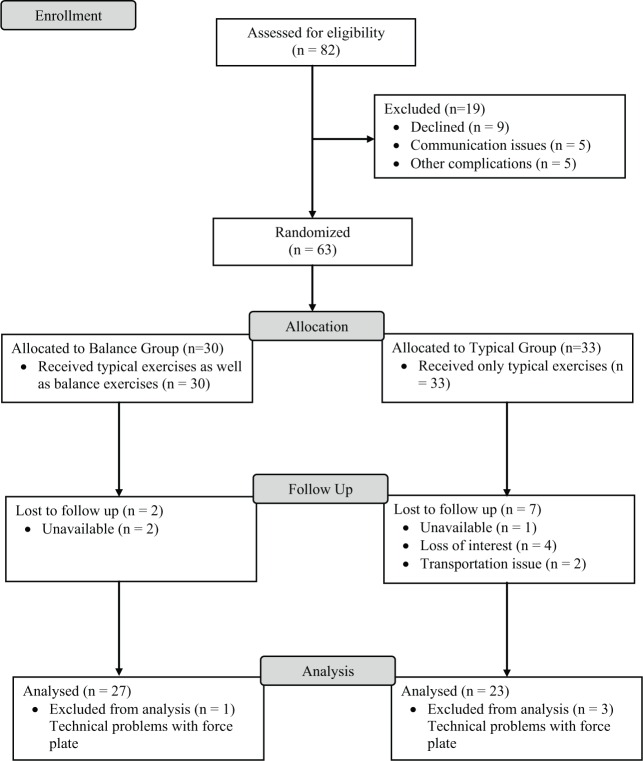
A total of 63 participants (22 males and 41 females) with a mean age of 66 ± 10 years were included in the study. Nine participants dropped out and did not complete the final balance testing. Reasons for dropping out included the following: (1) difficulty in getting transportation from patient’s home to the biomechanics laboratory, (2) traveling distance, (3) poor driving conditions during the winter months and (4) family functions and other appointments. Another four participants, who completed the exercise program but were not tested on the force plate due to technical problems with the equipment, were dropped from data analysis. Figure 2 shows the flow of participants in the study. Demographic information of participants who completed the study is presented in Table 1. No statistically significant differences in age, height, body mass, foot length and foot width were observed between the surgical (THA and TKA) and exercise (typical and balance) groups. Of the 50 participants, 30 were able to complete one-limb stance on their operated limb and 33 participants were able to complete one-limb stance on their non-operated limb. These participants identified pain rather than balance issues as the reason for not being able to complete the test. All participants were able to complete the two 10-s tests for all two-limb conditions that they considered not painful. No additional trials were required and no losses of balance during the tests were observed.
Figure 2.
Design and flow of participants through the trial.
Table 1.
Descriptive information for the participants (n = 50).
| Surgery |
THA |
TKA |
||
|---|---|---|---|---|
| Exercise group | Typical | Balance | Typical | Balance |
| Sample size (n) | 11 | 13 | 12 | 14 |
| Males (n) | 5 | 4 | 3 | 6 |
| Females (n) | 6 | 9 | 9 | 8 |
| Age (year) | 70 ± 6 | 67 ± 9 | 63 ± 10 | 63 ± 10 |
| Height (cm) | 158 ± 27 | 165 ± 6 | 164 ± 13 | 167 ± 10 |
| Mass (kg) | 75 ± 18 | 76 ± 15 | 89 ± 22 | 90 ± 22 |
| Foot length (cm) | 27 ± 3 | 25 ± 2 | 26 ± 3 | 26 ± 1 |
| Foot width (cm) | 29 ± 1 | 28 ± 2 | 29 ± 2 | 29 ± 1 |
THA: total hip arthroplasty; TKA: total knee arthroplasty; SD: standard deviation.
The 95% ellipse area covered by participants for each test condition in the balance and typical groups is provided in Table 2. The 2 two-limb standing conditions (anterior lean and posterior lean) were characterized by similar results on the ANOVAs—only the exercise group’s main effect was statistically significant (p < 0.01, Table 3). Participants in the balance group demonstrated a significant reduction in 95% ellipse area compared to the typical group. No statistically significant effects were observed for the two-limb stance and the 2 one-limb standing conditions (operated and non-operated limb). Data analyses using only those patients who completed all five test conditions (excluding those who were not able to perform the one-limb standing) produced identical results compared to results based on all participants including those who were not able to perform one-limb standing. Overall, no significant differences were observed between the THA and the TKA groups (p > 0.01), and all analyses were performed with the data on the THA and TKA groups pooled together.
Table 2.
Means and standard deviations for CoP area (cm2) for balance and typical groups.
| Test condition | Balance |
Typical |
||
|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | |
| Two-limb evenly distributed weight stance | 27 | 1.0 ± 1.0 | 23 | 2.7 ± 3.6 |
| Two-limb anterior lean stance | 27 | 1.5 ± 1.4 | 23 | 4.4 ± 3.7 |
| Two-limb posterior lean stance | 27 | 2.0 ± 1.9 | 23 | 5.3 ± 4.9 |
| Operated single-limb stance | 17 | 6.4 ± 6.3 | 13 | 7.3 ± 4.7 |
| Non-operated single-limb stance | 19 | 4.7 ± 5.0 | 14 | 8.6 ± 10.3 |
CoP: center of pressure; SD: standard deviation.
Table 3.
ANOVA summary table for CoP area of participants.
| Test condition | Subjects who completed the tests (n) | Surgery |
Exercise group |
Surgery ×Exercise group |
|||
|---|---|---|---|---|---|---|---|
| F-ratio | p-value | F-ratio | p-value | F-ratio | p-value | ||
| Two-limb evenly distributed weight stance | 50 | 0.41 | 0.52 | 5.11 | 0.03 | 1.45 | 0.24 |
| Two-limb anterior lean stance | 50 | 0.23 | 0.63 | 14.50 | 0.00* | 0.80 | 0.38 |
| Two-limb posterior lean stance | 50 | 0.15 | 0.70 | 10.00 | 0.00* | 1.03 | 0.32 |
| Operated single-limb stance | 30 | 1.64 | 0.21 | 0.72 | 0.40 | 2.79 | 0.11 |
| Non-operated single-limb stance | 33 | 0.00 | 0.97 | 2.02 | 0.17 | 2.63 | 0.12 |
CoP: center of pressure.
p<0.01.
Discussion
Participants in the balance group who performed balance exercises in addition to the typical joint ROM and muscle-strengthening exercises demonstrated better balance as compared to participants who performed only the typical exercises. Improvement in balance ability was found on two test conditions that involved standing on both limbs, the anterior lean and posterior lean standing conditions. The balance exercises used in this study perhaps improved the balance requirement to perform these two test conditions and did not address the balance requirement to perform single-limb stance or the static bilateral stance. Previous studies that assessed balance in individuals with TKA using force plates have also used two-limb standing tests and have showed them to be valid and reliable for assessing balance.17,18,31 Previous studies have also reported improvement in physical function as a result of joint ROM and muscle-strengthening exercises.32,33 In this study, balance exercises were added to the typical joint ROM and muscle-strengthening exercise program rather than replacing some of the typical exercises. This was done to determine whether balance exercises had any effect on balance in individuals following THA or TKA. Also, 5 weeks is typically the average duration for in-home rehabilitation program following THA or TKA after which patients go to the outpatient rehabilitation program in the hospital or clinical settings.
The seven typical joint ROM and muscle-strengthening exercises and the three balance exercises were selected by two physical therapists who routinely treated patients with THA and/or TKA. The exercises were described in various exercise protocols used in previous studies.32–35 In this study, the three added balance exercises were simple but they did challenge the balance of participants with THA or TKA. None of the participants in the balance group reported any problems from performing the balance exercises. Compliance was considered excellent, with 95% of participants reporting completion of all exercises as per the recommended frequency and number of repetitions. One participant in the balance group and two participants in the typical group did not perform exercises for a day due to a prior engagement.
This study also tested balance using one-limb standing conditions to examine balance directly as a result of either THA or TKA and minimize the contribution of the other limb in maintaining balance. On these tests, no significant difference was observed between participants in the balance group and typical group. Standing on either the operated limb or the non-operated limb was found to be a challenging task for the participants. Also, our balance intervention did not address the balance requirement necessary for one-limb stance. Of the 50 participants, only 30 were able to stand for 10 s on their operated limb and 33 participants on non-operated limb. As a result, sample sizes for the surgical group–exercise group combinations in the ANOVAs were relatively small, ranging from 6 to 11 per group. Furthermore, the observed standard deviations were relatively large for the means, which could have led to the non-significant results between the balance group and typical group for the one-limb standing tests. A study by Trudelle-Jackson et al.16 assessing balance in individuals with THA using one-limb standing positions on a force plate did so at about 1 year post-surgery and reported lower balance ability on the operated limb as compared to the non-operated limb. To our knowledge, this study is the first to assess balance in individuals with THA or TKA using one-limb standing position at an immediate post-surgery period.
The first 2 months after THA and TKA surgery are considered clinically important time periods during which patients must adapt to changes in their health status and techniques of performing physical function and mobility. In this post-surgery period, physical therapy is employed for rehabilitation purposes although patients are expected to continue their home exercise programs indefinitely. Results of this study suggest that balance exercises added to routine joint ROM and muscle-strengthening exercises for individuals following THA or TKA have a potential to improve balance ability as measured by CoP area. Improvement in balance could promote independence in mobility and function such as walking, stair climbing, getting in and out of vehicles and negotiating uneven terrain. Better balance could help individuals improve their balance confidence and help them understand their balance limits, enabling them to differentiate between functional activities that they can and cannot safely perform.
In this study, force-plate assessments on participants were performed in the acute post-operative period following their THA and TKA surgery. THA and TKA being major surgeries, patients have very limited physical abilities immediately after surgery due to consequent pain, swelling and stiffness in the operated limb. Presence of any other co-morbid condition also compromises the patients’ physical abilities along with their coping ability. Activity tolerance, as well as sanding tolerance, in these patients immediately after surgery is very low. Force-plate assessments are extensive and physically challenging to patients and require certain degree of physical ability and endurance. The protocol used for the force-plate analyses in this study included five test conditions that had one-limb standing task. Immediately after THA or TKA surgery, it is difficult for patients to perform not only one-limb standing task but also anterior and posterior lean standing tasks. Even if attempts were made to assess participants on force plate immediately after THA or TKA, it would not have been possible to gather enough data from these participants on all force-plate test conditions and would also have compromised the safety of participants. As a result, it was decided that participants in this study would be assessed on the force plate only after a period of few weeks following their THA or TKA surgery and after completion of the study intervention. Also, the outpatient home physical therapy provider and the physical therapists had no information of participants’ surgical status (date of surgery) or access to participants’ charts before surgery. Participants’ information could only be accessed upon their discharge to home following surgery when they were referred to the home physical therapy provider for physical therapy. As a result, pre-surgical force-plate assessments on participants were not completed.
Although this study did not had baseline (pretest) scores on the force-plate tests and only post-intervention (posttest) scores, the study design involved randomization and comparison groups (typical and balance). Portney and Watkins36 suggest that such “posttest-only design” also controls standard threats to internal validity and we can assume that the groups in the study are equivalent prior to intervention even without the pretest score and that its internal validity is strong. In addition, if pretest score on participants were obtained on force-plate tests, the participants may be sensitized to the force-plate test in a way that would influence their scores on a subsequent posttest.36 As a result, the external validity of the study design is also strong.36 Although researchers should not undermine the importance of the “pretest–posttest design,” the “posttest-only design” is identical to the “pretest–posttest design” except that a pretest is not administered to either group.36 The “posttest-only design” has been successfully used in a previous study to determine and compare lower limb force production during a single-leg horizontal press in operated and unoperated limbs in participants with TKA and the limb of age- and gender-matched control group.37 Another study by Bertocci et al.38 also used “posttest-only design” to evaluate differences in isokinetic hip flexion, extension and abduction muscle performance of limbs in participants with THA who completed outpatient or home-based physical therapy intervention compared to healthy participants.
Participants in this study represented a sample of convenience composed of patients referred to home-based outpatient physical therapy within a limited geographical area, and thus the generalizability of the results may be limited. All participants were discharged from the hospital after they fulfilled the basic criteria required by the surgeon of the operated hip and knee joint ROM being 0 –90, and participants being independent in basic transfers, mobility and stair climbing. Also, all participants had been advised by their surgeon to weight bear as tolerated on the operated limb. Consequently, the results of the study may not be generalized to individuals with THA and TKA who are advised to partial weight bear or non-weight bear on the operated limb, individuals with hip and knee joint ROM limited within 0 –90 or residual deformities such as genu varum and individuals dependent for basic transfers, mobility and stair climbing. This study examined the effectiveness of typical and added balance exercises used during a relatively short period following THA or TKA surgery, and other types of exercises were not evaluated. Long-term, 12–24 weeks, post-surgery assessments were not completed, and so the long-term effects of the exercises are not known. In addition, the therapists were not blinded to the participants’ group allocation.
In conclusion, the addition of three balance exercises to typical joint ROM and muscle-strengthening exercises has potential to improve two-limb standing balance in individuals following THA or TKA as demonstrated by a significant reduction in the 95% ellipse area of the CoP amplitude in participants who performed balance exercises in addition to a typical exercise protocol. Whether these balance improvements can be preserved longer than 5 weeks after THA or TKA surgery requires further study. Future studies could also possibly investigate the effects of balance exercises on functional assessment of balance in individuals with THA or TKA. The patients had no difficulties performing the balance exercises and they were highly compliant in doing so. Addition of balance exercises in the rehabilitation program for individuals with THA or TKA could improve their balance and subsequently improve their ability to perform balance-related daily physical activities.
Acknowledgments
The authors would like to thank all participants who took part in the study.
Appendix
Appendix 1.
Rehabilitation program (duration: 10 repetitions, 3 times a day).
| Typical exercises for THA | Typical exercises for TKA | Balance exercises for THA and TKA |
|---|---|---|
| 1. Assisted knee flexion with a strap in lying 2. Knee extension on a towel roll in lying 3. Isometric quadriceps in lying 4. Hip abduction in standing with holding a stable support 5. Hip extension in standing with holding a stable support 6. Hip flexion in standing with holding a stable support 7. Knee flexion in standing with holding a stable support |
1. Assisted knee flexion with a strap in lying 2. Knee extension on a towel roll in lying 3. Knee flexion by sliding foot on bed in lying 4. Straight leg raises in lying 5. Assisted knee extension with strap around the foot in lying 6. Knee extension in sitting 7. Knee flexion by sliding foot on the floor in sitting |
1. Rotate trunk clockwise and then in anti-clockwise direction in standing without support 2. Lunge in walk standing position without support and then repeat with the other leg forward 3. Shift weight to one side in a stride standing position without support and then repeat on the other side |
THA: total hip arthroplasty; TKA: total knee arthroplasty.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Ethical approval for the study was obtained from the Research Ethics Board for Health Sciences Research Involving Human Subjects (HSREB), The University of Western Ontario, London, Ontario, Canada. Review no. 12697E.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: All participants provided written consent prior to participation in the study.
Study registration: ClinicalTrials.gov Protocol Registration System; ClinicalTrials.gov ID: NCT01555307; Protocol ID: R-06-461.
References
- 1. Wegener L, Kisner C, Nichols D. Static and dynamic balance responses in persons with bilateral knee osteoarthritis. J Orthop Sports Phys Ther 1997; 25(1): 13–18. [DOI] [PubMed] [Google Scholar]
- 2. Cross MJ, McCloskey DI. Position sense following surgical removal of joints in man. Brain Res 1973; 55(2): 443–445. [DOI] [PubMed] [Google Scholar]
- 3. Barrack RL, Skinner HB, Cook SD, et al. Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol 1983; 50(3): 684–687. [DOI] [PubMed] [Google Scholar]
- 4. Karanjia PN, Ferguson JH. Passive joint position sense after total hip replacement surgery. Ann Neurol 1983; 13(6): 654–657. [DOI] [PubMed] [Google Scholar]
- 5. Wada M, Kawahara H, Shimada S, et al. Joint proprioception before and after total knee arthroplasty. Clin Orthop Relat Res 2002; 403(10): 161–167. [DOI] [PubMed] [Google Scholar]
- 6. Masui T, Hasegawa Y, Yamaguchi J, et al. Increasing postural sway in rural-community-dwelling elderly persons with knee osteoarthritis. J Orthop Sci 2006; 11(4): 353–358. [DOI] [PubMed] [Google Scholar]
- 7. Messier SP, Royer TD, Craven TE, et al. Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis, and Seniors Trial (FAST). J Am Geriatr Soc 2000; 48(2): 131–138. [DOI] [PubMed] [Google Scholar]
- 8. Giemza C, Ostrowska B, Matczak-Giemza M. The effect of physiotherapy training programme on postural stability in men with hip osteoarthritis. Aging Male 2007; 10(2): 67–70. [DOI] [PubMed] [Google Scholar]
- 9. Arokoski JPA, Leinonen V, Arokoski MH, et al. Postural control in male patients with hip osteoarthritis. Gait Posture 2006; 23(1): 45–50. [DOI] [PubMed] [Google Scholar]
- 10. Furnes O, Lie SA, Espehaug B, et al. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Joint Surg Br 2001; 83(4): 579–586. [DOI] [PubMed] [Google Scholar]
- 11. Yoshida Y, Mizner RL, Ramsey DK, et al. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech 2008; 23(3): 320–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Trudelle-Jackson E. Balance and postoperative lower extremity joint replacement. Orthop Phys Ther Clin N Am 2002; 11(1): 101–110. [Google Scholar]
- 13. Wykman A, Goldie I. Postural stability after total hip replacement. Int Orthop 1989; 13(4): 235–238. [DOI] [PubMed] [Google Scholar]
- 14. Ellison J, Miller J, Hocate MF, et al. Comparison of Berg Balance Scale scores between rehabilitated patients with total hip arthroplasty and matched healthy subjects. J Outcome Meas 2000; 4(1): 49–54. [Google Scholar]
- 15. Nallegowda M, Singh U, Bhan S, et al. Balance and gait in total hip replacement: a pilot study. Am J Phys Med Rehabil 2003; 82(9): 669–677. [DOI] [PubMed] [Google Scholar]
- 16. Trudelle-Jackson E, Emerson R, Smith S. Outcomes of total hip arthroplasty: a study of patients one year postsurgery. J Orthop Sports Phys Ther 2002; 32(6): 260–267. [DOI] [PubMed] [Google Scholar]
- 17. Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am 2004; 86(2): 328–334. [DOI] [PubMed] [Google Scholar]
- 18. McChesney JW, Woollacott MH. The effect of age-related declines in proprioception and total knee replacement on postural control. J Gerontol A Biol Sci Med Sci 2000; 55(11): M658–M666. [DOI] [PubMed] [Google Scholar]
- 19. Carroll NV, Slattum PW, Cox FM. The cost of falls among the community-dwelling elderly. J Manag Care Pharm 2005; 11(4): 307–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Duncan PW, Chandler J, Studenski S, et al. How do physiological components of balance affect mobility in elderly men? Arch Phys Med Rehabil 1993; 74(12): 1343–1349. [DOI] [PubMed] [Google Scholar]
- 21. Gage WH, Frank JS, Prentice SD, et al. Postural responses following a rotational support surface perturbation, following knee joint replacement: frontal plane rotations. Gait Posture 2008; 27(2): 286–293. [DOI] [PubMed] [Google Scholar]
- 22. Bellamy N, Buchanan WW, Goldsmith H, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumat 1988; 1: 95–108. [PubMed] [Google Scholar]
- 23. Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci 1995; 50: M28–M34. [DOI] [PubMed] [Google Scholar]
- 24. Berg K, Wood-Dauphinee S, Williams JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 1989; 41: 304–311. [Google Scholar]
- 25. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 26. Jogi P, Overend T, Spaulding S, et al. Effectiveness of balance exercises in the acute post-operative phase following total hip and knee arthroplasty: a randomized clinical trial. SAGE Open Med 2015; 3 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee G, Park AE. Development of a more robust tool for postural stability analysis of laparoscopic surgeons. Surg Endosc 2008; 22(4): 1087–1092. [DOI] [PubMed] [Google Scholar]
- 28. Swanenburg J, Bruin ED, Favero K, et al. The reliability of postural balance measures in single and dual tasking in elderly fallers and non fallers. BMC Musculoskelet Disord 2008; 9(1): 162–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. StatSoft Inc. STATISTICA 7.0. Tulsa, OK: StatSoft Inc, 2000. [Google Scholar]
- 30. Seely T. Standing balance before and after total knee arthroplasty: a pilot study. Master’s Thesis, The University of Western Ontario, London, ON, Canada, 2005. [Google Scholar]
- 31. Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil 1989; 70(7): 510–517. [PubMed] [Google Scholar]
- 32. Franklin PD, McLaughlin J, Boisvert CB, et al. Pilot study of methods to document quantity and variation of independent patient exercise and activity after total knee arthroplasty. J Arthroplasty 2006; 21(6 (Suppl. 2)):157–163. [DOI] [PubMed] [Google Scholar]
- 33. Trudelle-Jackson E, Smith SS. Effects of a late-phase exercise program after total hip arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil 2004; 85(7): 1056–1062. [DOI] [PubMed] [Google Scholar]
- 34. Sashika H, Matsuba Y, Watanabe Y. Home program of physical therapy: effect on disabilities of patients with total hip arthroplasty. Arch Phys Med Rehabil 1996; 77(3): 273–277. [DOI] [PubMed] [Google Scholar]
- 35. Kramer JF, Speechley M, Bourne R, et al. Comparison of clinic and home based rehabilitation programs after total knee arthroplasty. Clin Orthop Relat Res 2003; 410(5): 225–234. [DOI] [PubMed] [Google Scholar]
- 36. Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 2nd ed. Upper Saddle River, NJ: Prentice Hall, 2000, p. 181. [Google Scholar]
- 37. Rossi MD, Hasson S. Lower limb force production in individuals after unilateral total knee arthroplasty. Arch Phys Med Rehabil 2004; 85(8): 1279–1284. [DOI] [PubMed] [Google Scholar]
- 38. Berocci GE, Munin MC, Frost KL, et al. Isokinetic performance after total hip replacement. Am J Phys Med Rehabil 2004; 83: 1–9. [DOI] [PubMed] [Google Scholar]