Abstract
Background
Metallic dust is a heterogeneous substance with respiratory sensitizing properties. Its long term exposure adversely affected lung function, thus may cause acute or chronic respiratory diseases.
Methods
A cross-sectional study was conducted in a steel factory in Terengganu, Malaysia to assess the metal dust exposure and its relationship to lung function values among 184 workers. Metal dust concentrations values (Co, Cr, and Ni) for each worker were collected using air personal sampling. Lung function values (FEV1, FVC, and %FEV1/FVC) were determined using spirometer.
Results
Exposure to cobalt and chromium were 1–3 times higher than permissible exposure limit (PEL) while nickel was not exceeding the PEL. Cumulative of chromium was the predictor to all lung function values (FEV1, FVC, and %FEV1/FVC). Frequency of using mask was positively associated with FVC (Adj b = 0.263, P = 0.011) while past respiratory illnesses were negatively associated with %FEV1/FVC (Adj b = –1.452, P = 0.026). Only few workers (36.4%) were found to wear their masks all times during the working hours.
Conclusions
There was an exposure-response relationship of cumulative metal dust exposure with the deterioration of lung function values. Improvement of control measures as well as proper and efficient use or personal protection equipment while at work could help to protect the respiratory health of workers.
Keywords: Metal dust, Lung function, Exposure-response relationship, Cumulative metal dust, Respiratory protection devices
Introduction
Steel workers are occupationally exposed to inhalation of dust particles containing metallic compounds. Long-term exposure to metallic particles may cause impairment of pulmonary surfactant and lung function and result in chronic respiratory diseases.1–3A significant decline in lung function consistent with slight airway obstruction has been reported in individuals working in the continuous casting processes.4 Exposure to dust among steel workers has also been strongly associated with reduction of forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and %FEV1/FVC.5
Several studies have reported the exposure-response relationship between occupational agents and lung function impairment in developing countries.6–9 However, to our knowledge, no studies have reported the association between cumulative metal dust exposures and lung function deterioration. This research fills a gap by studying the concentration of metal dust and estimating the cumulative exposure of respirable metal dust (Co, Cr, and Ni) during the lifetime of steel industry workers using standardized measurements. Contributing factors to lung function, including smoking history and the frequency of protective mask use were also assessed.
Methods
Study population
A cross-sectional study was conducted in a factory employing 1675 workers in Terengganu, Malaysia. Employee information for 472 workers, including job title, age, and factory unit were provided by management. Stratified random sampling based on work unit was used to recruit the study population. Eligibility criteria included male gender, aged 18–56 years, and employed for a minimum of one year at this factory. No females were directly exposed to metal dust occupationally and were therefore excluded. The study protocol was explained to workers and each individual provided written informed consent prior to participation. The study was approved by the Research and Ethics Committee, Universiti Kebangsaan Malaysia (UKM) Medical Center, reference number UKM 1.5.3.5/244/FF-055-2013 (February 2013). The study took place between February and May 2013.
Measures
Information on socio-demographic characteristics, smoking history, and overall health was collected through a pretested questionnaire administrated by the authors.10,11 Height, weight and spirometry tests were measured in-person by the authors. Smoking history is the most common risk factor for lung diseases.12 Therefore, history of smoking was assessed through cigarette equivalent; the number of cigarettes smoked per day and duration of smoking was used to calculate pack-years of smoking for current smokers. A pack-year is defined as the equivalent of smoking 20 cigarettes per day for a year. The following definitions related to smoking were used: Non-smokers had no lifetime history of smoking; ex-smokers had previously smoked but not within the last six months; smokers had smoked within the last six months. Participants were grouped into non-current smokers (non-smokers and ex-smokers) and current smokers. The frequency of mask use during the entire work shift was categorized as often, seldom, and always. All interviews were conducted in Malay language by one author (NAH).
Exposure assessment and trace metal concentration analysis
Metal dust concentrations in work units were measured using Gil Air personal sampling pumps. The pumps were charged for 24 h and calibrated on site with a membrane filter (0.8 μm pore size, 37 mm diameter, mixed cellulose ester) prior to sampling. The personal sampling pumps equipped with a cyclone filter head were loaded with a membrane filter and attached to the waist belt of workers during their shift. The sampling procedures were performed according to the occupational exposure sampling strategy manual “Method for Exposure Monitoring” by the US National Institute for Occupational Safety and Health (NIOSH).13 The number of workers and valid samples in different work units are presented in Table 1.
Table 1.
Concentration and cumulative respirable metal dust exposure by different work unit
| Work unit | No of workers | No of samples | Time Weight Average (mg/m3) 8-h TWA |
Cumulative respirable metal dust exposure (mg/m3 × year) |
||||
|---|---|---|---|---|---|---|---|---|
| Total number | 472 | 192 | ||||||
| Metal dust | Co | Cr(VI) | Ni | Co | Cr(VI) | Ni | ||
| USECHH PEL (mg/m3) | 0.1 | 0.05 | 1.5 | Mean | ||||
| Furnace | ||||||||
| Supervisor & Foreman | 3 | 1 | 0.15 | 0.11 | 0.60 | 3.88 | 2.90 | 7.19 |
| Electric Arc Furnace controller | 3 | 1 | 0.09 | 0.10 | 0.05 | 1.23 | 1.39 | 4.33 |
| Melter | 18 | 10 | 0.15 | 0.15 | 0.66 | 11.84 | 3.47 | 11.46 |
| Ladle furnace | ||||||||
| Supervisor | 2 | 1 | 0.04 | 0.13 | 0.15 | 0.43 | 0.70 | 4.00 |
| Controlling room operator | 3 | 1 | 0.03 | 0.14 | 0.07 | 0.05 | 0.27 | 1.26 |
| Melter | 8 | 6 | 0.10 | 0.14 | 0.18 | 6.94 | 2.30 | 12.91 |
| Ladle handling | 0.04 | |||||||
| Supervisor | 2 | 1 | 0.10 | 0.02 | 0.49 | 4.80 | 0.41 | 8.64 |
| Controlling room operator | 3 | 1 | 0.11 | 0.08 | 0.07 | 0.85 | 0.47 | 1.58 |
| Ladleman | 8 | 6 | 0.15 | 0.12 | 0.63 | 5.26 | 1.63 | 9.11 |
| Continuous casting machine (MC-5) | ||||||||
| Supervisor & Foremen In charge | 6 | 2 | 0.12 | 0.02 | 0.49 | 4.80 | 0.41 | 8.64 |
| Controlling room operator | 3 | 1 | 0.11 | 0.08 | 0.07 | 0.85 | 0.47 | 1.58 |
| Caster | 30 | 11 | 0.19 | 0.12 | 0.63 | 5.26 | 1.63 | 9.11 |
| Continuous casting machine-Concast | ||||||||
| Supervisor & Foremen In Charge | 6 | 2 | 0.12 | 0.14 | 0.60 | 2.91 | 1.28 | 5.38 |
| Controlling room operator | 3 | 1 | 0.10 | 0.07 | 0.05 | 0.54 | 0.87 | 2.82 |
| Caster | 30 | 11 | 0.16 | 0.16 | 0.64 | 3.88 | 3.48 | 16.64 |
| Scrap bay | ||||||||
| Supervisor | 6 | 2 | 0.10 | 0.11 | 0.55 | 3.82 | 2.05 | 10.4 |
| Heavy equipment driver | 30 | 11 | 0.14 | 0.15 | 0.60 | 4.83 | 2.20 | 12.19 |
| Crane operation | ||||||||
| Supervisor | 6 | 2 | ND | 0.01 | 0.10 | 0 | 1.44 | 0.58 |
| Crane operator | 30 | 11 | ND | 0.02 | 0.10 | 0 | 1.88 | 1.12 |
| DR shed | ||||||||
| Supervisor | 6 | 1 | 0.13 | 0.12 | 0.09 | 0.72 | 0.33 | 0.19 |
| Material handling technician | 30 | 11 | 0.15 | 0.15 | 0.17 | 0.88 | 0.60 | 0.22 |
| DR Cleaning | ||||||||
| Supervisor | 3 | 1 | 0.15 | 0.11 | 0.05 | 1.80 | 0.94 | 0.26 |
| DR technician | 32 | 11 | 0.16 | 0.13 | 0.17 | 4.29 | 1.40 | 0.50 |
| Product handler | 32 | 11 | 0.17 | 0.13 | 0.17 | 10.27 | 1.85 | 0.76 |
| DR operation | ||||||||
| Supervisor | 3 | 1 | 0.10 | 0.09 | 0.13 | 2.29 | 1.96 | 0.56 |
| DR man | 32 | 11 | 0.14 | 0.11 | 0.14 | 4.12 | 3.15 | 0.58 |
| Fabrication | ||||||||
| Supervisor | 3 | 1 | 0.10 | 0.11 | 0.24 | 0.25 | 0.80 | 0.63 |
| Fabricator | 8 | 6 | 0.12 | 0.13 | 0.54 | 1.78 | 1.59 | 0.46 |
| Welder | 8 | 6 | 0.14 | 0.19 | 0.67 | 1.40 | 3.07 | 2.74 |
| Refractory | ||||||||
| Supervisor | 3 | 1 | 0.02 | 0.15 | 0.02 | 0.24 | 2.99 | 0.70 |
| Refractory man | 8 | 6 | 0.04 | 0.16 | 0.08 | 0.48 | 5.43 | 1.70 |
| Raw material handling | ||||||||
| Supervisor | 3 | 1 | 0.12 | 0.10 | 0.45 | 1.31 | 1.98 | 7.13 |
| Raw material handler | 10 | 7 | 0.15 | 0.14 | 0.60 | 2.79 | 2.00 | 7.43 |
| Upstream conveyor | ||||||||
| Supervisor | 3 | 1 | 0.10 | 0.10 | 0.15 | 2.17 | 1.08 | 7.13 |
| Conveyor man | 11 | 7 | 0.14 | 0.16 | 0.18 | 3.71 | 2.33 | 7.43 |
| Machining & mechanical | ||||||||
| Supervisor | 3 | 1 | 0.03 | 0.03 | ND | 0.05 | 0.15 | 0 |
| Mechanics | 8 | 6 | 0.05 | 0.05 | ND | 0.14 | 0.19 | 0 |
| Electrical & Instrumentation | ||||||||
| Supervisor & engineers | 3 | 1 | 0.01 | 0.03 | 0.11 | 0.08 | 0.10 | 0.18 |
| Instrument technician | 8 | 6 | 0.02 | 0.04 | 0.12 | 0.16 | 0.18 | 0.38 |
| Electrician | 8 | 6 | 0.02 | 0.06 | 0.09 | 0.15 | 0.16 | 0.35 |
| Logistics/workshop | ||||||||
| Mechanics | 11 | 7 | ND | ND | ND | 0 | 0 | 0 |
Abbreviation: PEL – Permissible Exposure Limit; ND – Not detected.
The exposure assessment collected 192 samples, representative of an eight-hour shift. Five samples were excluded from the analysis because of abnormal work routine, and three samples were excluded as a result of technical problems (substantially decreased flow rate). As a result, 184 valid samples were included in the final analysis. Steelworkers with samplers were provided instruction in wearing the samplers and how to record relevant information or observations, e.g. production halt, ventilation system not operating, or use of Personal Protective Equipment (PPE). Sample measurements represent eight-hour time-weighted averages (8-h TWA).14
A flow rate of 2.0 L per minute was maintained during air sampling. After fixing the filter papers in the sampling cassette (collecting device), personal samplers were fixed to the waist belt of employees before their shift. Each filter cassette was fixed to ensure the filter head was in the correct position. Samplers were run continuously during work and rest periods for an 8-h shift. At the end of the shift, the personal samplers were switched off. The filter papers were removed and stored in the desiccators. Final weights were recorded from the amount of dust particles settled on the paper and the volume of air sampled. Finally, the calculation for dust particles present in the air and their concentrations were expressed as mg/m3. Dust concentrations were calculated using the following formula:
 |
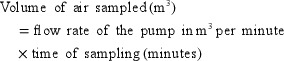 |
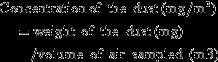 |
The respirable metal particulate samples were subjected to wet mineral acid mixture digestion (9:1 mixture of concentrated analytical grade nitric acid and perchloric acid) on a slow heating hot plate. The acid digested matter was filtered and topped up with quartz double distilled water until 10 mL of solution was obtained. Precautions were taken to prevent extraneous contamination by usage of thoroughly cleaned Borosil glassware. The end analysis for trace metal concentration was performed by atomic absorption spectrophotometer. All procedure analyses were performed according to NIOSH manual analytical methods for selected trace metals.15 Respirable metal dust concentrations were calculated by work unit.
Measurement of lung function
Lung function was measured with a standard spirometer (Spirolab II-MIR model) according to American Thoracic Society criteria.16 The spirometer was calibrated on site as recommended by the manufacturer with a one liter calibration syringe before and after use every day. The procedure for lung function tests was explained to each subject who was then given a practice test while standing. If blowing into the spirometer was satisfactory, the actual test was performed immediately. If the test was properly performed on the first attempt, then three reproducible tracings were obtained. Otherwise the subject was asked to repeat the whole test. A test record was recorded on paper and the American Thoracic Society best results were printed. Twelve subjects (6.25%) were excluded because of lack of reproducibility consistent with the American Thoracic Society guidelines.16 The routine lung function profile included FEV1, FVC, and FEV1/FVC.
Statistical analysis
Data were analyzed using Statistical Packages for Social Science Version 21 and Origin Version 6.1. Exposure-response relationships were examined for deterioration of lung function over the cumulative respirable metal dust exposure. The cumulative respirable metal dust exposure (Co, Cr, and Ni) for each worker according to the duration of employment and total of metal dust concentrations during working hours was calculated using the formula:
According to this equation and occupational history, the cumulative respirable metal dust (Co, Cr, and Ni) for each subject could be hypothetically estimated to investigate the exposure-response relationship with lung function values. The exposure relationship between lung function and cumulative metal dusts was calculated using linear regression.
Multiple linear regression analysis was applied to identify the factors associated with lung function values. The outcome variables analyzed were FEV1, FVC, and %FEV1/FVC. The exposure variables were cumulative respirable metal dust for Co, Cr, and Ni. The confounding variables were age, height, cigarette equivalent, past dusty occupations, past respiratory illnesses, and frequency of wearing mask. Ethnicity as a confounder did not contribute to the models of lung function as all subjects were Malay. Objective metal dust exposure indicators (respirable metal dust) and cigarette equivalent were not normally distributed and therefore transformed logarithmically to yield lognormal distributions before analysis. The significance level was P < 0.05.
Results
Background of the subjects
A hundred and eighty-four male Malay workers were included in the analysis. The mean age of participants was 36.7 ± 8.36 years (mean ± standard deviation) and mean duration of employment was 11.2 ± 7.76 years. Fifty-eight percent of the workers were current smokers and 75.5% had smoked cigarettes for more than 10 years. Mean cigarette equivalent was 10.7 ± 9.62 packs per year. Prior to joining this company, 3.8% had been exposed to occupational dusty environments and 8.5% had a history of respiratory diseases. Only 35.8% of workers wore masks “full time” during the working hours.
Metal dust exposure assessment
Personal sampling results showed the 8-h TWA concentration for cobalt and chromium exceeded the occupational exposure limit set by the Use and Standard Exposure to Chemical Hazardous to Health (USECHH) Occupational Safety and Health Act (OSHA) 1994, while the 8-h TWA concentration of nickel did not exceed the set value.17 The highest mean concentration for cobalt was found in caster (0.19 mg/m3), while the highest mean concentration for chromium and nickel was found in welder (0.19 and 0.67 mg/m3, respectively). The highest cumulative respirable exposure for cobalt (mg/m3 × year) was found in melter (11.84 mg/m3 × year) while the highest cumulative respirable of chromium and nickel were found in refractory workers (5.43 mg/m3 × year) and caster workers (16.64 mg/m3 × year), respectively (Table 1).
Practice
Respiratory protection devices (N95 particulate respirator) and masks were available to all workers. Sixty-seven (36.4%) workers used masks “full time” during the working hours, 88 workers (47.8%) used masks “most of the time”, and 29 workers (15.8%) “seldom” used masks. From the observation and walk-through survey, few workers used “traditional methods” to protect themselves from the dust by using ordinary cloth, handkerchief, and T-shirt.
Lung function
Lung function values were grouped according to cumulative respirable metal dust exposure for the lifetime working (mg/m3 × year) as shown in Table 2. Their mean values of FEV1, FVC, and %FEV1/FVC were 2.88 ± 0.44 L, 3.41 ± 0.50 L, and 84.49 ± 5.47 L, respectively. The three values gradually decreased among the groups defined by cumulative respirable metal dust exposure.
Table 2.
Comparison of lung function by different cumulative respirable metal dust exposure categories
| Cumulative respirable metal dust (Co) mg/m3x year |
|||||||
|---|---|---|---|---|---|---|---|
| General info | F Statistic (df) | P-value | Total | ||||
| <0.50 | 0.50–0.99 | 1.00–1.99 | 2.0++ | ||||
| Total | 55 | 25 | 33 | 71 | 184 | ||
| Lung function valuesa | |||||||
| FEV1* | 2.98 ± 0.46 | 2.97 ± 0.38 | 2.93 ± 0.48 | 2.76 ± 0.41 | 3.188 (3.180) | 0.025 b | 2.88 ± 0.44 |
| FVC* | 3.55 ± 0.49 | 3.49 ± 0.57 | 3.47 ± 0.45 | 3.27 ± 0.44 | 3.304 (3.180) | 0.022 b | 3.41 ± 0.50 |
| FEV1/FVC (%) | 85.66 ± 3.95 | 84.30 ± 5.31 | 84.24 ± 5.96 | 84.08 ± 6.52 | 0.611 (3.180) | 0.609 | 84.49 ± 5.47 |
| Cumulative respirable metal dust (Cr) mg/m3x year | F Statistic (df) | P-value | |||||
| Total | 33 | 41 | 48 | 62 | 184 | ||
| Lung function valuesa | |||||||
| FEV1# | 3.06 ± 0.38 | 3.02 ± 0.41 | 2.79 ± 0.40 | 2.75 ± 0.47 | 6.237 (3.180) | <0.001c | 2.88 ± 0.44 |
| FVC # | 3.64 ± 0.46 | 3.52 ± 0.45 | 3.31 ± 0.54 | 3.29 ± 0.45 | 5.928 (3.180) | 0.002d | 3.41 ± 0.50 |
| FEV1/FVC (%) | 85.82 ± 4.62 | 84.90 ± 4.55 | 84.58 ± 7.54 | 83.26 ± 5.21 | 1.986 (3.180) | 0.118 | 84.49 ± 5.47 |
| Cumulative respirable metal dust (Ni) mg/m3x year | F Statistic (df) | P-value | |||||
| Total | 42 | 19 | 16 | 107 | 184 | ||
| Lung function valuesa | |||||||
| FEV1 | 2.91 ± 0.42 | 2.90 ± 0.45 | 2.89 ± 0.45 | 2.76 ± 0.51 | 0.539 (3.180) | 0.656 | 2.88 ± 0.44 |
| FVC | 3.51 ± 0.51 | 3.43 ± 0.48 | 3.41 ± 0.52 | 3.22 ± 0.54 | 1.156 (3.180) | 0.328 | 3.41 ± 0.50 |
| FEV1/FVC (%) | 85.55 ± 5.60 | 84.61 ± 5.82 | 84.46 ± 5.22 | 83.13 ± 6.21 | 0.572 (3.180) | 0.634 | 84.49 ± 5.47 |
values in mean ± standard deviation.
Significance at: *P < 0.05, **P < 0.01, #P < 0.001.
Post hoc analysis: No significant difference in mean of FEV1 and FVC values among cumulative exposure of cobalt in each pair.
Post hoc analysis: Significant difference in mean of FEV1 among cumulative exposure of chromium <0.50 mg/m3 × year and 1.00–1.99 mg/m3 × year (P = 0.041),between cumulative of chromium <0.50 mg/m3 × year and >2.00 mg/m3 × year (P = 0.009), and between cumulative of chromium 0.50–0.99 mg/m3 × year and >2.00 mg/m3 × year (P = 0.023).
Post hoc analysis: Significant difference in mean of FVC was among cumulative exposure of chromium <0.50 mg/m3 × year and 1.00–1.99 mg/m3 × year (P = 0.016), and between the cumulative chromium <0.50 mg/m3 × year and >2.00 mg/m3 × year (P = 0.018) but no difference in the other pairs.
There was a mean difference of FEV1 and FVC among the cumulative exposure of cobalt with P = 0.025 and P = 0.022, respectively. Similarly, the mean difference of FEV1 and FVC among cumulative exposure of chromium was P < 0.001 and P = 0.002, respectively. However, post hoc analysis revealed that the mean of FEV1 and FVC among the cumulative exposure of cobalt was not different for each pair.
There was a significant difference in FEV1 between cumulative exposure to chromium groups (P < 0.001). The mean FEV1 of cumulative exposure to chromium group <50 mg/m3 × year was higher than the mean FEV1 of the cumulative of chromium exposure group 1.00–1.99 mg/m3 × year and cumulative exposure to chromium group >2.00 mg/m3 × year. The mean FEV1 of cumulative exposure to chromium group 0.50–0.99 mg/m3 × year was also higher than the mean FEV1 of respondents in the cumulative exposure to chromium group >2.00 mg/m3 × year.
There was also a significant difference between FVC and cumulative exposure to chromium group (P = 0.002). The mean FVC of cumulative exposure to chromium group <0.50 mg/m3 × year was higher than the mean FEV1 cumulative exposure to chromium group 1.00–1.99 mg/m3 × year. The mean FVC of cumulative exposure to chromium group <0.50 mg/m3 × years was also higher than the mean FVC in the group of cumulative exposure to chromium >2.00 mg/m3 × year.
Exposure-response relationship
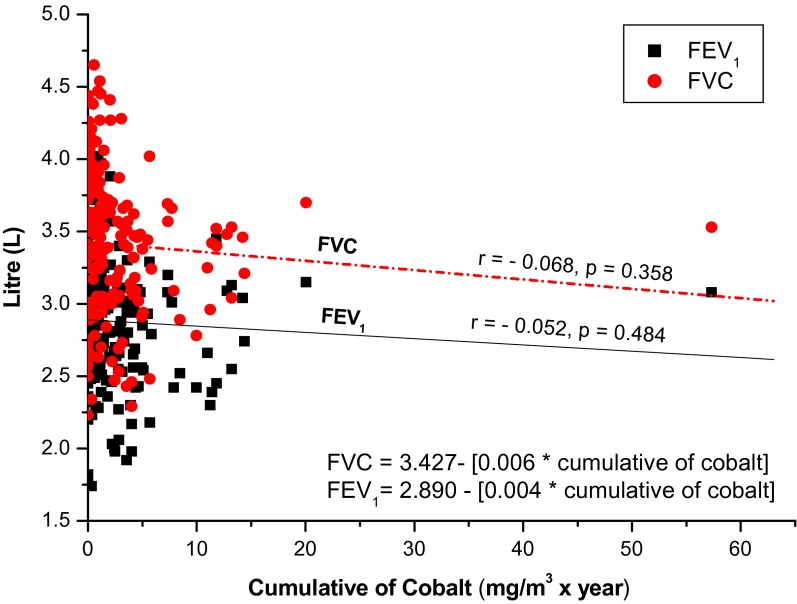
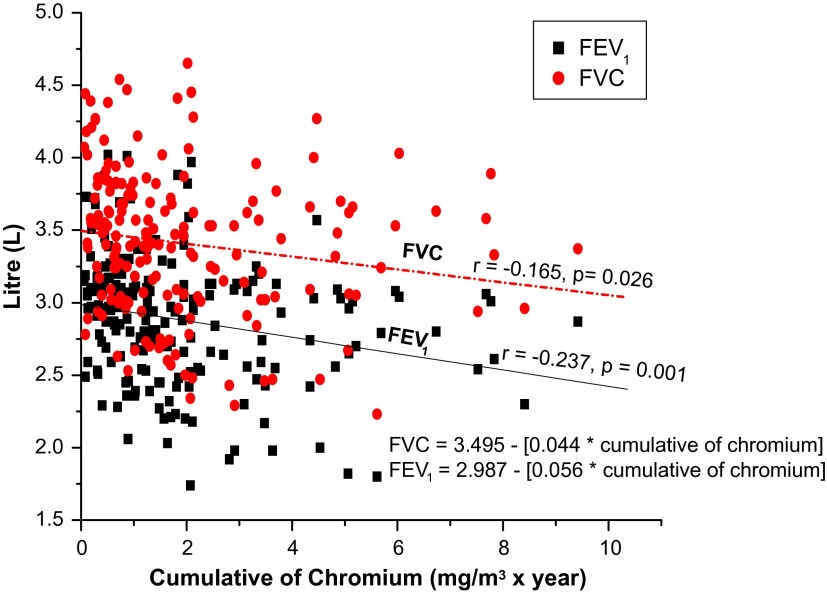
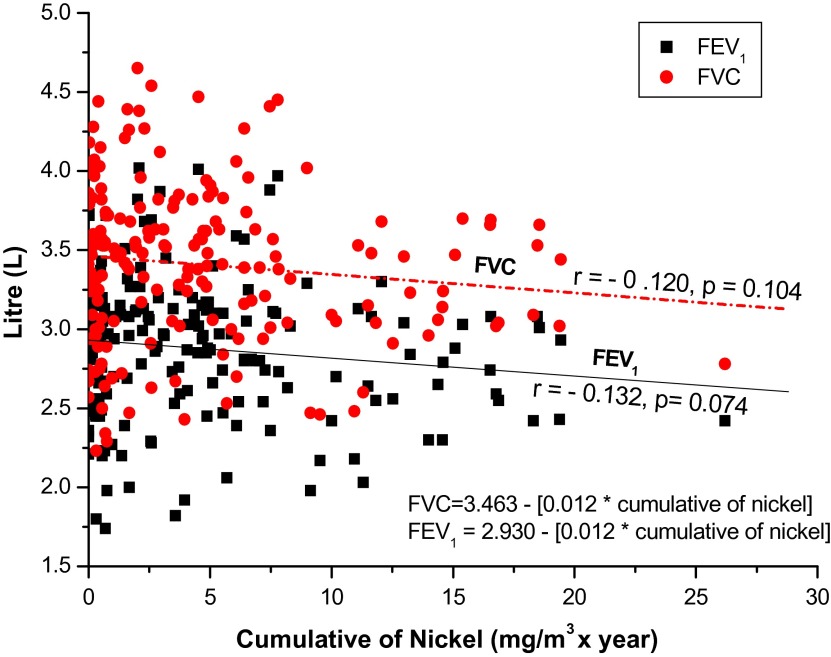
The exposure-response relationship for each cumulative respirable metal dust (Co, Cr, and Ni) and lung function deterioration was explored with linear regression. The lung function indices (FEV1, FVC, %FEV1/FVC) gradually decreased by cumulative respirable metal dust exposure (Figs. 1–3). There was a significant relationship of cumulative chromium exposure with FEV1 (r = –0.2307, P = 0.001) and FVC (r = –0.165, P = 0.026). In contrast, there was no significant relationship between cumulative of cobalt and nickel exposure with FEV1 and FVC (P > 0.05). There was a significant relationship between %FEV1/FVC and cumulative cobalt exposure (r = –0.204, P = 0.006) and cumulative chromium exposure (r = –0.204, P = 0.005). There was no significant relationship between cumulative chromium and nickel exposure with %FEV1/FVC (P > 0.05).
Figure 1.
Relationship between Cumulative Cobalt with FVC and FEV1
Figure 2.
Relationship between Cumulative Chromium with FVC and FEV1
Figure 3.
Relationship between Cumulative Nickel with FVC and FEV1
Contributing factors to lung function
Multiple linear regression analysis of contributing factors is presented in Table 3. As expected, age, height, and weight predicted lung function values. Cumulative chromium exposure was significantly associated with FEV1 (b = –0.249, P = 0.024), FVC (b = –0.260, P = 0.014), and %FEV1/FVC (b = –5.737, P < 0.001). The frequency of using a personal protective mask was positively associated with FVC (b = 0.263, P = 0.011), while past respiratory illnesses was negatively associated with %FEV1/FVC (b = –1.452, P = 0.026). In contrast, no association was found between past exposure to dusty occupations with lung function values (P > 0.05).
Table 3.
Predictors of lung function values in simple and multiple linear regression
| SLRa |
MLRb |
|||||
|---|---|---|---|---|---|---|
| Predictors | b (95% CI) | P value | Adj b (95% CI) | t-stat | P value | |
| FEV1 (L) | ||||||
| Constant | – | – | 2.992 (2.735, 3.248) | 23.148 | <0.001** | |
| Age (year) | −0.027 (–0.034, −0.021) | <0.001 | −0.031 (–0.044,–0.019) | −4.967 | <0.001** | |
| Height (cm) | 0.041 (0.032, 0.050) | <0.001 | 0.032 (0.020, 0.045) | 5.145 | <0.001** | |
| Weight (kg) | −0.002 (–0.007, −0.004) | 0.553 | −0.004 (–0.009, 0.001) | −1.484 | 0.141 | |
| Cumulative of Co (mg/m3 × year)c | −0.176 (–0.304, −0.0407) | 0.008* | −0.002 (–0.200, 0.195) | −0.024 | 0.981 | |
| Cumulative of Cr (mg/m3 × year)c | −0.284 (–0.420, −0.148) | <0.001** | −0.249 (–0.464, −0.034) | −2.296 | 0.024* | |
| Cumulative of Ni (mg/m3 × year)c | −0.062 (–0.162, 0.038) | 0.225 | −0.070 (–0.202, 0.062) | −1.056 | 0.294 | |
| Cigarette equivalent (packs/year)c | −0.303 (–0.488, −0.118) | 0.002* | −0.166 (–0.371,0.039) | −1.606 | 0.112 | |
| Past dusty occupations (Yes) | −0.247 (–0.608, 0.113) | 0.177 | −0.255 (–0.678.0.168) | −1.196 | 0.234 | |
| Past respiratory illnesses (Yes) | −0.039 (–0.290,0.212) | 0.760 | −0.025 (–0.251, 0.201) | −0.219 | 0.827 | |
| Frequency of using mask (Yes) | 0.165 (–0.009, 0.340) | 0.063 | 0.107 (0.110, 0.325) | 0.977 | 0.331 | |
| R2 | 0.491 | |||||
| FVC (L) | ||||||
| Constant | – | – | 3.409 (2.148, 5.162) | 4.558 | <0.001** | |
| Age (year) | −0.026 (–0.034, −0.019) | <0.001** | −0.024 (–0.038, –0.010) | −3.421 | 0.001* | |
| Height (cm) | 0.048 (0.038, 0.058) | < 0.001** | 0.042 (0.028.0.056) | 5.969 | <0.001** | |
| Weight (kg) | −0.001 (–0.007, 0.005) | 0.696 | −0.037 (–0.013, −0.001) | −2.174 | 0.032* | |
| Cumulative of Co (mg/m3 × year)c | 0.288 (–0.443, −0.132) | <0.001* | −0.195 (–0.433, 0.044) | −1.621 | 0.108 | |
| Cumulative of Cr (mg/m3 × year)c | −0.268 (–0.411, −0.125) | <0.001* | −0.260 (–0.478, −0.041) | −2.354 | 0.014* | |
| Cumulative of Ni (mg/m3 × year)c | −0.056 (–0.170, 0.057) | 0.330 | −0.028 (–0.175, 0.118) | −0.385 | 0.701 | |
| Cigarette equivalent (packs/year)c | −0.312 (–0.525, −0.100) | 0.004* | −0.146 (–0.373, 0.082) | −1.269 | 0.207 | |
| Past dusty occupations (Yes) | −0.218 (–0.626, 0.191) | 0.294 | −0.009 (–0.478, 0.461) | −0.036 | 0.971 | |
| Past respiratory illnesses (Yes) | −0.210 (–0.305, 0.263) | 0.885 | −0.125(–0.430, 0.180) | −0.815 | 0.417 | |
| Frequency of using mask (Yes) | 0.184 (–0.014,0.382) | 0.068 | 0.263 (0.062, 0.454) | 2.600 | 0.011* | |
| R2 | 0.500 | |||||
| FEV1/FVC (%) | ||||||
| Constant | – | – | 106.87 (74.49, 139.25) | 6.553 | <0.001** | |
| Age (year) | –0.156 (–0.249, −0.063) | <0.001** | −0.316 (–0.516, −0.116) | −3.316 | 0.002* | |
| Height (cm) | 0.027 (–0.106, 0.160) | 0.688 | −0.081 (–0.281, 0.119) | −0.801 | 0.425 | |
| Weight (kg) | −0.018 (–0.082, 0.046) | 0.578 | −0.045 (–0.132, 0.042) | −1.021 | 0.310 | |
| Cumulative of Co (mg/m3 × year)c | −1.571 (–3.324, 0.182) | 0.079 | −0.638 (–3.925, 2.649) | −0.385 | 0.701 | |
| Cumulative of Cr (mg/m3 × year)c | −1.169 (–1.890, −0.448) | 0.155 | −5.737 (–8.314, −3.160) | −4.420 | <0.001** | |
| Cumulative of Ni (mg/m3 × year)c | −0.565 (–1.812, 0.681) | 0.372 | −1.111 (–2.859, 0.638) | −1.261 | 0.210 | |
| Cigarette equivalent (packs/year)c | −1.150 (–3.777, 1.477) | 0.387 | −1.311 (–4.331, 1.709) | −0.862 | 0.391 | |
| Past dusty occupations (Yes) | −1.395 (–4.501,1.711 | 0.377 | −1.683 (–5.307, 1.942) | −0.922 | 0.359 | |
| Past respiratory illnesses (Yes) | −1.947 (–6.429, 2.535) | 0.393 | −1.452 (–7.070, 4.166) | −2.259 | 0.026* | |
| Frequency of using mask (Yes) | 0.186 (–2.003, 2.375 | 0.867 | 2.034 (–0.825, 4.892) | 1.412 | 0.161 | |
| R2 | 0.288 | |||||
SLR – Simple linear regression, MLR – Multiple linear regression.
Crude regression coefficients, .
bAdjusted regression coefficients.
Logarithm transformation before analysis, *P < 0.05, **P < 0.01, #P < 0.001.
Significance at P or below than 0.05, **Significance at P or below than 0.001.
The model fits reasonably well. Model assumptions are met. There are no interaction between independent variables and no multicollinearity problem.
Model of lung function among steel workers.
FEV1 (L) = 2.992 – [0.031 *age] + [0.032 *height] – [0.249 *log cumulative of chromium].
FVC (L) = 3.409 – [0.024 *age] + [0.042 *height] – [0.037 *weight] – [0.260 *log cumulative of chromium] + [0.263 *frequency of using mask].
FEV1/FVC (%) = 106.87 – [0.316 *age] – [5.737 *log cumulative of chromium] – [1.452 *past respiratory illnesses.
Discussion
We found that the concentrations of cobalt and chromium in workers from areas of high occupational exposure (furnace, casting, raw material, and fabrication areas) were one to three times higher than the Permissible Exposure Limit (PEL).17 However, the 8-h TWA concentrations of nickel did not exceed the PEL. The concentration of metal dust reported was lower compared to studies in other developing countries, likely explained by newer technology and effective control measures adopted in this factory.18,19
The variation in metal dust concentrations depended on the origins and level of ventilation. Metal dust concentrations were higher in furnace, casting, and fabrication areas, where most pollutants were generated. Particles formed when molten metal solidified in the air due to the temperature gradient outside the furnace. Without appropriate protective equipment, particles are easily inhaled, reach the alveoli, and damage respiratory function. This study found that the frequency of mask usage had a positive and significant relationship with FVC. PPE compliance can minimize health hazards, increase productivity, and ultimately life expectancy.20,21
Overall, full-time mask use was low among exposed workers. We observed workers using traditional methods of personal protection including wrapping towels, handkerchiefs, and/or T-shirts around their face to protect themselves from dust. This is an area that should be targeted for improvement.22 Temperature, cost of PPE, inappropriate PPE, and inadequate supervision and enforcement influenced the use of PPE.22,23 Some workers were reluctant to wear PPE due to poor fitting and hot weather.24
FEV1 and FVC are used to characterize the decline of lung function.25 Asthma, chronic bronchitis, and emphysema are different expressions of a single disease. These diseases develop allergy and hyper responsiveness influenced by age, gender, and other external factors.26 Long-term exposure to fumes, chemical substances, and dust in the workplace are known risk factors for the development of COPD.27
Occupational exposures are significantly associated with several respiratory diseases such as bronchial asthma and COPD.25,28,29 Several epidemiological studies found an association between dust, fumes, and gases with chronic bronchitis and airflow obstruction.30–33 However, the role of occupational exposure to airflow obstruction is still controversial. Smoking and occupational factors were determined by amount of cigarette smoked and duration of exposure.
The duration of exposure to dust-exposed occupations is important in assessing the effects of occupational exposure to lung function deterioration. Cumulative exposure to metal dust and duration of employment (job-specific) was associated with a steeper decline in FEV1.34,35 However, selection bias is more common in workforce-based studies due to the healthy worker effect (HWE).36
Cumulative respirable metal dust exposure (mg/m3 × year) was used as a surrogate for metal dust exposure for each worker. Personal metal dust monitoring was available for individuals workers, thus cumulative exposure for an individual was calculated according to their tasks and locations. This study demonstrated an exposure-response relationship of cumulative cobalt and chromium for the lifetime working period (mg/m3 × year) with deterioration of lung function values. A weak correlation (R = 20–24%) was found between cumulative cobalt with lung function values. Multiple linear regressions showed a clear dose response effect between cumulative chromium, thus becoming the predictors to the lung function values.
These findings were consistent with studies among other working populations. A significant decline in FEV1 (in relation to years of exposure of respirable dust) has been reported among tunnel workers28 and hard metals workers.37 Furthermore, acceleration of FVC was also found among gold miners 38 and asbestos workers.39 Iron oxide and silica contained in respirable dust could deteriorate lung function. However, this study did not analyze both the components. Neither haemosiderosis nor silicosis cases have been identified by occupational health doctor through annual chest X-ray examinations. Wide range of duration of employment would give a significant finding of lung function impairment among workers. Past respiratory illnesses also increased the deterioration of lung function, where an association was found with %FEV1/FVC. One out of five cases of chronic obstructive pulmonary diseases (COPD) may be attributable to occupational exposures.27 Therefore, physicians and health policy-makers should address this potential causes and consequences of COPD as well as introducing an ambient air safety protection at the workplace.
Effect of smoking is prominent among workers occupationally exposed to respiratory irritants especially to chemicals hazardous to health. Previous studies have shown the interaction between smoking and occupational exposures.30,40,41 Smokers who are exposed to occupational exposure had a higher risk to occupational respiratory diseases explained by interactions between irritant gases and particles exposure either through addition or multiplication for the development of chronic bronchitis, emphysema and/or airflow obstruction.
Study limitations
A limitation of the study is that current measurements were used as a proxy for cumulative metal dust concentrations for individual workers over their lifetime. Estimated cumulative exposure to metal dust per employee was calculated based on the exposure per day and the duration of work (mg/m3 × year). Bias calculation of cumulative exposure may have occurred due to the working period and dust exposures. Those exposed to high concentrations of metal dust in short period and those with low exposures for longer period will result in an over or underestimation of cumulative exposure, respectively. In addition, the effect of cumulative metal dust exposure of individual cannot be well established with the health outcomes. There might be inaccuracy in the interpretation of cumulative exposure due to technological or change in the work process during the last several decades.
The other potential limitation would be the selection of mechanism, such as HWE and selective survival. This would typically result in underestimation of the association between exposure and respiratory health effects. Confounding from previous job exposures prior to joining this factory was not fully considered. Another limitation of the study was the homogenous population.
Potential recall bias among subjects is common in population-based study.42 The result of health surveillance (chest X-ray and previous lung function) as well as medical records was not readily available for confirmation of self-reported data. Smoking was not found to further exacerbate the lung function among steel workers. This might be due to the low intensity of smoking and no differences between current smokers and ex-smokers in estimating pack-years. Moreover, the confounder was still retained by the existence of zero value for smoking index among ex-smokers. Therefore, the interaction between smoking and occupational exposure cannot be seen. Separate analysis according to smoking group, as well as excluding ex-smokers in statistical analysis might enhance the valid contrast and show a clear difference of the factors studied.43–46
Conclusion
This study revealed an exposure-response relationship between cumulative respirable metal dust exposures with deterioration of lung function among steel workers. Cumulative chromium was found to be a predictor of lung function values. The frequency of using mask had a positive relationship with the lung function values. Regular hygiene monitoring and improving safety practices as well as compliance of PPE are needed to improve the health and well-being of the workers.
Funding
This study was funded by UKM Medical Centre (UKM) with research (grant number FF-55-2013).
Acknowledgments
We are grateful for the assistance in air sampling and laboratory work provided by the National Institute of Occupational Safety and Health (NIOSH) Malaysia. Thanks to the workers who participated in this study for their willingness to contribute to research that will ultimately improve environmental and occupational health in the steel industry. Finally, special thanks to Dr. Mohd Firdaus Yhaya from School of Industrial Technology, Universiti Sains Malaysia for his assistance with this manuscript.
References
- 1.Gehr P, Sosnowski TR. Particle-lung interactions. New York: Marcel Dekker Inc; 2009. 323 p. [Google Scholar]
- 2.Reudiger HW. Hard metals particles and lung disease: coincidence or causality? Respiration. 2000;67(2):137–8. 10.1159/000029500 [DOI] [PubMed] [Google Scholar]
- 3.Norberg FG, Fowler BA, Norberg M, Friberg LT. Handbook on the toxicology of Metals. New York: Elsevier; 2007. 541 p. [Google Scholar]
- 4.Nemery B, Van Leemputten R, Goemaere E, Veriter C, Brasseur L. Lung function measurements over 21 days shift work in steelworkers from a strand casting department. Brit J Ind Med. 1985;42(9):601–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang ML, McCabe L, Hankinson JL, Shamssain MH, Gunel E, Lapp NL, et al. . Longitudinal and cross sectional analyses of lung function in steelworkers. Am J Resp Crit Care Med. 1996;153(6):1907–13. 10.1164/ajrccm.153.6.8665054 [DOI] [PubMed] [Google Scholar]
- 6.Nurul AH, Shamsul BMT, Noor Hassim I. Respiratory symptoms and pulmonary function among male steel workers in Terengganu, Malaysia. Malaysia J Public Health Med. 2014;14(1):10–8. [Google Scholar]
- 7.Azwan A, Mazlan A, Muhammad Nasir S, Azlihanis AH, Zulfazli H, Rusli N. The relationship of respiratory symptoms and lung function status among workers in steel plants. Malaysian J Comm Health. 2006;12(Supp 1):24. [Google Scholar]
- 8.Abdel-Rasoul GM, Mahrous OAE, Abou Salem ME, Al-Batanony HK, llam HK. Auditory and respiratory health in an iron and steel factory. Zagazig J Occup Health and Safety. 2009;2(1):1–10. [Google Scholar]
- 9.Gomes J, Lloyd OL, Norman NJ, Pahwa P. Dust exposure and impairment of lung function at a small iron foundry in a rapidly developing country. Occup Environ Med. 2001;58(10):656–62. 10.1136/oem.58.10.656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nurul AH, Shamsul Bahri MT, Noor Hassim I. Respiratory symptoms and pulmonary function among male steel workers in Terengganu, Malaysia. Malaysia J Public Health Med. 2014;14(1):10–8. [Google Scholar]
- 11.Nurul AH, Shamsul Bahri MT, Noor Hassim I. Metal dust exposure and respiratory health in male steel workers in Terengganu, Malaysia. Iran J Publ Health. 2014;43(3):153–66. [Google Scholar]
- 12.Jørgen V, Suzanne SH, Alvar GA, Paul WJ, Claus V, Antonio A, et al. . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(4):347–65. [DOI] [PubMed] [Google Scholar]
- 13.National Institute of Occupational Safety and Health [Internet]. Occupational Exposure Sampling Strategy Manual 1977. National Institute of Occupational Safety and Health; [cited 2010 Mar 26]. Avaialble from: www.osha.gov. [Google Scholar]
- 14.Leidel NA, Busch KA, Lynch JR. Occupational exposure sampling strategy manual. Cincinnati (OH): National Institute for Occupational Safety and Health (NIOSH) Publication No. 77-173 (available from the National Technical Information Service (NTIS), Publication No. PB274792; 1977. [Google Scholar]
- 15.National Institute of Occupational Safety and Health NIOSH manual analytical methods. 4th ed. Cincinnati (OH): Department of Health and Human Services (DHHS), Centre for Diseases Control and Prevention, National Institute of Occupational Health; 1994. [Google Scholar]
- 16.American Thoracic Society Standardization of spirometry 1994 update. Am Respir Crit Care Med. 1994;152(3):1107–36. [DOI] [PubMed] [Google Scholar]
- 17.Use of Chemical Hazardous to Health Regulation Occupational Safety and Health Act (Act 154). Malaysia: Ministry of Human Resource; 2000. [Google Scholar]
- 18.Ravichandran B, Krishnamurthy V, Ravibabu K, Raghavan S, Rajan BK, Rajmohan HR. Assessing dust exposure in an integrated iron and steel manufacturing plant in South India. Work. 2008;30(2):195–200. [PubMed] [Google Scholar]
- 19.Clarke EE, Levy LS, Spurgeon A, Calvert IA. The problems associated with pesticide use by irrigation workers in Ghana. Occup Med (London). 1997;47(5):301–8. 10.1093/occmed/47.5.301 [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization Epidemiological of Work-Related Diseases and Accidents. Tech Rep Ser. Geneva: 2009;777:8–10. [PubMed] [Google Scholar]
- 21.Antó JM, Vermeire P, Vestbo J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001;17(5): 982–94. [DOI] [PubMed] [Google Scholar]
- 22.Nurul AH, Shamsul Bahri MT, Noor Hassim I. Metal dust exposure and respiratory health in among steel workers: a dose-response relationship. Int J Collab Res Intern Med Public Health. 2015;7(3):24–39. [Google Scholar]
- 23.Clarke EE, Levy LS, Spurgeon A, Calvert IA. The problems associated with pesticide use by irrigation workers in Ghana. Occup Med (London). 1997;47(5):301–8. 10.1093/occmed/47.5.301 [DOI] [PubMed] [Google Scholar]
- 24.Mekonnen Y, Agonafir T. Pesticide sprayers’ knowledge, attitude and practice use on agricultural farms of Ethiopia. Occup Med (London). 2002;52(6):311–5. 10.1093/occmed/52.6.311 [DOI] [PubMed] [Google Scholar]
- 25.Antó JM, Vermeire P, Vestbo J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001;17(5):982–94. 10.1183/09031936.01.17509820 [DOI] [PubMed] [Google Scholar]
- 26.Becklake MR. Airways disease and occupational exposure to nonfibrogenic dust. Appl Occup Environ Hyg. 1989;13(8):586–92. [Google Scholar]
- 27.Silvana B, Afrim T. Chronic obstructive pulmonary diseases in iron-steel and ferro-chrome Industry. Cent Eur J Publ Heal. 2010;18(2):93–8. [DOI] [PubMed] [Google Scholar]
- 28.Ulvestad B, Bakke B, Eduard W, Kongerud J, Lund MB. Cumulative exposure to dust causes accelerated decline in lung function in tunnel workers. Occup Environ Med. 2002;58(10):663–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Post W, Heederik D, Houba R. Decline in lung function related to exposure and selection processes among workers in the grain processing and animal feed industry. Occup Environ Med. 1998;55(5):349–55. 10.1136/oem.55.5.349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burge PS. Occupation and chronic obstructive pulmonary disease (COPD). Eur Respir J. 1994;7(6):1032–4. [PubMed] [Google Scholar]
- 31.Mastrangelo G, Tartari M, Fedeli U, Fadda E, Saina B. Ascertaining the risk of chronic obstructive pulmonary disease in relation to occupation using a case-control design. Occup Med (London). 2003;53(3):165–72. 10.1093/occmed/kqg041 [DOI] [PubMed] [Google Scholar]
- 32.Trunpin L, Earnest G, San Pedro M, Balmes JR, Eisner MD, Yelin E, et al. . The occupational burden of chronic obstructive pulmonary diseases. Eur Respir J. 2003;22(3):462–9. 10.1183/09031936.03.00094203 [DOI] [PubMed] [Google Scholar]
- 33.Fishwick D, Naylor S. COPD and the workplace. Is it really possible to detect early cases? Occup Med (London). 2007; 57(2):82–4. [DOI] [PubMed] [Google Scholar]
- 34.Balmes J, Becklace M, Blanc P, Henneberger P, Kreiss K, Mapp C, et al. . Occupational contribution to the burden of airway disease. Am J Respir Crit Care Med. 2003;167(5):787–97. [DOI] [PubMed] [Google Scholar]
- 35.Oxman AD, Muir DC, Shannon HS, Stock SR, Hnidzo E, Lange HJ. Occupational dust exposure and chronic obstructive pulmonary disease. A Systemic review of the evidence. Am Rev Respir Dis. 1998;148(1):38–48. [DOI] [PubMed] [Google Scholar]
- 36.Zock JP, Sunyer J, Kogevinas M, Kromhout H, Burney P, Anto JM. Occupation, chronic bronchitis and lung function in young adults. An international study. Am J Respir Crit Care Med. 2001;163(7):1572–7. 10.1164/ajrccm.163.7.2004195 [DOI] [PubMed] [Google Scholar]
- 37.Rehfisch P, Anderson M, Berg P, Lampa E, Nordling Y, Svartengren M, et al. . Lung function and respiratory symptoms in hard metal workers exposed to cobalt. J Occup Environ Med. 2001;54(4):409–13. [DOI] [PubMed] [Google Scholar]
- 38.Ehrlich RI, Myers JE, te Water Naude JM, Thompson ML, Churchyard GJ. Lung function loss in relation to silica dust exposure in South African gold miners. Occup Environ Med. 2011;68(2):96–101. 10.1136/oem.2009.048827 [DOI] [PubMed] [Google Scholar]
- 39.Wang X, Wang M, Qiu H, Yu I, Yano E. Longitudinal changes in pulmonary function of asbestos workers. J Occup Health. 2010;52(5):272–7. 10.1539/joh.L10062 [DOI] [PubMed] [Google Scholar]
- 40.Hendrick DJ. Occupational and chronic obstructive pulmonary disease (COPD). Thorax. 1996;51(9):947–55. 10.1136/thx.51.9.947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kolarzyk E, Stepniewski M, Zapolaska I. Occurrence of pulmonary diseases in steel mill workers. Int J Occup Med Env. 2000;13(2):103–12. [PubMed] [Google Scholar]
- 42.Hamzah NA. Metal dust exposure (cobalt, chromium, and nickel) and respiratory health among male steel workers in Terengganu. [Doctorate Thesis]. Kuala Lumpur: Universiti Kebangsaan Malaysia; 2015. p. 425. [Google Scholar]
- 43.Garshick E, Schenker MB, Dosman JA. Occupationally induced airways obstruction. Med Clin North Am. 1996;80(4):851–78. 10.1016/S0025-7125(05)70470-3 [DOI] [PubMed] [Google Scholar]
- 44.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28(3):523–32. 10.1183/09031936.06.00124605 [DOI] [PubMed] [Google Scholar]
- 45.Chen PC, Doyle PE, Wang JD. Respirable dust exposure and respiratory health in male Taiwanese steelworkers. Ind Health. 2006;44(1):190–9. 10.2486/indhealth.44.190 [DOI] [PubMed] [Google Scholar]
- 46.Nurul AH, Shamsul BMT, Noor Hassim I. Respiratory health of steel workers in the eastern coast of Peninsular Malaysia. Am J App Sci. 2015;12(15):321–8. [Google Scholar]