Abstract
Background
In persistently unsafe environments, the cumulative exposure to violence predicts not only the development of posttraumatic stress disorder (PTSD), but also of increased aggression and violent outbursts. Substance use disorders interact with these developments, as drug consumption may blunt symptoms and also reduce the threshold for violent acts. Investigating the interplay between these variables and the possible cumulative effect of drug abuse on the attraction to cruelty is a crucial step in understanding the cycle of violence and developing intervention programs that address this cycle in violence-troubled communities such as low-income urban areas in South Africa.
Methods
Young males at risk (N = 290) were recruited through a reintegration center for offenders in Cape Town. We assessed types of traumatic events experienced, PTSD symptom severity, appetitive aggression, committed offenses and patterns of drug abuse prior to the perpetration of violence.
Results
Path-analyses confirmed a positive relationship between exposure to traumatic events and PTSD symptom severity, appetitive aggression, the number of committed offenses and drug abuse prior to violence. PTSD symptoms were positively associated with the propensity toward aggression. Furthermore, more severe drug abuse was related to higher attraction to violence and more committed offenses.
Conclusions
We conclude that like exposure to violence, drug abuse may play a key role in the attraction to aggression and criminal acts. Measures of violence prevention and psychotherapeutic interventions for trauma-related suffering may not be effective without enduring drug abuse rehabilitation.
Keywords: Violence perpetration, Substance abuse, Posttraumatic stress disorder, Appetitive aggression, South Africa
Highlights
-
•
Traumatic experiences positively related to posttraumatic stress and drug abuse
-
•
Violence exposure affiliated with more aggressive tendencies and cruel behavior
-
•
Drug abuse prior to violence commission linked to higher attraction to cruelty
-
•
Substance intake before crime perpetration associated with more committed offenses
-
•
Reducing substance abuse may lower high violence levels among young South Africans.
1. Introduction
Male adolescents and young adults living in low-income urban areas of South Africa are exposed to extreme levels of violence and crime. In the Cape Town metropolitan municipality, rates of severe crime are among the highest in the world (Groenewald et al., 2003). Due to the extreme levels of exposure to traumatic stressors (Lockhat & Niekerk, 2000) and involvement in gang violence (Maxson, Whitlock, & Klein, 1998), the boundary between victimization and criminalization in these environments is often blurred. Additionally, South Africa reports one of the highest levels of per-capita alcohol consumption worldwide for individuals drinking alcohol (Rehm et al., 2003); alcohol is the drug most commonly abused by adolescents in the country, followed by illicit drugs such as cannabis, methamphetamine (“tik”) and methaqualone (“mandrax”) (Parry et al., 2004, Ramlagan et al., 2010). The present study investigates the role of drug abuse, i.e. the excessive, socially problematic consumption of intoxicating substances (Doweiko, 2015), in the relationship between victimization and the perpetration of aggressive behavior in a sample of at-risk young males from low-income areas in Cape Town.
Previous research indicates a clear relationship between drug abuse and heightened aggressive behavior. Both alcohol and illegal drugs have been associated with murder, intimate partner violence and child abuse (e.g. Plüddemann et al., 2010, Roizen, 1997, Seedat et al., 2009). This correlation holds true for South Africa: Between 1999 and 2000, in Cape Town, Johannesburg and Durban, almost 50% of individuals arrested on charges related to family violence, homicide or rape were reported to have been either drunk or under the influence of drugs at the time of the offense (Parry, Plüddemann, et al., 2004). The severity of the committed crimes is positively associated with alcohol or drug consumption preceding the violent act (Chermack and Blow, 2002, Hecker and Haer, 2015, White et al., 2002). Although these data reveal that substance abuse represents a frequent precursor to aggressive behavior (Taylor & Chermack, 1993), the question of whether drug abuse functions as a catalyst (Ching, Daffern, & Thomas, 2012) or in a causal role, remains a controversial issue (Klostermann & Fals-Stewart, 2006).
Posttraumatic stress in relation to victimization has been indicated as another important risk factor in the perpetration of violence in low-income urban areas in South Africa (Sommer et al., in press). Symptoms such as hyperarousal, hostility and anger may be viewed as a behavioral pattern to (presumably ongoing) danger, which may lead to aggression (Hellmuth, Stappenbeck, Hoerster, & Jakupcak, 2012). Frequently, trauma survivors attempt to numb these traumatic stress symptoms through self-medication (Bremner, Southwick, Darnell, & Charney, 1996): Alcohol problems and drug abuse often co-occur with PTSD (e.g. Mathews et al., 2009, Stewart, 1996). The comorbidity between drug dependence and PTSD exacerbates aggressive tendencies and is associated with higher levels of perpetrated violence than either drug dependence or PTSD alone (Parrot, Drobes, Saladin, Coffey, & Dansky, 2003).
Aggressive behavior can be driven by the desire to defend oneself against a threat or to take revenge against those responsible for a trauma. This type of reactive aggression is often reported by individuals suffering from PTSD (Bayer, Klasen, & Adam, 2007). Additionally, aggressive behavior can be intrinsically rewarding: Offenders may simply get a thrill from being violent. We refer to this drive as appetitive aggression (Elbert, Weierstall & Schauer, 2010), a motivation that has been observed among youth offenders in low-income areas of Cape Town: Weierstall, Hinsberger et al. (2013) showed that participants with more traits of appetitive aggression presented with less impaired psychosocial functioning, implying that the attraction to aggressive behavior may reflect a process of adaptation to living in high-violence neighborhoods.
The role of alcohol and drugs in promoting appetitive aggression has yet to be investigated in a systematic manner: A recent study by Hecker and Haer (2015) examines the impact of prior drug abuse on emotional states during the perpetration of violence in combatants from the Democratic Republic of the Congo. Most combatants felt fearless, more powerful, and more aggressive after drug abuse and had a higher propensity to behave in an appetitively aggressive manner. Appetitive aggression may thus be fueled by drug abuse due to the (at times positive) qualities linked to substance abuse, such as increased arousal, lower social inhibitions and stronger feelings of companionship when in a group (Ching et al., 2012). Furthermore, as fear is reduced (Tyner & Fremouw, 2008), the urge to engage in aggression for the purposes of revenge and satisfaction may be unleashed.
Various factors – such as exposure to traumatic events and posttraumatic stress, appetitive aggression and substance abuse – have been hypothesized to contribute to the extremely high levels of violence in South Africa. Using path analyses, we have attempted to clarify the relationship between these factors in order to provide guidance for psychological programs for young offenders living in communities with high levels of violence and crime. In line with previous research, we investigated 1) whether exposure to violence is positively related to appetitive aggression, PTSD symptoms, substance abuse and the number of committed offenses; 2) whether posttraumatic stress has a positive correlation to drug abuse and the propensity toward aggressive behavior; 3) whether drug abuse is positively correlated to aggressive tendencies and the number of committed offenses; and 4) whether appetitive aggression is positively related to the number of violent offenses as the main outcome variable.
2. Materials and methods
2.1. Participants
In 2013–2014, structured clinical interviews were conducted with 290 males in the ages of 14–40 years (M = 21.96, SD = 4.53). All respondents were Black Africans of Xhosa ethnicity from low-income areas in Cape Town and were contacted through REALISTIC, a community-based organization that seeks to rehabilitate young offenders. Recruitment focused on former offenders currently attending a reintegration program (20%), and those who had previously completed such programs as well as individuals at risk for perpetrating or becoming victims of crime (80%). The educational level was rather low, with 81% of the participants failing to meet secondary-school graduation requirements.
The ethical review boards of the University of Konstanz, Stellenbosch University and the University of Cape Town approved the study, and all participants gave their informed consent. For those under the age of 18, parents or caretakers gave informed consent. For their participation in the interview, participants received financial compensation.
2.2. Procedure
In order to ensure confidentiality and privacy, data were collected at the organization's premises in Cape Town or at private offices nearby. The diagnostic interviews were conducted by a group of four German mental-health experts and three local counselors who had received 25 h of training in the theoretical concepts of mental disorders, trauma, aggression and clinical diagnosis through the use of structured interviews. Furthermore, to ensure the valid assessment of trauma symptoms and appetitive aggression, concepts and translations were discussed in detail with the interpreters before their application in the interviews. Bilingual native (Xhosa-speaking) interpreters who were specifically trained in translation in clinical settings assisted with administration and translated the questionnaires into isiXhosa and back to English. In cases in which participants reported suicidal thoughts or acute mental-health problems, counseling or referral to local psychiatric health services was provided.
2.3. Measures
2.3.1. Traumatic event types
A checklist of 36 potentially traumatic events (e.g. physical attack, sexual assault, torture) adapted from the Children's Exposure to Violence Checklist (CEVC; Amaya-Jackson, 1998) was administered to assess experienced and witnessed traumatic event types. This scale has demonstrated excellent internal consistency and good test-retest reliability, also in South African settings (Fehon et al., 2001, Fincham et al., 2009), and has proven its validity in offender populations (Weierstall, Hinsberger et al., 2013). We calculated the total number of self-experienced and witnessed traumatic events types, with a possible range from 0 to 36. Reliability was calculated according to Dunn, Baguley, and Brunsden (2014) by using omega (McDonald, 1999), a measure of internal consistency that is considered to be more sensible than Cronbach's alpha (e.g. Zinbarg, Revelle, Yovel, & Li, 2005). Coefficient omega in our sample was 0.79, 95% confidence interval (CI) [0.75–0.82].
2.3.2. Posttraumatic stress symptom severity
PTSD symptom severity during the past two weeks was assessed using the PTSD Symptom Scale-Interview (PSS-I; Foa & Tolin, 2000). For each of the 17 items, ratings ranged from 0 (not at all) to 3 (very much), expressing to which extent a specific trauma was associated with each of the B, C and D PTSD symptoms of the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000). The measure's validity has been proven in South African offender and other African populations (e.g. Köbach et al., 2015, Weierstall et al., 2013). The PSS-I sum score was calculated by summing all item scores; possible sum scores ranged from 0 to 51 points. Coefficient omega in this sample was 0.88, 95% CI [0.85–0.90].
2.3.3. Appetitive Aggression Scale
An individual's propensity toward perpetrating aggressive acts was assessed using the Appetitive Aggression Scale (AAS; Weierstall & Elbert, 2011), a structured interview that has been successfully implemented in previous African samples, including South African young offenders, and has been proven to have excellent psychometric properties (e.g. Weierstall et al., 2013, Weierstall et al., 2012). The AAS contains 15 questions concerning the appetitive perception of aggression (e.g. “Is it exciting for you if you make an opponent really suffer?”). Each item is scored on a 5-point Likert scale ranging from 0 (I totally disagree) to 4 (I totally agree). For the analysis, the AAS sum score was calculated, with a possible range from 0 to 60. The reliability of the scale was high in our sample (coefficient omega = 0.87, 95% CI [0.84–0.89]).
2.3.4. Number of offense types
To measure self-committed aggressive behavior, we assessed the number of committed offenses using a checklist of 21 different types of offenses (e.g. assault, rape, murder) from the AAS, which has previously been successfully administered in a South African population of youth offenders (Weierstall, Hinsberger et al., 2013). We summed the number of committed offenses to obtain the offense types sum score; possible scores ranged from 0 to 21 points. Coefficient omega in this sample was 0.88, 95% CI [0.86–0.90].
2.3.5. Drug abuse before offenses
In combination with the list of offense types, we asked about the frequency of drug abuse before the perpetration of violent acts (“How often did you drink or take drugs before these events?”). Participants answered on a 5-point Likert scale, ranging from 0 (not at all) to 4 (every time). Additionally, we assessed substance dependence with the Mini-International Neuropsychiatric Interview based on DSM-IV criteria (M.I.N.I. version 6.0.0; Sheehan et al., 1998).
2.4. Data analysis
Path analyses were performed with AMOS 22 for SPSS. To test the hypothesized relationships, we included traumatic events as a predictor variable for appetitive aggression, PTSD symptom severity, drug consumption prior to offenses and number of offenses, while appetitive aggression was included as predictor for the number of offenses, PTSD symptoms as a predictor for appetitive aggression and drug abuse, and drug abuse as a predictor for appetitive aggression and the number of offense types, which represented the main outcome variable. Of the 290 participants, 38 had missing data for one or more of the variables; these values were estimated using maximum likelihood estimation, thereby providing more accurate estimates of population parameters than other methods, such as deletion of missing cases (Enders, 2006).
3. Results
3.1. Characteristics of trauma, aggression and drug abuse
Demographic and trauma-, aggression- and drug-related sample characteristics are shown in Table 1. Participants were exposed to or had witnessed a broad range of 5–32 different traumatic experiences (M = 18.71, SD = 5.11), indicating high levels of poly-victimization. PTSD symptoms ranged from 0 to 39 points (M = 8.49), and the AAS score from 0 to 60 points (M = 15.42). Participants reported perpetration of a variety of violent acts, with scores ranging from 1 to 21 and a mean score of 11.65 violent acts committed. In the sample, 24.5% of the participants stated that they had mutilated at least one person in their lifetime, and 21.4% reported committing a murder at least once. With regard to drug abuse, 31.2% of the participants reported that they had never used drugs before committing violence, 28.4% declared that they had “rarely” or “sometimes” used drugs before offenses and 40.3% said they had used drugs “most of the time” or “every time” before perpetrating violence. 55.2% of the participants were diagnosed with a substance dependence disorder in the course of the interview. The most-used drugs related to substance dependence were cannabis (“dagga”, 38.6%), alcohol (33.4%), methamphetamine (“tik”, 13.4%) and methaqualone (“mandrax”, a sedative, 5.2%). Statistical analyses revealed no significant difference between those who had participated in a reintegration program at the time of the assessment and those who had not with regard to the outcome variables.
Table 1.
Demographic characteristics (n = 290) and clinical data.
| Variable | M (SD) or n (%) | [Range] |
|---|---|---|
| Age | 21.96 (4.53) | [14–40] |
| Years of formal education | 10.46 (1.77) | [1–16] |
| Traumatic events | 18.71 (5.11) | [5–32] |
| Index trauma | ||
| Being attacked with a weapon | 64 (24.9%) | – |
| Someone close being murdered | 23 (8.9%) | – |
| PSS-I | 8.49 (9.07) | [0–39] |
| AAS | 15.42 (13.08) | [0–60] |
| Offense types committed | 11.65 (4.35) | [1 − 21] |
| Mutilating at least one person | 71 (24.5%) | [0–>10] |
| Committing a murder at least once | 62 (21.4%) | [0–>10] |
| Substance dependence diagnosis | 160 (55.2%) | – |
| Drugs most used | ||
| Marijuana | 112 (38.6%) | – |
| Alcohol | 97 (33.4%) | – |
| Methamphetamine | 39 (13.4%) | – |
| Methaqualone (“mandrax”) | 15 (5.2%) | – |
PSS-I = PTSD symptom severity; AAS = appetitive aggression score.
3.2. Path analyses
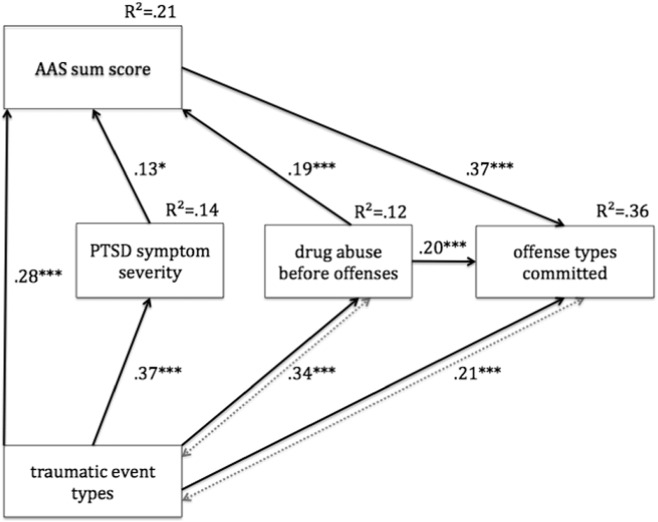
According to fit criteria (Hu & Bentler, 1999), the hypothesized model fit the data well: χ2 (1, N = 290) = 2.18, p = 0.140, CFI = 0.995, RMSEA = 0.064, 90% CI [0.000–0.184]. However, the hypothesized link between PTSD symptom severity and drug abuse prior to violence was non-significant. This link was excluded and a revised model obtained. Fig. 1 shows the final model.
Fig. 1.
Path model of relationships between traumatic events, PTSD symptoms, appetitive aggression, committed offense types and drug abuse prior to the commission of offenses. Paths with one arrowhead indicate directed associations. Paths connected through dotted arrows indicate possible reciprocal relations. Standardized regression weights are shown. *p < 0.05, **p < 0.01, ***p < 0.001.
The final model accounted for 21% of the variance in appetitive aggression, 14% in PTSD symptoms, 12% in drug consumption and 36% in the number of committed offense types. Fit statistics for the final model were good: χ2 (2) = 3.84, p = 0.146, χ2/df = 1.92, CFI = 0.993, RMSEA = 0.056, 90% CI [0.000–0.142].
In line with previous research, the model revealed that the number of traumatic event types exhibited strong positive relationships with appetitive aggression, PTSD symptoms, the number of offense types committed and drug abuse prior to the perpetration of violence. Furthermore, PTSD symptom severity was positively related to appetitive aggression, which itself was highly correlated to the number of offense types committed. Additionally, our results indicate that using drugs before committing violence seems to exacerbate the attraction to cruelty and the extent of perpetrated violence.
4. Discussion
This study investigated the relationships between traumatic experiences, PTSD symptoms, appetitive aggression, drug abuse and perpetrated violence in a sample of at-risk young men living in low-income urban areas in South Africa. Using path analyses, we obtained a dose-response effect between cumulative exposure to traumatic stressors and PTSD symptom severity, i.e. a positive relationship between the number of different traumatic events and the severity of PTSD symptoms, in line with previous research (Köbach et al., 2015, Neuner et al., 2004, Wilker et al., 2015). Moreover, appetitive aggression and the level of perpetrated violence seem to increase with a higher number of traumatic experiences, an effect that has also been reported in previous studies (e.g. Hecker et al., 2013, Weierstall et al., 2012). However, it must be considered that the likelihood of being victimized may also be enhanced by engagement in violent acts, such that this path most likely represents a reciprocal relationship (Fetchenhauer & Rohde, 2002). Additionally, we find that exposure to traumatic events is positively related to drug abuse prior to violent behavior. One explanation for this could be that youth from adverse environments often seek protection in gangs (Kerig, Wainryb, Twali, & Chaplo, 2013), groups in which drug abuse is integrated into everyday activities (Aldridge & Medina, 2008). Drug abuse in those who engage in gang violence may be reinforced by peer pressure and the desire to maintain one's status in the gang (Brunelle, Brochu, & Cousineau, 2000), and may play an important role in facilitating the commission of criminal acts, either by calming nerves or bolstering courage (Goldstein, Brownstein, Ryan, & Belluci, 1989). However, alcohol or drug abuse may also increase the probability of experiencing traumatic events, since one may become more likely to provoke or be involved in a fight, which may in turn result in a traumatic experience (Murdoch, Pihl, & Ross, 1990).
Furthermore, our data showed no significant relationship between PTSD symptom severity and drug abuse prior to the perpetration of violence. With regard to victim-offender populations, this result may be interpreted in accordance with Hecker and Haer (2015), who suggest that drugs may be consumed in order to feel more vigilant, powerful and fearless (Goldstein et al., 1989) when committing violent acts such as murder or rape, rather than to cope with the psychological impact of PTSD symptoms (Bonin, Norton, Asmundson, Dicurzio, & Pidlubney, 2000). However, we found a significant relationship between PTSD and appetitive aggression, and we hypothesize that comorbid PTSD symptoms, such as revenge fantasies (Maercker & Horn, 2013), may evolve into a proactive intrinsic motivation for violence, i.e. appetitive aggression. This may then encourage an individual to join criminal subcultures or gangs for revenge, groups that are commonly characterized by a violent and aggressive masculinity (Kynoch, 1999), providing a fertile ground for the development of cruel behavior. Additionally, as pointed out by Hinsberger et al. (2016), being part of such groups embossed by appetitive aggression, may also prolong PTSD symptoms as normative claims for vengeance of murdered gang members may trigger traumatic memories, leading to a complex association between PTSD and appetitive aggression.
Our model revealed a large effect for the relationship between drug abuse prior to the commission of violent acts and engagement in violence. It seems likely that drug abuse before committing violence leads to a full display of the person's potential for aggression, which may result in a greater extent of violent behavior in terms of the number and types of offenses. Furthermore, drugs may be used in order to avoid negative feelings of guilt or shame (Brunelle et al., 2000) and may therefore increase the probability of further violence committed under the influence. A reduction in negative emotions and an increase in the positive evaluation of violence may be reflected in the positive correlation between substance abuse and appetitive aggression. An increased lust for aggression when violence is committed under the influence of drugs may be due to drug-induced feelings of enhanced confidence and energy (Panenka et al., 2013), euphoria (Cheng, Jong, Li, Ko, & Wu, 2006) or emotions related to amusement and entertainment (Ching et al., 2012). The aforementioned beneficial effect of appetitive aggression in terms of adaptation to an adverse environment (Weierstall, Haer, Banholzer, & Elbert, 2013) may thus be enhanced by the positive features of drug or alcohol consumption (e.g. increased arousal, reduced inhibitions), which may in turn lead to a further increase in the number and severity of violent acts, as shown in our model.
In sum, the relationship between drug abuse and exposure to as well as engagement in violence may best be described as a vicious cycle in which the contributory factors are so tightly linked that it becomes difficult to disentangle cause and effect (Brunelle et al., 2000). However, the understanding that drug abuse – like traumatic stress and the exposure to violence – seems to increase appetitive aggression and violent outbursts is of great importance and has significant treatment implications.
4.1. Limitations
We assessed the impact of drug abuse on violence with an emphasis on young male South Africans at risk for criminal offenses, which may limit the external validity of these findings. In order to establish whether our findings of a drug-violence nexus are replicable in different conflict settings and thus have generalizability potential, the aforementioned relationships should be explored in future studies. Given the correlational and retrospective nature of this cross-sectional study, causality cannot be directly inferred, and conclusions about temporal or causal relationships between the variables should be drawn with caution.
4.2. Conclusions
Alarmingly high levels of violence and drug abuse, particularly in low-income areas in South Africa, indicate a clear need for a better understanding of the relationship between the various factors that contribute to a downward spiral; such an understanding could serve as the basis for violence- and drug-prevention programs as well as sensitive trauma- and aggression-focused treatments. This is of special importance as traumatic experiences, resulting aggression, and drug abuse have been indicated to be linked to school failure and dropout (e.g. Walker & Sprague, 1999) – which is also reflected by the high rate of participants in our study without a high school degree - and therefore stressing the aforementioned downward spiral.
The present study provides evidence of the necessity of simultaneously addressing multiple risk factors in violence intervention efforts, given that trauma, appetitive aggression and substance abuse are inextricably interlinked. Reducing substance abuse is likely to contribute to a decrease in the high rates of violence among young South Africans (Morojele & Brook, 2006). Compared to incarceration, multi-systemic interventions for serious offenders may reduce costs – financial costs and, more importantly, psychological and social costs – in the long term (Randall & Cunningham, 2003).
Role of funding sources
Funding for this study was provided by the European Research Council (T.E., ERC-2012-AdG-323977 MemoTV) and the German National Academic Foundation (J.S.). The European Research Council and the German National Academic Foundation had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Contributors
Thomas Elbert, Roland Weierstall, Jessica Sommer and Martina Hinsberger wrote the protocol and all authors contributed to the study design. Data collection was performed by Jessica Sommer and Martina Hinsberger. Jessica Sommer conducted literature searches and the statistical analysis. Jessica Sommer wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of interest
All authors declare that they have no conflicts of interest.
Acknowledgments
The authors wish to gratefully thank the study participants, the REALISTIC staff, the local counselors and interpreters, and Veronika Wieshammer, Noah Lorenz and Sarah Wilker, who helped to conduct this study. This research was supported by a scholarship of the German National Academic Foundation (J.S.) and the European Research Council (T.E., ERC-2012-AdG 323977 Memo TV).
Contributor Information
Jessica Sommer, Email: jessica.sommer@uni-konstanz.de.
Martina Hinsberger, Email: martina.hinsberger@uni-konstanz.de.
Thomas Elbert, Email: thomas.elbert@uni-konstanz.de.
Leon Holtzhausen, Email: leon.holtzhausen@uct.ac.za.
Debra Kaminer, Email: debbie.kaminer@uct.ac.za.
Soraya Seedat, Email: sseedat@sun.ac.za.
Solomon Madikane, Email: solomonmadikane@gmail.com.
Roland Weierstall, Email: roland.weierstall@uni-konstanz.de.
References
- Aldridge J., Medina J. ESRC; Swindon: 2008. Youth gangs in an English city: Social exclusion, drugs and violence: Full research report ESRC end of award report, RES-000-23-0615. [Google Scholar]
- Amaya-Jackson L. Trauma Evaluation, Treatment and Research Program, Centre for Child and Family Health; Durham, NC: 1998. Child's exposure to violence checklist. [Google Scholar]
- American Psychiatric Association . Author; Washington, DC: 2000. Diagnostic and statistical manual of mental disorders (4th ed., text rev.) [Google Scholar]
- Bayer C., Klasen F., Adam H. Association of trauma and PTSD symptoms with openness to reconciliation and feelings of revenge among former Ugandan and Congolese child soldiers. The Journal of the American Medical Association. 2007;298:555–559. doi: 10.1001/jama.298.5.555. [DOI] [PubMed] [Google Scholar]
- Bonin M.F., Norton G.R., Asmundson G.J.G., Dicurzio S., Pidlubney S. Drinking away the hurt: The nature and prevalence of PTSD in substance abuse patients attending a community-based treatment program. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31:55–66. doi: 10.1016/s0005-7916(00)00008-2. [DOI] [PubMed] [Google Scholar]
- Bremner J.D., Southwick S.M., Darnell A.D., Charney D.S. Chronic PTSD in Vietnam combat veterans: Course of illness and substance abuse. The American Journal of Psychiatry. 1996;153:369–375. doi: 10.1176/ajp.153.3.369. [DOI] [PubMed] [Google Scholar]
- Brunelle N., Brochu S., Cousineau M.-M. Drug-crime relations among drug-consuming juvenile delinquents: A tripartite model and more. Contemporary Drug Poblems. 2000;27:835–866. [Google Scholar]
- Cheng H.-L., Jong Y.-J., Li J.-H., Ko W.-K., Wu S.-M. Cation-selective exhaustive injection and sweeping MEKC for direct analysis of methamphetamine and its metabolites in urine. Electrophoresis. 2006;27:4711–4716. doi: 10.1002/elps.200600174. [DOI] [PubMed] [Google Scholar]
- Chermack S.T., Blow F.C. Violence among individuals in substance abuse treatment: The role of alcohol and cocaine consumption. Drug and Alcohol Dependence. 2002;66:29–37. doi: 10.1016/s0376-8716(01)00180-6. [DOI] [PubMed] [Google Scholar]
- Ching H., Daffern M., Thomas S. Appetitive violence: A new phenomenon? Psychiatry, Psychology and Law. 2012;19:745–763. [Google Scholar]
- Doweiko H.E. 9th ed. Cengage Learning; Stamford, CT, USA: 2015. Concept of chemical dependency. [Google Scholar]
- Dunn T.J., Baguley T., Brunsden V. From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. British Journal of Psychology. 2014;105(3):399–412. doi: 10.1111/bjop.12046. [DOI] [PubMed] [Google Scholar]
- Elbert T., Weierstall R., Schauer M. Fascination violence: On mind and brain of man hunters. European Archives of Psychiatry and Clinical Neuroscience. 2010;260:100–105. doi: 10.1007/s00406-010-0144-8. [DOI] [PubMed] [Google Scholar]
- Enders C.K. A primer on the use of modern missing-data methods in psychosomatic medicine research. Psychosomatic Medicine. 2006;68:427–736. doi: 10.1097/01.psy.0000221275.75056.d8. [DOI] [PubMed] [Google Scholar]
- Fehon D.C., Grilo C.M., Lipschitz D.S. Correlates of community violence exposure in hospitalized adolescents. Comprehensive Psychiatry. 2001;42:283–290. doi: 10.1053/comp.2001.24580. [DOI] [PubMed] [Google Scholar]
- Fetchenhauer D., Rohde P.A. Evolutionary personality psychology and victimology: Sex differences in risk attitudes and short-term orientation and their relation to sex differences in victimizations. Evolution and Human Behavior. 2002;23:233–244. [Google Scholar]
- Fincham D., Grimsrud A., Corrigall J., Williams D.R., Seedat S., Stein D.J., Myer L. Intermittent explosive disorder in South Africa: Prevalence, correlates and the role of the traumatic exposures. Psychopathology. 2009;42:92–98. doi: 10.1159/000203341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E.B., Tolin D.F. Comparison of the PTSD Symptom Scale-interview version and the clinician-administered PTSD Scale. Journal of Traumatic Stress. 2000;13:181–191. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- Goldstein P.J., Brownstein H.H., Ryan P.J., Belluci A. Crack and homicide in New York City, 1988: A conceptually based event analysis. Contemporary Drug Problems. 1989;16:651–687. [Google Scholar]
- Groenewald P., Bradshaw D., Nojilana B., Bourne D., Nixon J., Mohamed H. South African Medical Research Council; Cape Town: 2003. Cape town mortality 2001, part 1: Cause of death and premature mortality; p. 2003. (Available at: http://www.mrc.ac.za/bod/reports.htm) [Google Scholar]
- Hecker T., Haer R. Drugs boosting conflict? A micro-level test of the linkage between substance use and violence. Terrorism and Political Violence. 2015;27:205–224. [Google Scholar]
- Hecker T., Hermenau K., Maedl A., Schauer M., Elbert T. Aggression inoculates against PTSD symptom severity – Insights from armed groups in the eastern DR Congo. European Journal of Psychotraumatology. 2013;4:1–9. doi: 10.3402/ejpt.v4i0.20070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellmuth J.C., Stappenbeck C.A., Hoerster K.D., Jakupcak M. Modeling PTSD symptom clusters, alcohol misuse, anger and depression as they relate to aggression and suicidality in returning U.S. veterans. Journal of Traumatic Stress. 2012;25:527–534. doi: 10.1002/jts.21732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinsberger M., Sommer J., Kaminer D., Holtzhausen L., Weierstall R., Seedat S.…Elbert T. Perpetuating the cycle of violence in South African low-income communities: Attraction to violence in young men exposed to continuous threat. European Journal of Psychotraumatology. 2016;7:29099. doi: 10.3402/ejpt.v7.29099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):155. [Google Scholar]
- Kerig P.K., Wainryb C., Twali M.S., Chaplo S.D. America's child soldiers: Toward a research agenda for studying gang-involved youth in the United States. Journal of Aggression, Maltreatment & Trauma. 2013;22:773–795. [Google Scholar]
- Klostermann K.C., Fals-Stewart W. Intimate partner violence and alcohol use: Exploring the role of drinking in partner violence and its implications for intervention. Aggression and Violent Behavior. 2006;11:587–597. [Google Scholar]
- Köbach A., Schaal S., Elbert T. Combat high or traumatic stress: Violent offending is associated with appetitive aggression but not with symptoms of traumatic stress. Frontiers in Psychology. 2015;5:1518. doi: 10.3389/fpsyg.2014.01518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kynoch G. From the Ninevites to the hard livings gang: Township gangsters and urban violence in twentieth-century South Africa. African Studies. 1999;58(1):55–85. [Google Scholar]
- Lockhat R., Niekerk V. South African children: A history of adversity, violence and trauma. Ethnicity & Health. 2000;5:291–302. doi: 10.1080/713667462. [DOI] [PubMed] [Google Scholar]
- Maercker A., Horn A.B. A socio-interpersonal perspective on PTSD: The case for environments and interpersonal processes. Clinical Psychology & Psychotherapy. 2013;20:465–481. doi: 10.1002/cpp.1805. [DOI] [PubMed] [Google Scholar]
- Mathews S., Abrahams N., Jewkes R., Martin L.J., Lombard C. Alcohol use and its role in female homicides in the Western Cape, South Africa. Journal of Studies on Alcohol and Drugs. 2009;70:321–327. doi: 10.15288/jsad.2009.70.321. [DOI] [PubMed] [Google Scholar]
- Maxson C.L., Whitlock M.L., Klein M.W. Vulnerability to street gang membership: Implications for practice. Social Service Review. 1998;72:70–91. [Google Scholar]
- McDonald R.P. Lawrence Erlbaum; Mahwah, NJ: 1999. Test theory: A unified treatment. [Google Scholar]
- Morojele N.K., Brook J.S. Substance use and multiple victimisation among adolescents in South Africa. Addictive Behaviors. 2006;31:1163–1176. doi: 10.1016/j.addbeh.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Murdoch D., Pihl R.O., Ross D. Alcohol and crimes of violence: Present issues. The International Journal of the Addictions. 1990;25:1065–1081. doi: 10.3109/10826089009058873. [DOI] [PubMed] [Google Scholar]
- Neuner F., Schauer M., Karunakara U., Klaschik C., Robert C., Elbert T. Psychological trauma and evidence for enhanced vulnerability for PTSD through previous trauma in West Nile refugees. BMC Psychiatry. 2004;4:34. doi: 10.1186/1471-244X-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panenka W.J., Procyshyn R.M., Lecomte T., MacEwan G.W., Flynn S.W., Honer W.G., Alasdair M.B. Methamphetamine use: A comprehensive review of molecular, preclinical and clinical findings. Drug and Alcohol Dependence. 2013;129:167–179. doi: 10.1016/j.drugalcdep.2012.11.016. [DOI] [PubMed] [Google Scholar]
- Parrot D.J., Drobes D.J., Saladin M.E., Coffey S.F., Dansky B.S. Perpetration of partner violence: Effects of cocaine and alcohol dependence and posttraumatic stress disorder. Addictive Behaviors. 2003;28:1587–1602. doi: 10.1016/j.addbeh.2003.08.036. [DOI] [PubMed] [Google Scholar]
- Parry C.D.H., Myers B., Morojele N.K., Flisher A.J., Bhana A., Donson H., Plüddemann A. Trends in adolescent alcohol and other drug use: Findings from three sentinel sites in South Africa (1997–2001) Journal of Adolescence. 2004;27:429–440. doi: 10.1016/j.adolescence.2003.11.013. [DOI] [PubMed] [Google Scholar]
- Parry C.D.H., Plüddemann A., Louw A., Leggett T. The 3-metros study of drugs and crime in South Africa: Findings and policy implications. The American Journal of Drug and Alcohol Abuse. 2004;30:167–185. doi: 10.1081/ada-120029872. [DOI] [PubMed] [Google Scholar]
- Plüddemann A., Flisher A.J., McKetin R., Parry C., Lombard C. Methamphetamine use, aggressive behavior and other mental health issues among high-school students in Cape Town, South Africa. Drug and Alcohol Dependence. 2010;109:14–19. doi: 10.1016/j.drugalcdep.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramlagan S., Peltzer K., Matseke G. Epidemiology of drug abuse treatment in South Africa. South African Journal of Psychiatry. 2010;16:40–49. [Google Scholar]
- Randall J., Cunningham P.B. Multisystemic therapy: A treatment for violent substance-abusing and substance-dependent juvenile offenders. Addictive Behaviors. 2003;28:1731–1739. doi: 10.1016/j.addbeh.2003.08.045. [DOI] [PubMed] [Google Scholar]
- Rehm J., Rehn N., Room R., Monteiro M., Gmel G., Jernigan D., Frick U. The global distribution of average volume of alcohol consumption and patterns of drinking. European Addiction Research. 2003;9:147–156. doi: 10.1159/000072221. [DOI] [PubMed] [Google Scholar]
- Roizen J. Epidemiological issues in alcohol-related violence. In: Galanter M., editor. Recent developments in alcoholism. Vol. 13. Plenum Press; New York, NY: 1997. pp. 7–40. [DOI] [PubMed] [Google Scholar]
- Seedat M., Van Niekerk A., Jewkes R., Suffla S., Ratele K. Violence and injuries in South Africa: Prioritising an agenda for prevention. The Lancet. 2009;374:1011–1022. doi: 10.1016/S0140-6736(09)60948-X. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E.…Dunbar G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Sommer, J., Hinsberger, M., Weierstall, R., Holtzhausen, L., Kaminer, D., Seedat, S., Maercker, A., Madikane, S., & Elbert, T. Social acknowledgement of violent experiences and its role in PTSD and appetitive aggression among high-risk males in South Africa. Clinical Psychological Science, in press.
- Stewart S.H. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;1:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Taylor S.P., Chermack S.T. Alcohol, drugs and human physical aggression. Journal of Studies on Alcohol. 1993;11:78–88. doi: 10.15288/jsas.1993.s11.78. [DOI] [PubMed] [Google Scholar]
- Tyner E.A., Fremouw W.J. The relation of methamphetamine use and violence: A critical review. Aggression and Violent Behavior. 2008;13:285–297. [Google Scholar]
- Walker H.M., Sprague J.R. The path to school failure, delinquency, and violence. Intervention in School and Clinic. 1999;35:67–73. [Google Scholar]
- Weierstall R., Elbert T. The Appetitive Aggression Scale – Development of an instrument for the assessment of human's attraction to violence. European Journal of Psychotraumatology. 2011;2:8430. doi: 10.3402/ejpt.v2i0.8430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weierstall R., Huth S., Knecht J., Nandi C., Elbert T. Appetitive aggression as a resilience factor against trauma disorders: Appetitive aggression and PTSD in German World War II veterans. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0050891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weierstall R., Schalinski I., Crombach A., Hecker T., Elbert T. When combat prevents PTSD symptoms – Results from a survey with former child soldiers in Northern Uganda. BMC Psychiatry. 2012;12:41. doi: 10.1186/1471-244X-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weierstall R., Haer R., Banholzer L., Elbert T. Becoming cruel: Appetitive aggression released by detrimental socialization in former Congolese soldiers. International Journal of Behavioral Development. 2013;37:505–513. [Google Scholar]
- Weierstall R., Hinsberger M., Kaminer D., Holtzhausen L., Madikane S., Elbert T. Appetitive aggression and adaptation to a violent environment among youth offenders. Peace and Conflict: Journal of Peace Psychology. 2013;19:138–149. [Google Scholar]
- White H.R., Tice P.C., Loeber R., Stouthamer-Loeber M. Illegal acts committed by adolescents under the influence of alcohol and drugs. Journal of Research in Crime and Delinquency. 2002;39:131–152. [Google Scholar]
- Wilker S., Pfeiffer A., Kolassa S., Koslowski D., Elbert T., Kolassa I.T. How to quantify exposure to traumatic stressors? Reliability and validity of measures for cumulative trauma exposure in a post-conflict population. European Journal of Psychotraumatology. 2015;6 doi: 10.3402/ejpt.v6.28306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinbarg R., Revelle W., Yovel I., Li W. Cronbach's α, Revelle's β, and McDonald's ωH: Their relations with each other and two alternative conceptualizations of reliability. Psychometrika. 2005;70:123–133. [Google Scholar]