Abstract
Non-Hispanic blacks represent 13 % of the U.S.-born population but account for 37 % of tuberculosis (TB) cases reported in U.S.-born persons. Few studies have explored whether this disparity is associated with differences in TB-related knowledge and attitudes. Interviews were conducted with U.S.-born, non-Hispanic blacks and whites diagnosed with TB from August 2009 to December 2010 in cities and states that accounted for 27 % of all TB cases diagnosed in these racial groups in the U.S. during that time period. Of 477 participants, 368 (77 %) were non-Hispanic black and 109 (23 %) were non-Hispanic white. Blacks had significantly less knowledge and more misconceptions about TB transmission and latent TB infection than whites. Most TB patients in both groups recalled being given TB information; having received such information was strongly correlated with TB knowledge. Providing information to U.S.-born TB patients significantly increased their knowledge and understanding of TB. More focused efforts are needed to provide TB information to U.S.-born black TB patients.
Keywords: Health knowledge, Attitudes, Practice, Tuberculosis, U.S.-born, Race
Introduction
In the United States (U.S.), tuberculosis (TB) rates among U.S.-born persons decreased by 81 % from 1993 to 2012 [1]. Despite this success, certain populations remain disproportionately affected by TB. Non-Hispanic black persons represent 13 % of the U.S.-born population, yet account for 37 % of U.S.-born TB cases [2, 3]. Among U.S.-born racial and ethnic groups, the greatest racial disparity is among non-Hispanic blacks, whose TB rate in 2012 was six times higher than the rate for non-Hispanic whites [1, 3]. While this disparity is well documented in the literature [3–5], few studies to date have explored clinical, physiological, or cultural factors related to this disparity [6–10].
Knowledge constitutes one key factor integral to changing a person's behaviors [11–14]. Increasing understanding about latent TB infection (LTBI) and TB disease has been associated with healthy behaviors and more favorable outcomes for patients, including greater adherence to and completion of treatment for LTBI or TB [12, 15–19]. Studies have examined TB knowledge, attitudes, and behaviors (KAB) among the general U.S. population [12, 20, 21], and assessed TB knowledge for specific groups in the U.S. who are at high risk for TB, including foreign-born persons, drug and alcohol users, homeless persons and persons with LTBI [11, 15–17, 22–28]. No published research has measured TB KAB or assessed differences in TB knowledge between U.S.-born blacks and whites with TB. This analysis describes TB KAB of U.S.-born TB patients enrolled in a large, multi-site study and explores differences between black and white racial groups.
Methods
Participants
The Division of TB Elimination (DTBE) at the Centers for Disease Control and Prevention (CDC) funded the Tuberculosis Epidemiologic Studies Consortium (TBESC) to conduct epidemiologic, economic, operational, and behavioral studies related to TB; each of the 20 U.S. sites consisted of an academic or nonprofit organization linked to a local or state health department [29]. The main purpose of this study was to assess determinants of early diagnosis, prevention and treatment of TB between U.S.-born black and whites. Seven TBESC sites and three collaborating TB programs conducted this retrospective cohort study in locations that accounted for 36.8 % of TB cases among U.S.-born blacks and 15.8 % of cases among U.S.-born whites reported to the CDC's National Tuberculosis Surveillance System (NTBSS) during the enrollment period. The sites recruited recently diagnosed TB patients from health departments in the cities of Dallas, Houston, Philadelphia, New York, and Washington DC; the states of Maryland, New Jersey, North Carolina and Virginia; and urban jurisdictions within the states of Georgia and Tennessee. To be eligible to participate in the study, an individual had to be (1) diagnosed with a case of TB that met CDC reporting requirements [1], (2) U.S.-born, (3) non-Hispanic, (4) black, white, or a combination that included either race, (5) at least 15 years old at TB diagnosis, and (6) reported to the local health department from August 16, 2009 through December 31, 2010. Participants were enrolled sequentially from December 16, 2009 to March 31, 2011. Demographic and clinical characteristics of the final sample population were compared with those of cases in the NTBSS in the relevant catchment areas to assess representativeness. The study was approved by the CDC Institutional Review Board (IRB) and local IRBs. All participants provided written informed consent.
Data Collection and Variables
Data was collected through face-to-face interviews using a standardized questionnaire that asked about the TB diagnosis, care-seeking behaviors, medical and social history, and TB knowledge and attitudes. The TB knowledge portion of the questionnaire consisted of questions to assess participants’ knowledge about transmission, testing, and treatment for TB and LTBI. To assess how much TB education participants received from providers, participants were asked whether a doctor, nurse, or other health care provider discussed with them “what the TB medicines are for,” “how people get TB,” and “how to keep family and friends from getting TB.” Participants were also asked whether they had received enough information about TB or whether they would like more. The questionnaire also measured participants’ attitudes about TB, including perceptions of stigma, social norms, prioritization of treatment, perceived risk, and self-efficacy; these questions were measured on a four-point Likert scale, with 1 representing “Strongly disagree” and 4 representing “Strongly agree”.
For this analysis, we included responses to all questions on TB knowledge, attitudes and beliefs; recall of TB education by a provider; receipt of information about TB; and data on race, age, gender, education, employment status at time of interview, homelessness at time of interview, excessive alcohol use since the time of TB diagnosis, non-medical drug use since the time of TB diagnosis, history of incarceration, presence of a chronic illness, history of HIV/AIDS, history of TB disease, insurance status at time of interview, recall of TB education by a provider, and receipt of information about TB.
A knowledge score was created for each participant by summing correct responses to the individual knowledge questions; the maximum score was nine. Participants who responded that they did not know the answer were considered to have answered the question incorrectly. For each attitudinal item, the mean Likert score and standard deviation were calculated. For questions regarding the recall of TB education by a provider and the amount of TB information obtained, participants who responded “don't know” were considered to either have not discussed the topic with a provider or not received enough TB information.
Participants were categorized as racially black or white; a participant was considered black if the participant reported being black, African-American, black and white, or black and another race. Excessive alcohol use was defined as having five or more drinks on one occasion. Participants were classified as having a chronic illness if they reported ever being told by a doctor that they had diabetes, high blood pressure, asthma, heart problems, chronic obstructive pulmonary disease, or kidney problems.
Analysis
Differences between blacks and whites were assessed using two-sided chi-square tests for categorical variables and t-tests for continuous measures. The correlation matrix for all attitudinal items was examined, but due to low correlations, factor analysis could not be performed.
ANOVA was used to test the difference in mean knowledge scores by site. Since knowledge scores were normally distributed, bivariate and multivariate linear regression models examined associations between knowledge score and participant characteristics, recall of TB education, and the desire for more TB information. All variables with P value <0.15 were included in a multivariable regression analysis using backwards elimination. Multiplicative interaction terms were explored between race and other covariates in the final multivariable model. All analyses were conducted in SAS, Version 9.2 (SAS, INC, Cary, NC).
Results
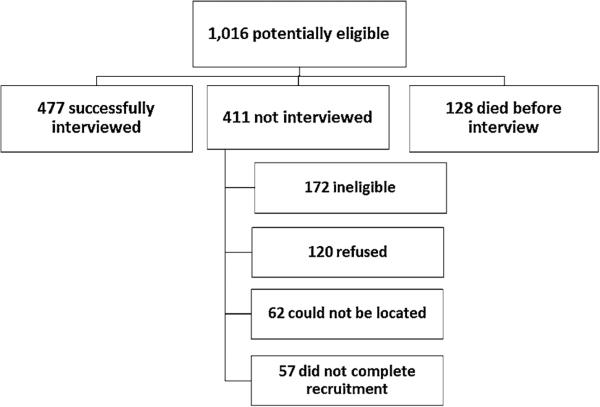
Based on surveillance data, 1,016 persons were potentially eligible for enrollment during the study period; 128 died before they could be interviewed, leaving 888 who could be approached for recruitment. Of these, 172 were ineligible (moved out of the jurisdiction, reported they were Hispanic or foreign-born, had a non-TB infection, or were incapable of providing consent); 120 refused; 62 could not be located or could not complete interviews after multiple tries; 57 did not complete recruitment; and 477 were successfully recruited (Fig. 1). Each site contributed 6–18 % to the study population.
Fig. 1.
Flowchart depicting outcome of attempts to enroll and interview U.S.-born, non-Hispanic black and white persons newly diagnosed with TB
Of the 477 participants who were interviewed (53.7 % of those who could be approached for recruitment), 368 (77.1 %) were black and 109 (22.9 %) were white (Table 1). The ratio of blacks to whites was 3:1, which was similar to the racial distribution of TB cases reported from the study catchment areas during the enrollment period. The mean age was 49.9 years and 324 (67.9 %) were male. The mean time between TB diagnosis and interview was 4 months (SD = 2; range 0–24). Blacks were younger, more likely to be unemployed, to have HIV/AIDS, and to report a history of incarceration than whites. Whites were more likely to have completed high school.
Table 1.
Demographics of all study participants
| Total study population (N = 477) X (SD) |
Black participants (N = 368) X (SD) |
White participants (N = 109) X (SD) |
P * | |
|---|---|---|---|---|
| Age (range 15–96 years) | 49.9 (17.2) | 47.9 (16.8) | 56.7 (16.8) | <0.0001 |
| N (%) | N (%) | N (%) | ||
| Male | 324 (67.9) | 244 (66.3) | 80 (73.4) | 0.164 |
| Current homelessness | 32 (6.7) | 25 (6.8) | 7 (6.4) | 0.892 |
| Completed high school | 298 (62.5) | 212 (57.6) | 86 (78.9) | <0.0001 |
| Prior TB diagnosis | 28 (5.9) | 21 (5.7) | 7 (6.4) | 0.780 |
| Excessive alcohol use | 63 (13.2) | 45 (12.2) | 18 (16.5) | 0.246 |
| Drug use | 62 (13.0) | 47 (12.8) | 15 (13.8) | 0.787 |
| Unemployed | 366 (76.7) | 295 (80.2) | 71 (65.1) | 0.001 |
| Uninsured | 223 (46.8) | 178 (48.4) | 45 (41.3) | 0.193 |
| Ever incarcerated | 235 (49.3) | 193 (52.4) | 42 (38.5) | 0.011 |
| History of a chronic illness | 304 (63.7) | 227 (61.7) | 77 (70.6) | 0.088 |
| History of HIV/AIDS | 81 (17.0) | 74 (20.1) | 7 (6.4) | 0.001 |
SD standard deviation
P value for the comparison of each variable by race
Knowledge
The mean knowledge score in the study population was 5.5 out of 9 (61.1 %; Table 2). Twenty participants (4.2 %) answered all knowledge questions correctly, and three participants responded “don't know” to all knowledge questions. The mean knowledge score did not differ significantly by site (P = 0.12; data not shown). Over 80 % of participants knew that a person could have TB germs in his/her body and not feel sick, that TB germs could be spread from person to person through the air, and that most cases of TB could be cured by taking medicines. Almost three quarters of participants incorrectly thought people with LTBI were contagious and that sharing dishes, bottles, or a toothbrush with someone who has TB increases a person's risk of getting TB (Table 2).
Table 2.
Numbers and proportions of study participants who correctly answered questions assessing TB knowledge, stratified by racea
| Question | Question answered correctly |
P * | ||
|---|---|---|---|---|
| Total study population (N = 477) N (%) |
Black participants (N = 368) N (%) |
White particpants (N = 109) N (%) |
||
| 1. Can a person have TB germs in their body and not feel sick? | 388 (81.3) | 287 (78.0) | 101 (92.7) | 0.001 |
| 2. If people have latent TB infection, that is, sleeping TB germs, can they give TB to other people?b | 137 (28.7) | 92 (25.0) | 45 (41.3) | 0.001 |
| 3. Are people with HIV more likely to develop TB than people who do not have HIV? | 258 (54.1) | 197 (53.5) | 61 (56.0) | 0.655 |
| 4. Does sharing dishes, bottles, or a toothbrush with someone who has TB, increase a person's chances of getting TB?b | 135 (28.3) | 99 (26.9) | 36 (33.0) | 0.212 |
| 5. Can TB germs be spread from person to person through the air? | 415 (87.0) | 314 (85.3) | 101 (92.7) | 0.046 |
| 6. Does a positive TB skin test always mean that a person has TB disease?b | 269 (56.4) | 198 (53.8) | 71 (65.1) | 0.036 |
| 7. Does a positive TB skin test usually mean that a person has TB germs in their body? | 361 (75.7) | 269 (73.1) | 92 (84.4) | 0.016 |
| 8. Are there medicines to prevent a person from getting TB? | 244 (51.2) | 202 (54.9) | 42 (38.5) | 0.003 |
| 9. Can most cases of TB be cured by taking medicines? | 426 (89.3) | 326 (88.6) | 100 (91.7) | 0.349 |
| Knowledge score [mean (SD)]c | 5.5 (1.8) | 5.4 (1.8) | 6.0 (1.6) | 0.004 |
SD standard deviation
P value for the comparison of each knowledge question by race
Participants who responded “don't know” or refused to answer were considered to have incorrectly answered the question
“No” was the correct response for questions 2, 4, and 6; for all other questions “Yes” was the correct response
Out of possible total score of 9
Whites had significantly higher overall knowledge scores than blacks. Blacks were more likely than whites to know that medicines are available to prevent a person from getting TB.
Recall of TB Education by a Provider
High proportions of participants reported that providers discussed the purpose of TB medicines (78.8 %), how people get TB (75.9 %), and how to avoid spreading TB (69.0 %). Participants who reported discussing these items with providers were significantly more likely to correctly answer the corresponding TB knowledge items (Table 3).
Table 3.
Association between correct responses to specific TB knowledge questions and recall of TB education by a provider
| Recall of communication with a provider | TB knowledge items |
P * | |
|---|---|---|---|
| Can most cases of TB be cured by taking medications? | |||
| Correct (n = 426) | Incorrect (n = 51) | ||
| Did the doctor tell you what TB medicines are for? | |||
| Yes (n = 376) | 342 (91.0 %) | 34 (9.0 %) | 0.025 |
| No (n = 101) | 84 (83.2 %) | 17 (16.8 %) | |
| Can TB germs be spread from person to person through the air? |
P * | ||
|---|---|---|---|
| Correct (n = 415) | Incorrect (n = 62) | ||
| Did the doctor tell you how people get TB? | |||
| Yes (n = 362) | 331 (91.4 %) | 31 (8.6 %) | <0.0001 |
| No (n = 115) | 84 (73.0 %) | 31 (27.0 %) | |
| Does sharing dishes, bottle or a toothbrush with someone who has TB increase a person's chances of getting TB? |
P * | ||
|---|---|---|---|
| Correct (n = 135) | Incorrect (n = 342) | ||
| Did the doctor tell you how to keep family and friends from getting TB? | |||
| Yes (n = 329) | 103 (31.3 %) | 226 (68.7 %) | 0.030 |
| No (n = 148) | 32 (21.6 %) | 116 (78.4 %) | |
P value for the comparison of the proportion of correct answers among those who received education to proportion of correct answers among those who did not receive education
Overall, 63 % of participants stated that they received enough information about TB (data not shown). While whites were more likely than blacks to say that they had enough TB information (P = 0.001), the mean knowledge score did not differ significantly between those who stated they had enough information and those who desired more; this relationship did not differ by race.
Participants who reported discussing the purpose of TB medicines with a provider were significantly more likely to report that they received enough TB information compared to those who reported that they did not discuss TB medicines with a provider (P = 0.001; data not shown). This association was seen among both whites (P = 0.031) and blacks (P = 0.004).
Factors Predicting Knowledge
In multivariable linear regression, a higher knowledge score was associated with white race, younger age, completion of high school, and recall that a provider discussed both what TB medicines were for and how people get TB (data not shown). For race, the adjusted model changed the coefficient from −0.56 to −0.75, a 33.9 % increase in effect. Translating the coefficients into an effect on the knowledge score and holding all other variables constant, white race was associated with an 18.8 % higher knowledge score. For example, a white 50 year old who did not complete high school and did not recall discussing with a provider what TB medicines were for or how people get TB has a predicted knowledge score of 4.74, compared to a score of 3.99 for a black person with the same characteristics. Interaction terms between race and the other covariates were examined; no interaction terms were significantly associated with knowledge.
Attitudes
Black and white participants had similar responses on 12 of the 18 attitudinal items (Table 4). Whites were more likely than blacks to agree that doctors were correct when diagnosing TB, that TB medicines can cause health problems, and that having TB will greatly affect their lives. Blacks were more likely than whites to agree that they would stop taking TB medications if the medications made them feel sick and that they know better than the doctor when it's time to stop taking medicine. Whites were more likely than blacks to agree that people get TB because they have bad luck. Participants of both races did not feel strongly stigmatized by TB, reporting that they would feel only “a little embarrassed” to tell people they had TB (Table 4).
Table 4.
Attitudes and beliefs about TB among study participants, stratified by race
| Attitudinal and belief statementa | Total study Population (N = 477) Mean (SD) |
Black participants (N = 368) Mean (SD) |
White participants (N = 109) Mean (SD) |
P * |
|---|---|---|---|---|
| 1. Your doctors were correct when they told you that you have TB | 3.5 (0.9) | 3.5 (0.9) | 3.7 (0.7) | 0.029 |
| 2. You feel ashamed to have TB | 1.9 (1.1) | 2.0 (1.2) | 1.8 (1.1) | 0.235 |
| 3. TB is as serious as other worries in your life | 3.2 (1.1) | 3.1 (1.1) | 3.4 (1.0) | 0.055 |
| 4. You have told people close to you that you have TB | 3.3 (1.1) | 3.3 (1.1) | 3.5 (1.0) | 0.057 |
| 5. You care what people close to you think of your TB treatment | 2.7 (1.3) | 2.7 (1.3) | 2.8 (1.3) | 0.407 |
| 6. Your doctor knows how to treat TB | 3.8 (0.6) | 3.7 (0.6) | 3.8 (0.5) | 0.257 |
| 7. TB medicines will cause health problems | 2.9 (1.1) | 2.8 (1.2) | 3.2 (0.9) | 0.003 |
| 8. You would stop taking your medications if they made you feel sick | 2.2 (1.3) | 2.3 (1.3) | 1.8 (1.2) | 0.001 |
| 9. People close to you care if you take TB medicines | 3.4 (1.1) | 3.4 (1.0) | 3.3 (1.2) | 0.167 |
| 10. You know better than the doctor when it's time to stop taking your medicines | 1.3 (0.8) | 1.4 (0.8) | 1.2 (0.5) | 0.007 |
| 11. People get TB because they have bad luck | 1.3 (0.8) | 1.3 (0.7) | 1.5 (0.9) | 0.013 |
| 12. You could have done something to keep from getting TB | 1.7 (1.1) | 1.8 (1.1) | 1.6 (1.0) | 0.065 |
| 13. Having TB will greatly affect your life | 2.4 (1.3) | 2.3 (1.3) | 2.7 (1.2) | 0.005 |
| 14. TB is something you can talk about with others | 3.0 (1.1) | 3.0 (1.2) | 3.1 (1.1) | 0.203 |
| 15. People close to you would avoid you if they thought you had TB | 2.2 (1.2) | 2.2 (1.2) | 2.3 (1.2) | 0.597 |
| 16. Other things going on in your life might keep you from finishing your TB treatment | 1.2 (0.6) | 1.3 (0.6) | 1.2 (0.6) | 0.432 |
| 17. You have been hurt by how people reacted when they found out you had TB | 1.8 (1.1) | 1.8 (1.1) | 1.7 (1.1) | 0.876 |
| 18. How embarrassed would you be to tell people you had TB?b | 3.1 (1.1) | 3.2 (1.1) | 3.1 (1.1) | 0.706 |
SD standard deviation
P value for the comparison of each item by race
Items measured on a 4-point Likert scale, where 1 = Strongly disagree, 2 = Disagree somewhat, 3 = Agree somewhat, and 4 = Strongly agree
This item was measured on a 4-point Likert scale where, where 1 = Very embarrassed, 2 = Moderately embarrassed, 3 = A little embarrassed, and 4 = Not at all embarrassed
Discussion
The influence of knowledge on changing a person's behaviors is well recognized; in particular, increasing TB knowledge has been associated with healthy behaviors and more favorable outcomes for TB patients [11–19]. This is the first study that compared TB knowledge and attitudes between U.S.-born black and white TB patients. Overall, patients had good understanding of airborne TB transmission and the availability of curative treatment for TB (>85 % correct), particularly when compared with a representative U.S. population (<45 % correct) and TB patients in other countries [19, 21, 30]. However, substantial misconceptions remained about the difference between TB and LTBI, TB transmission by casual contact, and the availability of effective treatment for LTBI. Even after controlling for other factors, blacks had significantly less knowledge and more misconceptions about TB and LTBI than whites; this has important implications for addressing the TB disparity in U.S.-born blacks.
Explaining the difference between infectious TB and noninfectious LTBI is extremely challenging, perhaps partly because of successful public health campaigns about other infectious diseases, such as HIV, that can be transmitted by asymptomatic persons. Similarly, well-publicized recommendations to avoid casual contact in order to prevent infectious diseases such as intestinal disorders may have contributed to the widespread misconception that TB is also spread by sharing dishes and other casual contact [31]. Documentation of this confusion appears repeatedly in the literature from studies of TB patients, persons with LTBI, and among both U.S.-born and foreign-born populations [17, 19, 23, 27, 30, 32–34]. This study suggests that an important factor in improving TB knowledge is simply providing an opportunity for patients to discuss TB-related topics with providers. A majority of participants recalled discussing TB-related topics with a provider, and those participants were more likely to correctly answer the corresponding TB knowledge questions. Moreover, participants who recalled talking about TB with a provider were more likely to report that they had enough TB information. The high percentages of TB patients in this study who understood that TB is transmitted through the air and is curable could be the result of discussions with providers; doctors and nurses could focus conversations on less well-understood topics to clear up misconceptions in these areas.
This is not the first study to show that simple interactions with patients can have beneficial effects in promoting knowledge and/or healthy behaviors. A New York City study involving 614 close contacts of TB patients found that TB program staff could significantly increase acceptance of HIV counseling, testing, and referral by simply asking participants about HIV status and offering the test to those who did not know their status [35].
Black TB patients in this study had less knowledge and more misconceptions about TB than whites. An important demographic difference between the two groups was education: more than three-quarters of whites had at least a high school education, compared to <60 % of blacks. Other studies have found that less formal education is associated with poorer understanding of TB [11, 21]. In this study, blacks were more likely to say that they did not have enough information about TB. Asking whether the person wants more information is a simple way to identify persons who could benefit from more discussion, and is an easy entry to a more focused conversation.
Studies among foreign-born persons found that participants reported feeling stigmatized because of their TB diagnosis [11, 33, 36]. A previous study of TB patients in North Carolina found significant social isolation [23]. However, our study did not find strong feelings of stigma among U.S.-born whites or blacks; most were not or only a little embarrassed by their TB diagnosis and felt they could talk to others about TB. This may reflect changes over time in attitudes towards TB. Timing of the interview may also have had an effect: our patients were interviewed relatively late in their treatment, and previous research has reported significant improvement in mental health and social functioning in TB patients over time. [37, 38]. The low level of stigma may provide an opportunity for providers to talk with patients about TB, and patients in turn may educate close friends and family about TB.
Generalizability of study conclusions could be limited by the high proportion of persons who refused or could not be recruited for other reasons. However, using data routinely collected on all TB cases reported to NTBSS, we found no differences in demographic and clinical variables (age, gender, race, HIV status, site of TB disease, and presence of pulmonary cavities on radiographs) between study participants and all U.S.-born non-Hispanic persons diagnosed with TB in the study catchment areas during the enrollment period. Another potential limitation is that the study population was a regional, not a national, sample. However, the jurisdictions involved accounted for more than one-fourth of all TB cases diagnosed among U.S.-born non-Hispanic persons during the enrollment period, and more than a third of all TB cases diagnosed among U.S.-born non-Hispanic blacks. Moreover, except for the higher proportion of blacks in the study jurisdictions—an intentional feature of the study design—NTBSS data showed that participants were also demographically and clinically similar to the entire national population of U.S.-born blacks and whites diagnosed with TB during the study period. This suggests that the study findings can be generalized to the national population of U.S.-born, non-Hispanic blacks and whites with TB.
It remains possible that persons not included in this study had different knowledge or attitudes about TB compared to study participants. Potential participants were told they would be asked about their diagnosis, and their health and social history, but were not told specific questions before enrollment. We have no reason to believe that potential participants would avoid the study due to concerns about specific questions. If knowledge influenced the decision to participate, it is most likely that persons with the least knowledge would be less likely to participate. In that case our findings may overstate the level of knowledge among TB patients. On the other hand, our findings may understate the feelings of stigma if those who felt strongly stigmatized evaded contact or were more likely to refuse participation.
Conclusions
Education is a continuous process, requiring repetition, trust, and different approaches to transmitting information [15]. This study shows that a majority of participants recall being given information on TB transmission, treatment, and protection of family and friends, and that participants who reported discussing TB medicines and TB transmission with a provider were more likely to correctly answer questions about these topics. Yet TB patients lacked an understanding about important differences between TB and LTBI as well as TB transmission and diagnosis, which are key issues for TB prevention and elimination in the U.S. Since providers were effective in relaying some information to recently diagnosed patients, continuing this educational process after diagnosis and increasing focus on topics that are less well understood may improve TB knowledge in this population. At a time of reduced funding and resources at all levels of public health programs [39], it is imperative that the information shared with patients is presented as effectively and accurately as possible. While improving TB knowledge may not eliminate the existing TB disparity between blacks and whites, understanding the role knowledge may play and what influences knowledge will allow us to better tailor messages and education to the populations who need it most.
Acknowledgments
We thank the investigators and staff at all the participating locations: Georgia: Gemina Albritton, Henry M. Blumberg, Michael Leonard, Jerome Mack, Jane Tapia; New York, NY: Holly Anger, Hugo Ortega; North Carolina: Shelly Harris, Monique Clayton, Burton Levine, Qiang Xia; Houston, TX: Edward A. Graviss, Larry Teeter, Pandora Williams;Virginia: Suzanne Keller, Brenda Mayes; Dallas, TX: Kenya Kemp, Chasity Lovely, Charles Wallace; Maryland and Washington, D.C.: Wendy Cronin, Fran Maurer, Bee Munk, Heather Rutz; Tennessee: Tamara Chavez-Lin-dell, Joe Pinilla, Trudy Stein-Hart, Jon Warkentin; New Jersey and Philadelphia, PA: Amy Davidow, Anna Sevilla, Jennifer Vergeon; We also thank the CDC DTBE project coordinator Melissa Pagaoa.
Footnotes
Conflict of interest The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Meredith M. Howley and Chaturia D. Rouse share responsibility as first author.
Contributor Information
Meredith M. Howley, New York State Department of Health, Albany, NY, USA
Chaturia D. Rouse, Case Western Reserve University School of Medicine, Cleveland, OH, USA
Dolores J. Katz, Centers for Disease Control and Prevention, Mailstop F-61, 1600 Clifton Road NE, Atlanta, GA, USA
Paul W. Colson, Charles P. Felton National Tuberculosis Center, Mailman School of Public Health, Columbia University, New York, NY, USA
Yael Hirsch-Moverman, Charles P. Felton National Tuberculosis Center, Mailman School of Public Health, Columbia University, New York, NY, USA.
Rachel A. Royce, RTI International, Research Triangle Park, NC, USA
References
- 1.Centers for Disease Control and Prevention . Reported Tuberculosis in the United States, 2012. U.S. Department of Health and Human Services, CDC; Atlanta, GA: 2013. [Google Scholar]
- 2.Grieco EM. Race and Hispanic origin of the foreign-born population in the United States: 2007. American Community Survey Reports, ACS-11. U.S. Census Bureau; Washington, DC: 2009. [13 May 2013]. http://www.census.gov/prod/2010pubs/acs-11.pdf. [Google Scholar]
- 3.Centers for Disease Control and Prevention Trends in tuberculosis—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(11):201–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Racial disparities in tuberculosis-selected southeastern states, 1991–2002. MMWR Morb Mortal Wkly Rep. 2004;53:556–9. [PubMed] [Google Scholar]
- 5.Stout JE, et al. Racial and ethnic disparities in pediatric tuberculosis in North Carolina. Arch Pediatr Adolesc Med. 2006;160(6):631–7. doi: 10.1001/archpedi.160.6.631. [DOI] [PubMed] [Google Scholar]
- 6.Serpa JA, et al. Tuberculosis disparity between US-born blacks and whites, Houston, Texas, USA. Emerg Infect Dis. 2009;15(6):899–904. doi: 10.3201/eid1506.081617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Golub JE, et al. Patient and health care system delays in pulmonary tuberculosis diagnosis in a low-incidence state. Int J Tuberc Lung Dis. 2005;9(9):992–8. [PubMed] [Google Scholar]
- 8.Kimerling ME, et al. Preventable childhood tuberculosis in Alabama: implications and opportunity. Pediatrics. 2000;105(4):E53. doi: 10.1542/peds.105.4.e53. [DOI] [PubMed] [Google Scholar]
- 9.O'Donnell MR, et al. Racial disparities in primary and reactivation tuberculosis in a rural community in the southeastern United States. Int J Tuberc Lung Dis. 2010;14(6):733–40. [PubMed] [Google Scholar]
- 10.Cantwell MF, et al. Tuberculosis and race/ethnicity in the United States. Am J Respir Crit Care Med. 1998;157(4):1016–20. doi: 10.1164/ajrccm.157.4.9704036. [DOI] [PubMed] [Google Scholar]
- 11.Colson PW, et al. Examining the impact of patient characteristics and symptomatology on knowledge, attitudes, and beliefs among foreign-born tuberculosis cases in the US and Canada. J Immigr Minor Health. 2014;16(1):125–35. doi: 10.1007/s10903-013-9787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ailinger RL, et al. Americans’ knowledge and perceived risk of tuberculosis. Public Health Nurs. 2003;20(3):211–5. doi: 10.1046/j.0737-1209.2003.20308.x. [DOI] [PubMed] [Google Scholar]
- 13.Champion VL, Skinner CS. The Health Belief Model. In: Glanz K, Rimer B, Viswanath K 4th, editors. Health behavior and health education: theory, research, and practice. Jossey-Bass; San Francisco: 2008. pp. 45–62. [Google Scholar]
- 14.Finnegan JR, Viswanath K. Communication theory and health behavior change: The media studies framework. In: Glanz K, Rimer B, Viswanath K 4th, editors. Health behavior and health education: Theory, research, and practice. Jossey-Bass; San Francisco: 2008. pp. 363–84. [Google Scholar]
- 15.Candy PC. [20 July 2013];Lifelong Learning and Information Literacy. White Paper prepared for UNESCO, the US National Commission on Libraries and Information Science, and the National Forum on Information Literacy, for use at the Information Literacy Meeting of Experts, Prague, The Czech Republic. 2002 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.119.5676&rep=rep1&type=pdf.
- 16.Carey JW, et al. Tuberculosis beliefs among recent Vietnamese refugees in New York State. Public Health Rep. 1997;112(1):66–72. [PMC free article] [PubMed] [Google Scholar]
- 17.Colson PW, et al. Tuberculosis knowledge, attitudes, and beliefs in foreign-born and US-born patients with latent tuberculosis infection. J Immigr Minor Health. 2010;12(6):859–66. doi: 10.1007/s10903-010-9338-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sebastian MS, Bothamley GH. Tuberculosis preventive therapy: perspective from a multi-ethnic community. Respir Med. 2000;94(7):648–53. doi: 10.1053/rmed.1999.0877. [DOI] [PubMed] [Google Scholar]
- 19.Liam CK, et al. Attitudes and knowledge of newly diagnosed tuberculosis patients regarding the disease, and factors affecting treatment compliance. Int J Tuberc Lung Dis. 1999;3(4):300–9. [PubMed] [Google Scholar]
- 20.Kirtland KA, et al. Knowledge and perceived risk of tuberculosis: US racial and regional differences. Ethn Dis. 2006;16(2):468–75. [PubMed] [Google Scholar]
- 21.Marks SM, et al. Knowledge, attitudes and risk perceptions about tuberculosis: US National Health Interview Survey. Int J Tuberc Lung Dis. 2008;12(11):1261–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Wolfe H, et al. Tuberculosis knowledge among New York City injection drug users. Am J Public Health. 1995;85(7):985–8. doi: 10.2105/ajph.85.7.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West EL, et al. Tuberculosis knowledge, attitudes, and beliefs among North Carolinians at increased risk of infection. NC Med J. 2008;69(1):14–20. [PubMed] [Google Scholar]
- 24.Peterson Tulsky J, et al. Street talk: knowledge and attitudes about tuberculosis and tuberculosis control among homeless adults. Int J Tuberc Lung Dis. 1999;3(6):528–33. [PubMed] [Google Scholar]
- 25.Marinac JS, et al. Knowledge of tuberculosis in high-risk populations: survey of inner city minorities. Int J Tuberc Lung Dis. 1998;2(10):804–10. [PubMed] [Google Scholar]
- 26.Joseph HA, et al. TB perspectives among a sample of Mexicans in the United States: results from an ethnographic study. J Immigr Minor Health. 2008;10(2):177–85. doi: 10.1007/s10903-007-9067-5. [DOI] [PubMed] [Google Scholar]
- 27.Ailinger RL, et al. Latino immigrants’ knowledge of tuberculosis. Public Health Nurs. 2004;21(6):519–23. doi: 10.1111/j.0737-1209.2004.21603.x. [DOI] [PubMed] [Google Scholar]
- 28.Nyamathi A, et al. Tuberculosis knowledge, perceived risk and risk behaviors among homeless adults: effect of ethnicity and injection drug use. J Community Health. 2004;29(6):483–97. doi: 10.1007/s10900-004-3396-2. [DOI] [PubMed] [Google Scholar]
- 29.Katz D, et al. Setting the agenda: a new model for collaborative tuberculosis epidemiologic research. Tuberculosis (Edinb) 2007;87(1):1–6. doi: 10.1016/j.tube.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Westaway MS. Knowledge and attitudes about tuberculosis of black hospitalised TB patients. Tubercle. 1990;71(1):55–9. doi: 10.1016/0041-3879(90)90062-d. [DOI] [PubMed] [Google Scholar]
- 31.CDC . Preventing norovirus infection. Atlanta, GA: 2014. [23 July 2014]. http://www.cdc.gov/norovirus/preventing-infection.html. [Google Scholar]
- 32.Tasnim S, Rahman A, Hoque FM. Patient's knowledge and attitude towards tuberculosis in an Urban setting. Pulm Med. 2012;2012:352850. doi: 10.1155/2012/352850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liefooghe R, et al. Perception and social consequences of tuberculosis: a focus group study of tuberculosis patients in Sialkot, Pakistan. Soc Sci Med. 1995;41(12):1685–92. doi: 10.1016/0277-9536(95)00129-u. [DOI] [PubMed] [Google Scholar]
- 34.Bakhshi SS, Ali S. Knowledge, attitude and behaviour of TB patients. J Public Health Med. 1995;17(3):343–8. [PubMed] [Google Scholar]
- 35.Li J, et al. Human immunodeficiency virus counseling, testing, and referral of close contacts to patients with pulmonary tuberculosis: feasibility and costs. J Public Health Manag Pract. 2007;13:252–62. doi: 10.1097/01.PHH.0000267683.85411.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mushtaq MU, et al. Urban-rural inequities in knowledge, attitudes and practices regarding tuberculosis in two districts of Pakistan's Punjab province. Int J Equity Health. 2011;10(1):8. doi: 10.1186/1475-9276-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marra CA, et al. Health-related quality of life trajectories among adults with tuberculosis: differences between latent and active infection. Chest. 2008;133:396–403. doi: 10.1378/chest.07-1494. [DOI] [PubMed] [Google Scholar]
- 38.Kelly P. Isolation and stigma: the experience of patients with active tuberculosis. J Community Health Nurs. 1999;16:233–41. doi: 10.1207/S15327655JCHN1604_3. [DOI] [PubMed] [Google Scholar]
- 39.Levi J, et al. Investing In America's Health: A state-by-state look at public health funding and key health facts. [17 April 2013];Trust for America's Health. 2013 Apr; http://healthyamericans.org/report/105/.