Abstract
Objective
To determine the feasibility of body weight–supported treadmill training (BWSTT) as a strategy for improving independent ambulation among patients who had sustained a hip fracture.
Design
Nonrandomized controlled trial.
Setting
Inpatient rehabilitation.
Participants
Patients with a stable hip fracture and at least 50% weight-bearing.
Intervention
BWSTT in lieu of standard walking exercises throughout stay in rehabilitation.
Main Outcomes Measures
Feasibility outcomes included the number of patients agreeing to participate in treadmill walking, the number who returned for follow-up assessments, compliance, and the number of adverse events. Secondary outcomes included the Lower Extremity Functional Scale, the Timed Up & Go test, a 2-minute walk test, and the Falls Self-Efficacy Scale. Univariate regression was used to assess the group effect on score changes from baseline to discharge and from baseline to follow-up.
Results
Among 41 potentially eligible patients, 21 (51%) agreed to participate and 14 returned for follow-up assessments. The recruitment goal of 12 patients agreeing to BWSTT was achieved; however, retention by 3-month follow-up was 67%. The average compliance was 3 sessions a week; however, several patients were below average. No adverse events of BWSTT were reported. There were no significant differences between groups with respect to secondary outcomes.
Conclusions
BWSTT may be a feasible method for retraining gait among patients with hip fracture. However, future studies evaluating its efficacy need rigorous methods for ensuring compliance and retention.
Keywords: Hip fractures, Physical therapy techniques, Rehabilitation
Hip fractures result in substantial morbidity and disability among older adults. Almost one half of women who have had a hip fracture will sustain a new fracture.1 The 1-year mortality rate after hip fracture has been reported to be 25%, and 24.3% of the survivors who were previously independent were living in institutions after the fracture.2 Almost 50% of patients living in the community after a hip fracture required a walking aid, such as a cane (32%), walker (39.4%), or wheelchair (31.8%).3 Patients with hip fracture have reported a fear of falling and a lower quality of life than those without hip fracture.4,5
Ambulatory capacity is a predictor of returning home after discharge after hip fracture.6,7 Mobility may be linked to lower extremity function; power of the leg extensors in the fractured leg has been positively associated with walking speed and stair-climbing time among patients after hip fracture.8,9 Current strategies for training independent ambulation involve muscle strengthening, weight shifting, and balance exercises, as well as walking with or without assistive aids, generally in the hallways of inpatient units. Patients with hip fracture may not be allowed to bear full body weight initially,10 which may be difficult for rehabilitation providers to control during walking exercises. Although participation in an inpatient rehabilitation program can achieve improvements in mobility, many patients with hip fracture remain dependent in transfers and locomotion at discharge.10,11 Further, patients with a hip fracture continue to experience functional impairment a year after the fracture.12,13
A Cochrane review highlighted the paucity of evidence for rehabilitation strategies aimed at improving mobility after hip fracture.14 BWSTT may be a useful method for retraining gait in patients with hip fracture because those who are not able to bear full weight on their lower limbs can walk with partial body weight support.15 A randomized controlled trial comparing 10 days of BWSTT to conventional therapy after total hip arthroplasty demonstrated significant improvements in Harris score (pain and mobility), muscle strength, and gait symmetry in favor of BWSTT, and these improvements persisted after 12 months.16 However, the population of hip arthroplasty patients includes mainly patients with osteoarthritis, a population that is very different with respect to age and other health-related characteristics than patients with hip fracture. Whether BWSTT is feasible among patients with hip fractures remains to be determined. Finally, there is little available information about the feasibility of recruitment and retention of patients with hip fracture for clinical trials implemented in the inpatient rehabilitation setting.
Therefore, the primary aim of the present study was to determine the feasibility of recruitment and implementation for a study of BWSTT as a strategy for improving independent ambulation among patients who had sustained a hip fracture and were participating in inpatient rehabilitation. As secondary aims, the study investigated the responsiveness of outcomes of interest (ie, mobility, fall concerns, and lower extremity function) to BWSTT among inpatients with hip fracture.
METHODS
Participants
Patients treated for a hip fracture by orthopedic surgeons and admitted to the inpatient rehabilitation floor of a teaching hospital between September 2006 and November 2007 were considered for participation. A break in recruitment was implemented from November to early January to avoid variation in physiotherapy care related to staff holidays. Patients were considered eligible for inclusion in the study if they were deemed by the surgeons to have a stable fracture or adequate fixation; they were able to follow 2-step commands; their rehabilitation restrictions were to be 50% weight-bearing or weight-bearing as tolerated; and they were able to take a few steps with the help of an assistive device. Exclusion criteria were as follows: in isolation; cultures positive for methicillin-resistant Staphylococcus aureus; able to walk without assistive devices; had hip, knee, or ankle surgery before the hip fracture; unable to understand instructions or give informed consent; incontinent; uncontrolled cardiovascular disease, uncontrolled hypertension, uncontrolled diabetes, neuromuscular disease, or other musculoskeletal disease such as rheumatoid arthritis; or uncontrolled pain. This study received approval by the local research ethics board.
Research Design
The research design was a pilot, nonrandomized controlled trial. It was a priority to ensure that at least 12 patients completed the intervention in the specified time frame. Therefore, participants were recruited to participate in the intervention until 12 patients completed the intervention and discharge assessments. All subsequent patients were allocated to the control group. To determine feasibility of recruitment, our aim was to recruit 24 patients in the specified time frame, with a minimum of 12 patients completing the intervention and discharge assessments. The criterion of 12 patients was specified so that we had a sufficient number of participants to evaluate the safety and tolerability of the intervention.
Intervention: Body Weight–Supported Treadmill Training
A treadmilla and a suspension system (Pneumex Pneu-weightb) were used during the intervention component of this study. The Pneumex Pneuweight is a pneumatic unweighting system that allows for the provision of up to 136kg of BWS. Participants are fitted into a specialized harness, and the harness is secured to the overhead cable. A level of BWS was chosen where patients could feel that some of their body weight was being supported, but did not produce discomfort or alter their gait pattern (range, 0–25kg). Participants self-selected a walking speed at the start of each session that was progressively increased as the patient improved. Participants completed 2 to 3 bouts of walking, and rested either sitting or standing in between, according to preference. Participants were encouraged to try to walk for a longer duration than the previous bout if possible. Participants began with walking bouts of 2 to 5 minutes or less, according to tolerance, up to a maximum total time of 20 minutes. The maximum of 20 minutes was chosen to resemble actual clinical conditions, such that the physiotherapist would not normally walk in the hallway with the participant for more than 20 minutes in one session. Patients in the control group participated in standard physiotherapy sessions, which included walking and bed exercises. To ensure that BWSTT and control groups received the same volume of therapy, the patients participating in BWSTT did so in lieu of their daily walking activities with the physiotherapist. Physiotherapy sessions occurred on most weekdays, excluding holidays.
Primary Feasibility Outcomes
Feasibility outcomes included the number of patients agreeing to participate in treadmill walking; the number of patients who returned for follow-up assessments at 3 months postdis-charge; the number of treadmill sessions completed compared with the number of potential sessions and the number of adverse events of therapy reported. The number of BWSTT sessions completed divided by the number of weekdays spent in rehabilitation activities (not including weekend days or holidays) was determined to get an idea of the number of sessions completed relative to the number of potential sessions. Physiotherapists were instructed to replace at least 3 of 5 walking sessions a week with BWSTT, or a completion of 60% of potential BWSTT sessions. The reasons for missed sessions were documented.
Criteria for Success of Feasibility
The criteria for success related to recruitment and retention were defined as having at least 12 patients agree to participate in treadmill walking, and having 90% of all participants return for follow-up assessments. The feasibility criterion for compliance was 3 out of 5 potential walking sessions, or 60%. If any serious adverse events occurred that were directly attributed to BWSTT, the intervention would not be considered feasible.
Secondary Outcomes
Secondary outcomes measured at baseline, discharge, and at 3-month follow-up included the LEFS, the TUG test, a 2MWT, and the Falls Self-Efficacy Scale. The LEFS measures functional impairment in patients with disorders of one or both lower extremities.17 The TUG test was used as an index of dynamic balance and functional mobility.18 The Falls Self-Efficacy Scale was used as a measure of fall concerns.19 A 2MWT was used to assess ambulatory function. Outcome assessors were not blinded to group allocation. We collected the following patient variables to describe participants: age, cognition (Mini-Mental State Examination), fracture type (sub-capital or intertrochanteric), surgical procedure, type of dwelling before fracture, ambulatory status before fracture, time postfracture, and comorbidities.
Statistical Analysis
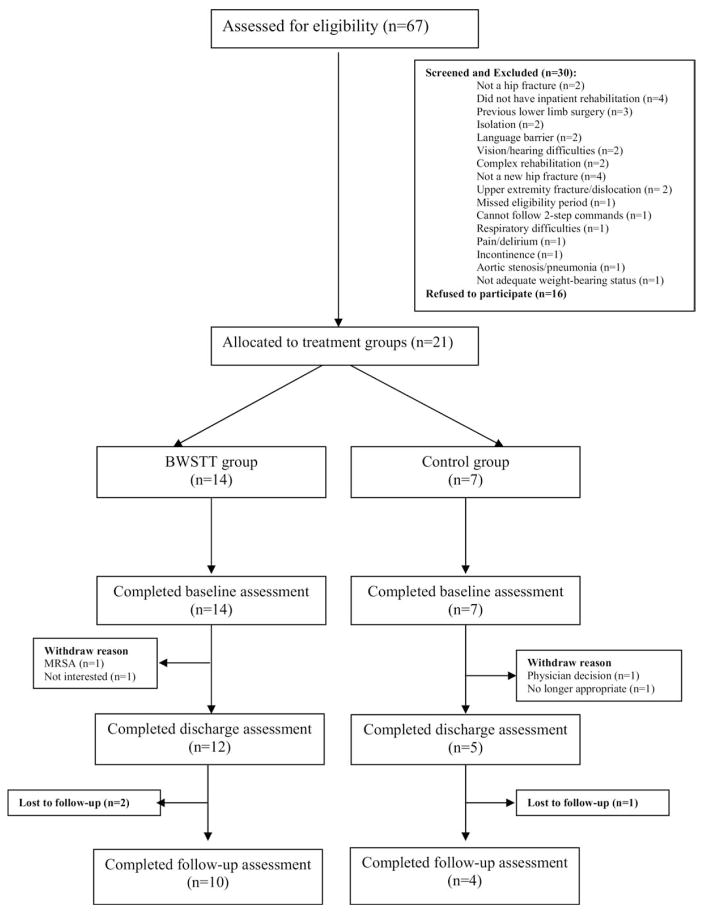
We reported the results in accordance with the TREND criteria.20,21 The follow-up of patients in the study is summarized using a TREND follow-diagram. The characteristics of the participants are reported as mean ±SD for continuous variables and count (percent) for categorical variables. We used multiple imputation to impute missing data (eg, inability to perform test at baseline, loss to follow-up).22 We performed exploratory hypothesis-generating analyses using univariate regression to assess the group (ie, intervention vs control) effect on score changes from baseline to discharge and score changes from baseline to follow-up. The results are reported as estimate of the effect (corresponding 95% confidence interval) and associated P value. The criterion for statistical significance was set at alpha =0.05. All analyses were performed using SAS version 9.1.c
RESULTS
Among 37 potentially eligible patients, 21 (57%) agreed to participate in the pilot study (fig 1). Examples of reasons for not participating included the following: not interested (n=4), did not want to answer questionnaires (n=3), wanted regular rehabilitation (n=1), did not want to walk on a treadmill (n=1), too old to try something new (n=1), concerned about heart problems (n=1), was blind (n=1), did not want to return for 3-month follow-up appointment (n=2), could not communicate well (n=1), and 1 person did not give a reason. Participant characteristics are presented in table 1, and feasibility outcomes are presented in table 2. The remaining patients in the BWSTT group completed a mean ±SD of 8.5±2.8 BWSTT sessions during their rehab stay, corresponding with 60%±20% of weekdays that they participated in rehabilitation activities. Six of the 12 participants had acceptable (60%) compliance with the BWSTT sessions. Reasons for missed BWSTT sessions included the following: experienced a fall that day unrelated to the study and did not want to walk (n=1), leg soreness (n=1), a lag between the day of consent and the first BWSTT session (n=4), or a planned session was missed because of scheduling conflicts and could not be made up before the end of the week (n=2). If the impact of lag time between consent and the first BWSTT session was removed, 10 of 12 participants had acceptable compliance.
Fig 1.
Flow chart of trial participants. Abbreviation: MRSA, methicillin-resistant Staphylococcus aureus.
Table 1.
Participant Characteristics
| Characteristics | BWSTT Group (n=14) | Control Group (n=7) |
|---|---|---|
| Age (y) | 79.9±7.0 | 83.7±8.6 |
| Sex (male/female) | 2/12 | 1/6 |
| MMSE | 26.8±3.0 | 26.4±2.6* |
| No. of days in inpatient rehabilitation | 20±4.8 | 26.1±17.6 |
| Comorbidities (Yes/No) | ||
| 1. Arthritis | 3/11 | 0/7 |
| 2. Stroke | 1/13 | 1/6 |
| 3. Cardiac | 3/11 | 1/6 |
| 4. Hypertension | 9/5 | 4/3 |
| 5. Cancer | 2/12 | 0/7 |
| 6. Diabetes | 1/13 | 0/7 |
| 7. Osteoporosis | 8/6 | 4/3 |
| 8. Renal | 0/14 | 1/6 |
| Assistive devices before fracture (Yes/No) | Valid n=12 6/6 |
Valid n=6 3/3 |
NOTE. Values are mean ±SD or n.
Abbreviation: MMSE, Mini-Mental State Examination.
Valid n=5.
Table 2.
Criteria for Success of Feasibility and Associated Outcomes
| Variable | Criteria for Success of Feasibility | Study Outcome |
|---|---|---|
| Recruitment | 12 patients agree to participate in treadmill walking. | 12 |
| Retention | 90% of all patients return for follow-up assessments. | 14 of 21 (67%) |
| Compliance | Mean compliance is 3 out of 5 potential walking sessions, or 60%. | 60%±20% |
| Adverse events | No serious adverse events directly attributed to BWSTT | 0 |
NOTE. Values are mean ±SD or as otherwise indicated.
The mean ±SD treadmill speed and distance traveled in the first session were 1.1±0.2km/h and 0.1±0.1km, respectively. All participants were able to progressively increase their average treadmill speed and distance traveled during their rehab stay; speed and distance traveled during the last BWSTT session were 1.5±0.4km/h and 0.4±0.2 km, respectively. The mean ±SD BWS provided during treadmill walking was 17.1±4.6kg at the first session and 16.9±6.2kg at the last session. Participants reported the following symptoms during or after BWSTT sessions: shortness of breath (n=2); pain in back (n=2); hip, leg, or knee soreness (n=6); and fatigue (n=3). One patient experienced oxygen desaturation while walking on or off the treadmill.
Estimates of Effect of BWSTT on Secondary Outcomes
The secondary outcome data collected at baseline, discharge, and follow-up are provided in table 3. No statistically significant difference was observed in the change scores between BWSTT and control groups at discharge or at follow-up. Any missing data points were due to participants being unable to complete the assessment or failing to return for follow-up assessment.
Table 3.
Average Scores on Secondary Outcome Measures at Baseline and Discharge, and Comparison of Score Differences Between Baseline and Discharge From Rehabilitation for the BWSTT and Control Groups
| Outcome | Values at Baseline
|
Values at Discharge
|
Values at Follow-up
|
Score Differences Between Baseline and Discharge
|
Score Differences Between Baseline and Follow-up
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BWSTT (n=14) | Control (n=7) | BWSTT (n=12) | Control (n=5) | BWSTT (n=10) | Control (n=4) | Estimate (SE) | 95% CI | P | Estimate (SE) | 95% CI | P | |
| TUG (s) | 73.5±29.1* | 45.6±10.3† | 25.2±7.0 | 20.7±5.0 | 18.0±6.8 | 12.8±0.9 | −26.3 (23.4) | (−72.1, 19.6) | .32 | −13.1 (16.7) | (−45.8, 19.7) | .45 |
| 2MWT (m) | 18.7±18.9‡ | 23.6±15.3 | 70.6±17.3* | 79.4±17.9 | 87.8±20.6§ | 51.2±59.4 | −4.52 (10.0) | (−24.2, 15.1) | .66 | 38.1 (22.3) | (−5.7, 81.8) | .10 |
| LEFS (score/80)|| | 16.6±8.0 | 25.7±16.5 | 35.3±7.5 | 46.4±7.2 | 45.4±9.4 | 48.0±4.4 | 0.08 (4.1) | (−8.0, 8.1) | .98 | 5.8 (5.4) | (−4.8, 16.5) | .30 |
| FSES (score/40)¶ | 22.4±9.2 | 22.0±8.2 | 17.7±6.6 | 12.8±4.4 | 14.4±2.6 | 15.3±5.2 | 2.8 (3.3) | (−3.6, 9.2) | .40 | −2.1 (4.7) | (−11.4, 7.1) | .66 |
NOTE. Values are mean ±SD or as otherwise indicated. Also, the n for each cell represents the value indicated in the column heading unless otherwise indicated. Abbreviations: CI, confidence interval; FSES, Falls Self-Efficacy Scale.
Valid n=8.
Valid n =4.
Valid n=11.
Valid n=9.
A higher score indicates greater lower extremity function.
A higher score indicates poorer falls self-efficacy.
DISCUSSION
Our findings provide important insights into the feasibility of recruitment and retention of patients with hip fracture in the inpatient rehabilitation setting, as well as feasibility information specific to implementing BWSTT as a potential gait-retraining intervention among patients who have had a hip fracture. Recruitment of patients with hip fracture is feasible in the inpatient setting, but it may be necessary to screen at least 3 times as many participants as the sample size requirement dictates. Retention of patients with hip fracture is a challenge and may require rigorous methods to reduce loss to follow-up.
Patients who agreed to participate in BWSTT sessions rarely declined their daily sessions; most missed sessions were attributable to people implementing the intervention rather than patients declining participation. The trial was designed so that the existing physiotherapists would implement the intervention, to test feasibility in the setting in which it would be implemented. Future trials examining the efficacy of BWSTT should include dedicated research personnel for implementing the intervention to enhance adherence to the study protocol.
An important factor influencing the feasibility of rehabilitation research among patients with hip fracture is the complexity of their health status; 20 of the 30 patients excluded from the current study had health-related complications or barriers such as previous lower limb surgery, vision or hearing difficulties, or being in isolation (see fig 1). The average cognition of our participants was quite high, suggesting that they may represent the least frail or cognitively impaired among patients with hip fracture. Future studies of rehabilitation interventions may need to have less rigid inclusion criteria to facilitate the recruitment of adequate participants and to improve the generalizability of the results. Approximately 24% of potential participants declined participation, which is not uncommon among older adults with fractures. For example, of 738 patients with femur, wrist, or humerus fractures treated by orthopedic surgeons and screened to participate in a telephone survey, 25% declined participation.23 Finally, almost 18% of participants in the current study were not willing or able to return for the 3-month follow-up assessment. To ensure adequate follow-up of patients with hip fracture, future studies of inpatient rehabilitation interventions will need rigorous methods for ensuring participant retention, such as having assessments performed in the participant’s home. The absence of evidence for hip fracture rehabilitation strategies in general14 may be due in part to the difficulties observed here in conducting research in this population.
Although the estimates of the effect of BWSTT on some secondary outcomes do not suggest it is more beneficial than hallway walking, these data should be interpreted with caution given the pilot, nonrandomized nature of the study design. We did not test for baseline differences between groups because the small sample size may have limited our ability to detect true differences. The intervention group appeared to have poorer scores on the TUG test, LEFS, and 2MWT at baseline, a younger average age, and a shorter stay in rehabilitation; however, these data should be interpreted with caution given the small sample size and missing data. In fact, approximately 30% of participants could not complete the TUG test or 2MWT at baseline, suggesting that these may not be ideal outcome measures for clinical trials among patients with hip fracture in the acute stages postfracture. One other study by Baker et al24 did not observe differences in gait-related outcomes between patients with hip fracture participating in traditional gait retraining versus treadmill gait retraining. However, among hip arthroplasty patients, BWSTT had a positive effect on muscle strength, gait symmetry, and Harris score, suggesting that treadmill walking has the potential to improve gait-related outcomes among patients who undergo hip surgery.16 Despite these positive observations among hip arthroplasty patients, there were distinct differences between that study by Hesse et al16 and the current one; patients in that study were excluded if older than 75 years or if they were unable to walk with reciprocal crutches, whereas in the current study the average age of BWSTT participants was 79 years, and many had limited mobility at baseline. Further, because the current study was focused primarily on feasibility, the intensity and frequency of the training in the current study were lower and were based on participant tolerance. Finally, the outcomes chosen in the current study, scores on the LEFS, TUG test, and 2MWT, were not comparable to the outcomes measured by Hesse or by Baker, suggesting the need for standardization of post–hip fracture rehabilitation outcomes to enhance the homogeneity across research studies in inpatient rehabilitation.
Study Limitations
It was not possible within the scope of the current pilot study to blind the outcome assessors. There may be channeling bias; we did not randomize participants because we wanted to be sure to recruit a minimum of 12 participants to participate in the intervention within the period that the study was conducted to test the feasibility of intervention implementation. The data presented here provide insight into the responsiveness of the selected outcomes to the BWSTT intervention. Because the control group had a longer length of stay on average, participants in that group may have received more sessions of physiotherapy overall. Only 3 physiotherapy sessions a week included BWSTT. The rehabilitation professionals working on the project revealed that it was easier to implement hallway walking than BWSTT because of the time required to put on the harness. However, they also indicated that for some of the patients, such as obese patients or those with a great degree of pain during weight-bearing, BWSTT was useful because a proportion of body weight could be unloaded.
CONCLUSIONS
In summary, the current study provides preliminary evidence that it may be feasible to implement supported treadmill walking for patients with hip fracture in an inpatient rehabilitation setting. The current study also provides important feasibility information for future studies of interventions for patients with hip fracture in inpatient rehabilitation with respect to the screening-to-recruitment ratio, the recruitment challenges, and the magnitude of loss to follow-up after discharge. Although evaluation of the efficacy of hip fracture rehabilitation interventions is needed, the challenges demonstrated here illustrate the difficulties of conducting rehabilitation research in this population. To optimize future research of hip fracture rehabilitation strategies, trials with sufficient sample size and rigorous methods for recruitment and retention are needed, as well as standardization of outcomes to facilitate comparisons across studies.
Acknowledgments
Supported by the Hamilton Health Sciences New Investigator Fund (grant no. NIF-05055).
We thank Kevin Letcher, MD, FRCPC, for assisting with recruitment of patients and consulting with the team during study planning and daily operations; Donna Auld, BHSc.PT, Richard Olaveson, BHSc.PT, and the rehabilitation team at the Henderson Hospital for their work in implementing the BWSTT and outcome assessment; Ruth McCallum, MSc KIN, Madeline Nixon, BSc KIN, and Janet Prichard, BSc, for study coordination and outcome assessment; and Jinhui Ma, MSc, for assistance in analysis of study results.
List of Abbreviations
- BWS
body weight support
- BWSTT
body weight–supported treadmill training
- LEFS
Lower Extremity Functional Scale
- 2MWT
2-minute walk test
- TREND
Transparent Reporting of Evaluations with Nonrandomized Designs
- TUG
Timed Up & Go
Footnotes
Woodway, W229 N591 Foster Ct, Waukesha, WI 53186.
Pneumex Inc, 2605 North Boyer Ave, Sandpoint, ID 83864.
SAS Institute Inc, 100 SES Campus Dr, Cary, NC 27513-2414.
Clinical trial registration no.: NCT00197496.
Reprints are not available from the author.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
References
- 1.von Friesendorff M, Besjakov J, Akesson K. Long-term survival and fracture risk after hip fracture: a 22-year follow-up in women. J Bone Miner Res. 2008;23:1832–41. doi: 10.1359/jbmr.080606. [DOI] [PubMed] [Google Scholar]
- 2.Papaioannou A, Wiktorowicz ME, Adachi JD, et al. Mortality, independence in living and re-fracture, one year following hip fracture in Canadians. J Soc Obstet Gynaecol Can. 2000;22:591–7. [Google Scholar]
- 3.Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E. Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int. 2001;12:271–8. doi: 10.1007/s001980170116. [DOI] [PubMed] [Google Scholar]
- 4.Adachi JD, Loannidis G, Berger C, et al. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int. 2001;12:903–8. doi: 10.1007/s001980170017. [DOI] [PubMed] [Google Scholar]
- 5.Petrella RJ, Payne M, Myers A, Overend T, Chesworth B. Physical function and fear of falling after hip fracture rehabilitation in the elderly. Am J Phys Med Rehabil. 2000;79:154–60. doi: 10.1097/00002060-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Borgquist L, Ceder L, Thorngren KG. Function and social status 10 years after hip fracture: prospective follow-up of 103 patients. Acta Orthop Scand. 1990;61:404–10. doi: 10.3109/17453679008993550. [DOI] [PubMed] [Google Scholar]
- 7.Fitzgerald JF, Dittus RS. Institutionalized patients with hip fractures: characteristics associated with returning to community dwelling. J Gen Intern Med. 1990;5:298–303. doi: 10.1007/BF02600395. [DOI] [PubMed] [Google Scholar]
- 8.Lamb SE, Morse RE, Evans JG. Mobility after proximal femoral fracture: the relevance of leg extensor power, postural sway and other factors. Age Ageing. 1995;24:308–14. doi: 10.1093/ageing/24.4.308. [DOI] [PubMed] [Google Scholar]
- 9.Madsen OR, Lauridsen UB, Sorensen OH. Quadriceps strength in women with a previous hip fracture: relationships to physical ability and bone mass. Scand J Rehabil Med. 2000;32:37–40. doi: 10.1080/003655000750045721. [DOI] [PubMed] [Google Scholar]
- 10.Jones GR, Miller TA, Petrella RJ. Evaluation of rehabilitation outcomes in older patients with hip fractures. Am J Phys Med Rehabil. 2002;81:489–97. doi: 10.1097/00002060-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Eastwood EA, Magaziner J, Wang J, et al. Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc. 2002;50:1240–9. doi: 10.1046/j.1532-5415.2002.50311.x. [DOI] [PubMed] [Google Scholar]
- 12.Haentjens P, Autier P, Barette M, Boonen S. Predictors of functional outcome following hip fracture in elderly women: a one-year prospective cohort study. Injury. 2005;36:842–50. doi: 10.1016/j.injury.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55:M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 14.Handoll HH, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database Syst Rev. 2007;(1):CD001704. doi: 10.1002/14651858.CD001704.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Visintin M, Barbeau H, Korner-Bitensky N, Mayo NE. A new approach to retrain gait in stroke patients through body weight support and treadmill stimulation. Stroke. 1998;29:1122–8. doi: 10.1161/01.str.29.6.1122. [DOI] [PubMed] [Google Scholar]
- 16.Hesse S, Werner C, Seibel H, et al. Treadmill training with partial body-weight support after total hip arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil. 2003;84:1767–73. doi: 10.1016/s0003-9993(03)00434-9. [DOI] [PubMed] [Google Scholar]
- 17.Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network Phys Ther. 1999;79:371–83. [PubMed] [Google Scholar]
- 18.Podsiadlo D, Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 19.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:239–43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 20.Armstrong R, Waters E, Moore L, et al. Improving the reporting of public health intervention research: advancing TREND and CONSORT. J Public Health (Oxf) 2008;30:103–9. doi: 10.1093/pubmed/fdm082. [DOI] [PubMed] [Google Scholar]
- 21.Des Jarlais DC, Lyles C, Crepaz N the TREND Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94:361–6. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Refaat M. Data preparation for data mining using SAS. New York: Morgan Kaufmann; 2007. [Google Scholar]
- 23.Giangregorio L, Papaioannou A, Thabane L, et al. Do patients perceive a link between a fragility fracture and osteoporosis? BMC Musculoskelet Disord. 2008;9:38. doi: 10.1186/1471-2474-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baker PA, Evans OM, Lee C. Treadmill gait retraining following fractured neck-of-femur. Arch Phys Med Rehabil. 1991;72:649–52. [PubMed] [Google Scholar]