Abstract
The initial goal of this study was to investigate alterations in adenosine A2A receptor (A2AR) density or function in a rat model of Huntington disease (HD) with reported insensitivity to an A2AR antagonist. Unsuspected negative results led to the hypothesis of a low striatal adenosine tone and to the search for the mechanisms involved. Extracellular striatal concentrations of adenosine were measured with in vivo microdialysis in two rodent models of early neuropathological stages of HD disease, the Tg51 rat and the zQ175 knock-in mouse. In view of the crucial role of the equilibrative nucleoside transporter (ENT1) in determining extracellular content of adenosine, the binding properties of the ENT1 inhibitor [3H]-S-(4-Nitrobenzyl)-6-thioinosine were evaluated in zQ175 mice and the differential expression and differential coexpression patterns of the ENT1 gene (SLC29A1) were analyzed in a large human cohort of HD disease and controls. Extracellular striatal levels of adenosine were significantly lower in both animal models as compared with control littermates and striatal ENT1 binding sites were significantly upregulated in zQ175 mice. ENT1 transcript was significantly upregulated in HD disease patients at an early neuropathological severity stage, but not those with a higher severity stage, relative to non-demented controls. ENT1 transcript was differentially coexpressed (gained correlations) with several other genes in HD disease subjects compared to the control group. The present study demonstrates that ENT1 and adenosine constitute biomarkers of the initial stages of neurodegeneration in HD disease and also predicts that ENT1 could constitute a new therapeutic target to delay the progression of the disease.
Keywords: adenosine, ENT1, A2A receptor, Huntington Disease
Introduction
Huntington disease (HD) is an inherited neurodegenerative disorder generally affecting young adults and characterized by progressive chorea, cognitive impairments and emotional disturbances. HD is caused by a single dominant gene mutation that is an expanded CGA repeat in the huntingtin (HTT) gene (The Huntington Disease Collaborative Research Group, 1993). The pathological hallmark of the disease is the atrophy of the striatum (Vonsattel et al., 1985; Ferrante et al., 1987) with considerable loss of projecting medium spiny neurons, but neurodegeneration in the cortex and other brain areas is also observed (Vonsattel et al., 1985). Among the two subtypes of medium spiny neurons, the GABAergic enkephalin-containing neurons, which selectively express dopamine D2 receptors (D2R) and adenosine A2A receptors (A2AR) (Ferré et al., 1993; Quiroz et al., 2009), are the most vulnerable (Mitchell et al., 1999). In fact, previous studies found a preferential decrease in the striatal A2AR and D2R versus dopamine D1 receptor density in the early stages of the disease (Glass et al., 2000). But the decrease in the density of A2AR seems to involve a downregulation independent of neurodegeneration, related to alterations in the normal regulation of transcription of the A2AR gene (Chiang et al., 2005; Villar-Menéndez et al., 2013). A2AR is usually shown to be downregulated in early stages of neuropathological development in rodent models of HD and several preclinical and clinical studies have suggested that the decrease in A2AR density or its tonic activation could be involved in the pathogenesis of HD (reviewed in Lee and Chern, 2014). In fact, tonic activation of A2AR is necessary for the action of brain-derived neurotrophic factor (BDNF; Diogenes et al., 2004; Rodrigues et al., 2014), which is greatly impaired during HD progression (Zuccato et al., 2001). Finally, genetic and epidemiological studies also support the involvement of A2AR. Several polymorphisms in the A2AR gene have been associated to a reduced age of onset of the disease (Dhaenens et al. 2009; Taherzadeh-Fard et al., 2010) and, in a recent study, caffeine (non-selective adenosine receptor antagonist) intake (more than 190 mg/day) was significantly associated with a reduced age of onset of HD by about 4 years (Simonin et al., 2013). Apart from these findings involving specifically A2AR, diverse alterations in other adenosine receptor subtypes and in adenosine homeostasis have also been documented in animal models of HD (Lee and Chern, 2014).
We previously reported that the A2AR antagonist KW-6002 did not induce locomotor activation at early neuropathological stages of HD phenotypic development in the transgenic rat expressing a fragment of the HTT gene with 51 CAG repeats (Tg51) (von Horsten et al., 2003), which was interpreted as a possible alteration in A2AR density or function (Orrú et al., 2011). The initial aim of the present study was to investigate the type of A2AR alteration involved. Unexpectedly, an A2AR agonist produced similar psychomotor depressant effects in Tg51 rats as compared to wild-type (WT) littermate controls. Furthermore, radioligand-binding experiments would not show any significant difference in the properties of striatal A2AR antagonist binding in Tg51 rats as compared to controls. The possibility of a low striatal adenosine tone was therefore addressed. This was demonstrated with in vivo microdialysis experiments both in Tg51 rats and in a more recently introduced animal model of HD, the zQ175 knock-in mouse, which expresses a HTT carrying 188 CAG repeats (Heikkinen et al., 2012; Menalled et al., 2012).
We then investigated the possibility of changes in a crucial player in the major route to uptake extracellular adenosine into the cells, the equilibrative nucleoside transporter ENT1, a protein mainly expressed by astroglial cells. The present study demonstrates that, in fact, ENT1 is not only upregulated in the striatum of zQ175 knock-in mice, but its gen (SLC29A1) is also significantly overexpressed in the brain of patients with initial neuropathological stages of HD and differentially coexpressed in HD patients as compared to the control group.
Materials and Methods
Animals and drugs
Transgenic HD rats expressing a fragment of 727 amino-acids of HTT with 51 CAG repeats (Tg51; initially provided by the Department of Medical Genetics, University of Tubingen, Germany, and bred in our Institute (von Horsten et al., 2003), and knock-in HD mice with constitutive HTT carrying 188 CAG repeats (zQ175) provided by CHDI Foundation; Los Angeles, CA; (Heikkinen et al., 2012; Menalled et al., 2012) were used. For Tg51 rats, 3- and 12-month old animals from three genotypes (homozygous, heterozygous and wild-type littermates) were used. For zQ175 mice, 12-month old animals from two genotypes (heterozygous and wild-type littermates) were used. The previously reported neuropathological changes of 12-month old hetero- and homozygous Tg51 rats (Kántor et al., 2006) and 12-month old heterozygous zQ175 mice (Heikkinen et al., 2012) correspond to grade 2 in the Vonsattel neuropathological severity score in patients with HD (see below). Animals were housed in pairs per cage and kept on a 12/12-dark/light cycle with food and water available ad libitum. All animals used in the study were maintained in accordance with the guidelines of National Institutes of Health animal care and the animal research approved by the NIDA IRP Animal Care and Use Committee (protocol #09-BNRB-73). The A2AR agonist CGS-21680 was kindly provided by CHDI Foundation.
Locomotor activity
Locomotor activity in rats was measured in open field soundproof chambers (50 × 50 cm, Med Associates Inc., VT). The rats were not habituated to the experimental cages and recording of the locomotor activity started immediately after administration of the A2AR agonist CGS-21680, by placing the animals in the box. Locomotion was measured by counting the number of breaks in the infrared beams of the chamber during consecutive periods of min. Results were analyzed as the average of 10-min period transformed (square root) counts during the 90-min period of observation. All the animals were tested only once.
In vivo microdialysis
Rats and mice were anesthetized with 3 ml/kg of Equithesin (4.44 g of chloral hydrate, 0.972 g of Na pentobarbital, 2.124 g of MgSO4, 44.4 ml of propylene glycol, 12 ml of ethanol and distilled H2O up to 100 ml of final solution; NIDA Pharmacy, Baltimore, MD). A concentric microdialysis probe with 2-mm long dialysis membranes (Eicom Corp, Tokyo, Japan) was implanted into the dorsolateral striatum of rats (coordinates were 0.0 mm anterior, 4.5 mm lateral and 7.0 mm ventral from bregma) or mice (coordinates were 1.0 mm anterior, 1.5 mm lateral and 4.5 ventral from bregma). In both cases, the probe was fixed to the skull with successive layers of glass ionomer cement (CX Plus, Shofu Dental, Japan). The in vivo microdialysis experiments were performed on freely moving rats and mice 24 h after probe implantation. An artificial cerebrospinal solution (in mM, 144 NaCl, 4.8 KCl, 1.7 CaCl2, and 1.2 MgCl2) was pumped through the microdialysis probe at a constant rate of 1 µl/min. After a washout period of 90 min, dialysate samples were collected at 30-min intervals and immediately frozen at −80°C until adenosine levels were determined. The adenosine content in the samples was analyzed by HPLC coupled to a fluorescence detector (RF-10A XL; Shimadzu Scientific Instruments, Columbia, MD) as previously reported (Melani et al., 1999). Adenosine was detected as a fluorescent derivative (1,N6-ethenoadenosine) following derivatization with chloroacetaldehyde. Zinc acetate (0.14 µl, 0.1 M) was added to each µl sample. The solution was transferred into glass vials, where 0.18 µl of chloroacetaldehyde (4.5%) was added for each ml of solution obtained. This solution was kept at 100° C for 20 min. Adenosine was identified by its disappearance after incubation of the sample with 1U of adenosine deaminase at room temperature for 1 min. The minimum detectable amount of adenosine was 0.01 pmol. Standard solutions were arranged with Tris/HCl pH 7.4 and subjected to an identical procedure as that one of samples. The in vitro recovery rate of adenosine was 9.84 ± 0.81%. The concentration values reported were not corrected for recovery. Mean of adenosine concentrations of eight microdialysis samples obtained from each animal were calculated.
Radioligand-binding experiments
Striatal membrane preparations from Tg51 rats or zQ175 mice were used to analyze binding of the A2AR antagonist [3H] 4-(2-[7-Amino-2-(2-furyl)[1,2,4]triazolo[2,3-a][1,3,5]triazin-5-ylamino]ethyl)phenol ([3H] ZM241385; American Radiolabelled Chemicals, St. Louis, MO) and the ENT1 inhibitor [3H]-S-(4-Nitrobenzyl)-6-thioinosine ([3H]NBTI; PerkinElmer, Boston, MA) (Choi et al., 2004). Animals were deeply anesthetized with Equithesin (see in vivo microdialysis subsection) and euthanized by decapitation. The brains were quickly removed on ice, the striatum dissected out and homogenized in 50 mM Tris-HCl buffer (pH 7.4) containing a protease inhibitor cocktail (1:1000, Sigma, US). Membranes were obtained by centrifugation at 100,000 g (45 min, 4°C) and washed 2 times in the same conditions. Protein was quantified by the bicinchoninic acid method (Pierce, Rockford, IL). Pellets were resuspended and membrane suspensions (0.2 mg of protein/ml) were incubated in 50 mM Tris-HCl (pH 7.4) containing 2 I.U./ml of adenosine deaminase (Roche, Basel, Switzerland) and increasing concentrations of the radiolabelled adenosine A2AR antagonist or the ENT1 inhibitor. In both cases, free and membrane-bound ligand were separated by rapid filtration on 500 µl aliquots in a 96-well plate harvester (Brandel, Gaithersburg, MD) and washed with 2 ml of ice-cold Tris-HCl. Non-specific binding was determined in the presence of 10 mM ZM241385 or 10 mM non-labeled NBTI. Filter plates were incubated with Microscint-20 (65 µl/well) scintillation liquid (PerkinElmer), incubated overnight at RT and radioactivity counts were determined in a MicroBeta2 plate counter (PerkinElmer) with an efficiency of 41%. Saturation curves were analyzed by non-linear regression using Prism 4 (GraphPad Software, La Jolla, CA).
Analysis of transcript levels of ENT1 in postmortem human prefrontal cortex
The relative transcript level (differential expression, DE) of the ENT1 gene (SLC29A1) in the postmortem prefrontal cortex of 157 non-HD subjects and 127 HD patients were derived from gene expression data collected in a previous study (Narayanan et al., 2014). The expression data was adjusted for the same covariates (such as age and gender) as in the previous study using the same method, robust linear regression (rlm) except for one difference: Instead of fitting an rlm model of each gene expression data separately for the AD, HD, and control groups using the covariates as in the previous study, we fit an rlm model of each gene expression data once using all AD, HD, and control expression values to ensure that the DE signal is not lost in the adjustment. Two different probes (probe 1: 5’ -GCA CCC TGT ACA GTT GCC ACG TTA CTG CCT TTT TTA AAA ATA TAT TTG ACAG AAA CCA GG- 3’; probe 2: 5’-TTG ACA GAA ACC AGG TGC CTT CAG AGG CTC TCT GAT TTA AAT AAA CCT TTC TTG TTT- 3’), which hybridize to the 3’ untranslated region of the human ENT1 gene, were utilized in the microarray chip to detect the ENT1 transcript. Of note, probe 2 also maps to another location in chromosome 13, based on a default “human BLAT search” available at http://moma.ki.au.dk/genome-mirror/cgi-bin/hgBlat. ENT1 expression levels in the postmortem frontal cortex were studied in both control and HD groups and further grouped by their Vonsattel neuropathologicalal severity score, which consists of five stages of progression of striatal abnormalities, which correlate with the degree of clinical symptoms: grade 0, clinical evidence but no pathological abnormalities; grade 1, minimal microscopic abnormalities (neuronal loss and astrocytosis) with no macroscopic abnormalities (reduced striatal volume, atrophy); grade 2, more pronounced microscopic abnormalities and minimal macroscopic abnormalities; grade 3 and 4, severe and very severe microscopic and macroscopic abnormalities (Vonsattel et al., 1985).
Differential coexpression analysis
Differential coexpression (DC) was tested using a self-contained test (Narayanan et al., 2014), which inspects if a gene of interest (SLC29A1 in our case) shows DC patterns between HD versus control samples on their own right, without reference to any other genes in the genome. This is done by collecting all partner genes correlated to a “hub” gene of interest (like SLC29A1) in either the HD or controls group, and testing if the median change in correlation strength between the hub gene and the partner genes are beyond sampling noise estimated from bootstrap resampling. Specifically, to compute the bootstrap-based p-value, we bootstrap resample the HD dataset 1000 times and Control dataset 1000 times and compute how often the median change in correlation between a hub gene and all other partner genes (specifically difference of Fisher-Z transformed Spearman correlation coefficient in HD and Control groups) happen in the resampled datasets. This test served as an additional confirmation of the SLC29A1 hub seen in the overall HD versus control DC network controlled at FDR 1%.
Results
Unaltered A2AR agonist-mediated psychomotor depression and A2AR antagonist binding properties in Tg51 rats
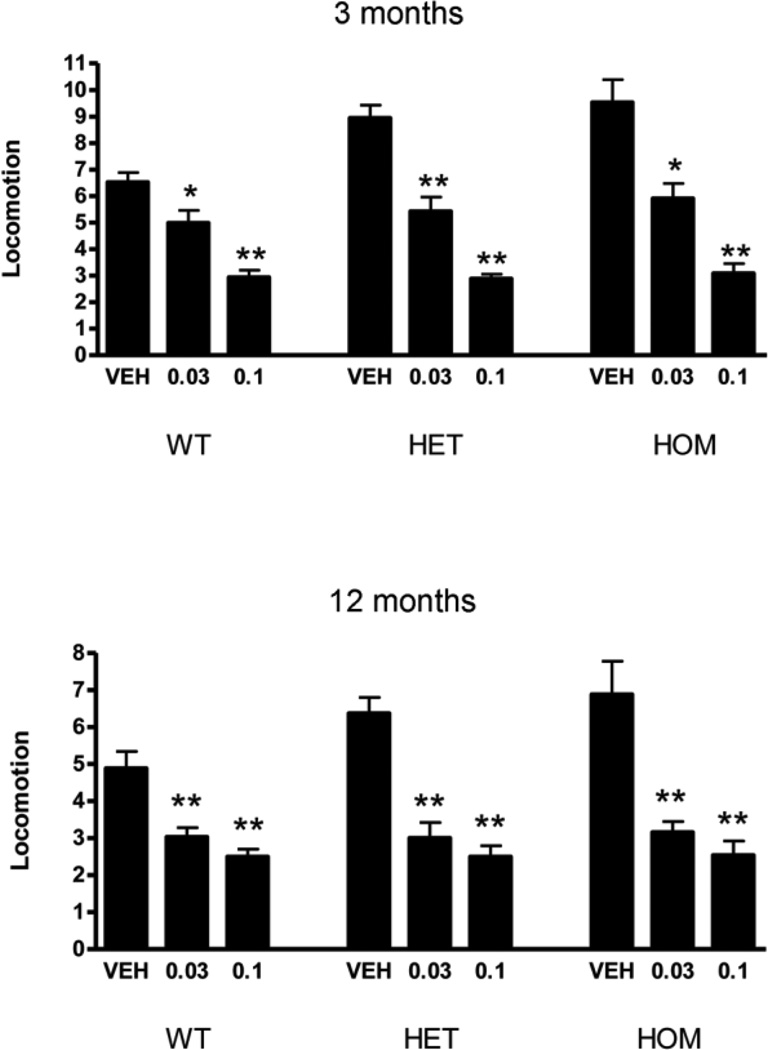
Previous results of experiments in Tg51 rats showed the inability of the selective A2AR antagonist KW-6002 to increase locomotor activity at 6 and 12, but not at 3 months of age (Orrú et al., 2011). These results were interpreted as an alteration in the density (decrease) or function of striatal A2AR at still early neuropathological stages of this HD animal model. In that case we would also expect differences in the psychomotor depressant effects of an A2AR agonist, such as CGS-21680. In fact, both the psychomotor activating effects of KW-6002 and depressant effects of CGS-21680 depend on the integrity of the striatal A2AR, as they are eliminated in A2AR KO mice (Chen et al., 2001; Yu et al., 2008). CGS 21680 (0.03 and 0.1 mg/kg, i.p.) produced a depressant effect in 3- and 12-month old Tg51, both for heterozygous (HET) and homozygous (HOM), as compared to WT littermates (Fig. 1). As shown in Fig. 1, there was an apparent increase in locomotor activity with vehicle administration in Tg51 rats as compared with WT. Nevertheless, both for 3-month and 12-month old rats, a bifactorial ANOVA showed a very significant effect of CGS-21680 (p<0.0001 in both cases) without significant genotype effect or CGS-21680-genotype interaction. Furthermore, comparison of the binding properties of the A2AR antagonist [3H]ZM-241385 in striatal preparations of 3- and 12-month old HET and HOM Tg51 and WT controls did not show any significant differences in affinity (KD) or number of binding sites (Bmax) based on ANOVA followed by Dunnett’s post hoc test (Table 1). These behavioral and biochemical results indicated unimpaired striatal A2AR density or function in Tg51 rats.
Figure 1.
Locomotor depression induced by the A2AR agonist CGS-21680 (0.03 and 0.1 mg/kg, i.p.) in homozygous (HOM) and heterozygous (HET) Tg51 rats and wild-type littermates WT measured at 3 and 12 months of age. Values represent means ± S.E.M. (n = 6–8 per group) of the average of 10-min period transformed counts (square root) during the 90-min period of observation. * and **: significantly different compared to vehicle-treated rats (VEH); p<0.05 and p<0.01, respectively; Bifactorial ANOVA, followed by one-way ANOVA with Dunnett’s post hoc test.
Table 1.
Binding of the A2AR ligand [3H]ZM-241385 to striatal membranes of 3-month and 12-month old Tg51 rats measured in wild-type (WT) heterozygous (HET) and homozygous (HOM) animals. Results represent means ± S.E.M. (n = 6–8 per group).
| WT | HET | HOM | ||||
|---|---|---|---|---|---|---|
| 3 months | 12 months | 3 months | 12 months | 3 months | 12 months | |
| KD (nM) | 2.3 ± 0.5 | 3.1 ± 0.3 | 2.5 ± 0.2 | 3.0 ± 0.3 | 3.0 ± 0.3 | 4.8 ± 0.9 |
| Bmax (pmol/mg prot) |
1.8 ± 0.2 | 1.1 ± 0.2 | 1.9 ± 0.2 | 1.1 ± 0.2 | 1.9 ± 0.3 | 0.8 ± 0.2 |
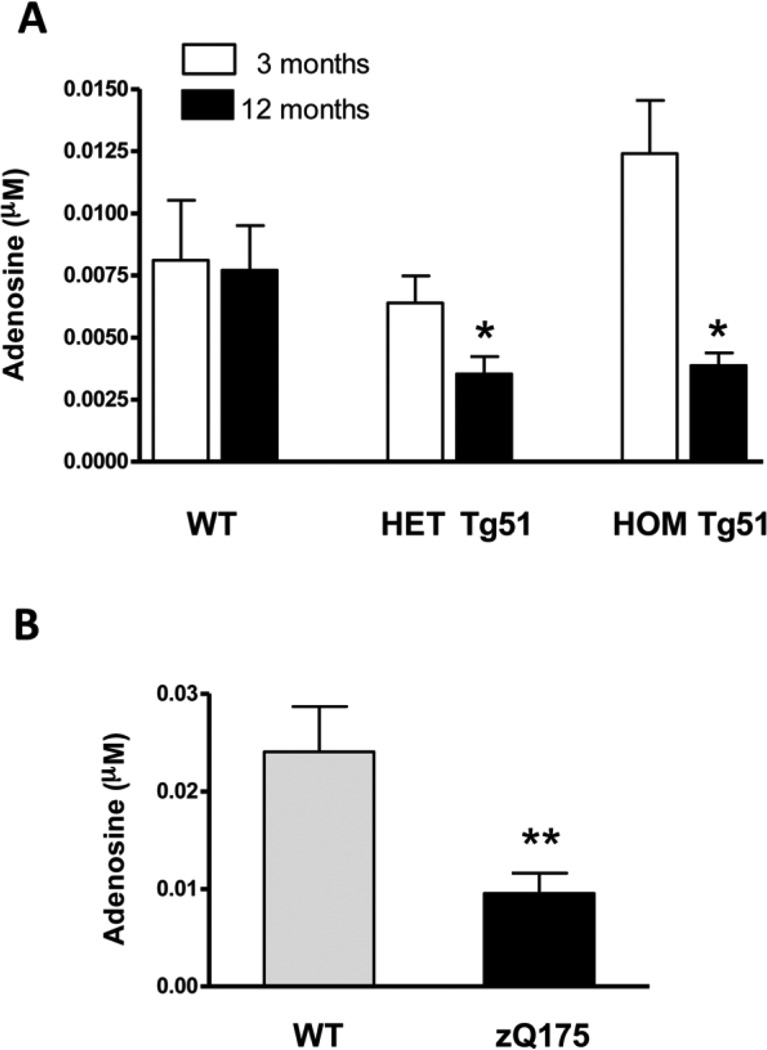
Low striatal extracellular levels of adenosine in Tg51 rats and zQ175 mice
A low adenosine tone could explain the existence of an impairment of the pharmacological effects of an A2AR antagonist without a concomitant impairment of the A2AR density or function. In fact, both in HOM and HET 12-month old Tg51 rats, the striatal levels of adenosine, measured by in vivo microdialysis, were significantly lower as compared with WT littermates (Fig. 2A). No significant differences were observed between the different genotype groups at 3 months of age. We then tested for striatal adenosine levels in the zQ175 knock-in mouse, recently developed by Menalled and colleagues in an attempt to have the HTT gene in a context that causes a phenotype more closely mimicking HD in humans (Menalled et al., 2012). In fact, behavioral, electrophysiological, histological, biochemical and imaging data indicate that the progressive phenotypes of both HOM and HET zQ175 mice up to 12 months of age recapitulate better the early phenotypic stages of HD than previous animal models (Menalled et a., 2012; Heikkinen et al., 2012; Peng et al., 2016). HET zqQ175 mice were chosen for the present study since they provide a more insidious and less penetrating genotype than HOM (Peng et al., 2016) and similar neuropathological changes than the 12-month old hetero- and homozygous Tg51 rats (Kántor et al., 2006; Heikkinen et al., 2012), which correspond to grade 2 in the Vonsattel neuropathological severity score in patients with HD (see above).The results confirmed those obtained with Tg51 rats and zQ175 mice showed striatal extracellular levels of adenosine that were significantly lower than for WT littermates (Fig. 2B).
Figure 2.
Basal striatal levels of adenosine as measured with in vivo microdialysis in homozygous (HOM) and heterozygous (HET) Tg51 rats measured at 3 and 12 months of age (A) and in heterozygous 12 month-old zQ175 knock-in mice (B) at 12 months of age as compared with wild-type littermates (WT). Results are expressed as means ± S.E.M. (n = 6–8 per group) of the concentration of adenosine (µM). * and **: significantly different compared to WT; p<0.05 and p<0.01, respectively; ANOVA with Dunnett’s post hoc test or non-paired Student’s t test.
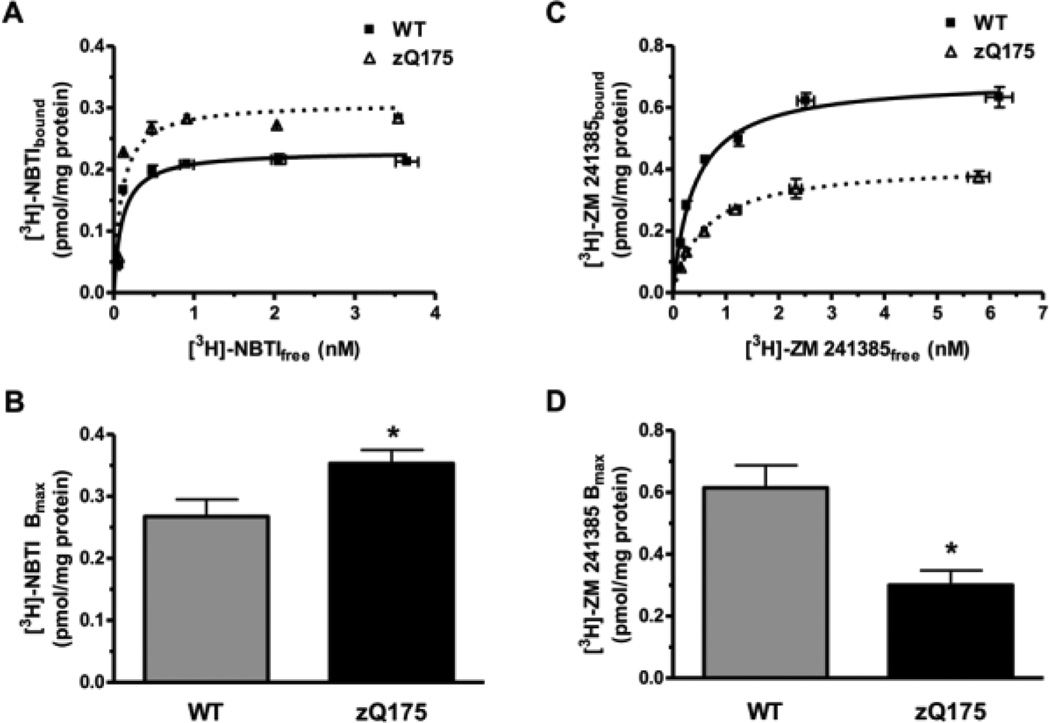
High striatal density of ENT1 and low striatal density of A2AR antagonist binding sites in zQ175 mice
In view of the crucial role of ENT1 in determining the extracellular content of adenosine in the brain, we investigated the possibility of an ENT1 upregulation in the striatum of zQ175 mice, performing saturation experiments of the ENT1 inhibitor [3H]NBTI. In fact, the striatal binding of the ENT1 inhibitor [3H]NBTI was increased in zQ175 mice as compared to WT littermates (Figs. 3A and 3B), with a significant increase in the number of binding sites (Bmax: 0.35 ± 0.02 pmol/mg protein versus 0.27 ± 0.03 pmol/mg of protein) and no significant change in affinity (KD: 0.11 ± 0.03 versus 0.11 ± 0.01 nM). The striatal density of A2AR was also analyzed with saturation experiments with [3H]ZM-241385. The binding of the A2AR antagonist was decreased in zQ175 mice as compared to WT littermates (Figs. 3C and 3D), with a significant decrease in the number of binding sites (Bmax: 0.30 ± 0.04 pmol/mg protein versus 0.62 ± 0.07 pmol/mg of protein) and no significant change in affinity (KD: 0.50 ± 0.08 versus 0.49 ± 0.08 nM).
Figure 3.
Binding of ENT1 and A2AR ligands in the striatum of zQ175 mice wild-type littermates (WT). A. Representative saturation curves of the ENT1 ligand [3H]NBTI. B. Bmax values of [3H]NBTI binding; results are expressed as means ± S.E.M. (n = 8–10 per group). C. Representative saturation curves of the A2AR ligand [3H]ZM-241385. D. Bmax values of [3H]ZM-241385 binding; results are expressed as means ± S.E.M. (n = 5 per group). *: significantly different compared to WT; p< 0.01; unpaired Student’s t test.
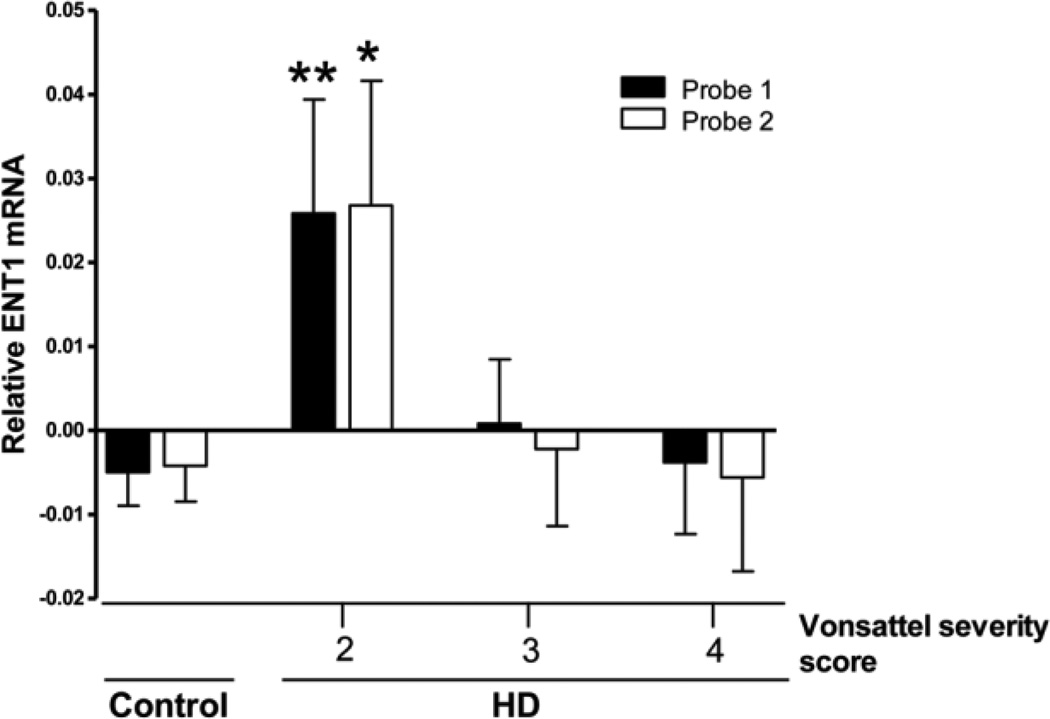
Increased expression of the ENT1 transcript in HD
If zQ175 mice do represent a valid model of the HD, we could expect an upregulation of ENT1 in postmortem brain tissue from patients with less severe neuropathological stages of HD. Analysis of the relative level of ENT1 transcript (SLC29A1) in the postmortem prefrontal cortex of 157 non-HD subjects and 127 HD patients with different neuropathological severity of the disease was performed using two different probes, as detailed in the Methods section. Data analysis revealed that HD patients with Vonsattel severity score 2, but not those with higher severity stage 3 or 4, expressed significantly higher levels of ENT1 transcript than non-HD subjects (Fig. 4).
Figure 4.
ENT1 transcript expression in HD patients. The relative expression of the ENT1 gene (SLC29A1) from the prefrontal cortex of 157 non-demented controls and 127 HD patients derived from gene expression data of a previous study and two different probes were used (see Methods). Disease severity was determined based on Vonsattel staging as mild/moderate (Stage 2; n = 38) or severe (Stage 3; n = 59; Stage 4, n = 30). Values represent means ± S.E.M.; * and **: significantly different as compared to controls; * and **: significantly different compared to WT; p<0.05 and p<0.01, respectively; ANOVA with Dunnett’s post hoc test.
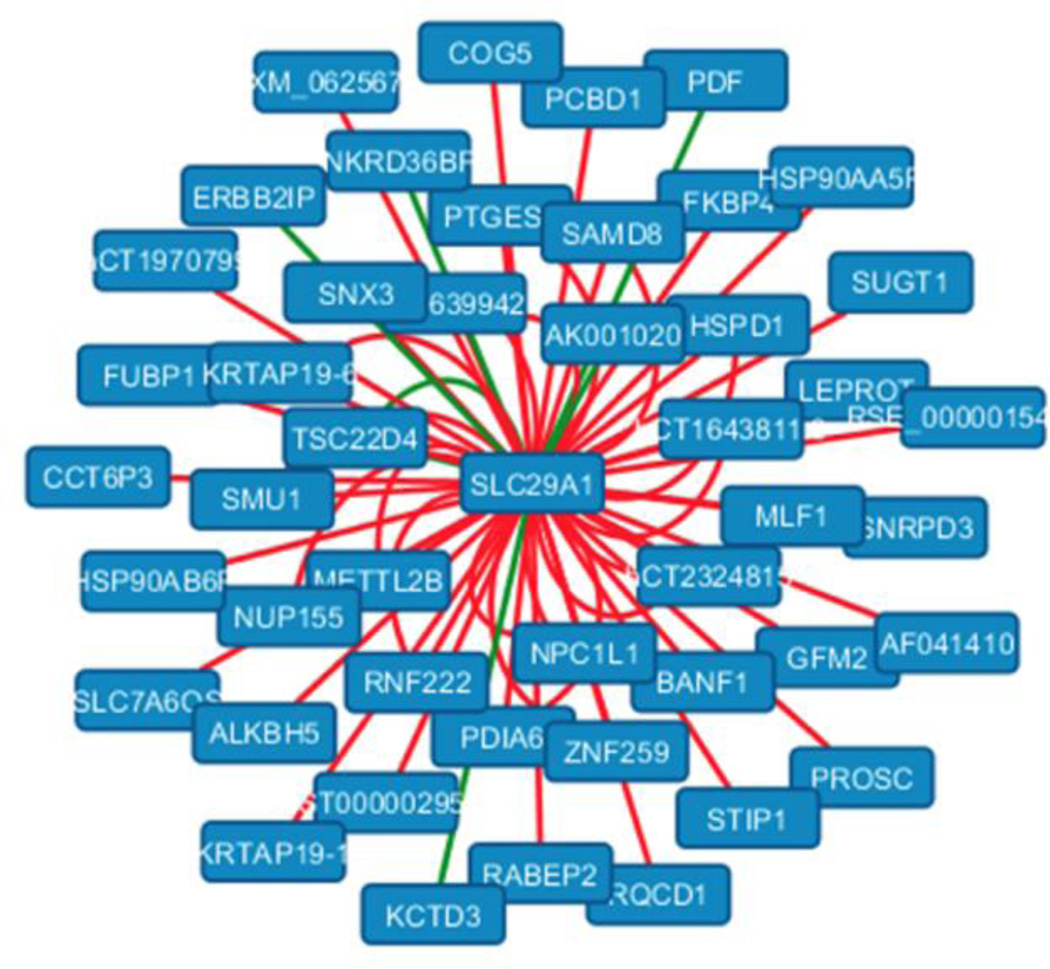
In addition to comparing the average expression level of SLC29A1 in the HD versus the control group (in differential expression analysis), we also inspected if the coordinate regulation of SLC29A1 with other genes in the genome were disrupted (gained/lost) in the HD group relative to controls. Several recent studies have utilized DC analysis to identify disease-dysregulated genes that are complementary to signature genes found in a DE analysis (Narayanan et al., 2011), since the correlation among two genes across individuals could be gained or lost in the disease group relative to controls without any significant change in their mean expression level across the two groups. We took the network of previously published DC relations identified at FDR 1% in this cohort of HD versus control individuals and extracted those DC relations that involved SLC29A1. This subnetwork revealed that the gene for ENT1 (SLC29A1) exhibited differential correlations (mostly gain of correlations) to at least 60 other gene reporters in HD patients relative to controls suggesting that it serves as a hub of HD-induced dysregulation (Fig. 5; P<1/1000 in bootstrap-based test; see Methods). This hub-like DC pattern appears to be reflective of the drastic rewiring of the entire gene-gene coexpression network observed when comparing HD versus control groups (Narayanan et al., 2014). The genes that SCL29A1 was differentially correlated with between the HD versus controls groups were enriched for protein folding annotations at p<0.05 (Bonferroni-corrected p value computed through PANTHER over-representation test, available at pantherdb.org and released 2016-07-15, for GO-Slim Biological Process terms in PANTHER version 11.0, released 2016-07-15). Amongst these DC partner genes of SLC29A1, the ones annotated with protein folding or chaperone related functions included PTGES3, HSPD1, HSP90AA5P, FKBP4, SUGT1, and STIP1. Importantly, the role of autophagy mediated by chaperones such as Hsp90 proteins in the clearance of Htt has been previously described (Qi and Zhang, 2014).
Figure 5.
Altered coexpression pattern of the ENT1 transcript SLC29A1 in HD patients versus controls. The graph shows all genes differentially coexpressed with SLC29A1 in HD versus controls individuals, as chosen from the HD versus controls DC network identified at FDR 1% in a previously published study (see text). SLC29A1 acts as a hub that is dysregulated with many other genes; red edges indicate gain of correlation between the gene pair in disease, and green edges are loss of correlation.
Discussion
The role of adenosine receptors in the pathogenesis of HD has been the focus of intense research. Preclinical, clinical and genetic studies strongly point to a particularly important role of A2AR, and downregulation of A2AR has been consistently reported in HD rodent models and also in early stages of the disease (see Introduction and Lee and Chern, 2014). It was therefore surprising that our experiments in transgenic HD Tg51 rats did not show any evidence for a change in the number of A2AR antagonist binding sites, while in a previous report we had shown that HD Tg51 rats were insensitive to the locomotor activating effects of an A2AR antagonist (Orrú et al., 2011). Since the analysis of locomotor depression induced by an A2AR agonist also indicated no evidence for A2AR functional abnormalities, it became obvious to investigate a reduction in the striatal adenosine tone. In fact, the striatal extracellular concentration of adenosine was significantly reduced in Tg51 rats and also in the recently introduced animal model of HD, the zQ175 knock-in mouse (Heikkinen et al., 2012; Menalled et al., 2012). A2AR antagonist binding was nevertheless found to be significantly reduced in zQ175 mice, even though both rodent models were analyzed at ages that show a similar neuropathological degree, which correspond to early neuropathological stages of HD (grade 2 in the Vonsattel scale). This suggests that reduced adenosine (evident in both models) and reduced A2AR density (only evident in zQ175 mice) are two independent processes that develop during the initial neuropathological stages of the disease.
Brain adenosine homeostasis is under the control of several transporters and enzymes. Evidence has been accumulating indicating the involvement of adenosine and astroglia in HD (Lee and Chern, 2014). Adenosine may be released as such from cells (Melani et al., 2012) or may be a product of ATP that is released mostly by astrocytes and is transformed into adenosine by means of membrane-associated ecto-5’-nucleotidases (CD39 and CD73) (Boison et al., 2010). Extracellular adenosine removal depends mostly on the uptake via the equilibrative nucleoside transporter ENT1 (Li et al., 2013), also predominantly expressed in astrocytes (Peng, 2005; Wu et al., 2010). Upregulation of ENT1 should lead to reduced adenosine tone, a mechanism that has been invoked to be involved in the pathogenesis of several neuropsychiatric disorders, including alcohol use disorder and depression (Prediger et al., 2006; Gass et al., 2010; Sari et al., 2013; Hines and Haydon, 2014). We therefore sought for an upregulation of ENT1 in HD rodent models. Indeed, we did not only found the striatal density of ENT1 expression significantly increased in the zQ175 knock-in mouse, but the expression of the ENT1 transcript (SLC29A1) was significantly increased in postmortem prefrontal cortex from HD patients with a grade 2 Vonsattel severity score. The difference in SLC29A1 expression was not seen in more severe neuropathological stages (Vonsattel severity score 3 and 4). The demonstration of the same biochemical changes in equivalent neuropathological stages in the rodent model and HD patients strongly supports ENT1 as a biomarker for HD. Furthermore, a differential coexpression analysis demonstrated that SLC29A1 serves as a critical hub of HD-induced gene dysregulation. These results underscore a significant pathogenetic role of ENT1, especially considering that our DC analysis showed ENT1 gained correlations to several other genes in the HD group comprising all HD stage samples relative to controls.
Altogether, the present study demonstrates that ENT1 and striatal extracellular adenosine constitute biomarkers of the initial stages of neurodegeneration in HD. It is well established that adenosine plays an important neuroprotective role (Stone et al., 2009; Ribeiro et al., 2016) and evidence has been accumulating indicating the involvement of adenosine and astroglia in HD (Lee and Chern, 2014). As mentioned in the Introduction, an insufficient tonic activation of A2AR, which can be related to decreased levels of both the neurotransmitter and the receptor, can be involved in the previously described impairment of BDNF-neuroprotective effect in HD (Zuccato et al., 2001; Lee and Chern, 2014). But altered expression and function of the adenosine receptor (A1R) has also recently reported in mice and patients with HD (Ferrante et al., 2014; Matusch et al., 2014). The potential impact of lower adenosine tone on the function of dysregulated A1R (Blum et al., 2002; Ferrante et al., 2014) during HD progression warrants further investigation.
Therefore, reduced extracellular levels of adenosine secondary to ENT-1 upregulation can be fundamental in the progression of the disease and most probably contributes to the reduced age of onset of HD associated with an A2AR polymorphism and with caffeine intake (Dhaenens et al., 2009; Taherzadeh-Fard et al., 2010). Collectively, these findings predict that ENT1 could constitute a new therapeutic target and ENT1 blockers, such as dipyridamole and T1–11 (Huang et al., 2011), could at least delay the age of onset of HD.
Highlights.
-
*
Decrease in striatal extracellular levels of adenosine was found in HD rodent models
-
*
This was paralleled by upregulation of the equilibrative nucleoside transporter ENT1
-
*
ENT1 was also demonstrated in postmortem brain tissue from HD patients
-
*
Adenosine and ENT1 can constitute biomarkers an therapeutic targets for HD
Acknowledgments
We thank Dr. Ling-Hui Li for the assistance in data extraction from the GEO database and statistical analyses and Dr. Alessia Melani for her assistance in the microdialysis experiments. Work supported by the Intramural Funds of NIDA and NIAID, and from CHDI Foundation.
Abbreviations
- A1R
Adenosine A1 receptor
- A2AR
Adenosine A2A receptor
- D2R
Dopamine D2 receptor
- DC
differential coexpression
- DE
differential expression
- HD
Huntington disease
- HET
heterozygous
- HOM
homozygous
- HTT
huntingtin
- rlm
robust linear regression
- WT
wild type
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors declare no conflict of interest.
References
- Boison D, Chen JF, Fredholm BB. Adenosine signaling and function in glial cells. Cell Death Differ. 2010;17:1071–1082. doi: 10.1038/cdd.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum D, Gall D, Galas MC, d'Alcantara P, Bantubungi K, Schiffmann SN. The adenosine A1 receptor agonist adenosine amine congener exerts a neuroprotective effect against the development of striatal lesions and motor impairments in the 3-nitropropionic acid model of neurotoxicity. J Neurosci. 2002;22:9122–9133. doi: 10.1523/JNEUROSCI.22-20-09122.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JF, Moratalla R, Impagnatiello F, Grandy DK, Cuellar B, Rubinstein M, et al. The role of the D(2) dopamine receptor (D(2)R) in A(2A) adenosine receptor (A(2A)R)-mediated behavioral and cellular responses as revealed by A(2A) and D(2) receptor knockout mice. Proc Natl Acad Sci USA. 2001;98:1970–1975. doi: 10.1073/pnas.98.4.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang MC, Lee YC, Huang CL, Chern Y. cAMP-response element-binding protein contributes to suppression of the A2A adenosine receptor promoter by mutant Huntingtin with expanded polyglutamine residues. J Biol Chem. 2005;280:14331–14340. doi: 10.1074/jbc.M413279200. [DOI] [PubMed] [Google Scholar]
- Choi DS, Cascini MG, Mailliard W, Young H, Paredes P, McMahon T, et al. The type 1 equilibrative nucleoside transporter regulates ethanol intoxication and preference. Nat Neurosci. 2004;7:855–861. doi: 10.1038/nn1288. [DOI] [PubMed] [Google Scholar]
- Dhaenens CM, Burnouf S, Simonin C, Van Brussel E, Duhamel A, Defebvre L, et al. A genetic variation in the ADORA2A gene modifies age at onset in Huntington's disease. Neurobiol Dis. 2009;35:474–476. doi: 10.1016/j.nbd.2009.06.009. [DOI] [PubMed] [Google Scholar]
- Diógenes MJ, Fernandes CC, Sebastião AM, Ribeiro JA. Activation of adenosine A2A receptor facilitates brain-derived neurotrophic factor modulation of synaptic transmission in hippocampal slices. J Neurosci. 2004;24:2905–2913. doi: 10.1523/JNEUROSCI.4454-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrante RJ, Kowall NW, Beal MF, Martin JB, Bird ED, Richardson EP., Jr Morphologic and histochemical characteristics of a spared subset of striatal neurons in Huntington's disease. J Neuropathol Exp Neurol. 1987;46:12–27. doi: 10.1097/00005072-198701000-00002. [DOI] [PubMed] [Google Scholar]
- Ferrante A, Martire A, Pepponi R, Varani K, Vincenzi F, Ferraro L, et al. Expression, pharmacology and functional activity of adenosine A1 receptors in genetic models of Huntington's disease. Neurobiol Dis. 2014;71:193–204. doi: 10.1016/j.nbd.2014.08.013. [DOI] [PubMed] [Google Scholar]
- Ferré S, O'Connor WT, Fuxe K, Ungerstedt U. The striopallidal neuron: a main locus for adenosine-dopamine interactions in the brain. J Neurosci. 1993;13:5402–5406. doi: 10.1523/JNEUROSCI.13-12-05402.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredholm BB, IJzerman AP, Jacobson KA, Linden J, Müller CE. International Union of Basic and Clinical Pharmacology. LXXXI. Nomenclature and classification of adenosine receptors--an update. Pharmacol Rev. 2011;63:1–34. doi: 10.1124/pr.110.003285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gass N, Ollila HM, Utge S, Partonen T, Kronholm E, Pirkola S, et al. Contribution of adenosine related genes to the risk of depression with disturbed sleep. J Affect Disord. 2010;126:134–139. doi: 10.1016/j.jad.2010.03.009. [DOI] [PubMed] [Google Scholar]
- Glass M, Dragunow M, Faull RL. The pattern of neurodegeneration in Huntington's disease: a comparative study of cannabinoid, dopamine, adenosine and GABA(A) receptor alterations in the human basal ganglia in Huntington's disease. Neuroscience. 2000;97:505–519. doi: 10.1016/s0306-4522(00)00008-7. [DOI] [PubMed] [Google Scholar]
- Heikkinen T, Lehtimäki K, Vartiainen N, Puoliväli J, Hendricks SJ, Glaser JR, et al. Characterization of neurophysiological and behavioral changes, MRI brain volumetry and 1H MRS in zQ175 knock-in mouse model of Huntington's disease. PLoS One. 2012;7:e50717. doi: 10.1371/journal.pone.0050717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines DJ, Haydon PG. Astrocytic adenosine: from synapses to psychiatric disorders. Philos Trans R Soc Lond B Biol Sci. 2014;369:20130594. doi: 10.1098/rstb.2013.0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang NK, Lin JH, Lin JT, Lin CI, Liu EM, Lin CJ, et al. A new drug design targeting the adenosinergic system for Huntington's disease. PLoS One. 2011;6:e20934. doi: 10.1371/journal.pone.0020934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kántor O, Temel Y, Holzmann C, Raber K, Nguyen HP, Cao C, et al. Selective striatal neuron loss and alterations in behavior correlate with impaired striatal function in Huntington's disease transgenic rats. Neurobiol Dis. 2006;22:538–547. doi: 10.1016/j.nbd.2005.12.014. [DOI] [PubMed] [Google Scholar]
- Lee C-F, Chern Y. Adenosine receptors and Huntington’s disease. Int Rev Neurobiol. 2014;119:195–232. doi: 10.1016/B978-0-12-801022-8.00010-6. [DOI] [PubMed] [Google Scholar]
- Li B, Gu L, Hertz L, Peng L. Expression of nucleotide transporter in freshly isolated neurons and astrocytes from mouse brain. Neurochem Res. 2013;38:2351–2358. doi: 10.1007/s11064-013-1146-5. [DOI] [PubMed] [Google Scholar]
- Matusch A, Saft C, Elmenhorst D, Kraus PH, Gold R, Hartung HP, et al. Cross sectional PET study of cerebral adenosine A1 receptors in premanifest and manifest Huntington's disease. Eur J Nucl Med Mol Imaging. 2014;41:1210–1220. doi: 10.1007/s00259-014-2724-8. [DOI] [PubMed] [Google Scholar]
- Melani A, Pantoni L, Corsi C, Bianchi L, Monopoli A, Bertorelli R. Striatal outflow of adenosine, excitatory amino acids, gamma-aminobutyric acid, and taurine in awake freely moving rats after middle cerebral artery occlusion: correlations with neurological deficit and histopathological damage. Stroke. 1999;30:2448–2454. doi: 10.1161/01.str.30.11.2448. [DOI] [PubMed] [Google Scholar]
- Melani A, Corti F, Stephan H, Müller CE, Donati C, Bruni P, et al. Ecto-ATPase inhibition: ATP and adenosine release under physiological and ischemic in vivo conditions in the rat striatum. Exp Neurol. 2012;233:193–204. doi: 10.1016/j.expneurol.2011.09.036. [DOI] [PubMed] [Google Scholar]
- Menalled LB, Kudwa AE, Miller S, Fitzpatrick J, Watson-Johnson J, Keating N, et al. Comprehensive behavioral and molecular characterization of a new knock-in mouse model of Huntington's disease: zQ175. PLoS One. 2012;7:e49838. doi: 10.1371/journal.pone.0049838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell IJ, Cooper AJ, Griffiths MR. The selective vulnerability of striatopallidal neurons. Prog Neurobiol. 1999;5:691–719. doi: 10.1016/s0301-0082(99)00019-2. [DOI] [PubMed] [Google Scholar]
- Narayanan M, Huynh JL, Wang K, Yang X, Yoo S, McElwee J, et al. Common dysregulation network in the human prefrontal cortex underlies two neurodenerative diseases. Mol Syst Biol. 2014;10:743–758. doi: 10.15252/msb.20145304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orrú M, Zanoveli JM, Quiroz C, Nguyen HP, Guitart X, Ferré S. Functional changes in postsynaptic adenosine A(2A) receptors during early stages of a rat model of Huntington’s disease. Exp Neurol. 2011;232:76–80. doi: 10.1016/j.expneurol.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng L, Huang R, Yu AC, Fung KY, Rathbone MP, Hertz L. Nucleoside transporter expression and function in cultured mouse astrocytes. Glia. 2005;52:25–35. doi: 10.1002/glia.20216. [DOI] [PubMed] [Google Scholar]
- Peng Q, Wu B, Jiang M, Jin J, Hou Z, Zheng J, et al. Characterization of behavioral, neuropathological, brain metabolic and key molecular changes in zQ175 Knock-In mouse model of Huntington's disease. PLoS One. 2016;11:e0148839. doi: 10.1371/journal.pone.0148839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prediger RD, da Silva GE, Batista LC, Bittencourt AL, Takahashi RN. Activation of adenosine A1 receptors reduces anxiety-like behavior during acute ethanol withdrawal (hangover) in mice. Neuropsychopharmacology. 2006;31:2210–2220. doi: 10.1038/sj.npp.1301001. [DOI] [PubMed] [Google Scholar]
- Qi L, Zhang XD. Role of chaperone-mediated autophagy in degrading Huntington'sdisease-associated huntingtin protein. Acta Biochim Biophys Sin. 2014;46:83–91. doi: 10.1093/abbs/gmt133. [DOI] [PubMed] [Google Scholar]
- Quiroz C, Luján R, Uchigashima M, Simoes AP, Lerner TN, Borycz J, et al. Key modulatory role of presynaptic adenosine A2A receptors in cortical neurotransmission to the striatal direct pathway. ScientificWorldJournal. 2009;9:1321–1344. doi: 10.1100/tsw.2009.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro FF, Xapelli S, Miranda-Lourenço C, Tanqueiro SR, Fonseca-Gomes J, Diógenes MJ, et al. Purine nucleosides in neuroregeneration and neuroprotection. Neuropharmacology. 2016;104:226–242. doi: 10.1016/j.neuropharm.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Rodrigues TM, Jerónimo-Santos A, Sebastião AM, Diógenes MJ. Adenosine A(2A) Receptors as novel upstream regulators of BDNF-mediated attenuation of hippocampal Long-Term Depression (LTD) Neuropharmacology. 2014;79:389–398. doi: 10.1016/j.neuropharm.2013.12.010. [DOI] [PubMed] [Google Scholar]
- Sari Y, Sreemantula SN, Lee MR, Choi DS. Ceftriaxone treatment affects the levels of GLT1 and ENT1 as well as ethanol intake in alcohol-preferring rats. J Mol Neurosci. 2013;51:779–787. doi: 10.1007/s12031-013-0064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonin C, Duru C, Salleron J, Hincker P, Charles P, Delval A, et al. Association between caffeine intake and age at onset in Huntington's disease. Neurobiol Dis. 2013;58:179–182. doi: 10.1016/j.nbd.2013.05.013. [DOI] [PubMed] [Google Scholar]
- Stone TW, Ceruti S, Abbracchio MP. Adenosine receptors and neurological disease: neuroprotection and neurodegeneration. Handb Exp Pharmacol. 2009;193:535–587. doi: 10.1007/978-3-540-89615-9_17. [DOI] [PubMed] [Google Scholar]
- Taherzadeh-Fard E, Saft C, Wieczorek S, Epplen JT, Arning L. Age at onset in Huntington's disease: replication study on the associations of ADORA2A, HAP1 and OGG1. Neurogenetics. 2010;11:435–439. doi: 10.1007/s10048-010-0248-3. [DOI] [PubMed] [Google Scholar]
- The Huntington’s Disease Collaborative Research Group. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell. 1993;72:971–983. doi: 10.1016/0092-8674(93)90585-e. [DOI] [PubMed] [Google Scholar]
- Villar-Menéndez I, Blanch M, Tyebji S, Pereira-Veiga T, Albasanz JL, Martín M, et al. Increased 5-methylcytosine and decreased 5-hydroxymethylcytosine levels are associated with reduced striatal A2AR levels in Huntington's disease. Neuromolecular Med. 2013;15:295–309. doi: 10.1007/s12017-013-8219-0. [DOI] [PubMed] [Google Scholar]
- von Hörsten S, Schmitt I, Nguyen HP, Holzmann C, Schmidt T, Walther T, et al. Transgenic rat model of Huntington's disease. Hum Mol Genet. 2003;12:617–624. doi: 10.1093/hmg/ddg075. [DOI] [PubMed] [Google Scholar]
- Vonsattel JP, Myers RH, Stevens TJ, Ferrante RJ, Bird ED, Richardson EP., Jr Neuropathological classification of Hunt1ington's disease. J Neuropathol Exp Neurol. 1985;44:559–577. doi: 10.1097/00005072-198511000-00003. [DOI] [PubMed] [Google Scholar]
- Wu J, Lee MR, Choi S, Kim T, Choi DS. ENT1 regulates ethanol-sensitive EAAT2 expression and function in astrocytes. Alcohol Clin Exp Res. 2010;34:1110–1117. doi: 10.1111/j.1530-0277.2010.01187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Shen HY, Coelho JE, Araújo IM, Huang QY, Day YJ, et al. Adenosine A2A receptor antagonists exert motor and neuroprotective effects by distinct cellular mechanisms. Ann Neurol. 2008;63:338–346. doi: 10.1002/ana.21313. [DOI] [PubMed] [Google Scholar]
- Zuccato C, Ciammola A, Rigamonti D, Leavitt BR, Goffredo D, Conti L, et al. Loss of huntingtin-mediated BDNF gene transcription in Huntington's disease. Science. 2001;293:493–498. doi: 10.1126/science.1059581. [DOI] [PubMed] [Google Scholar]