Abstract
Introduction
This systematic review examines the excess cost of chronic conditions on the economic burden of cancer survivorship among adults in the US.
Areas covered
Twelve published studies were identified. Although studies varied substantially in populations, comorbidities examined, methods, and types of cost reported, costs for cancer survivors with comorbidities generally increased with greater numbers of comorbidities or an increase in comorbidity index score. Survivors with comorbidities incurred significantly more in total medical costs, out-of-pocket costs, and costs by service type compared to cancer survivors without additional comorbidities.
Expert commentary
Cancer survivors with comorbidities bear significant excess out-of-pocket costs and their care is also more expensive to the healthcare system. On-going evaluation of different payment models, care coordination, and disease management programs for cancer survivors with comorbidities will be important in monitoring impact on healthcare costs.
Keywords: Cancer survivors, chronic conditions, economic burden, systematic review
1. Introduction
Cancer survivors, both those undergoing active treatment or who have lived with the diagnosis long-term, are a steadily growing segment of the US population [1]. There are approximately 15.5 million cancer survivors in the United States, with numbers projected to exceed 20 million by 2026 [1,2]. Older age and other behavioral factors, such as tobacco use and lack of physical activity, are concurrent risk factors for cancer as well as developing other chronic conditions (e.g. obesity, diabetes, chronic obstructive pulmonary disease) [3]. Cooccurrence of these conditions (or multiple chronic conditions [MCCs] or multi-morbidity) is highly-prevalent among cancer survivors, occurring in about 7 out of 10 survivors [4–6]. MCCs among cancer survivors [4,7,8] can complicate health-care delivery (i.e. cancer treatment) and create practical concerns about survivorship care [9]. The presence of MCCs may also increase health-care costs for patients and the health-care system more broadly.
The economic burden of cancer survivorship in the United States is substantial [10–13]. Cancer survivors continue to have unique medical and psychosocial health-care needs related to their cancer diagnosis that impact health-care costs long after diagnosis [11]. Prior studies have demonstrated that cancer survivors incur, on average, $3000–4000 (US $2011 dollars) in added medical costs compared to individuals without a cancer history [13]. Additionally, survivors have been shown to have more health concerns posttreatment than age- and sex-matched controls [14], and are also more likely to have hospitalizations, emergency room visits, ambulatory surgeries, and office visits than individuals without a cancer history [15,16]. Cancer survivors also face varying degrees of challenges with coexisting conditions, unmet psychological needs, and financial hardship throughout survivorship [11,17]. In light of recent transformations in the health-care system [18,19] and as more people survive to older ages with MCCs, it is critical to examine the excess burden that chronic conditions impose on survivors’ medical-care costs as well as other aspects of economic burden, including productivity losses due to employment disability, missed work days, and inability to participate in usual activities.
The purpose of this study was to systematically review and synthesize findings from the published literature on the economic burden of chronic conditions among cancer survivors in the United States. Our findings will inform understanding of the potential benefits of effective prevention and early detection efforts and chronic disease management efforts for cancer survivors. This review will also identify research gaps and areas for future health intervention efforts.
2. Methods
2.1. Search strategy and study selection
Published papers examining the excess cost of chronic conditions among cancer survivors were identified from the following electronic databases: PubMed, Web of Science Core Collection, and EconLit via EBSCOHost. The searches were limited to English language studies published from January 2000 through December 2015. Search terms were identified to retrieve articles addressing the three main concepts in the research question: (1) cancer survivors (i.e. any person who has ever been diagnosed with cancer) [1], (2) comorbidities/multi-morbidity/(multiple) chronic conditions, and (3) economic burden, including medical-care costs and productivity losses. Specific comorbidity and chronic condition terms were derived from the most prevalent conditions [3] and key relevant articles [20,21]. Terms to identify health-care costs were adapted from a summary of health-care cost data sources [22]. The exact search strategy used in each of the electronic databases is reported in Appendix. Because electronic search strategies may be incomplete [23], we also manually searched the reference lists from selected articles to ensure a comprehensive review of the literature.
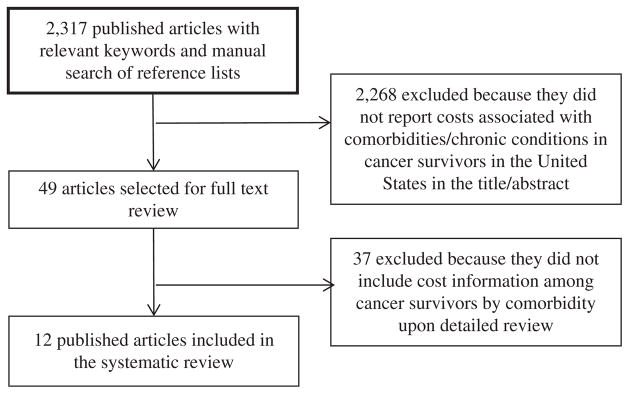
All references were uploaded to Covidence Systematic Review software (https://www.covidence.org), a web-based tool designed to facilitate and track each step of the abstraction and review process. Two reviewers (SHR and GPG) conducted dual review of the titles and abstracts. Articles were excluded if the abstract did not contain some indication of ‘cost,’ ‘comorbidities,’ or ‘cancer’; or the study population consisted only of cancer survivors outside the United States. A full-text review of all potentially relevant articles to further assess eligibility was then conducted. Study inclusion criteria entailed the reporting of estimates of costs (medical expenditures, lost productivity, or financial burden) related to chronic conditions among adult cancer survivors. Studies that analyzed the impact of comorbidities only on the cost of a specific procedure (i.e. surgery) or medication among cancer survivors were excluded. We also excluded gray literature (dissertations, government reports, issue briefs), editorials, essays, reviews/systematic reviews, and cost-effectiveness studies. Any discrepancies about eligibility were resolved through discussion and consensus between the two reviewers. Our search identified 2,317 studies of which 2,268 were excluded based on abstract review, leaving 49 articles for full-text review. Of the 49 articles, 37 did not include cost information among cancer survivors by comorbidity, and 12 met all inclusion criteria (Figure 1) [21,24–34]. No additional articles were identified through manual reference list search.
Figure 1.
Flowchart illustrating the study selection process.
2.2. Data abstraction
We abstracted detailed information on the study characteristics, cancer survivor population, comorbidities reported, and type of cost estimates included. The study characteristics included data source(s), method of identifying the cancer survivor study population (registry, claims, self-report), data year(s), and geographic setting (single state, multistate, national). For each study, the cancer survivor population was described by size (number of survivors), age, and type of cancer. The additional costs due to the presence of comorbidities were quantified both overall, and by service type (inpatient, outpatient, and prescription drugs) and source of payment (out-of-pocket expenditures), when available. Comorbidity cost estimates were abstracted separately for each individual condition and for the presence of MCCs. We did not adjust costs to a single reference year because of the heterogeneity in patient populations, care settings, measures, treatment costs, and other differences in methodology that would prohibit a meaningful interpretation of estimates [35]. Additionally, the studies were conducted across periods with varying treatment patterns and health-care payment models. Instead, we report all costs as presented in the underlying studies. This heterogeneity across studies also prohibited a quantitative synthesis of cost estimates.
3. Results
3.1. Study characteristics
Table 1 provides an overview of the 12 studies included in the systematic review. While each study included information on medical expenditures due to comorbidities, none provided estimates of lost productivity. To estimate medical expenditures, the studies used a variety of data sources, including Surveillance, Epidemiology, End Result (SEER)-Medicare linked data (five studies), the Medical Expenditure Panel Survey (MEPS) (four studies), Medicaid (two studies), and the Medicare Current Beneficiary Survey (one study). The majority (10 studies) utilized national or nationally representative data and represented different cancers including thyroid, oral cavity/pharyngeal, renal cell carcinoma, head/neck cancers, ovarian, colon, and ‘all cancer’ sites. Most articles (10 of 12 studies) reported an aggregated index for comorbidities (e.g. Charlson Comorbidity Index, Washington University Head and Neck Cancer Comorbidity Index) and 2 articles examined both individual chronic conditions and multiple conditions as a count. Because claims-based indexes typically use information about conditions prior to cancer diagnosis, some studies using Medicare claims data restrict their samples to patients ages 66 and older (1 year after age-based Medicare eligibility). All articles were published between 2003 and 2015.
Table 1.
Characteristics of studies examining the economic burden of chronic conditions among cancer survivors.
| Study | Data sources | Cancer survivor population |
Geographic setting |
Cancer patient identification |
Time frame of costs |
Cost by service type | Individual conditions examined |
Multiple chronic conditions |
|---|---|---|---|---|---|---|---|---|
| Bernard et al. [24] | 2001–2008 MEPS, and 2001–2008 NHIS-MEPS linked sample | 4243 adults aged 18–64 years reporting any cancer diagnosis/receiving cancer treatment | National | Self-report | 1 year | Yes (0, 1+) | ||
| Boltz et al. [25] | 1995–2005 SEER Medicare | 2823 adults aged ≥65 years with a differentiated thyroid cancer diagnosis | National | Registry | 1 and 5-year costs following diagnosis | Yes (0, 1 or 2, 3+) | ||
| Cohen et al. 2003 [26] | 1997 MEPS | Adults aged ≥18 years with medical expenditures for any cancer. Sample size not provided. | National | Self-report | 1 year | Inpatient, ambulatory, prescription drugs, home health care | Yes (1, 2, 3) | |
| Davidoff et al. [27] | 1997–2007 MCBS linked to Medicare claims | 1868 Medicare beneficiaries aged >65 years with any cancer diagnosis | National | Claims | 2 year following identification | Yes (0–1, 2–4, 5–8, ≥9) | ||
| Forde et al. [28] | 1992–2009 SEER Medicare | 4506 women aged ≥65 years with an ovarian cancer diagnosis who underwent PDS or NACT | National | Registry/Claims | 7-months after PDS or NACT | Yes (0, 1, 2+) | ||
| Han et al. [29] | 2008–2010 MEPS | 4326 adults aged ≥18 years with any cancer ever diagnosed | National | Self-report | 1 year | Serious psychological distress | ||
| Hollenbeak et al. [32] | 1984–1994 SEER Medicare | 1780 Medicare beneficiaries with head and neck cancer diagnosisa | National | Registry | 1 and 5-year costs | Yes (WUHNCCI) | ||
| Hollenbeak et al. [31] | 1995–2002 SEER Medicare | 4938 Medicare beneficiaries with renal cell carcinoma ever diagnoseda | National | Registry | 1 and 5-year costs following diagnosis | Anemia, hyperlidemia | Yes (CCI) | |
| Hollenbeak et al. [30] | 1995–2005 SEER Medicare | 10711 Medicare beneficiaries aged ≥66 years with oral cavity (n = 6724) or pharyngeal cancer (n = 3987) ever diagnosed | National | Registry | 5-year costs following diagnosis | Yes (0, 1–2, 3+) | ||
| Luo et al. [33] | 1996–2000 Michigan Medicaid and Medicare data merged with the Michigan Tumor Registry | 6462 Medicare beneficiaries aged ≥66 years (765 were also insured by Medicaid) with colon cancer diagnosis | Single state (Michigan) | Registry | 1 year following diagnosis | Yes (0, 1, 2, 3+) | ||
| Pan et al. [34] | 2006–2009 MEPS | 4766 adults aged ≥21 years with any cancer | National | Self-report | 1 year costs | Inpatient, outpatient, prescription drugs, emergency department, otherb | Depression | |
| Subramanian et al. [21] | 2000–2003 Medicaid administrative data linked to cancer registry data | 6212 Medicaid beneficiaries aged 21–64 years with any cancer diagnosis | Multiple states (Georgia, Maine, and Illinois) | Registry | 0–6 months following diagnosis | Hospital stays, ambulatory care services, prescription drugs, long-term care | Cardiac, Respiratory, Diabetes, Mental Health | Yes (1, 2, 3–4) |
MEPS: Medical Expenditure Panel Survey; NHIS: National Health Interview Survey; SEER: surveillance, epidemiology, end result; CCI: Charlson Comorbidity Index; WUHNCCI: Washington University Head and Neck Cancer Comorbidity Index; PDS: primary debulking surgery; NACT: neo-adjuvant chemotherapy; MCBS: Medicare Current Beneficiary Survey.
The age of Medicare beneficiaries included could not be ascertained from the published article; we assume aged ≥66 years.
Other expenditures include home health care, dental, vision, durable medical equipment, and other miscellaneous items.
3.2. Excess medical costs per person associated with specific chronic conditions among cancer survivors
Four studies provided estimates of the additional medical costs attributable to individual chronic conditions (Table 2) [21,29,31,34]. Among cancer survivors enrolled in Medicaid in three states (Georgia, Maine, or Illinois), the additional total cost of care over a 6-month period ranged from $3418 to $4385 for cardiac conditions; $5040 to $8155 for respiratory conditions; and $7483 to $7714 for diabetes (all US$ 2003) [21]. Among elderly renal cell carcinoma cancer survivors, the additional 1-year Medicare costs of care attributed to hyperlipidemia and anemia were $2745 and $2167 (US$ 2005), respectively [31]. Within a nationally representative sample, the additional annual cost of psychosocial distress was estimated to be $4431 (US$ 2010) [29] and $6310 (US$ 2009) for depression [34] among cancer survivors. Meanwhile, among cancer survivors enrolled in Medicaid in Georgia, Maine, or Illinois [21], the estimated additional costs of mental health disorders (including schizophrenic disorders, episodic mood disorders, delusional disorders, anxiety/personality disorders, and depressive disorders) was $8004 to $11,009 over a 6-month period (US$ 2003) [21].
Table 2.
Additional per person medical costs associated with specific chronic conditions among cancer survivors.
| Study | Costs measured | Chronic conditions | Total costs | Costs by service type | |||
|---|---|---|---|---|---|---|---|
| Hospital /Inpatient costs | Prescription drug costs | Long-term care costs | Ambulatory/Outpatient care costs | ||||
| Han et al. [29] | 1-year costs (US$ 2010) for survivors with all cancers | Serious psychological distress | $4431* | ||||
| Hollenbeak et al. [31] | 1-year costs for renal cell carcinoma patients (US$ 2005) | Hyperlipidemia | $2745* | ||||
| Anemia | $2167 | ||||||
| 5-year costs for renal cell carcinoma patients (US$ 2005) | Hyperlipidemia | $2551 | |||||
| Anemia | $1113 | ||||||
| Pan, X. et al. [34]b | 1-year costs (US$ 2009) for survivors with all cancers | Depression | $6310* | $2272*c | $2297* | $858* | |
| Subramanian et al. [21] | Additional 6-month cost of all cancer care, including those who died during the 6-month follow-up (US$ 2003) | Cardiac | $3418* | $2732* | $168 | $362* | $156 |
| Respiratory | $5040* | $4618* | $345* | -$28 | $105 | ||
| Diabetes | $7483* | $4678* | $1037* | $601* | $1167* | ||
| Mental healtha | $8004* | $4979* | $546* | $1722* | $756* | ||
| Additional 6-month cost of all cancer care, excluding those who died during the 6-month follow-up (US$ 2003) | Cardiac | $4385* | $3311* | $288 | $525* | $261 | |
| Respiratory | $8155* | $6714* | $488* | $147 | $807 | ||
| Diabetes | $7714* | $5112* | $1011* | $683* | $909* | ||
| Mental healtha | $11,009* | $6883* | $715* | $2214* | $1198* | ||
Mental health includes schizophrenic disorders, episodic mood disorders, delusional disorders, anxiety/personality disorders, and depressive disorders.
The study also reports on emergency department cost ($155) and other costs ($715), which include other expenditures like home health care, dental, vision, durable medical equipment, and other miscellaneous items.
Only includes costs among individuals with expenditures on these inpatient services.
Denotes that the difference was statistically significant at p < .05, per the respective underlying study.
Two studies provided estimates of the additional medical costs associated with individual chronic conditions by service type [21,34]. Hospital costs accounted for the largest additional per person 6-month medical costs associated with cardiac conditions, respiratory conditions, diabetes, and mental health [21]. Additional prescription drug costs per person were highest for survivors with diabetes ($1011, US$ 2003) [21]. Mental health had the highest hospital ($6883), long-term care ($2214), and ambulatory care costs ($1198) compared to other conditions (in US$ 2003) [21]. The added 1-year costs per cancer survivor with depression were highest in the hospital and ambulatory care setting [34].
3.3. Excess total medical costs per person associated with MCCs among cancer survivors
Regardless of the specific comorbid condition(s), the average cost of care for patients with chronic comorbidities increased with greater numbers of comorbidities or with an increase in the comorbidity index score (Table 3). Having one additional comorbidity compared to none was associated with increased annual costs of $2762 among colon cancer survivors with Medicare/Medicaid in Michigan (US$ 2001) [33], and increased 6-month costs of $4584 among cancer survivors of all sites in Medicaid patients in Georgia, Maine, or Illinois (US$ 2003) [21]. For ovarian cancer patients, the 7-month cost of care (US$ 2010 dollars) for having one comorbidity (compared to none) was $1793 for stage IIIC patients and $5625 for stage IV patients [28]. As the number of comorbidities increased, the cost attributed to comorbidities increased substantially. For example, costs were $13,369 and $25,739 higher among cancer survivors of all sites in Medicaid in Georgia, Maine, or Illinois with 2 comorbidities and ≥3 comorbidities, respectively, compared to cancer survivors with no additional comorbidities (US$ 2003) [21]. Similar trends were found across several studies for thyroid, oral cavity, pharyngeal, colon, and ovarian cancer survivors [25,28,30,31,33].
Table 3.
Additional per person total medical costs associated with multiple chronic conditions among cancer survivors.
| Study | Costs measureda | Number of comorbidities | Total costs |
|---|---|---|---|
| Boltz et al. [25] | 1-year costs for thyroid cancer patients (US$ 2009) | None | Reference |
| 1–2 Comorbidities | $13,972* | ||
| 3+ Comorbidities | $37,350* | ||
| 5-year costs for thyroid cancer patients (US$ 2009) | None | Reference | |
| 1–2 Comorbidities | $27,648* | ||
| 3+ Comorbidities | $62,234* | ||
| Cohen et al. [26]b | Mean spending per person (any cancer) with expenditure (US$ 1997) | 1 Comorbidity | $7317* |
| 2 Comorbidities | $5262* | ||
| 3+ Comorbidities | $12,810* | ||
| Forde et al. [28] | 7-month (unadjusted median) cost of care for FIGO stage IIIC ovarian cancer patients (US$ 2010) | None | Reference |
| 1 Comorbidity | $1793* | ||
| 2+ Comorbidities | $3949* | ||
| 7-month (unadjusted median) cost of care for FIGO stage IV ovarian cancer patients (US$ 2010) | None | Reference | |
| 1 Comorbidity | $5625 | ||
| 2+ Comorbidities | $10,207* | ||
| Luo et al. [33] | 1-year costs for colon cancer patients (US$ 2000) | None | Reference |
| 1 Comorbidity | $2762* | ||
| 2 Comorbidities | $3095* | ||
| 3+ Comorbidities | $7717* | ||
| Hollenbeak et al. [32] | 5-year costs for head and neck cancer patients. Marginal effect at representative values: 60-year white male with local disease, treated with single modality surgery (US$ 1994)c | Increase in WUHNCCI 0–1 | $1658* |
| Increase in WUHNCCI 4–5 | $2105* | ||
| Increase in WUHNCCI 9–10 | $2837* | ||
| Hollenbeak et al. [31] | 1-year costs for renal cell carcinoma patients (US$ 2005) | 1-point increase in CCI | $4493* |
| 5-year costs for renal cell carcinoma patients (US$ 2005) | 1-point increase in CCI | $9505* | |
| Hollenbeak et al. [30] | 5-year cost for oral cavity cancer patients (US$ 2005) | 0 Comorbidity | Reference |
| 1–2 Comorbidities | $13,342* | ||
| 3+ Comorbidities | $22,196* | ||
| 5-year cost for pharyngeal cancer patients (US$ 2005) | 0 Comorbidity | Reference | |
| 1–2 Comorbidities | $14,139* | ||
| 3+ Comorbidities | $27,799* |
CCI: Charlson Comorbidity Index; WUHNCCI: Washington University Head and Neck Cancer Comorbidity Index; FIGO: International Federation of Gynecologists and Obstetricians.
Costs measured are for all cancer sites unless otherwise noted. Costs are reported as presented in the respective underlying studies.
Cohen et al. is the only paper that does not report on the additional cost of comorbidities. The authors report that estimates for cancer patients with zero comorbidities were too small to make reliable national estimates.
The year of cost adjustment could not be ascertained from the study; we assumed it to be the last year of data, 1994.
Denotes that the difference was statistically significant at p < .05, per the respective underlying study.
The excess cost of comorbidities was about twofold higher among those with three to four comorbidities compared to survivors with two comorbidities, when examined by service type (Table 4). Hospital costs, for example were $18,211 for cancer patients with 3–4 comorbidities compared to $9891 among patients with 2 comorbidities (US$ 2003) [21].
Table 4.
Additional per person medical costs by service type associated with multiple chronic conditions among cancer survivors.
| Study | Costs measureda | Number of comorbidities | Cost by service type | ||||
|---|---|---|---|---|---|---|---|
| Hospital costs | Prescription drug costs | Home health costs | Ambulatory care costs | Long-term care costs | |||
| Cohen et al.b [26] | Mean spending per person (any cancer) with expenditure (US$ 1997) | 1 Comorbidity | $4407* | $175* | $631* | $1876* | |
| 2 Comorbidities | $2741* | $370* | $33* | $1839* | |||
| 3+ Comorbidities | $6201* | $1067* | $1004* | $3498* | |||
| Subramanian et al. [21] | Additional 6-month cost of all cancer care, including those who died during the 6-month follow-up (US$ 2003) | None | Reference | Reference | Reference | Reference | |
| 1 Comorbidity | $1824 | $373* | $646* | $335 | |||
| 2 Comorbidities | $7000* | $967* | $976* | $861* | |||
| 3–4 Comorbidities | $14,596* | $1715* | $1787* | $2066* | |||
| Additional 6-month cost of all cancer care, excluding those who died during the 6-month follow-up (US$ 2003) | None | Reference | Reference | Reference | Reference | ||
| 1 Comorbidity | $2727* | $435* | $1006* | $416 | |||
| 2 Comorbidities | $9891* | $1033* | $1319* | $1126* | |||
| 3–4 Comorbidities | $18,211* | $2199* | $2396* | $2933* | |||
Costs measured are for all cancer sites unless otherwise noted. Costs are reported as presented in the respective underlying studies.
Cohen et al. is the only paper that does not report on the additional cost of comorbidities. The authors report that estimates for cancer patients with zero comorbidities were too small to make reliable national estimates.
Denotes that the difference was statistically significant at p < .05, per the respective underlying study.
Two studies examined the additional out-of-pocket expenditures attributed to comorbidities and found that annual out-of-pocket expenditures also increased as the number of comorbidities increased (Table 5) [24,27]. Among cancer survivors in Medicare, out-of-pocket costs were $2133 and $3275 higher (in US$ 2007 dollars) among individuals with 5–8 comorbidities and ≥9 comorbidities, respectively, compared to those with no additional comorbidities [27]. Among a nationally representative sample of cancer survivors, out-of-pocket costs were $879 (US$ 2008) higher among those with other comorbidities compared to cancer survivors with no additional comorbidities [24] (Table 5).
Table 5.
Additional per person medical costs by payer associated with multiple chronic conditions among cancer survivors.
| Study | Costs measureda | Number of comorbidities | Cost by payer | |
|---|---|---|---|---|
| Out-of-pocket | Medicare only | |||
| Bernard et al. [24] | Annual out-of-pocket expenditures on health care (US$ 2008) | Cancer only | Reference | |
| Cancer with other chronic conditions | $879* | |||
| Davidoff et al. [27] | 2-year out-of-pocket expenditures on health care (US$ 2007) | 0–1 Comorbidity | Reference | |
| 2–4 Comorbidities | $1670 | |||
| 5–8 Comorbidities | $2133* | |||
| 9+ Comorbidities | $3275* | |||
| Luo et al. [33] | 1-year costs for colon cancer patients (US$ 2000) | None | Reference | |
| 1 Comorbidity | $2781* | |||
| 2 Comorbidities | $3136* | |||
| 3+ Comorbidities | $7796* | |||
Costs measured are for all cancer sites unless otherwise noted. Costs are reported as presented in the respective underlying studies.
Denotes that the difference was statistically significant at p < .05, per the respective underlying study.
4. Discussion
In this study, we conducted a systematic review of studies published within the last 15 years on the economic burden of chronic conditions among cancer survivors. Despite the increasing prevalence of cancer survivorship and chronic conditions, few studies have addressed this important topic. As expected, the studies varied on the patient populations included, data collection methods used, comorbidities considered, and costing approaches. Although the differences between studies complicate any direct comparison and quantitative synthesis across studies [35], our findings do highlight some, key commonalities. First, within each study, the additional cost of care for cancer survivors with chronic conditions increased with greater numbers of conditions or with an increase in the comorbidity index score, regardless of the specific comorbid condition(s). Mental health disorders [21], psychological distress [29], and depression [34] were among those associated with considerably greater total health-care costs by all service types. Second, within studies examining out-of-pocket medical costs [24,27], survivors with the highest number of comorbidities paid considerably more out-of-pocket (up to $3275, US$ 2007) compared to cancer survivors without comorbidities, even after controlling for type of insurance. Thus, our findings highlight the potential economic gains that could be realized by preventing or reducing chronic conditions among cancer survivors. They also underscore the need for continued efforts in evaluating the economic burden of cancer survivorship and the financial hardship faced by cancer survivors. Improved understanding of the relative importance of different aspects of economic burden at the societal, health system, employer, and patient and family levels will be important for future research.
Our findings are salient for adult cancer survivors with greater number of comorbidities, whom tend to incur excess financial burden throughout survivorship and will likely continue to experience greater burden as the cost of cancer therapies increase [11,36]. Along with rising health-care costs [37], the affordability of care is also a major concern as the onus of medical costs have gradually shifted toward the patient with increasing deductibles, copayments, and use of coinsurance [11,36]. Even with health insurance, cancer survivors and particularly those with a higher number of comorbidities will be vulnerable to the deductibles and out-of-pocket costs. For example, the maximum out-of-pocket limit for a family plan is $13,700 (Health Insurance Marketplace in 2016), or the equivalent of approximately one-fifth of the median family income for a family of four in the United States (according to the US Census Bureau, American Community Survey 2014). In addition, given the increasing prevalence of material and psychological financial hardship (e.g. debt, bankruptcy, and worries about medical bills) associated with cancer [11,36], improved education, targeted interventions, and/or coordinated disease management efforts continue to be critical. As oncologists are increasingly discussing the financial consequences of treatment options with their patients as a component of delivering high-quality care [38,39], greater awareness, and educational/social support tools are useful to help address the economic burden among survivors with MCCs.
4.1. Addressing comorbidities in cancer survivorship
Persons with MCCs have been in the spotlight as a priority population, particularly in the past two decades [40,41]. This renewed attention coincides with the recognition that more people are living with chronic conditions [3], surviving cancers long-term [1], and that the proportion of individuals with both cancer and MCCs is sizable and growing. These concerns, coupled with the shifting focus of the health-care system toward delivering person-centered, team-based, coordinated health care [40], creates a need to consider different, innovative models of health-care delivery for this subgroup. As the projected cost of cancer care reaches an estimated $160 billion in 2020 [2], identifying ways of ensuring access to continued follow-up care and reducing unnecessary and avoidable health-care utilization through effective chronic disease management and coordinated efforts is important.
For example, patient-centered medical homes (PCMH) have emerged as one model of health-care delivery that may be well suited for persons with complex, comorbid conditions. Specifically, the ‘COME HOME Program’ [42] (http://www.comehomeprogram.com/index.php/come-home-practices/), an oncology PCMH model conducted within seven community oncology practices in the United States, actively integrates infrastructure-, clinical-, and payment-systems changes to deliver better patient-centered, coordinated, comprehensive care [42]. Preliminary evaluation of the program showed a reduction in unnecessary emergency room visits and hospitalizations, improved patient satisfaction, and projected Medicare savings of $4178 per member per year, though independent evaluation results have yet to be published. Other payment models, such as the Oncology Care Model (OCM) (https://innovation.cms.gov/initiatives/oncology-care/) for cancer patients receiving chemotherapy, focus on care coordination, improving clinic access, and providing guideline-consistent care. Implementation of the 5-year OCM began on July 1, 2016; however, as it progresses, evaluation of outcomes of cancer patients with multiple comorbidities will be important.
As the spending associated with chronic disease/comorbidities among cancer survivors increases for both the patient-(out-of-pocket) and health-care systems [43], it will increasingly be necessary to identify novel programs and implement proven, scalable ones for survivors with MCCs. ‘Fostering health care and public health system changes’ and ‘maximizing the use of proven self-care management and other services’ to improve the health of individuals with MCCs are among the US Department of Health and Human Services (DHHS) strategic vision for Individuals with MCCs [44]. Per this DHHS strategic vision, there is a call to ‘facilitate research to fill knowledge gaps about, and interventions and systems to benefits, individuals with multiple chronic conditions.’ [44] Our analysis identified several research gaps and areas for future research, as a starting point for these efforts.
Currently, comprehensive, population-based, longitudinal data on cancer patients and comorbidities is limited. These data are critical for understanding the timing of the onset of chronic conditions and cancer diagnosis. The published literature addressing cancer survivors with multiple comorbidities mainly included two data sources, SEER-Medicare and the MEPS, both of which have inherent limitations in generalizability and representativeness of the full cancer burden within the United States. The linked SEER-Medicare data only include information about Medicare payments for covered services, and do not include detailed information about out-of-pocket spending or other payers or any information about services that are not covered by the Medicare program. Medicare payments have been estimated to be about 60% of total spending [45]. In addition, these data are limited to Medicare beneficiaries, the majority of whom are aged ≥65 years. As such, estimates provided from these studies likely underestimate the impact of chronic conditions on cancer survivorship. Only four studies included in the systematic review represent younger cancer survivor populations under age 65 years, many of whom may be less likely to have MCCs but also may experience greater out-of-pocket burden and costs associated with survivorship compared to individuals their age without a cancer history. Furthermore, SEER registries capture only about 28% of the US population and over-represent urban area and individuals with higher income [46].
The second commonly used data set, MEPS, is a nationally representative household survey of health-care utilization and expenditures; while it is one of the most detailed data sources available for estimating medical expenditures and out-of-pocket costs, it is not without limitations. The sample is only inclusive of the non-institutionalized, civilian, adult US population and these data rely on household-reporting, including the identification of cancer survivors, which introduces a potential for reporting bias [47]. The cancer diagnosis question in the MEPS refers to cancer or a malignancy of any kind, which may result in identifying those with pre-invasive disease as cancer survivors. Additionally, as others have noted, population-based household surveys are less likely to identify individuals with rare and short-survival, high-cost cancers [48,49]. Analyses using MEPS data also were unable to examine costs associated with terminal care, which are arguably among the most costly patients per capita and the data were also unable to examine the burden by cancer site given inadequate sample size [50]. To the extent that this is the case, the impact of cancer survivorship on out-of-pocket burden would be underestimated in the identified studies.
4.2. Future research
This systematic review of the literature identified several gaps that warrant further exploration. First, there were several common chronic conditions in which the economic burden was not estimated among cancer survivors (e.g. heart conditions, chronic obstructive pulmonary disease, asthma, mental and trauma-related disorders [20]). For example, while four studies reported on specific chronic conditions, only two of those studies itemized the costs associated with the most prevalent and costly chronic conditions [3,20] outside of mental health conditions. No studies specifically reported on the excess cost of trauma-related disorders and arthritis, two of the top five most costly conditions, among adults cancer survivors [20]. Second, our systematic review identified no published studies that quantified the economic burden of lost productivity resulting from comorbidities among cancer survivors. Given that prior studies have shown chronic conditions to be associated with increased lost productivity among cancer survivors [21,51], this is a key area for further research. Third, only two studies reported on the added out-of-pocket costs that cancer survivors with comorbidities incur over those without comorbidities. Given the evidence that cancer survivors experience financial hardship, debt, and bankruptcy [11,36], more research is needed in this area to further assess the impact of rising out-of-pocket health-care costs among cancer survivors with additional chronic conditions. This work will be especially important among the uninsured and previously uninsured, who may face additional challenges with care coordination. Fourth, there was substantial variation across data sources, as previously noted [52], and by cancer types. Very few studies were able to stratify cost by cancer sites. This highlights the importance of conducting studies assessing economic burden using other data sources, such as commercial claims data. Lastly, while we only examined the excess costs from additional numbers of comorbidities in this systematic review, and not the impact of the magnitude or severity of comorbidities, we expect that the added cost would significantly increase with greater severity of chronic conditions. In this respect, future cost analyses are needed to examine the economic impact of severity and longitudinal coexistence of chronic conditions. Better documentation of the timing of chronic condition onset in relation to cancer diagnoses would allow better use of estimates in cost-effectiveness analyses of cancer treatment.
4.3. Limitations
Our systematic review of the published literature has some limitations. Because of the heterogeneity across studies, there were significant challenges to synthesizing the costs of chronic conditions among cancer survivors based on the data from the underlying studies. Many of the challenges that others have noted [35], including the omission of cost adjustment years, inadequate explanation of methodology, and concerns about sample selection and representativeness, also pertained to this review. Furthermore, though we used several large databases (PubMed/MEDLINE, Web of Science Core Collection, and EconLit via EBSCOHost) devoted to health and economic literature/publications and also conducted a comprehensive review of the reference lists for additional studies according to best practices for systematic reviews, it is still possible that we may have still missed some studies for inclusion based on our search strategy.
4.4. Conclusion
In summary, our review of the published literature found that caring for cancer survivors with greater numbers of comorbidities cost more to the health-care system, accounting for greater health-care spending, including excess out-of-pocket costs compared to cancer survivors without chronic conditions. In this review, we observed several areas for future research that may aid in efforts to identify and implement chronic disease prevention, care coordination, and disease management programs for cancer survivors with comorbidities may help to mitigate these costs.
5. Expert commentary & 5-year view
‘The good physician treats the disease; the great physician treats the patient who has the disease.’
(William Osler, 19th century physician-scientist)
Some of the greatest challenges in the current health-care system may be in providing high-quality evidence-based care to medically complex patients, including cancer survivors with MCCs. These challenges arise, in part, from the limited research not only on cancer survivors and those with coexisting chronic conditions, but also the combination of individuals with both cancer and multiple (coexisting) chronic conditions. The latter subpopulation, in particular, has largely been understudied to date given the clinical heterogeneity and complexity of conditions involved [41] and lack of successful models on how to effectively and efficiently deliver comprehensive and coordinated care for these individuals. With the US population aging rapidly, the proportion of cancer survivors growing, and the number of adults with chronic conditions increasing at about 1% per year [45], greater focus on delivering appropriate and high-quality, patient-centered care will be important for this population.
Cost of care in this subpopulation equally deserves attention. Given the substantial economic burden of caring for cancer survivors with MCCs and significant gaps in the literature, further research that enables a more granular examination of costs by different combinations of comorbidities, cancers, and measures of economic burden (i.e. lost productivity, years of potential life lost, quality-adjusted and disability-adjusted life years) are needed. Importantly, given that all of the studies in our systematic review were conducted using data prior to the introduction and full implementation of the Affordable Care Act (ACA), similar economic studies and those that include longer term trends of economic burden among cancer survivors with MCCs post-ACA will be needed, as more people obtain affordable coverage under insurance plans offered through the Health Insurance Marketplace or Medicaid and subsequently access the health-care system. To these ends, attention to the impact of other provisions of the ACA – like the granting of coverage despite preexisting chronic conditions, prohibiting of annual and lifetime coverage limitations, and the expansion of Medicaid coverage in some states – may also be particularly relevant among cancer survivors with severe and multiple chronic conditions.
Approximately 40% of Americans are expected to develop cancer in their lifetime [53]. And more than 70% of US adults aged ≥65 years will have two or more chronic conditions [45]. If recent trends continue, cancer care spending will continue to accelerate due to the high cost of new therapies and the growing population of cancer patients at need of treatment and follow-up care [38]. Engaging and understanding viewpoints of the patients, providers, industry, and payers for how rising cancer costs can impact the system at each level will be important [38].
Over the next 5- to 10 years, the economic burden of medical care, particularly among the sickest patients (with cancer and/or severe or MCCs) may expand as a result of underlying demographics and developments of novel treatments as well as changes in the health-care system with the ACA [54]. While the care of cancer survivors may consider costs and affordability both to the individual and health-care system, it should not be at the expense of continuing to offer high-quality, patient-centered care to each individual. Greater efforts around patient education, disease management, and communication (among the ‘triad’ of decision-makers: patient, family/caregiver, physician [55]) could help to ensure that the patient voice, needs, and preferences are incorporated in the health-care decision-making process.
On-going research and evaluation efforts around patient-centered outcomes research initiatives, personalized (or precision) medicine Initiatives and value-based payment models such as the OCM and ‘COME HOME’ Program are necessary for progress to be made in providing high-quality, patient-centered care, while considering costs. Furthermore, most cancer survivors with severe chronic diseases will likely have an on-going need to ascertain symptoms for periodic changes and adjustments in medications, accordingly. Though big data and rapid learning health-care systems are still nascent in its uses, having the ability to link more robust information sources for diagnostic, medical, and treatment-related information with patient-reported outcomes will be likely be a promising resource in improving patient care and providing evidence for researchers how to optimize treatment delivery and effectiveness. Social and health systems policies continue to be necessary to help make these efforts sustainable and effective, long-term.
Key issues.
Cancer survivors with multiple chronic conditions account for greater healthcare spending, including out-of-pocket costs, than survivors without other chronic conditions.
Out-of-pocket costs may be a significant financial barrier to care, particularly for cancer survivors with multiple comorbidities.
There is a dearth of published studies that quantified the economic burden of multiple chronic conditions among cancer survivors, with the economic impact of several common chronic and most costly conditions not previously examined.
No published studies have examined lost productivity resulting from comorbidities among cancer survivors.
Acknowledgments
Funding
This paper was not funded.
Appendix
Earliest publication date: January 1, 2000
Date of last search: January 27, 2016
Language: English
Publication status: published studies
Search Strategy:
PUBMED
Search (Neoplasms[mesh] OR Neoplasm*[tw] OR Cancer*[tw]) AND (Chronic Disease*[tw] OR Chronic Condition*[tw] OR Chronic Illness*[tw] OR Chronically Ill[tw] OR Comorbid*[tw] OR Co morbid*[tw] OR Multimorbid*[tw] OR Multi morbid*[tw] OR Multiple Morbidit*[tw] OR Symptom burden*[tw] OR High Blood Pressure*[tw] OR Hypertension* [tw] OR Hyperlipidemias[Mesh] OR Hyperlipidemia*[tw] OR High Blood Cholesterol[tw] OR Arthritis[Mesh] OR Arthritis[tw] OR Diabetes[tw] OR Diabetic*[tw] OR Prediabetic*[tw] OR Metabolic Syndrome[tw] OR Cardiovascular Diseases[Mesh] OR Cardiovascular Disease*[tw] OR Heart Disease*[tw] OR Heart Attack*[tw] OR Myocardial Infarction*[tw] OR Mood Disorders[Mesh] OR Depression[tw] OR Bipolar[tw] OR Anxiety Disorders [Mesh] OR Stress[tw] OR Distress[tw] OR Sinusitis[tw] OR Asthma[tw] OR ‘Pulmonary Disease, Chronic Obstructive’[Mesh] OR Chronic Obstructive Lung Disease*[tw]) AND (Cost[tw] OR Costs[tw] OR Economic*[tw] OR Expenditure*[tw] OR Productivity[tw] OR Financial burden*[tw]) AND ((Medical Expenditure*[tw] AND Panel Survey[tw]) OR MEPS[tw] OR ((Health care Cost*[tw] OR Healthcare Cost*[tw]) AND Utilization Project [tw]) OR HCUP[tw] OR Nationwide Inpatient Sample*[tw] OR NIS[tw] OR State Inpatient Database*[tw] OR Medicare[tw] OR Medicaid[tw] OR Health Interview Survey*[tw] OR NHIS[tw] OR Behavioral Risk Factor Surveillance System[tw] OR BRFSS[tw] OR Surveillance Epidemiology and End Results [tw] OR SEER[tw] OR Cancer Survivor Study[tw] OR Livestrong[tw] OR Claim Data[tw] OR Claims Data[tw] OR Health and Retirement Study[tw] OR National Cancer Data Base[tw] OR National Cancer Database[tw] OR Cancer regist*[tw] OR MarketScan[tw] OR Market Scan[tw] OR Insurance [tw] OR Health Plan*[tw] OR HealthPlan*[tw] OR Retrospective[tw] OR Chart review*[tw]) NOT (Animals[mesh] NOT Humans [mesh]) Filters: Publication date from 2000/01/01; English
Web of Science
TOPIC: (Neoplasm* OR Cancer*) AND TOPIC: (Chronic Disease* OR Chronic Condition* OR Chronic Illness* OR Chronically Ill OR Comorbid* OR Co morbid* OR Multimorbid* OR Multi morbid* OR Multiple Morbidit* OR Symptom burden* OR High Blood Pressure* OR Hypertension* OR Hyperlipidemia* OR High Blood Cholesterol OR Arthritis OR Diabetes OR Diabetic* OR Prediabetic* OR Metabolic Syndrome OR Cardiovascular Disease* OR Heart Disease* OR Heart Attack* OR Myocardial Infarction* OR Mood Disorder* OR Depression OR Bipolar OR Anxiety Disorder* OR Stress OR Distress OR Sinusitis OR Asthma OR Chronic Obstructive Pulmonary Disease* OR Chronic Obstructive Lung Disease*) AND TOPIC: (Cost OR Costs OR Economic* OR Expenditure* OR Productivity OR Financial burden*) AND TOPIC: (Medical Expenditure Panel Survey OR MEPS OR Healthcare Cost AND Utilization Project OR HCUP OR Nationwide Inpatient Sample* OR NIS OR State Inpatient Database* OR Medicare OR Medicaid OR Health Interview Survey* OR NHIS OR Behavioral Risk Factor Surveillance System OR BRFSS OR Surveillance Epidemiology and End Results OR SEER OR Cancer Survivor Study OR Livestrong OR Claim Data OR Claims Data OR Health and Retirement Study OR National Cancer Data Base OR National Cancer Database OR Cancer regist* OR MarketScan OR Market Scan OR Health insurance OR Health Plan* OR HealthPlan* OR Retrospective OR Chart review*)
EconLit
(Neoplasm* OR Cancer*) AND (Chronic Disease* OR Chronic Condition* OR Chronic Illness* OR Chronically Ill OR Comorbid* OR Co morbid* OR Multimorbid* OR Multi morbid* OR Multiple Morbidit* OR Symptom burden* OR High Blood Pressure* OR Hypertension* OR Hyperlipidemia* OR High Blood Cholesterol OR Arthritis OR Diabetes OR Diabetic* OR Prediabetic* OR Metabolic Syndrome OR Cardiovascular Disease* OR Heart Disease* OR Heart Attack* OR Myocardial Infarction* OR Mood Disorder* OR Depression OR Bipolar OR Anxiety Disorder* OR Stress OR Distress OR Sinusitis OR Asthma OR Chronic Obstructive Pulmonary Disease* OR Chronic Obstructive Lung Disease*) AND (Cost OR Costs OR Economic* OR Expenditure* OR Productivity OR Financial burden*)
Abstraction Criteria
Excluded if:
Title or abstract does NOT contain some indication of ‘cost,’ ‘comorbidities,’ or ‘cancer.’
The focus is a specific (single) procedure costs (i.e. cost of surgery X among Y cancer patients). [Note that general ‘cancer treatment’ is ok.]
Cost is a part of cost-effectiveness or comparative-effectiveness studies.
Non-US. (Patient populations outside the United States.)
Publication prior to 2000.
Non-English articles.
Review articles.
Non-adult cancer populations.
Included if:
Costs related to comorbid conditions in cancer survivors (all patients who have ever been diagnosed with cancer).
Costs = health-care treatment costs; financial burden to patient or society; cost of lost productivity.
Footnotes
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
Papers of special note have been highlighted as of interest (•) to readers.
- 1.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivor-ship statistics, 2016. CA Cancer J Clin. 2016;66:271–289. doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- 2.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103(2):117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerteis J, Izrael D, Deitz D, et al. Multiple chronic conditions chart-book. MD: Agency for Healthcare Research and Quality, Rockville; 2014. Apr 30, [Google Scholar]
- 4.Hudson SV, Miller SM, Hemler J, et al. Cancer survivors and the patient-centered medical home. Transl Behav Med. 2012;2(3):322–331. doi: 10.1007/s13142-012-0138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogle KS, Swanson GM, Woods N, et al. Cancer and comorbidity: redefining chronic diseases. Cancer. 2000;88(3):653–663. doi: 10.1002/(sici)1097-0142(20000201)88:3<653::aid-cncr24>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Edwards BK, Noone AM, Mariotto AB, et al. Annual report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120(9):1290–1314. doi: 10.1002/cncr.28509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edgington A, Morgan MA. Looking beyond recurrence: comorbidities in cancer survivors. Clin J Oncol Nurs. 2011;15(1):E3–E12. doi: 10.1188/11.CJON.E3-E12. [DOI] [PubMed] [Google Scholar]
- 8.Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33(7):1674–1685. doi: 10.2337/dc10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis. 2014;11:E62. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guy GP, Jr, Yabroff KR, Ekwueme DU, et al. Healthcare expenditure burden among non-elderly cancer survivors, 2008–2012. Am J Prev Med. 2015;49(6 Suppl 5):S489–S497. doi: 10.1016/j.amepre.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yabroff KR, Dowling EC, Guy GP, Jr, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259–267. doi: 10.1200/JCO.2015.62.0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zheng Z, Yabroff KR, Guy GP, Jr, et al. Annual medical expenditure and productivity loss among colorectal, female breast, and prostate cancer survivors in the United States. J Natl Cancer Inst. 2016;108(5):djv382. doi: 10.1093/jnci/djv382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ekwueme DU, Yabroff KR, Guy GP, Jr, et al. Medical costs and productivity losses of cancer survivors–United States, 2008–2011. MMWR Morb Mortal Wkly Rep. 2014;63(23):505–510. [PMC free article] [PubMed] [Google Scholar]
- 14.Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(11 Suppl):2577–2592. doi: 10.1002/cncr.23448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoekstra RA, Heins MJ, Korevaar JC. Health care needs of cancer survivors in general practice: a systematic review. BMC Fam Pract. 2014;15(1):94. doi: 10.1186/1471-2296-15-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yabroff KR, Guy GP, Jr, Ekwueme DU, et al. Annual patient time costs associated with medical care among cancer survivors in the United States. Med Care. 2014;52(7):594–601. doi: 10.1097/MLR.0000000000000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kent EE, Arora NK, Rowland JH, et al. Health information needs and health-related quality of life in a diverse population of long-term cancer survivors. Patient Educ Couns. 2012;89(2):345–352. doi: 10.1016/j.pec.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenbaum S. The patient protection and affordable care act: implications for public health policy and practice. Public Health Rep. 2011;126(1):130–135. doi: 10.1177/003335491112600118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Patient Protection and Affordable Care Act. Pub. L. No. 111–148. 2010 Mar 23;124.
- 20.Soni A. Statistical Brief #471. Rockville (MD): Agency for Healthcare Research and Quality; 2015. Apr, Top five most costly conditions among adults age 18 and older, 2012: Estimates for the U.S. Civilian Noninstitutionalized Adult Population. Available from: http://www.meps.ahrq.gov/mepsweb/data_files/publications/st471/stat471.shtml. [PubMed] [Google Scholar]
- 21•.Subramanian S, Tangka FK, Sabatino SA, et al. Impact of chronic conditions on the cost of cancer care for Medicaid beneficiaries. Medicare Medicaid Res Rev. 2012;2(4):E1–E21. doi: 10.5600/mmrr.002.04.a07. This article is included in Tables 1, 2, and 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lund JL, Yabroff KR, Ibuka Y, et al. Inventory of data sources for estimating health care costs in the United States. Med Care. 2009;47(7 Suppl 1):S127–S142. doi: 10.1097/MLR.0b013e3181a55c3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. BMJ. 1994;309(6964):1286–1291. doi: 10.1136/bmj.309.6964.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24•.Bernard DS, Farr SL, Fang Z. National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol. 2011;29(20):2821–2826. doi: 10.1200/JCO.2010.33.0522. This article is included in Tables 1 and 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25•.Boltz MM, Hollenbeak CS, Schaefer E, et al. Attributable costs of differentiated thyroid cancer in the elderly Medicare population. Surgery. 2013;154(6):1363–1369. doi: 10.1016/j.surg.2013.06.042. discussion 1369–1370. This article is included in Tables 1 and 3. [DOI] [PubMed] [Google Scholar]
- 26•.Cohen JW, Krauss NA. Spending and service use among people with the fifteen most costly medical conditions, 1997. Health Aff (Millwood) 2003;22(2):129–138. doi: 10.1377/hlthaff.22.2.129. This article is included in Tables 1, 3, and 4. [DOI] [PubMed] [Google Scholar]
- 27•.Davidoff AJ, Erten M, Shaffer T, et al. Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 2013;119(6):1257–1265. doi: 10.1002/cncr.27848. This article is included in Table 1 and Table 5. [DOI] [PubMed] [Google Scholar]
- 28•.Forde GK, Chang J, Ziogas A, et al. Costs of treatment for elderly women with advanced ovarian cancer in a Medicare population. Gynecol Oncol. 2015;137(3):479–484. doi: 10.1016/j.ygyno.2015.03.050. This article is included in Tables 1 and 3. [DOI] [PubMed] [Google Scholar]
- 29•.Han X, Lin CC, Li C, et al. Association between serious psychological distress and health care use and expenditures by cancer history. Cancer. 2015;121(4):614–622. doi: 10.1002/cncr.29102. This article is included in Tables 1 and 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30•.Hollenbeak CS, Kulaylat AN, Mackley H, et al. Determinants of medicare costs for elderly patients with oral cavity and pharyngeal cancers. JAMA Otolaryngol Head Neck Surg. 2015;141(7):628–635. doi: 10.1001/jamaoto.2015.0940. This article is included in Tables 1 and 3. [DOI] [PubMed] [Google Scholar]
- 31•.Hollenbeak CS, Nikkel LE, Schaefer EW, et al. Determinants of medicare all-cause costs among elderly patients with renal cell carcinoma. J Manag Care Pharm. 2011;17(8):610–620. doi: 10.18553/jmcp.2011.17.8.610. This article is included in Tables 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32•.Hollenbeak CS, Stack BC, Jr, Daley SM, et al. Using comorbidity indexes to predict costs for head and neck cancer. Arch Otolaryngol Head Neck Surg. 2007;133(1):24–27. doi: 10.1001/archotol.133.1.24. This article is included in Tables 1 and 3. [DOI] [PubMed] [Google Scholar]
- 33•.Luo Z. Colon Cancer Treatment Costs for Medicare and Dually Eligible Beneficiaries. Health Care Financ Rev. 2009;31(1):35–50. This article is included in Tables 1 and 5. [PMC free article] [PubMed] [Google Scholar]
- 34•.Pan X, Sambamoorthi U. Health care expenditures associated with depression in adults with cancer. J Community Support Oncol. 2015;13(7):240–247. doi: 10.12788/jcso.0150. This article is included in Tables 1 and 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yabroff KR, Borowski L, Lipscomb J. Economic studies in colorectal cancer: challenges in measuring and comparing costs. J Natl Cancer Inst Monogr. 2013;46:62–78. doi: 10.1093/jncimonographs/lgt001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Banegas MP, Guy GP, Jr, De Moor JS, et al. For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff (Millwood) 2016;35(1):54–61. doi: 10.1377/hlthaff.2015.0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blumberg LJ, Waidmann TA, Blavin F, et al. Trends in health care financial burdens, 2001 to 2009. Milbank Q. 2014;92(1):88–113. doi: 10.1111/1468-0009.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meropol NJ, Schrag D, Smith TJ, et al. American society of clinical oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009;27(23):3868–3874. doi: 10.1200/JCO.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 39.National Cancer Policy Forum; Board on Health Care Services; Institute of Medicine. Workshop Summary. Washington (DC): National Academies Press (US); 2014. Dec 23, Ensuring patient access to affordable cancer drugs: workshop summary. [cited 2016 May 2]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK268684/Accessed. [PubMed] [Google Scholar]
- 40.Leroy L, Bayliss E, Domino M, et al. The agency for healthcare research and quality multiple chronic conditions research network: overview of research contributions and future priorities. Med Care. 2014;52(Suppl 3):S15–S22. doi: 10.1097/MLR.0000000000000095. [DOI] [PubMed] [Google Scholar]
- 41.Grembowski D, Schaefer J, Johnson KE, et al. A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med Care. 2014;52(Suppl 3):S7–S14. doi: 10.1097/MLR.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 42.Page RD, Newcomer LN, Sprandio JD, et al. The patient-centered medical home in oncology: from concept to reality. Am Soc Clin Oncol Educational Book /ASCO. Am Soc Clin Oncology Meet. 2015;35:e82–e89. doi: 10.14694/EdBook_AM.2015.35.e82. [DOI] [PubMed] [Google Scholar]
- 43.Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff (Millwood) 2010;29(4):718–724. doi: 10.1377/hlthaff.2009.0474. [DOI] [PubMed] [Google Scholar]
- 44.U.S. Department of Health and Human Services. Multiple chronic conditions – a strategic framework: optimum health and quality of life for individuals with multiple chronic conditions. Washington (DC): U.S. Department of Health and Human Services; 2010. Dec, [Google Scholar]
- 45.Anderson G. Chronic care: making the case for ongoing care. Princeton (NJ): Robert Wood Johnson Foundation; 2010. [Google Scholar]
- 46.Warren JL, Klabunde CN, Schrag D, et al. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8 Suppl):IV-3–18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 47.Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(7 Suppl 1):S44–S50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 48.Byrne J, Kessler LG, Devesa SS. The prevalence of cancer among adults in the United States: 1987. Cancer. 1992;69(8):2154–2159. doi: 10.1002/1097-0142(19920415)69:8<2154::aid-cncr2820690823>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 49.Hewitt M, Breen N, Devesa S. Cancer prevalence and survivorship issues: analyses of the 1992 National health interview survey. J Natl Cancer Inst. 1999;91(17):1480–1486. doi: 10.1093/jnci/91.17.1480. [DOI] [PubMed] [Google Scholar]
- 50.Guy GP, Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31(30):3749–3757. doi: 10.1200/JCO.2013.49.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dowling EC, Chawla N, Forsythe LP, et al. Lost productivity and burden of illness in cancer survivors with and without other chronic conditions. Cancer. 2013;119:3393–3401. doi: 10.1002/cncr.28214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yabroff KR, Warren JL, Banthin J, et al. Comparison of approaches for estimating prevalence costs of care for cancer patients: what is the impact of data source? Med Care. 2009;47(7 Suppl 1):S64–S69. doi: 10.1097/MLR.0b013e3181a23e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Howlader N, Noone AM, Krapcho M, et al., editors. SEER cancer statistics review. Bethesda (MD): National Cancer Institute; Apr, 2015. 1975–2012 Available from: http://seer.cancer.gov/csr/1975_2012/. Based on November 2014 SEER data submission, posted to the SEER web site. [Google Scholar]
- 54.Weir HK, Thompson TD, Soman A, et al. Meeting the healthy people 2020 objectives to reduce cancer mortality. Prev Chronic Dis. 2015;12:E104. doi: 10.5888/pcd12.140482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rim SH, Hall IJ, Fairweather ME, et al. Considering racial and ethnic preferences in communication and interactions among the patient, family member, and physician following diagnosis of localized prostate cancer: study of a US population. Int J Gen Med. 2011;4:481–486. doi: 10.2147/IJGM.S19609. [DOI] [PMC free article] [PubMed] [Google Scholar]