Abstract
Purpose
The purpose of this study was to perform a systematic review and meta-analysis of prospective cohort studies that examined the relationship between anxiety disorders, or clinically significant anxiety symptoms, at baseline and all-cause mortality at follow-up relative to control participants without clinically significant anxiety.
Methods
PubMed, EMBASE, PsycInfo and CINAHL were searched through July 2015, along with manual searches of published reviews and forward and backward snowball searches of included studies. Studies were excluded if anxiety was not defined with a standardized instrument, or if participants were followed up for one year or less. The initial search yielded 7,901 articles after removal of duplicates, of which 328 underwent full-text screening.
Results
Forty-two estimates from 36 articles were included in the meta-analysis with a total sample of 127,552 participants and over 11,573 deaths. The overall Hazard Ratio (HR) estimate of mortality in clinically anxious participants relative to controls was 1.09 (95% CI: 1.01–1.16), however this was reduced after adjusting for publication bias (1.03; 95% CI: .95–1.13). There was no evidence of increased mortality risk among anxious participants derived from community samples (0.99; 95% CI: 0.96–1.02) and in studies that adjusted for a diagnosis of depression (1.01; 95% CI: 0.96–1.06).
Conclusions
These findings suggest that positive associations in the literature are attributable to studies in smaller samples, comorbid depression (or other psychiatric conditions) among participants, and possible confounding in medical patient samples followed up for short durations.
Keywords: Anxiety disorders, anxiety, death, mortality, survival
Anxiety disorders are among the most prevalent and disabling mental health conditions across the globe [1–5], but the relationship between anxiety disorders and mortality is uncertain. Some studies have reported increased mortality risk [6, 7], whereas others have reported no increase in risk [8, 9], and some forms of anxiety have been associated with lower risk of death [8, 10].
A recent meta-analysis that assessed the relationship between mental disorders and all-cause mortality observed that anxiety disorders are associated with an increased risk of death [11]. However, this study was criticized for a number of methodological shortcomings; for example, drawing inferences to the general population on the basis of a large number of studies conducted in patient samples [12]. Another recent meta-analysis that addressed the relationship between psychological distress and all-cause mortality also observed an increased risk of death among those with symptoms of anxiety and depression [13]. However this study was unable to disentangle the relative effects of anxiety and depression. Depression has been repeatedly found to be associated with an increased risk of death [11, 14–16], and at least two independent studies have reported that mortality among individuals with comorbid depression and anxiety is attributable to depression [9, 17]. A more detailed understanding of the association between clinically significant anxiety and mortality is critical for evidence-based service provision and clinical decision-making.
The purpose of this study was to estimate the association between anxiety disorders, or clinically significant anxiety symptoms, and all-cause mortality by combining the results obtained from prospective cohort studies. The term ‘clinically significant’ is used to denote that anxiety symptoms were sufficient to meet the validated diagnostic threshold of the instrument. Three significant sources of uncertainty surrounding the relationship between anxiety and all-cause mortality include the population from which samples have been drawn; whether diagnoses were obtained from standardized clinical interviews or questionnaires; and whether depression was adjusted for. In this analysis, we address how the risk of all-cause mortality associated with clinically significant anxiety varies across these study characteristics.
Method
Search Strategy
We conducted this study according to the MOOSE guidelines for Meta-Analyses and Systematic Reviews of Observational Studies [18], and prospectively registered it with PROSPERO (CRD42015024706). We developed a search strategy for PubMed combining MeSH and open terms for anxiety, mortality, and prospective study design, which was later translated for other databases (EMBASE, PsycInfo, and CINAHL). Data Supplement 1 presents the search strategy for all of the databases. Searches were conducted in English through July 2015. We also hand-searched the references of previously published systematic reviews for additional articles [11, 19–21]. A forward snowball search of all included studies was conducted in January 2016 using Google Scholar, to identify studies that may have been published up to six months after our initial search, and a backward snowball search was conducted to identify studies that the original search may have missed.
Study Selection
We included observational studies that assessed anxiety at baseline and all-cause mortality at follow-up using a prospective design, focusing on studies that measured anxiety disorders or symptoms using standardized structured clinical interviews or self-report questionnaires validated against standardized structured clinical interviews. We excluded studies that did not use standardized instruments with valid definitions to diagnose anxiety and studies that did not include an asymptomatic control group. We also excluded studies with a follow up period of one year or less in order to attenuate confounding from other potential proximal causes of mortality, such as a terminal physical illness which would be associated with anxiety. Although all of the studies included in the present review reported Hazard Ratio (HR) estimates, we did not place an initial restriction against studies that did not report time-based measures of association based on survival analyses. Following removal of duplicate records and an initial screen of all titles by one reviewer to discard irrelevant publications (BM), two independent reviewers examined each study abstract against the inclusion criteria (BM or AB or DGB). All disagreements were resolved through discussion.
Data Extraction and Quality Assessment
Two reviewers (BM or DGB or AB) independently extracted information about the country in which the study was conducted, sample size and characteristics, diagnostic instrument and anxiety sub-type or cut-off scores used, prevalence of anxiety, mortality ascertainment, total follow-up period, and adjustment for other variables using a data extraction form developed for this systematic review. Hazard Ratios (HR) and 95% confidence intervals were extracted for each study. We contacted authors of included records by email up to three times to obtain further information (e.g., clarification of definition of anxiety, missing or unreported data). Multiple estimates were included from a single study if they were not overlapping (e.g., from different data sets, or analyses were conducted in males and females separately). If multiple estimates were based on different sub-types or clinical interviews, only the most inclusive estimate was retained due to concerns about collinearity. Otherwise, if there were multiple estimates according to the same clinical definition, we opted for the most adjusted estimate, the estimate derived using the longest follow-up period, or using the cutoff score with the best overall psychometric properties against diagnostic interviews. We assessed methodological quality through a set of questions covering clear description of inclusion criteria, number of dropouts (non-mortality), adjustment for potential confounders, group allocation, and appropriateness of statistical analyses. Quality assessment was conducted using a modified version of the Newcastle-Ottawa Quality Assessment Scale [22] (See Data Supplement 2).
Meta-Analyses
HRs were categorized according to the study sample (institutionalized/patient samples or not) and type of diagnostic instrument (interview vs. questionnaire). Random-effects meta-analysis models were used to estimate pooled HR estimates [23]. The I2 statistic was used to estimate the percentage of the total variation in effect sizes across studies attributable to heterogeneity [24]. Sub-group analyses were conducted according to sample type (community, patient, and veterans), diagnostic instrument (interview vs. questionnaire), and adjustment for depression.
Egger’s test was used to indicate whether there was a bias of effect estimates (natural log of HR) relative to the precision of those estimates (standard error of the log of HR) [25]. Duval & Tweedie’s [26] trim-and-fill method was used to account for publication bias by first removing biased estimates from the sample, and then refilling those estimates along with their “missing” counterparts imputed so as to maintain symmetry in the funnel plot. Finally, a sensitivity analysis was performed using random-effects meta-regression to examine the association of follow-up period with effect size (natural log of HR) in patient samples.
Results
The literature search of four databases and systematic reviews yielded 10,359 articles. After removal of duplicate records, 7,901 abstracts were screened and 328 articles met eligibility criteria. These full-text articles were screened and 45 eligible studies were subsequently extracted and quality assessed. Of those, seven articles were excluded from the meta-analysis because of overlapping data with other articles, and two studies were excluded due to missing estimates. Forty-two estimates from 36 articles were included in the final meta-analysis [6–9, 27–58]. See Data Supplement 3 for flow chart of included studies.
Twenty-three estimates were based on medical patient samples, 15 were based on community samples, and four on veteran samples. Thirty estimates were obtained using self-report questionnaires, and 12 from structured diagnostic interviews. Thirty-four HRs were adjusted for covariates, and eight were not. Of those adjusted for covariates, 11 adjusted for comorbid depression. Eighteen studies had follow up periods of 5 years or less, 14 studies had follow up periods between 6 and 10 years, and 10 studies had follow up periods of over 10 years. Twenty-five out of 36 studies were based in Europe, 6 in the USA, 4 in Australia, and one in China (See Data Supplement 4 for list of specific European countries by publication). The meta-analysis was based on 127,552 participants and over 11,573 deaths.
The overall pooled estimate of HR for all-cause mortality among people with anxiety disorders or clinically significant anxiety was 1.09 (95% CI: 1.01–1.16). The summary HRs were 1.79 (95% CI: 1.41–2.16) among veteran samples, 1.14 (95% CI: 0.98–1.30) among patient samples, and 0.99 (95% CI: 0.96–1.02) among community samples (See Figure 1). Stratifying the analyses by adjustment for depression indicated that anxiety was positively associated with all-cause mortality when depression was unadjusted for (HR: 1.18; 95% CI: 1.05–1.31), however there was no evidence of an association between anxiety and all-cause mortality in studies adjusting for depression (HR: 1.01; 95% CI: 0.96–1.06).
Figure 1.
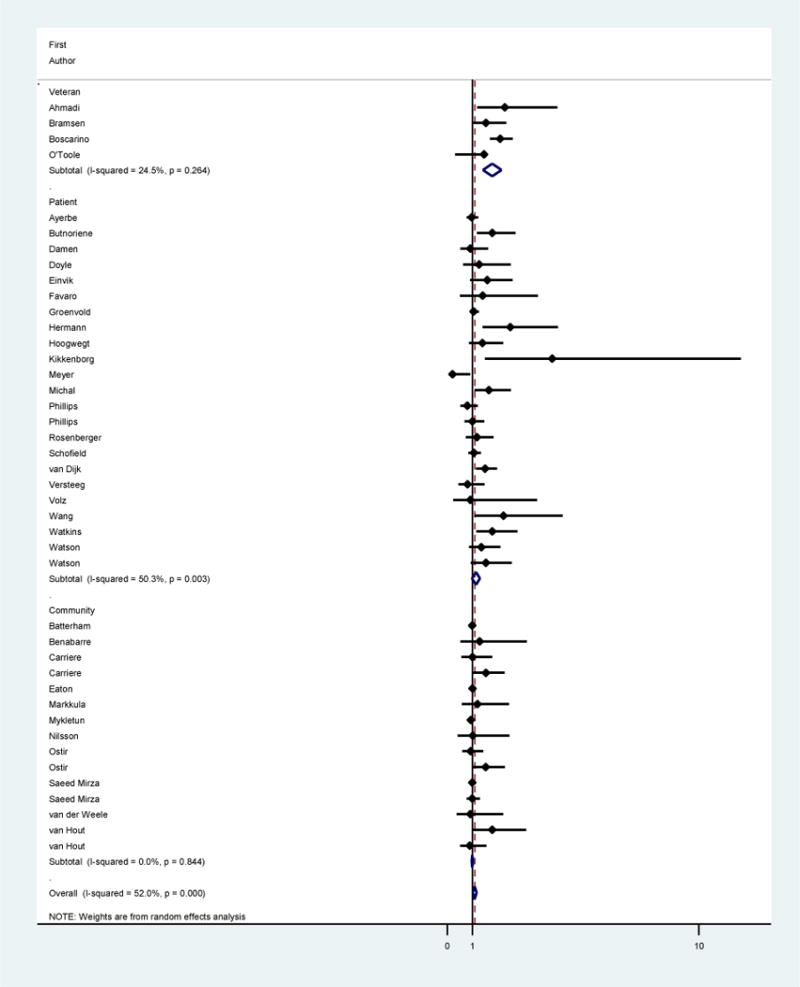
Hazard Ratios and 95% confidence intervals for clinically significant anxiety and all-cause mortality by sample type (veteran, patient, and community).
There was a moderate degree of heterogeneity between studies (I2 = 52%). Significant heterogeneity was observed between studies that did not adjust for depression (I2 = 62%), those that defined anxiety using self-report questionnaires (I2 = 60%), adjusted for covariates (I2 = 58%), and were based on patient samples (I2 = 50%). No heterogeneity was observed in studies adjusting for depression, nor in studies conducted in community samples.
A funnel plot and results of Egger’s test (p<0.01) suggested a publication bias favoring small studies with large, positive associations (see Data Supplement 5). Using a trim and fill method [26], eleven estimates were imputed to adjust for missing studies. As a result, the overall HR was reduced to 1.03 (95% CI: .95–1.13).
Sensitivity Analyses
A series of sensitivity analyses was conducted in order to better understand the factors contributing to heterogeneity in this study, and their impact on the overall HR estimate. Studies based on regression models that adjusted for covariates were found to account for significant heterogeneity in the present study, however no heterogeneity was observed in studies that adjusted for depression and in estimates obtained from unadjusted models. Therefore, we compared estimates from models that adjusted for depression (among other variables) to models that were generally adjusted for covariates (excluding depression). Estimates based on unadjusted models (HR: 1.04; 95% CI: 0.89–1.19) and on models adjusted for depression (HR: 1.01; 95% CI: 0.96–1.06) were not associated with mortality, and displayed no heterogeneity. However, models that adjusted for covariates that excluded depression were positively associated with mortality (HR: 1.23; 95% CI: 1.07–1.40), and exhibited the most substantial heterogeneity that was observed in the present study (I2=69%). When we replaced 17 of the most adjusted estimates with their unadjusted, or less adjusted counterparts, we found that the overall HR did not change. Removal of two outliers did not have a significant impact on these results either.
Second, although we did not initially intend to exclude any study based on the type of estimate that was used (e.g., HR, OR, or RR), all but four estimates used survival analysis methodology to estimate HRs adjusted for time-to-event and censorship [59–62]. We decided to exclude these four estimates (three ORs and one RR) from the primary analysis due to concerns about their comparability with the HR estimates. Repeating the analyses with the inclusion of these estimates increased the effect size by .01 after adjustment for publication bias and did not significantly influence these results.
Third, all four estimates obtained from veteran samples, and a fifth estimate based on a medical sample, were based on a diagnosis of PTSD, which is no longer classified as an anxiety disorder in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorder (DSM-5). Repeating the analysis with the exclusion of these estimates increased the overall HR by .01 after adjustment for publication bias and did not significantly influence the overall pattern of results.
Finally, a random-effects meta-regression analysis was conducted in order to examine the relationship between follow-up periods and effect sizes. We expected that shorter follow-up periods would be associated with larger effect sizes specifically in medical patient samples, due to the influence of other proximal variables on mortality. A second-degree fractional polynomial (P1 = −.5, P2 = −.5) provided the best fit, indicating a decline in effect sizes up to approximately 5 years in patient samples (See Figure 2). The results of piecewise random-effects meta-regression analyses split at 5 years of follow-up indicated a significant decrease in effect size with increasing follow-up period up to 5 years (β = −.23; 95% CI: −.37, −.09; p=0.004), and no association between follow-up period and effect size 5 years and after (β = .01; 95% CI: −.02, .04; p=0.5). No statistically significant relationship between follow-up period and effect size was observed in community samples.
Figure 2.
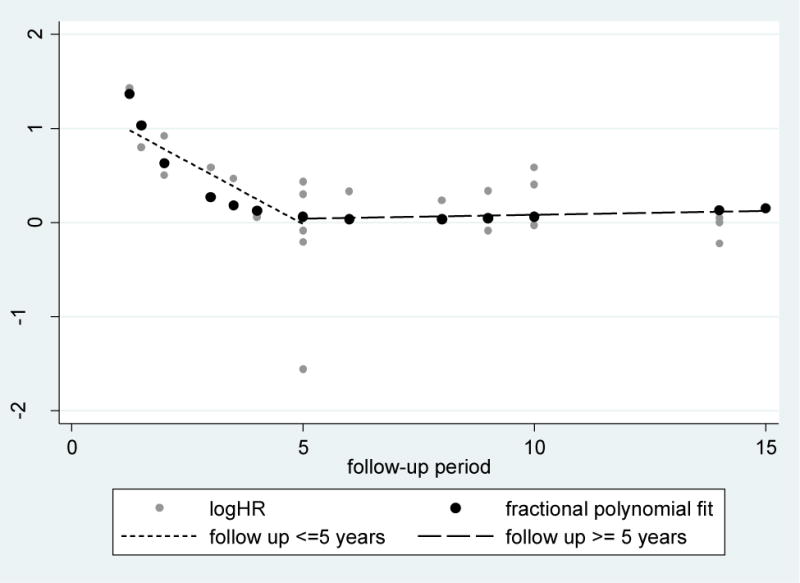
Relationship of the HR (natural log) of all-cause mortality and follow-up period in the 23 patient samples included in the meta-analysis. The association is modeled by a second-degree fractional polynomial and by piecewise linear terms up to and after five years of follow-up.
Discussion
We conducted a systematic review and meta-analysis of prospective cohort studies that reported HRs of the association between anxiety disorders, or clinically significant anxiety symptoms, and all-cause mortality. The overall HR indicated that anxiety was positively associated with mortality; however, this was not the case after adjusting for publication bias. Sub-group analyses revealed no evidence of increased mortality risk in community samples, or in studies that adjusted for depression. The largest heterogeneity that was observed was among studies that did not adjust for depression, and among studies based on adjusted models (particularly, those that adjusted for covariates excluding depression).
Anxiety is among the most prevalent mental disorders in the world [1, 3], and has been estimated to account for approximately 15% of disability-adjusted life years (DALYs) attributable to mental disorders [4]. The finding that anxiety is not associated with mortality after adjustment for depression suggests that the mortality risk attributable to anxiety in the unadjusted studies may be due to comorbid depression. Indeed, anxiety and depression have been found to co-occur substantially, as measured during the past-year or over the lifetime [63–65], and a number of studies have found that depression is independently associated with an increased risk of death [11, 14–16, 20]. Several studies have also found that depression accounts for higher proportions of the global burden of disease than anxiety, as measured by DALYs and annual expenditures [4, 66]. However, it is also possible that depression among individuals with anxiety is a better indicator of other comorbidities, such as substance disorders, that are also substantially associated with disease and mortality [4, 8].
There was no evidence of an association between anxiety and mortality in community samples, however a positive association was observed in veteran samples and a positive trend was observed in patient samples. One explanation of these findings is that anxiety might exacerbate outcomes particularly among individuals of poorer health, or that anxiety may be associated with increased risk of some medical conditions that mediate the link with mortality. For example, anxiety may be associated with increased risk of incident cardiovascular and metabolic diseases [67, 68]. A similar explanation could also be invoked for the findings in veterans: one of the four veteran samples consisted of outpatients [27], and the other three consisted of Vietnam War or World War II veterans [6, 31, 46]. Veterans have generally been found to have poorer overall health and health behaviors relative to civilians and army reserve members [69], potentially explaining the highest risk of mortality associated with anxiety observed in this group. Additionally, all of the veteran samples were assessed only for PTSD, which, although no longer categorized as an anxiety disorder in the DSM-5, may have a stronger association with mortality than the other exposures in this study.
A second possibility is that the increased mortality risk observed in veteran and patient samples is not due to anxiety. Individuals with poorer health status are at higher risk of mortality irrespective of anxiety, and anxiety may reflect poorer health. For example, the prevalence of anxiety is pronounced in medical samples [70–76], and those with recently diagnosed illnesses tend to report higher anxiety symptoms [77–79]. Finally, these findings may also be attributable to depression: whereas eight out of 15 studies in community samples adjusted for depression, only three out of 23 of the studies conducted in patient samples and none of the veteran samples adjusted for depression. Indeed, a recent meta-analysis of studies conducted in transplant patients found that whereas depression was associated with increased mortality risk, anxiety was not [20].
There was also evidence of a publication bias of studies addressing the relationship of anxiety and all-cause mortality, such that smaller studies more frequently reported larger HR estimates. After adjusting for this publication bias, there was no evidence of a significant effect of anxiety on mortality. Exploratory analyses indicated that studies conducted in patient samples with up to 5 years of follow-up tended to have inflated effect estimates, possibly due to confounding from other proximal influences on mortality.
The comprehensive search strategy employed in the present study is a significant strength: only prospective cohort studies that reported using validated diagnostic instruments to measure anxiety, and included asymptomatic controls, with greater than one-year follow-up and that adjusted for time-to-event were included. However, the stringency of our criteria sometimes led to the exclusion of otherwise high quality studies, and as a result we were unable to examine how estimates vary as a result of other study characteristics and outcomes. For example, some otherwise strong studies did not report using standardized instruments or valid definitions to diagnose clinically significant anxiety symptoms [80, 81], ascertained anxiety retrospectively [82], or assessed mortality by specific causes [83]. Additionally, some studies in patient samples that used valid measures of anxiety and used prospective designs were excluded because they combined clinically adverse events with mortality as the main outcome [84, 85]. It is possible that anxiety disorders are associated with increased risk of mortality due to some specific causes; for example, suicide attempts [86, 87]. Anxiety does not appear to be associated with increased mortality among patients with coronary heart disease [19], despite the results of one meta-analysis suggesting that anxiety is associated with higher incidence of coronary heart disease [67]. However, depression has been found to be associated with increased risk of mortality among patients with coronary heart disease [88].
More work is needed to investigate the relative contributions of depression and anxiety to disease outcomes and all-cause and cause-specific mortality. Specifically, due to the frequent co-occurrence of these disorders, it is important for future work to adjust for one disorder when addressing the relationship of the other with incident physical conditions, adverse medical outcomes, or mortality risk. It is also important for future studies to assess the role of substance use [89–93], physical activity [94, 95], inflammatory markers, diet and other potential intermediary variables. Previous studies have reported that such behavioral and biologic variables mediate the relationship between depression and all-cause mortality [96, 97], however whether these also explain the relationship between anxiety and all-cause mortality has to our knowledge remained unexplored.
It is possible that the relationship of anxiety and mortality depends on the nature of the anxiety. Obsessive-compulsive disorder, although no longer classified as an anxiety disorder by the DSM-5, captures anxiety-related characteristics that may be associated with lower risk of death because the individual is more likely to take protective actions [8, 98, 99]. Other anxiety disorders may be associated with higher risk of mortality, such as panic disorder, associated with strong physiological activity; blood illness phobia, associated with avoidance of preventive medical treatment; or agoraphobia, associated with both possibilities. The resulting mixture of all types of anxiety disorders, of necessity the focus of this review, may have contributed to the null result found in this study.
Relative to asymptomatic controls, there was no evidence of an increased risk of mortality among individuals with anxiety disorders or clinically significant anxiety symptoms. These findings were obtained with the highest consistency in community samples and when depression was adjusted for, suggesting that the positive association between anxiety and mortality in some studies may be attributable to comorbid depression, or to other medical comorbidities among studies conducted in veteran and patient samples.
Supplementary Material
Acknowledgments
We thank Lori Rosman for her assistance with the literature search, and the various authors who responded to our requests for data or for additional information. This work was supported by the Johns Hopkins Epidemiology and Biostatistics of Aging Training Program of the NIA under award number T32AG000247, and NIDA grant 026652 to Dr. Eaton.
Footnotes
Conflicts of Interest: None.
References
- 1.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- 2.Baxter AJ, Vos T, Scott KM, et al. The global burden of anxiety disorders in 2010. Psychol Med. 2014;44:2363–2374. doi: 10.1017/S0033291713003243. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- 4.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 5.Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Boscarino JA. Posttraumatic Stress Disorder and mortality among U.S. army veterans 30 years after military service. Ann Epidemiol. 2006;16:248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk MR, Utens EMWJ, Dulfer K, et al. Depression and anxiety symptoms as predictors of mortality in PCI patients at 10 years of follow-up. Eur J Prev Cardiol. 2015 doi: 10.1177/2047487315571889. [DOI] [PubMed] [Google Scholar]
- 8.Eaton WW, Roth KB, Bruce M, et al. The relationship of mental and behavioral disorders to all-cause mortality in a 27-year follow-up of 4 epidemiologic catchment area samples. Am J Epidemiol. 2013;178:1366–1377. doi: 10.1093/aje/kwt219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mykletun A, Bjerkeset O, Øverland S, et al. Levels of anxiety and depression as predictors of mortality: The HUNT study. Br J Psychiatry. 2009;195:118–125. doi: 10.1192/bjp.bp.108.054866. [DOI] [PubMed] [Google Scholar]
- 10.Lee WE, Wadsworth MEJ, Hotopf M. The protective role of trait anxiety: A longitudinal cohort study. Psychol Med. 2006;36:345–351. doi: 10.1017/S0033291705006847. [DOI] [PubMed] [Google Scholar]
- 11.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raven M. Inappropriate use of epidemiological data in analysis of mortality in mental disorders 2015 [Google Scholar]
- 13.Russ TC, Stamatakis E, Hamer M, et al. Association between psychological distress and mortality: Individual participant pooled analysis of 10. BMJ. 2012;345:e4933. doi: 10.1136/bmj.e4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cuijpers P, Vogelzangs N, Twisk J, et al. Differential mortality rates in major and subthreshold depression: Meta-analysis of studies that measured both. Br J Psychiatry. 2013;202:22–27. doi: 10.1192/bjp.bp.112.112169. [DOI] [PubMed] [Google Scholar]
- 15.Cuijpers P, Vogelzangs N, Twisk J, et al. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry. 2014;171:453–462. doi: 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- 16.Khan A, Faucett J, Morrison S, Brown WA. Comparative mortality risk in adult patients with schizophrenia, depression, bipolar disorder, anxiety disorders, and attention-deficit/hyperactivity disorder participating in psychopharmacology clinical trials. JAMA Psychiatry. 2013;70:1091–1099. doi: 10.1001/jamapsychiatry.2013.149. [DOI] [PubMed] [Google Scholar]
- 17.Laan W, Termorshuizen F, Smeets HM, et al. A comorbid anxiety disorder does not result in an excess risk of death among patients with a depressive disorder. J Affect Disord. 2011;135:284–291. doi: 10.1016/j.jad.2011.08.026. [DOI] [PubMed] [Google Scholar]
- 18.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 19.Celano CM, Millstein RA, Bedoya CA, et al. Association between anxiety and mortality in patients with coronary artery disease: A meta-analysis. Am Heart J. 2015;170:1105–1115. doi: 10.1016/j.ahj.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dew MA, Rosenberger EM, Myaskovsky L, et al. Depression and anxiety as risk factors for morbidity and mortality after organ transplantation: A systematic review and meta-analysis. Transplantation. 2015;0:1–16. doi: 10.1097/TP.0000000000000901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sokoreli I, de Vries JJG, Pauws SC, Steyerberg EW. Depression and anxiety as predictors of mortality among heart failure patients: Systematic review and meta-analysis. Heart Fail Rev. 2016;21:49–63. doi: 10.1007/s10741-015-9517-4. [DOI] [PubMed] [Google Scholar]
- 22.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2016 [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;188:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95:89–98. [Google Scholar]
- 27.Ahmadi N, Hajsadeghi F, Mirshkarlo HB, et al. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol. 2011;108:29–33. doi: 10.1016/j.amjcard.2011.02.340. [DOI] [PubMed] [Google Scholar]
- 28.Ayerbe L, Ayis SA, Crichton S, et al. Natural history, predictors and associated outcomes of anxiety up to 10 years after stroke: The South London Stroke Register. Age Ageing. 2014;43:542–547. doi: 10.1093/ageing/aft208. [DOI] [PubMed] [Google Scholar]
- 29.Batterham PJ, Christensen H, Mackinnon AJ. Mental health symptoms associated with morbidity, not mortality, in an elderly community sample. Soc Psychiatry Psychiatr Epidemiol. 2012;47:79–85. doi: 10.1007/s00127-010-0313-0. [DOI] [PubMed] [Google Scholar]
- 30.Benabarre S, Olivera J, Lorente T, et al. Psychiatric symptoms are not an independent mortality risk factor in community-living elderly people. Int Psychogeriatr. 2014;26:911–920. doi: 10.1017/S1041610214000143. [DOI] [PubMed] [Google Scholar]
- 31.Bramsen I, Deeg DJH, van der Ploeg E, Fransman S. Wartime stressors and mental health symptoms as predictors of late-life mortality in World War II survivors. J Affect Disord. 2007;103:121–129. doi: 10.1016/j.jad.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 32.Butnoriene J, Bunevicius A, Saudargiene A, et al. Metabolic syndrome, major depression, generalized anxiety disorder, and ten-year all-cause and cardiovascular mortality in middle aged and elderly patients. Int J Cardiol. 2015;190:360–366. doi: 10.1016/j.ijcard.2015.04.122. [DOI] [PubMed] [Google Scholar]
- 33.Carrière I, Ryan J, Norton J, et al. Anxiety and mortality risk in community-dwelling elderly people. Br J Psychiatry. 2013;203:303–309. doi: 10.1192/bjp.bp.112.124685. [DOI] [PubMed] [Google Scholar]
- 34.Damen NL, Versteeg H, Boersma E, et al. Depression is independently associated with 7-year mortality in patients treated with percutaneous coronary intervention: results from the RESEARCH registry. Int J Cardiol. 2013;167:2496–2501. doi: 10.1016/j.ijcard.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 35.Doyle F, Conroy R, McGee H. Differential predictive value of depressive versus anxiety symptoms in the prediction of 8-year mortality after acute coronary syndrome. Psychosom Med. 2012;74:711–716. doi: 10.1097/PSY.0b013e318268978e. [DOI] [PubMed] [Google Scholar]
- 36.Einvik G, Dammen T, Høiseth AD, et al. Psychological distress and mortality in patients with acute dyspnea: Data from the Akershus Cardiac Examination (ACE) 2 Study. Gen Hosp Psychiatry. 2015;37:548–553. doi: 10.1016/j.genhosppsych.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 37.Favaro A, Gerosa G, Caforio AL, et al. Posttraumatic stress disorder and depression in heart transplantation recipients: the relationship with outcome and adherence to medical treatment. Gen Hosp Psychiatry. 2011;33:1–7. doi: 10.1016/j.genhosppsych.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Groenvold M, Petersen MA, Idler E, et al. Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat. 2007;105:209–219. doi: 10.1007/s10549-006-9447-x. [DOI] [PubMed] [Google Scholar]
- 39.Hermann C, Brand-Driehorst S, Kaminsky B, et al. Diagnostic groups and depressed mood as predictors of 22-month mortality in medical inpatients. Psychosom Med. 1998;60:570–577. doi: 10.1097/00006842-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Hoogwegt MT, Theuns DA, Pedersen SS, Kupper N. Long-term mortality risk in patients with an implantable cardioverter-defibrillator: Influence of heart rate and QRS duration. Int J Cardiol. 2014;175:560–564. doi: 10.1016/j.ijcard.2014.06.030. [DOI] [PubMed] [Google Scholar]
- 41.Kikkenborg Berg S, Caspar Thygesen L, Hastrup Svendsen J, et al. Anxiety predicts mortality in ICD patients: results from the cross-sectional national CopenHeartICD survey with register follow-up. PACE. 2014;37:1641–1650. doi: 10.1111/pace.12490. [DOI] [PubMed] [Google Scholar]
- 42.Markkula N, Harkanen T, Perala J, et al. Mortality in people with depressive, anxiety and alcohol use disorders in Finland. Br J Psychiatry. 2012;200:143–149. doi: 10.1192/bjp.bp.111.094904. [DOI] [PubMed] [Google Scholar]
- 43.Meyer T, Hussein S, Lange HW, Hermann-Lingen C. Anxiety is associated with a reduction in both mortality and major adverse cardiovascular events five years after coronary stenting. Eur J Prev Cardiol. 2015;22:75–82. doi: 10.1177/2047487313505244. [DOI] [PubMed] [Google Scholar]
- 44.Michal M, Prochaska JH, Keller K, et al. Symptoms of depression and anxiety predict mortality in patients undergoing oral anticoagulation: Results from the thrombEVAL study program. Int J Cardiol. 2015;187:614–619. doi: 10.1016/j.ijcard.2015.03.374. [DOI] [PubMed] [Google Scholar]
- 45.Nilsson J, Östling S, Karlsson B, et al. The 1-month prevalence of generalized anxiety disorder according to DSM-IV, DSM-V, and ICD-10 among nondemented 75-year-olds in Gothenburg, Sweden. Am J Geriatr Psychiatry. 2012;20:963–972. doi: 10.1097/JGP.0b013e318252e749. [DOI] [PubMed] [Google Scholar]
- 46.O’Toole BI, Catts SV, Outram S, et al. Factors associated with civilian mortality in Australian Vietnam Veterans three decades after the war. Mil Med. 2010;175:88–96. doi: 10.7205/milmed-d-09-00071. [DOI] [PubMed] [Google Scholar]
- 47.Ostir GV, Goodwin JS. High anxiety is associated with an increased risk of death in an older tri-ethnic population. J Clin Epidemiol. 2006;59:534–540. doi: 10.1016/j.jclinepi.2005.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phillips KA, Osborne RH, Giles GG, et al. Psychosocial factors and survival of young women with breast cancer: A population-based prospective cohort study. J Clin Oncol. 2008;26:4666–4671. doi: 10.1200/JCO.2007.14.8718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rosenberger EM, DiMartini AF, DeVito Dabbs AJ, et al. Psychiatric predictors of long-term transplant-related outcomes in lung transplant recipients. Transplantation. 2016;100:239–247. doi: 10.1097/TP.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saeed Mirza S, Arfan Ikram M, Hofman A, Tiemeier H. Anxiety does not predict mortality. A population-based study. World Psychiatry. 2015;14:103–104. doi: 10.1002/wps.20192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schofield PE, Stockler MR, Zannino D, et al. Hope, optimism and survival in a randomised trial of chemotherapy for metastatic colorectal cancer. Support Care Cancer. 2016;24:401–408. doi: 10.1007/s00520-015-2792-8. [DOI] [PubMed] [Google Scholar]
- 52.Van der Weele GM, Gussekloo J, De Waal MWM, et al. Co-occurrence of depression and anxiety in elderly subjects aged 90 years and its relationship with functional status, quality of life and mortality. Int J Geriatr Psychiatry. 2009;24:595–601. doi: 10.1002/gps.2162. [DOI] [PubMed] [Google Scholar]
- 53.van Hout HP, Beekman AT, de Beurs E, et al. Anxiety and the risk of death in older men and women. Br J Psychiatry. 2004;185:399–404. doi: 10.1192/bjp.185.5.399. [DOI] [PubMed] [Google Scholar]
- 54.Versteeg H, Hoogwegt MT, Hansen TB, et al. Depression, not anxiety, is independently associated with 5-year hospitalizations and mortality in patients with ischemic heart disease. J Psychosom Res. 2013;75:518–525. doi: 10.1016/j.jpsychores.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 55.Volz A, Schmid JP, Zwahlen M, et al. Predictors of readmission and health related quality of life in patients with chronic heart failure: a comparison of different psychosocial aspects. J Behav Med. 2011;34:13–22. doi: 10.1007/s10865-010-9282-8. [DOI] [PubMed] [Google Scholar]
- 56.Wang G, Cui J, Wang Y, et al. Anxiety and adverse coronary artery disease outcomes in Chinese patients. Psychosom Med. 2013;75:530–536. doi: 10.1097/PSY.0b013e3182984317. [DOI] [PubMed] [Google Scholar]
- 57.Watkins LL, Koch GG, Sherwood A, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc. 2013;2:e000068. doi: 10.1161/JAHA.112.000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Watson M, Haviland JS, Greer S, et al. Influence of psychological response on survival in breast cancer: a population-based cohort study. Lancet. 1999;354:1331–1336. doi: 10.1016/s0140-6736(98)11392-2. [DOI] [PubMed] [Google Scholar]
- 59.Bull Bringager C, Arnesen H, Friis S, et al. A long-term follow-up study of chest pain patients: effect of panic disorder on mortality, morbidity, and quality of life. Cardiology. 2008;110:8–14. doi: 10.1159/000109400. [DOI] [PubMed] [Google Scholar]
- 60.Dew MA, Kormos RL, Roth LH, et al. Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. J Heart Lung Transplant. 1999;18:549–562. doi: 10.1016/s1053-2498(98)00044-8. [DOI] [PubMed] [Google Scholar]
- 61.Lou P, Zhu Y, Chen P, et al. Interaction of depressive and anxiety symptoms on the mortality of patients with COPD: A preliminary study. COPD. 2014;11:444–450. doi: 10.3109/15412555.2013.822856. [DOI] [PubMed] [Google Scholar]
- 62.Mollica RF, Sarajilic N, Chernoff M, et al. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA. 2001;286:546–554. doi: 10.1001/jama.286.5.546. [DOI] [PubMed] [Google Scholar]
- 63.Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. 2001;110:585–599. doi: 10.1037//0021-843X.110.4.585. [DOI] [PubMed] [Google Scholar]
- 64.Lamers F, van Oppen P, Comijs HC, et al. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: The Netherlands Study of Depression and Anxiety (NESDA) J Clin Psychiatry. 2011;72:341–348. doi: 10.4088/JCP.10m06176blu. [DOI] [PubMed] [Google Scholar]
- 65.Mineka S, Watson D, Clark LA. COMORBIDITY OF ANXIETY AND UNIPOLAR MOOD DISORDERS. Annu Rev Psychol. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- 66.Eaton WW, Martins SS, Nestadt G, et al. The burden of mental disorders. Epidemiol Rev. 2008;30:1–14. doi: 10.1093/epirev/mxn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease. J Am Coll Cardiol. 2010;56:38–46. doi: 10.1016/j.jacc.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 68.Scott KM. Depression, anxiety and incident cardiometabolic diseases. Curr Opin Psychiatry. 2014;27:289–293. doi: 10.1097/YCO.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 69.Hoerster KD, Lehavot K, Simpson T, et al. Health and health behavior differences: U.S. military, veteran, and civilian men. Am J Prev Med. 2012;43:483–489. doi: 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 70.Bryant C, Jackson H, Ames D. The prevalence of anxiety in older adults: Methodological issues and a review of the literature. J Affect Disord. 2008;109:233–250. doi: 10.1016/j.jad.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 71.Derogatis LR, Morrow GR, Fetting J, et al. The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751–757. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 72.Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13:7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sansone RA, Hendricks CM, Gaither GA, Reddington A. Prevalence of anxiety symptoms among a sample of outpatients in an internal medicine clinic: A pilot study. Depress Anxiety. 2004;19:133–136. doi: 10.1002/da.10143. [DOI] [PubMed] [Google Scholar]
- 74.Watts S, Prescott P, Mason J, et al. Depression and anxiety in ovarian cancer: A systematic review and meta-analysis of prevalence rates. BMJ Open. 2015;5:e007618. doi: 10.1136/bmjopen-2015-007618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wells KB, Golding JM, Burnam MA. Chronic medical conditions in a sample of the general population with anxiety, affective, and substance use disorders. Am J Psychiatry. 1989;146:1440–1446. doi: 10.1176/ajp.146.11.1440. [DOI] [PubMed] [Google Scholar]
- 76.Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: Prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010:1209–1221. doi: 10.1002/gps.2463. [DOI] [PubMed] [Google Scholar]
- 77.Campbell-Burton CA, Murray J, Holmes J, et al. Frequency of anxiety after stroke: A systematic review and meta-analysis of observational studies. Int J Stroke. 2013;8:545–559. doi: 10.1111/j.1747-4949.2012.00906.x. [DOI] [PubMed] [Google Scholar]
- 78.Cassileth BR, Lusk EJ, Strouse TB, et al. Psychosocial status in chronic illness: A comparative analysis of six diagnostic groups. N Engl J Med. 1984;311:506–511. doi: 10.1056/NEJM198408233110805. [DOI] [PubMed] [Google Scholar]
- 79.Cumming TB, Blomstrand C, Skoog I, Linden T. The high prevalence of anxiety disorders after stroke. Am J Geriatr Psychiatry. 2015 doi: 10.1016/j.jagp.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 80.Chang Z, Lichtenstein P, Larsson H, Fazel S. Substance use disorders, psychiatric disorders, and mortality after release from prison: A nationwide longitudinal cohort. Lancet Psychiatry. 2015;2:422–430. doi: 10.1016/S2215-0366(15)00088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Grossardt BR, Bower JH, Geda YE, et al. Pessimistic, anxious, and depressive personality traits predict all-cause mortality: The Mayo Clinic Cohort Study of Personality and Aging. Psychosom Med. 2009;500:491–500. doi: 10.1097/PSY.0b013e31819e67db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wedegaertner F, Arnhold-kerri S, Sittaro N, et al. Depression- and anxiety-related sick leave and the risk of permanent disability and mortality in the working population in Germany: A cohort study. BMC Public Health. 2013;13:145. doi: 10.1186/1471-2458-13-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Joukamaa M, Heliovaara M, Knekt P, et al. Mental disorders and cause-specific mortality. Br J Psychiatry. 2001;179:498–502. doi: 10.1192/bjp.179.6.498. [DOI] [PubMed] [Google Scholar]
- 84.Roest AM, Zuidersma M, Jonge PD. Myocardial infarction and generalised anxiety disorder: 10-year follow-up. Br J Psychiatry. 2012;200:324–329. doi: 10.1192/bjp.bp.111.103549. [DOI] [PubMed] [Google Scholar]
- 85.Williams JB, Alexander KP, Morin J, et al. Preoperative anxiety as a predictor of mortality and major morbidity in patients aged > 70 years undergoing cardiac surgery. Am J Cardiol. 2013;111:137–142. doi: 10.1016/j.amjcard.2012.08.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Johnson J, Weissman MM, Klerman GL. Panic disorder, comorbidity, and suicide attempts. Arch Gen Psychiatry. 1990;47:805–808. doi: 10.1001/archpsyc.1990.01810210013002. [DOI] [PubMed] [Google Scholar]
- 87.Weissman MM, Klerman GL, Markowitz JS, Ouellette R. Suicidal ideation and suicide attempts in panic disorder and attacks. N Engl J Med. 1989;321:1209–1214. doi: 10.1056/NEJM198911023211801. [DOI] [PubMed] [Google Scholar]
- 88.Barth J, Schumacher M, Hermann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 89.Grant BF, Stinson FS, Dawson DA, Chou SP. Prevalence and Co-occurrence of Substance Use Disorders and Independent Mood and Anxiety Disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 90.Morissette SB, Tull MT, Gulliver SB, et al. Anxiety, anxiety disorders, tobacco use, and nicotine: A critical review of interrelationships. Psychol Bull. 2007;133:245–272. doi: 10.1037/0033-2909.133.2.245. [DOI] [PubMed] [Google Scholar]
- 91.Grant BF, Goldstein RB, Chou SP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Buckner JD, Schmidt NB, Lang AR, et al. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schneier FR, Foose TE, Hasin DS, et al. Social anxiety disorder and alcohol use disorder co-morbidity in the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2010;40:977–988. doi: 10.1017/S0033291709991231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36:698–703. doi: 10.1016/s0091-7435(03)00042-2. [DOI] [PubMed] [Google Scholar]
- 95.Ströhle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. 2009;116:777–784. doi: 10.1007/s00702-008-0092-x. [DOI] [PubMed] [Google Scholar]
- 96.Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health beahviors, and risk for cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hamer M, Bates CJ, Mishra GiD. Depression, physical function, and risk of mortality: National diet and nutrition survey in adults older than 65 years. Am J Geriatr Psychiatry. 2010;19:72–78. doi: 10.1097/JGP.0b013e3181df465e. [DOI] [PubMed] [Google Scholar]
- 98.Boyer P, Liénard P. Why ritualized behavior? Precaution Systems and action parsing in developmental, pathological and cultural rituals. Behav Brain Sci. 2006;29:595–650. doi: 10.1017/s0140525x06009332. [DOI] [PubMed] [Google Scholar]
- 99.Szechtman H, Woody E. Obsessive–Compulsive Disorder as a disturbance of security motivation. Psychol Rev. 2004;111:111–127. doi: 10.1037/0033-295X.111.1.111. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


