Abstract
BACKGROUND
Crack cocaine dependence has become a severe public health problem in Brazil, and current psychosocial approaches to this problem have shown little or no effectiveness. Although contingency management is among the most effective behavioral treatments for substance use disorders, it has never been applied in the treatment of crack cocaine-dependent individuals in Brazil.
AIMS
To evaluate the efficacy of incorporating contingency management into standard outpatient treatment for crack cocaine dependence, as well as the impact that doing so has on treatment attendance, retention in treatment, maintenance of abstinence, and the frequency of substance use.
METHODS
We evaluated 65 treatment-seeking, crack cocaine-dependent individuals, randomized to receive 12 weeks of standard treatment plus contingency management (STCM; n = 33) or 12 weeks of standard treatment alone (STA; n = 32). Those in the STCM group received monetary incentives for being abstinent, earning up to US$235.50 if they remained abstinent throughout the entire treatment period.
RESULTS
The STCM group participants attended a mean of 19.5 (SD = 14.9) treatment sessions, compared with 3.7 (SD = 5.9) for the STA group participants (p < 0.01). Those in the STCM group were 3.8, 4.6, and 68.9 times more likely to be retained in treatment at weeks 4, 8, and 12 than were those in the STA group. The likelihood of detecting 4, 8, and 12 weeks of continuous abstinence was 17.7, 9.9, and 18.6 times higher in the STCM group than in the STA group (p < 0.05). Compared to the STA group, the STCM group submitted a significantly higher proportion of crack cocaine, THC, and alcohol negative samples (p < 0.001) when all expected samples were included in the denominator, but not when only submitted samples were considered. The average monthly cost/participant for incentives was $29.00.
CONCLUSIONS
Contingency management showed efficacy in a sample of Brazilian crack cocaine users. The intervention holds promise for broader application in international settings.
Keywords: Crack cocaine, contingency management, behavioral treatment, randomized clinical trial, substance use in Brazil
Introduction
During the last several decades, crack cocaine use has increased significantly in most Latin-American countries (UNODC, 2015), becoming a severe public health issue in the region. In Brazil, this public health problem has reached devastating proportions, the country having been reported to be among the largest crack cocaine markets in the world. According to the Second Brazilian National Alcohol and Drugs Survey, 1.5% of Brazilians ≥ 14 years of age have smoked crack cocaine at least once in their lifetime, with over 0.8% of the population having used this substance in the previous year (Abdalla et al., 2014). Although the proportions of crack cocaine users may seem small, in the last decade the demand for substance abuse treatment in Brazil has grown more for crack cocaine than for any other substance. Thus, the use of crack cocaine has surpassed that of all other illicit substances as a cause of hospital admission in the country (Dunn, Laranjeira, Silveira, Formigini, & Ferri, 1996; Noto, Moura, Nappo, Galduroz, & Carlini, 2002).
As in other countries, crack cocaine use in Brazil is more prevalent in the urban population, particularly among young adult males who are homeless (Noto et al., 2003; Santos Cruz et al., 2013). Although crack cocaine users are usually polydrug users, crack cocaine is typically their drug of choice (Guindalini, Vallada, Breen, & Laranjeira 2006; Oliveira, & Nappo 2008). Crack cocaine use is associated with concomitant severe psychiatric comorbidities, a higher probability of living or having lived on the streets, and exposure to risky sexual behaviors, with elevated rates of HIV infection and hepatitis (Carvalho & Seibel 2009; Von Diemen, De Boni, Kessler, Benzano, & Pechansky, 2010; Malta et al., 2010; Zubaran, Foresti, Thorell, Franceschini, & Homero, 2010; Kessler et al., 2012; Narvaez et al., 2014). Crack cocaine users are also more likely to be or to have been involved in illegal activities and to have been incarcerated (Dunn & Laranjeira 1999; Ribeiro, Sanchez, & Nappo 2010). Consequently, mortality is seven times higher in crack-dependent individuals than in the general population, 17.6% of crack cocaine users dying during the first five years after crack cocaine dependence has been established (Ribeiro, Dunn, Laranjeira, & Sesso 2004).
Over the last twenty years, a behavioral treatment known as contingency management (CM) has been widely studied in the United States (Higgins et al., 1991; Higgins, Wong, Badger, Ogden, & Dantona, 2000; Petry et al., 2005; McDonnell et al., 2013; Petry & Carroll, 2013), recent trials having also been conducted in Spain (Garcia-Rodriguez et al., 2011, 2009; Secades-Villa et al., 2013, 2011), Switzerland (Petitjean et al., 2014), the United Kingdom (Weaver et al 2014) and China (Chen et al., 2013; Jiang et al., 2012). Various meta-analyses and review articles have presented consistent, robust evidence that, when applied alone or in combination with psychosocial or pharmacological treatment, CM is among the most effective treatments with regard to retention in treatment and promoting continuous abstinence from the use of cocaine and other stimulants (Prendergast, Podus, Finney, Greenwell, & Roll, 2006; Lussier, Heil, Mongeon, Badger, & Higgins, 2006; Dutra et al., 2008; Miguel, Yamauchi, Simões, da Silva, & Laranjeira, 2015). Despite the clear scientific evidence of the effectiveness of CM, the approach has never been coupled with psychosocial treatment for substance use disorder in Brazil.
This study aimed to evaluate the impact that combining CM with standard treatment has on treatment attendance, retention in treatment, the maintenance of abstinence, and the frequency of substance use among treatment-seeking crack cocaine-dependent individuals in Brazil.
Methods
Study location
The study was conducted at the Vila Maria Specialized Medical Outpatient Clinic for Alcohol and Drug Treatment, the main referral center for alcohol- and drug-related disorders in the northern region of the city of São Paulo, Brazil, which includes several favelas, or slums.
Participants
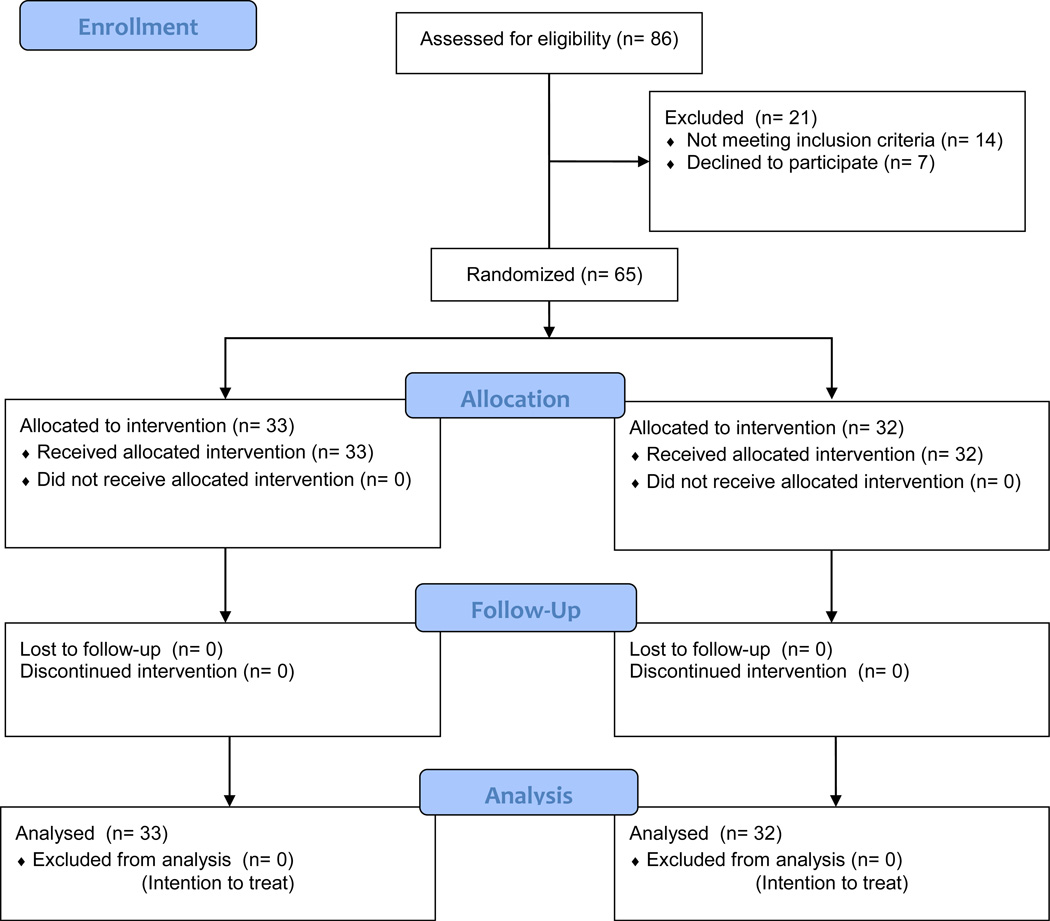
Between August 2012 and July 2014, a total of 86 individuals were screened for inclusion in the study. We included those who were between 18 and 60 years of age, had a current diagnosis of crack cocaine dependence according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth edition (DSM-IV), as assessed with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), reported having used crack cocaine in the last 4 weeks and were seeking treatment for crack cocaine addiction. Individuals who had been abstinent from crack cocaine use for ≥ 4 weeks were excluded, as were those whose drug of choice was not crack cocaine, those with a DSM-IV diagnosis of schizophrenia, and those who were unable to attend treatment sessions at least three times per week. Thus, 21 individuals were excluded. Therefore, the study sample comprised 65 treatment-seeking crack cocaine-dependent individuals. The study was approved by the Research Ethics Committee of the Federal University of Sao Paulo and by the Ethics Committee of the Brazilian National Ministry of Health (Protocol no. CAAE 00745912.4.0000.5505). All participants gave written informed consent. This study was registered at “ClinicalTrials.gov” under the identifier number NCT01815645.
Intake assessments
Intake interviews lasted up to 90 minutes and included the collection of sociodemographic data, as well as assessments of the history and pattern of drug use. We collected data related to previous treatment history and risky sexual behaviors. Using the SCID-I (First, Spitzer, Gibbon, & Williams, 1997), we screened participants for a DSM-IV diagnosis of substance use disorder. After the intake assessments, each participant provided the initial urine sample (to assess crack cocaine and marijuana use) and the initial breath sample (to assess recent alcohol use). Thereafter, urine and breath were sampled three times per week.
Randomization
After the baseline assessment, we used permuted block randomization in order to place each participant into one of two treatment groups: 12 weeks of standard treatment alone (STA) or 12 weeks of standard treatment plus CM (STCM). Participants were stratified by the concurrent diagnosis of alcohol dependence.
STA
Participants in the STA group (n = 32) attended weekly 90-minute group meetings on relapse prevention, including coping skills training; weekly 90-minute occupational therapy sessions; at least one individual session per month with a psychiatrist; and weekly psychotherapy sessions of up to 40 minutes each. Treatment participation was monitored by a designated nurse who was responsible for contact upkeep and rescheduling. After submitting a urine sample, participants were informed immediately of their results. When participants submitted a sample that tested negative for crack cocaine, treatment staff would congratulate them for being present as well as for being abstinent. When participants submitted a sample that tested positive for crack cocaine, treatment staff would encourage them to stop using crack cocaine and congratulate them for continuing to attend treatment despite their use. No form of monetary incentive was given to participants in the STA group.
STCM
Participants in the STCM group (n = 33) received the exact same treatment as did those in the STA group except that they could earn vouchers for being abstinent. After the first sample testing negative for crack cocaine, participants immediately received a voucher with a corresponding monetary value, in Brazilian reals (R$), of R$5.00—equivalent to US$1.25 (as of January 2016, 1 US dollar was equal to approximately 4 Brazilian reals). Voucher value increased by R$2.00 for every consecutive negative sample until reaching a maximum of R$15.00. When abstinent from crack cocaine use, participants could earn an additional R$2.00 voucher for each consecutive breath sample testing negative for alcohol. Participants who tested negative for crack cocaine in all three urine samples collected in a given week received a R$20.00 bonus voucher. Another R$10.00 bonus was given to participants who, during the same week, not only tested negative for crack cocaine in all three urine samples but also tested negative for alcohol in all three breath samples and for delta-9-tetrahydrocannabinol (THC) in all three urine samples. When participants submitted a urine sample that tested positive for crack cocaine or missed an appointment, they would not earn any vouchers that day and the value of the subsequent voucher would reset to R$5.00, voucher value escalation restarting from that point.
In order to maximize the effect of the STCM intervention, we used vouchers that participants could immediately exchange for goods or services. Treatment staff would accompany participants for up to 1 km from the treatment facility to exchange the vouchers for goods available in the surrounding community, such as bus passes, subway tickets, food, clothing, electronic devices, phone cards, and other commodities. The vouchers could also be converted to mobile phone credits or applied toward utility bill payments. Tobacco and alcohol were the only goods that could not be obtained with the vouchers. Participants could also decide to allow their vouchers to accumulate and did not lose the accumulated value after submitting a urine sample that tested positive for crack cocaine. However, participants could spend their vouchers only after submitting a negative crack cocaine urine sample. If all samples submitted by a participant during the 12 weeks of treatment tested negative for crack cocaine, THC, and alcohol, the participant would earn a total of R$942.00 (US$235.50).
Urine and breath sampling
Participants were instructed to appear at the Outpatient Clinic three times a week (on Monday, Wednesday, and Friday), between 10 a.m. and 4 p.m., to provide urine samples (in the presence of a same sex observer) to be dipstick tested for crack cocaine and THC, as well to submit to breath analysis (in the presence of a nurse) to detect recent alcohol consumption. Breath alcohol results appeared instantly, and urine test results were obtained within 5 minutes. Participants were immediately informed of the results. The entire process took no longer than 10 minutes.
Crack cocaine use was assessed with a rapid cocaine screening test (Abon Biopharm, Hangzhou, China) capable of detecting ≥ 300 ng/ml of benzoylecgonine in a urine sample, and marijuana use was assessed with a rapid THC screening test (Abon Biopharm) capable of detecting ≥ 50 ng/ml of THC in a urine sample. Urine samples were validated by temperature and creatinine concentration. If a sample was deemed invalid, the participant was encouraged to submit a new sample. Alcohol use was assessed with single-use breath-alcohol testers (Contralco, Gignac, France) capable of detecting alcohol levels ≥ 0.3 g/L.
Primary outcome measures
Treatment attendance was expressed as the total number of sessions attended during the 12 weeks of treatment. Retention in treatment was quantified as the period elapsed between treatment intake and dropout (last appearance at the treatment facility) or the end of treatment.
The longest duration of confirmed crack cocaine abstinence (LDA) was defined by the longest sequence of consecutive negative samples submitted. To address missing data in calculating LDA, missing visits due to holidays, if preceded and followed by negative samples, were coded as negative, and up to once a week, excused missing visits, if preceded and followed by negative samples, were also coded as negative.
The proportion of samples testing negative for crack cocaine was determined by dividing the number of negative samples by the total number of samples submitted. A second proportion was defined by the number of crack cocaine negative samples divided by the expected samples (36 samples). The first variable makes no assumption about whether missing samples are positive or negative, while the second assumes missing samples are positive, and this latter proportion is impacted by attrition or missed samples.
Secondary outcome measures
Proportions of samples testing negative for marijuana and alcohol were also quantified. For each substance, the number of submitted samples was included in the denominator for one analysis, and with 36 samples in denominator for a second.
Sample size calculation
Sample size calculations were conducted using the longest duration of confirmed abstinence outcome to power the study. Following Cohen’s (1988) parameters to encounter moderate size effects on chi-square group comparisons, we used a significance level of α = 0.05, a power of 1 − β = 0.80, a contingency table with 1 degree of freedom, and an effect size of w = 0.35. Using those criteria, we calculated a sample size of 65 subjects.
Statistical analysis
For all baseline assessments, between-group comparisons were conducted using chi-square tests for dichotomous variables and t-tests for continuous variables. Independent samples t-test compared groups based on mean number of attended sessions and retention in treatment. Odd ratios and 95% confidence intervals are also presented for the proportions of participants who remained in the treatment program for > 1 week, ≥ 4 weeks, ≥ 8 weeks, or the full 12 weeks.
To address the efficacy of the intervention on the longest duration of confirmed crack cocaine abstinence, we conducted two analyses. First, the mean LDA of both groups was compared via t-tests. Second, we compared the two groups in terms of the proportion of participants who were abstinent for ≥ 4 weeks, for ≥ 8 weeks, or for the full 12 weeks. Odds ratios, with their respective 95% confidence intervals, are presented.
To evaluate differences between groups on the proportions of samples testing negative, t-tests compared groups using both submitted samples and expected samples in the denominators. An alpha threshold of 0.05 was used for all analyses. All statistical analyses were performed with the SPSS Statistics software package, version 22.0 (IBM Corporation, Armonk, NY).
Results
Baseline characteristics
As shown in Table 1, the baseline demographic variables and patterns of substance use did not differ statistically between the two groups. The sample was composed of individuals with a low level of education and high rates of unemployment (over 80%); approximately 25% were living on the streets at the time of treatment intake. Most (85%) of the participants were male, and 75% had more than one substance use disorder. Nearly half of the participants presented with at least one psychotic symptom at the start of treatment. The average length of crack cocaine use was over 12 years, with an average age of onset of approximately 22 years. Most of the participants had a history of inpatient treatment for crack cocaine dependence, and nearly half of the samples submitted at baseline tested positive for crack cocaine.
Table 1.
Demographic characteristics and patterns of drug use among crack dependent individuals under treatment
| Control (STA) (n = 32) |
Experimental (STCM) (n = 33) |
||||
|---|---|---|---|---|---|
| Mean/% | SD | Mean/% | SD | p - value | |
| Age | 35.4 | 8.5 | 35.3 | 8.7 | 0.849 |
| Sex (male) | 81.3% | 90% | 0.260 | ||
| Education (years) | 9.774 | 3.747 | 8.911 | 3.441 | 0.337 |
| Unemployment | 84.4% | 84.8% | 0.957 | ||
| Homelessness | 28.1% | 18.2% | 0.341 | ||
| Psychosis Symptoms | 46.9% | 45.5% | 0.895 | ||
| Alcohol Dependence | 65.6% | 66.7% | 0.954 | ||
| Multiple Substance Dependence | 75.0% | 63.6% | 0.323 | ||
| Baseline positive urine exam | 46.9% | 51.5% | 0.708 | ||
| Age of onset (years) | 23.6 | 7.3 | 21.8 | 6.6 | 0.396 |
| Period of use (years) | 11.8 | 7.5 | 13.5 | 7.4 | 0.324 |
| Slept on the streets due to use | 59.4% | 69.7% | 0.384 | ||
| Been in Crackland due to use | 93.8% | 84.8% | 0.247 | ||
| History of treatment | 81,1% | 87,5% | 0.733 | ||
| Number of previous treatments | 2.5 | 3.1 | 3.2 | 4.8 | 0.600 |
Abbreviations: STCM, Standard Treatment plus Contingency Management; STA, Standard Treatment Alone; SD, Standard Deviation.
Treatment attendance and retention
The mean number of sessions attended was higher in the STCM group than in the STA group—19.5 (SD = 14.9) versus 3.7 (SD = 5.9)—a difference that was statistically significant (t = 5.57; p < 0.01).
The STCM group was retained for a mean of 7.7 (SD = 5.2) weeks in comparison to 3.0 (SD = 4.0) weeks in the STA group. These results are statistically different (t= 4.06; p< 0.01). As can be seen in Table 2, the likelihood of very early dropout in less than one week, was significantly higher in the STA group than in the STCM group. Similarly, STCM participants were significantly more likely to be retained 4, 8 and 12 weeks than STA participants.
Table 2.
Retained in treatment along the 12 weeks of intervention
| Treatment | STA (%) | STCM (%) | OR* | P-value |
|---|---|---|---|---|
| Retention | (n=32) | (n=33) | (95%CI) | |
| Less then 1 week | 56.2 | 15.2 | 0.14 (0.04 – 0.45) | 0.0007 |
| ≥4 weeks | 34.4 | 66.7 | 3.8 (1.4 – 10.7) | 0.013 |
| ≥8 weeks | 25 | 62.5 | 4.6 (1.6 – 13.3) | 0.005 |
| 12 weeks | 0 | 51.5 | 68.9 (3.8 – 1219.4) | 0.0001 |
the reference group is the Standard Treatment Alone condition.
Abbreviations: STCM, Standard Treatment plus Contingency Management; STA, Standard Treatment Alone; OR, Odds Ratio; CI, Confidence Interval
Crack cocaine abstinence
The mean number of consecutive negative crack cocaine urine samples submitted was 2.4 (SD= 5.3) for the STA group and 13.1 (SD= 13.3) for the STCM group, resulting in an average of 0.8 and 4.4 weeks of abstinence, respectively (t = 4.16; p< 0.01). Table 3 shows that the odds of achieving at least 4, 8, and 12 weeks of continuous abstinence from crack cocaine use were significantly higher for STCM group participants than for STA group participants.
Table 3.
Confirmed continuous crack/cocaine abstinence during the 12 weeks of intervention
| Continuous | STA (%) | STCM (%) | OR | p-value |
|---|---|---|---|---|
| Abstinence | (n=32) | (n=33) | (95%CI) | |
| ≥4 weeks | 3.1 | 36.4 | 17.7 (2.1 – 146.7) | 0.001 |
| ≥8 weeks | 3.1 | 24.2 | 9.9 (1.2 – 84.7) | 0.027 |
| 12 weeks | 0 | 21.2 | 18.4 (1.1 – 337.1) | 0.011 |
the reference group is the Standard Treatment Alone condition.
Abbreviations: STCM, Standard Treatment plus Contingency Management; STA, Standard Treatment Alone; OR, Odds Ratio; CI, Confidence Interval
As can be seen in Table 4, the STCM group participants submitted 52.9% of the 36 possible urine samples for crack cocaine testing during the 12 week treatment period, compared with 9.8% for the STA group participants. Thus, rates of urine sample submission differed significantly between the groups.
Table 4.
Submitted samples of the primary and secondary target drugs
| STA (32) % (n° of samples) |
STCM (33) % (n° of samples) |
t-value* | p-value | |
|---|---|---|---|---|
| Total Samples Submitted | ||||
| Crack/cocaine | 9.8 (113) | 52.9 (628) | 4.286 | 0.0001 |
| THC | 10.3 (119) | 53.5 (636) | 4.206 | 0.0001 |
| Alcohol | 9.8 (113) | 54.2 (644) | 4.310 | 0.0001 |
|
Negative Samples Submitted (considering all expected samples) |
||||
| Crack/cocaine | 8.3 (96) | 46.5 (552) | 4.138 | 0.0001 |
| THC | 9.8 (113) | 50.3 (598) | 3.906 | 0.0001 |
| Alcohol | 9.4 (108) | 53.9 (641) | 4.408 | 0.0001 |
|
Negative Samples Submitted (considering submitted samples only) |
||||
| Crack/cocaine | 89.2 (96) | 87.8 (552) | −0.872 | 0.386 |
| THC | 93 (113) | 92.6 (598) | −0.112 | 0.911 |
| Alcohol | 98.4 (113) | 99.7 (641) | 1.075 | 0.287 |
the reference group is the Standard Treatment Alone condition.
Abbreviations: STCM, Standard Treatment plus Contingency Management; STA, Standard Treatment Alone; THC, tetrahydrocannabinol.
When all expected samples were considered in the denominator, the proportion of samples testing negative for crack cocaine was statistically higher in the STCM group than the STA group. However, no group difference was observed in the proportion of samples testing negative for crack cocaine when submitted samples were considered in the denominator.
Marijuana and alcohol abstinence
As can also be seen in Table 4, the STCM group participants submitted significantly more urine and breath samples for THC and alcohol testing. When all expected samples were considered in the denominator, the proportion of samples testing negative for THC was significantly higher in the STCM group than in the STA group, but the two groups submitted similar proportions of THC negative samples when the denominator consisted of submitted samples.
At the end of the intervention, we calculated the per-participant expenditures for vouchers. The mean cost per participant for purchased goods was R$348.80 (approximately US$87.00) for the full 12 weeks of treatment.
Discussion
Over the last 30 years, crack cocaine use has increased in Brazil. The morbidity and mortality related to crack cocaine dependence, together with our inability to treat this complex disorder, has made it a cause for concern among health care authorities, policy makers, and the community at large. The high rates of unemployment, low education level, homelessness, and multiple substance use disorders observed in our sample at baseline assessments highlight the acute state of social vulnerability among crack cocaine-dependent individuals in Brazil. To our knowledge, this was the first randomized controlled trial of CM conducted in Brazil. We have demonstrated how poor the results can be when standard treatment is used in isolation. We found that combining CM with standard treatment for crack cocaine dependence is efficacious in enhancing treatment attendance, encouraging treatment retention, and promoting sporadic and continuous crack cocaine abstinence.
Non-attendance and early dropout are highly prevalent in the setting of outpatient treatment for dependence on cocaine or crack cocaine, such factors being associated with relapse, continued drug use, and poor treatment outcomes (Hser, Evans, Huang, & Anglin, 2004; Ball, Carroll, Canning-Ball, & Rounsaville, 2006). Therefore, treatment attendance and retention in treatment are essential to assessments of treatment efficacy. Although the CM modality employed in this study was not designed to reinforce attendance or retention, our results suggest that CM targeting abstinence can have a substantial effect on those outcomes. We found that CM not only promoted significantly better treatment attendance but also increased by 68.9 times the likelihood of full retention in treatment with over 50% of the STCM participants being retained until the end of the treatment period. These results are consistent with those of other trials of CM targeting cocaine abstinence, including voucher-based programs (Higgins et al., 1994, 1993, 1991; Garcia-Rodriguez et al., 2009; Secades-Villa et al., 2011) and prize-based programs (Petry et al., 2004; Petry, Martin, & Simcic, 2005; Petry, Alessi, & Ledgerwood, 2012) targeting abstinence from cocaine, as well as with those of trials of CM targeting abstinence from multiple stimulants, including cocaine (Petry et al., 2005; Rawson et al., 2006).
The proportions of crack cocaine negative samples submitted were significantly higher in the experimental (STCM) group than in the control (STA) group (46.5% vs. 8.3%) when all expected samples were considered in the denominator, but these differences primarily related to differential sample submission rates between the groups. Patients in the control condition submitted only about 10% of the expected 36 samples, and the proportions of submitted samples that tested negative were similarly high in both groups. Nevertheless, more than one fifth of the participants in the STCM group documented consistent abstinence for the entire treatment period, compared with none of those in the STA group. Such results suggest that a proportion of crack cocaine users can achieve optimal responses once appropriate treatment has been provided.
Our findings are in keeping with those of several other trials of CM targeting cocaine abstinence (Higgins et al., 1994, 1993; 1991; Silverman et al., 1996; Petry et al., 2004; Petry, Martin, & Simcic, 2005; Garcia-Rodriguez et al., 2011, 2009; Secades-Villa et al., 2011; Petry, Alessi, & Ledgerwood, 2012) as well as with those of trials of CM targeting abstinence from stimulants in general (Petry et al., 2005; Pierce et al., 2006; Rawson et al., 2006; McDonnell et al., 2013). In all of those trials, the likelihood of submitting cocaine-negative urine samples was considerably greater among the participants receiving CM interventions, who also achieved longer periods of continuous abstinence.
Limitations and Future Directions
Our study has several limitations that should be considered. First, a substantial number of urine test results were missing, especially among the control group participants. We can hypothesize that this is partially due to the severity of crack cocaine dependence in the studied population and the lack of efficacy of the standard treatment. However, the differential rates of missing data between the groups impact a full understanding of the effects of this intervention. Therefore, the large effect size of the CM intervention when all expected samples were considered in the denominator, as well as the lack of evidence of efficacy of CM when only submitted samples were considered, can be partially attributed to the large quantity of missing data. It is of note that different results (including smaller between-group differences) might have been obtained if the control group had received an intervention that provided more data for analysis. Furthermore, it’s important to state that we attempted to conduct 3 and 6-month follow-up evaluations to assess CM’s long-term effects. However, very few patients completed the follow-up assessments, impeding any adequate quantitative analyses of these outcomes.
Another limitation is that our study was performed at a single center. Considering that there is no standardization of addiction treatment protocols in Brazil, our results could vary if replicated at centers where different treatment methods are employed and patient demographics differ. Hence, it is difficult to predict how representative the results obtained for STCM and STA are in comparison with the standard treatments currently available in the country. In addition, our study offers limited insight into how effective CM can be when applied in combination with other treatment approaches.
Regardless of its limitations, our study produced results suggesting that implementing CM in the setting of outpatient treatment at public health care facilities can be an effective strategy to address the public health crisis of crack cocaine use in Brazil. Finally, even though our study was not designed to conduct cost-effectiveness evaluations, the average monthly cost of US$29.00 per patient appears insignificant when compared with the social and financial burden of crack cocaine use in Brazil.
There is a need for additional studies of CM targeting crack cocaine abstinence, conducted at multiple centers, involving larger samples, including different reinforcement strategies (in terms of schedule and magnitude), targeting other desirable responses (such as retention and medication compliance), offering different forms of reinforcers (such as housing and access to employment) and designed to address cost-effectiveness issues. Such studies could provide further evidence of the efficacy of CM in the treatment of crack cocaine dependence.
Figure 1.
Consort Flow Diagram
Acknowledgments
We would like to extend our appreciation and gratitude to Professor John Strang for his invaluable input and for helping to shed light on this project.
Role of funding source: This study was supported by grants from Fundação de Amparo a Pesquisa de Sao Paulo (FAPESP) during the design, conduct and stages of data analyses and interpretation (Regular Research award number 2011/01469-7 and Ph.D. Scholarship award number 2013/04138-7). This study was also supported by a grant from the Clinical Trials Network Pacific Northwest Node (award number 5 U10 DA013714-10) from the National Institute on Drug Abuse (NIDA).
Footnotes
Declaration Of Interest: All authors report no real or potential conflict(s) of interest, including financial, personal, or other relationships with other organizations or pharmaceutical/biomedical companies that may inappropriately impact or influence the research and interpretation of the findings.
References
- Abdalla RR, Madruga CS, Ribeiro M, Pinsky I, Caetano R, Laranjeira R. Prevalence of Cocaine Use in Brazil: Data from the II Brazilian National Alcohol and Drugs Survey (BNADS) Addictive behaviors. 2014;39(1):297–301. doi: 10.1016/j.addbeh.2013.10.019. [DOI] [PubMed] [Google Scholar]
- Araujo RB, Pedroso RS, Castro MDGTD. Adaptação transcultural para o idioma português do Cocaine Craving Questionnaire-Brief. Rev. psiquiatr. clín.(São Paulo) 2010;37(5):195–198. [Google Scholar]
- Arndt S. Stereotyping and the treatment of missing data for drug and alcohol clinical trials. Substance abuse treatment, prevention, and policy. 2009;4(1):1. doi: 10.1186/1747-597X-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball SA, Carroll KM, Canning-Ball M, Rounsaville BJ. Reasons for dropout from drug abuse treatment: Symptoms, personality, and motivation. Addictive behaviors. 2006;31(2):320–330. doi: 10.1016/j.addbeh.2005.05.013. [DOI] [PubMed] [Google Scholar]
- Carvalho HB, Seibel SD. Crack cocaine use and its relationship with violence and HIV. Clinics. 2009;64(9):857–866. doi: 10.1590/S1807-59322009000900006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Hong Y, Zou X, McLaughlin MM, Xia Y, Ling L. Effectiveness of prize-based contingency management in a methadone maintenance program in China. Drug and alcohol dependence. 2013;133(1):270–274. doi: 10.1016/j.drugalcdep.2013.05.028. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, New Jersey: L: 1988. [Google Scholar]
- Cunha JA. Manual da versão em português das Escalas Beck. São Paulo: Casa do Psicólogo; 2001. [Google Scholar]
- Diemen LV, Szobot CM, Kessler F, Pechansky F. Adaptation and construct validation of the Barratt Impulsiveness Scale (BIS 11) to Brazilian Portuguese for use in adolescents. Revista Brasileira de Psiquiatria. 2007;29(2):153–156. doi: 10.1590/s1516-44462006005000020. [DOI] [PubMed] [Google Scholar]
- Dunn J, Laranjeira RR, Silveira DX, Formigoni MLOS, Ferri CP. Crack cocaine: an increase in use among patients attending clinics in São Paulo: 1990–1993. Substance Use and Misuse. 1996;31:519–527. doi: 10.3109/10826089609045824. [DOI] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Power MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry. 2008;165:563–570. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. User's guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version. American Psychiatric Pub; 1997. [Google Scholar]
- García-Fernández G, Secades-Villa R, García-Rodríguez O, Sánchez-Hervás E, Fernández-Hermida JR, Higgins ST. Adding Voucher-Based Incentives to Community Reinforcement Approach Improves Outcomes during Treatment for Cocaine Dependence. The American Journal on Addictions. 2011;20(5):456–461. doi: 10.1111/j.1521-0391.2011.00154.x. [DOI] [PubMed] [Google Scholar]
- Garcia-Rodriguez O, Secades-Villa R, Higgins ST, Fernandez-Hermida JR, Carballo JL, Errasti Perez JM, Diaz SAH. Effects of voucher-based intervention on abstinence and retention in an outpatient treatment for cocaine addiction: a randomized controlled trial. Experimental and Clinical Psychopharmacology. 2009;17(3):131. doi: 10.1037/a0015963. [DOI] [PubMed] [Google Scholar]
- Group, W. H. O. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Guindalini C, Vallada H, Breen G, Laranjeira R. Concurrent crack and powder cocaine users from Sao Paulo: Do they represent a different group? BMC Public Health. 2006;6(1):10. doi: 10.1186/1471-2458-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Hughes JR, Foerg F, Badger G. Achieving cocaine abstinence with a behavioral approach. The American journal of psychiatry. 1993 doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg FE, Donham R, Badger GJ. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of general psychiatry. 1994;51(7):568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Delaney DD, Budney AJ, Bickel WK, Hughes JR, Foerg F, Fenwick JM. A behavioral approach to achieving initial cocaine abstinence. American Journal of Psychiatry. 1991;148:1218–1224. doi: 10.1176/ajp.148.9.1218. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Wong CJ, Badger GJ, Ogden DEH, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. Journal of Consulting and Clinical Psychology. 2000;68(1):64. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E, Huang D, Anglin DM. Relationship between drug treatment services, retention, and outcomes. Psychiatric Services. 2004 doi: 10.1176/appi.ps.55.7.767. [DOI] [PubMed] [Google Scholar]
- Jiang H, Du J, Wu F, Wang Z, Fan S, Li Z, Zhao M. Efficacy of contingency management in improving retention and compliance to methadone maintenance treatment: a random controlled study. Shanghai archives of psychiatry. 2012;24(1):11. doi: 10.3969/j.issn.1002-0829.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler FHP, Terra MB, Faller S, Stolf AR, Peuker AC, Benzano D, et al. Crack users show high rates of antisocial personality disorder, engagement in illegal activities and other psychosocial problems. The American Journal on Addictions. 2012;21(4):370–380. doi: 10.1111/j.1521-0391.2012.00245.x. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Malta M, Magnanini M, Mello M, Pascom AR, Linhares Y, Bastos F. HIV prevalence among female sex workers, drug users and men who have sex with men in Brazil: A systematic review and meta-analysis. BMC Public Health. 2010;10:317. doi: 10.1186/1471-2458-10-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonell MG, Srebnik D, Angelo F, McPherson S, Lowe JM, Sugar A, Ries RK. Randomized controlled trial of contingency management for stimulant use in community mental health patients with serious mental illness. American Journal of Psychiatry. 2013;170(1):94–101. doi: 10.1176/appi.ajp.2012.11121831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miguel AQC, Yamauchi R, Simões V, da Silva CJ, Laranjeira RR. From Theory to treatment: Understanding Addiction from an operant behavioral perspective. Journal of Modern Education Review. 2015;5(8):778–787. [Google Scholar]
- Narvaez JC, Jansen K, Pinheiro RT, Kapczinski F, Silva RA, Pechansky F, Magalhães PV. Psychiatric and substance-use comorbidities associated with lifetime crack cocaine use in young adults in the general population. Comprehensive psychiatry. 2014;55(6):1369–1376. doi: 10.1016/j.comppsych.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Noto AR, Baptista MC, Faria ST, Nappo SA, Galduróz JCF, Carlini EA. Drugs and health in the Brazilian press: an analysis of articles published in newspapers and magazines. Cadernos de Saúde Pública. 2003;19(1):69–79. doi: 10.1590/s0102-311x2003000100008. [DOI] [PubMed] [Google Scholar]
- Noto AR, Moura YG, Nappo SG, Galduroz JCF, Carlini EA. Admissions for mental and behavioural disorders due to the use of psychoactive substances: A national epidemiological survey between 1988 and 1999. Jornal Brasileiro de Psiquiatria. 2002;51(2):113–121. [Google Scholar]
- Oliveira LGD, Nappo SA. Crack na cidade de São Paulo: acessibilidade, estratégias de mercado e formas de uso. Revista de Psiquiatria Clínica. 2008;35(6):212–218. [Google Scholar]
- Peirce JM, Petry NM, Stitzer ML, Blaine J, Kellogg S, Satterfield F, Li R. Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment: A National Drug Abuse Treatment Clinical Trials Network study. Archives of General Psychiatry. 2006;63(2):201–208. doi: 10.1001/archpsyc.63.2.201. [DOI] [PubMed] [Google Scholar]
- Petitjean SA, Dürsteler-MacFarland KM, Krokar MC, Strasser J, Mueller SE, Degen B, Farronato NS. A randomized, controlled trial of combined cognitive-behavioral therapy plus prize-based contingency management for cocaine dependence. Drug and alcohol dependence. 2014;145:94–100. doi: 10.1016/j.drugalcdep.2014.09.785. 94-100. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Ledgerwood DM. A randomized trial of contingency management delivered by community therapists. Journal of consulting and clinical psychology. 2012;80(2):286. doi: 10.1037/a0026826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Carroll KM. Contingency management is efficacious in opioid-dependent outpatients not maintained on agonist pharmacotherapy. Psychology of Addictive Behaviors. 2013;27(4):1036. doi: 10.1037/a0032175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Martin B, Simcic F., Jr Prize reinforcement contingency management for cocaine dependence: integration with group therapy in a methadone clinic. Journal of consulting and clinical psychology. 2005;73(2):354. doi: 10.1037/0022-006X.73.2.354. [DOI] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, Li R. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: a national drug abuse treatment clinical trials network study. Archives of General Psychiatry. 2005;62(10):1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Austin M, Nich C, Carroll KM, Rounsaville BJ. Prize reinforcement contingency management for treating cocaine users: how low can we go, and with whom? Addiction. 2004;99(3):349–360. doi: 10.1111/j.1360-0443.2003.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, Ling W. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–274. doi: 10.1111/j.1360-0443.2006.01312.x. [DOI] [PubMed] [Google Scholar]
- Ribeiro M, Dunn J, Laranjeira R, Sesso R. High mortality among young crack cocaine users in Brazil: a 5-year follow-up study. Addiction. 2004;99:1133–1135. doi: 10.1111/j.1360-0443.2004.00804.x. [DOI] [PubMed] [Google Scholar]
- Ribeiro LA, Sanchez ZM, Nappo SA. Surviving crack: A qualitative study of the strategies and tactics developed by crack users to deal with the risks associated with the drug. BMC Public Health. 2010;10(671) doi: 10.1186/1471-2458-10-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos Cruz M, Andrade T, Bastos FI, Leal E, Bertoni N, Villar LM, Fischer B. Key drug use, health and socio-economic characteristics of young crack users in two Brazilian cities. International Journal of Drug Policy. 2013;24(5):432–438. doi: 10.1016/j.drugpo.2013.03.012. [DOI] [PubMed] [Google Scholar]
- Secades-Villa R, García-Rodríguez O, García-Fernández G, Sánchez-Hervás E, Fernandez-Hermida JR, Higgins ST. Community reinforcement approach plus vouchers among cocaine-dependent outpatients: Twelve-month outcomes. Psychology of Addictive Behaviors. 2011;25(1):174. doi: 10.1037/a0021451. [DOI] [PubMed] [Google Scholar]
- Secades-Villa R, García-Fernández G, Peña-Suárez E, García-Rodríguez O, Sánchez-Hervás E, Fernández-Hermida JR. Contingency management is effective across cocaine-dependent outpatients with different socioeconomic status. Journal of substance abuse treatment. 2013;44(3):349–354. doi: 10.1016/j.jsat.2012.08.018. [DOI] [PubMed] [Google Scholar]
- Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EJ, Schuster CR, Preston KL. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Archives of General Psychiatry. 1996;53(5):409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. World Drug Report 2015. Vienna: UN Office on Drugs and Crime; 2015. [Google Scholar]
- Von Diemen L, De Boni R, Kessler F, Benzano D, Pechansky F. Risk behaviors for HCV-and HIV-seroprevalence among female crack users in Porto Alegre, Brazil. Archives of women's mental health. 2010;13(3):185–191. doi: 10.1007/s00737-009-0089-y. [DOI] [PubMed] [Google Scholar]
- Weaver T, Metrebian N, Hellier J, Pilling S, Charles V, Little N, Strang J. Use of contingency management incentives to improve completion of hepatitis B vaccination in people undergoing treatment for heroin dependence: a cluster randomised trial. The Lancet. 2014;384(9938):153–163. doi: 10.1016/S0140-6736(14)60196-3. [DOI] [PubMed] [Google Scholar]
- Wood AM, White IR, Thompson SG. Are missing outcome data adequately handled? A review of published randomized controlled trials in major medical journals. Clinical trials. 2004;1(4):368–376. doi: 10.1191/1740774504cn032oa. [DOI] [PubMed] [Google Scholar]
- Zubaran C, Foresti K, Thorell MR, Franceschini P, Homero W. Depressive symptoms in crack and inhalant users in southern Brazil. Journal of Ethnicity in Substance Abuse. 2010;9(3):221–236. doi: 10.1080/15332640.2010.501626. [DOI] [PubMed] [Google Scholar]