Abstract
Remission is a primary end point of in clinical practice and trials of treatments for rheumatoid arthritis (RA). The 2011 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) remission criteria were developed to provide a consensus definition of remission. This study aimed to assess the concordance between the new remission criteria and the physician’s clinical judgment of remission and also to identify factors that affect the discordance between these two approaches. A total of 3,209 patients with RA were included from the KORean Observational Study Network for Arthritis (KORONA) database. The frequency of remission was evaluated based on each approach. The agreement between the results was estimated by Cohen’s kappa (κ). Patients with remission according to the 2011 ACR/EULAR criteria (i.e. the Boolean criteria) and/or physician judgment (n = 855) were divided into three groups: concordant remission, the Boolean criteria only, and physician judgment only. Multinomial logistic regression analysis was used to identify factors responsible for the assignment of patients with remission to one of the discordant groups rather than the concordant group. The remission rates using the Boolean criteria and physician judgment were 10.5% and 19.9%, respectively. The agreement between two approaches for remission was low (κ = 0.226) and the concordant remission rate was only 5.5% (n = 177). Pain affected classification in both discordant groups, whereas fatigue was associated with remission only by physician clinical judgment. The Boolean criteria were more stringent than clinical judgment. Patient subjective symptoms such as pain and fatigue were associated with discordance between the two approaches.
Keywords: Arthritis, Rheumatoid; Remission; Discordance
Graphical Abstract
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic inflammatory disease associated with substantial disability after a few years of disease progression (1). The ultimate objective in management of RA is to prevent disease progression, reduce or improve disability, and maintain quality of life. This objective can often be met by early treatment with disease-modifying anti-rheumatic drugs (DMARDs) (2). Advances in the treatment of RA have enabled the target of treatment for some patients to be remission, as has been highlighted in the most recent international guidelines for RA treatment (3,4,5). In addition, the ability of a new therapy to initiate a state of remission has been increasingly appreciated; for example, this goal has become a recommended outcome for clinical trials (6).
Remission in RA has been previously defined in several ways using different measurement instruments (7). However, the stringency of these different definitions has been shown to vary widely (8). Moreover, country-wide differences in remission rates have been suggested to vary according to the measuring instruments used in the different countries (9). In 2011, the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) developed new definitions of RA remission. These definitions were created to improve RA outcomes and decrease functional disability by ensuring more uniform reporting of outcomes (10). Previous studies that applied the 2011 ACR/EULAR remission criteria to data from observational cohorts have shown that these criteria are discordant with other classification criteria (11,12). The 2011 ACR/EULAR remission criteria provide the stringent definition of remission, but may be not always concordant with the state of remission defined by physician’s clinical judgment.
The purpose of this study was to assess the extent of concordance between the 2011 ACR/EULAR criteria and physician judgment of remission and to identify factors that influence the discordance between these two approaches.
MATERIALS AND METHODS
Data source and study participants
Patients over the age of 18 who satisfied the 1987 ACR classification criteria for RA and who were due to have blood samples taken for routine evaluation were recruited consecutively by rheumatologists in 23 centers. All patients were recruited during routine clinic visits as part of the KORean Observational Study Network for Arthritis (KORONA), a database generated by rheumatologists across South Korea from July 2009. All patients provided informed consent under the institutional review board (IRB)-approved study protocol. Patients were followed up annually and completed questionnaires to establish their demographic profiles, socio-economic statuses, and disease-specific outcomes. Further details of the study have been provided elsewhere (13). A total of 3,209 patients with RA were recruited.
Prevalence of remission according to each set of criteria
The prevalence of remission was estimated based on various definitions, including disease activity score (DAS) 28 - C reactive protein (CRP) (< 2.6), DAS28 - erythrocyte sedimentation rate (ESR) (< 2.6), simplified disease activity index (SDAI) (≤ 3.3), clinical disease activity index (CDAI) (≤ 2.8), and the 2011 ACR/EULAR remission criteria, which are Boolean criteria in which patients are considered to be in remission at any time point in time if they satisfy all of the following criteria: tender joint count (TJC) ≤ 1, swollen join t count (SJC) ≤ 1, CRP ≤ 1 mg/dL, and patient global assessment (PGA) ≤ 1 (on a 0–10 scale).
Each physician was also asked to assess his/her patient disease activity levels when he/she enrolled patients in this database. After dividing the patients into remission and nonremission groups, the extent of agreement between physician judgment and each set of criteria for remission was estimated.
Factors that influence the discordance between the Boolean criteria and physician judgment for remission
Patients with remission according to the Boolean criteria and/or physician judgment (n = 855) were divided into the following three groups: concordant (remission by both Boolean criteria and physician judgment), remission based on the Boolean criteria (remission only by Boolean criteria), and remission based on physician judgment (remission only by physician judgment). After comparing the baseline characteristics of patients in each group, we performed multinomial logistic regression analysis to identify the factors that affect the discordance between the Boolean criteria and physician judgment for determining remission in patients with RA.
Statistical analysis
The prevalence of remission was evaluated based on various definitions, including the Boolean criteria, the DAS28-CRP score, the DAS28-ESR score, and physician judgment. The prevalence of remission among all the patients with RA was determined. The agreement between the different criteria was estimated by Cohen’s kappa (κ). Factors influencing the discordance between the Boolean criteria and physician judgment for remission were identified by univariate analysis using the χ2 test and ANOVA. Multinomial logistic regression analysis identified factors that influenced both discordant groups compared with the concordant group with respect to remission. All data were analyzed with SPSS 21.0 (SPSS, Chicago, IL, USA); P values < 0.05 were considered statistically significant.
Ethics statement
This study was approved by the institutional review board of Hanyang University Hospital (HYUH IRB 2009-04-003). All participants provided informed consent under a protocol approved by the institutional review board.
RESULTS
Prevalence of remission in patients with RA
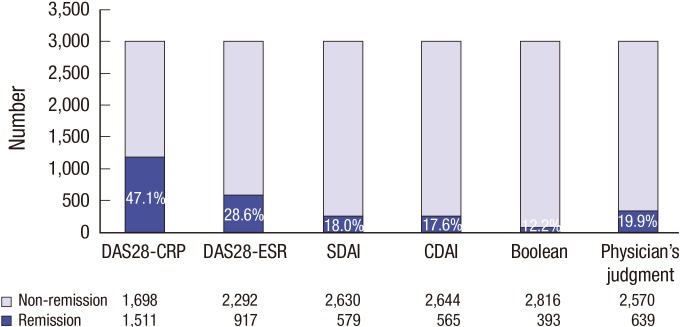
The remission rate was highest when it was based on the DAS28-CRP score (47.1%). A total of 1,511 patients had remission based on the DAS28-CRP score out of all enrolled patients (n = 3,209), whereas the other 1,698 patients had nonremission. Remission rates also varied among the other sets of criteria: 28.6% of patients (n = 921) had remission based on the DAS28-ESR score, 18.0% of patients (n = 579) had remission based on the SDAI, 17.6% of patients (n = 565) had remission based on the CDAI, and 12.2% of patients (n = 393) had remission based on the Boolean criteria. The physician-judged remission rate was 19.9% (n = 639) and the nonremission rate was 80.1% (n = 2,570) (Fig. 1).
Fig. 1.
Prevalence of remission in patients with RA according to each set of criteria.
DAS = disease activity score, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, SDAI = simplified disease activity index, CDAI = clinical disease activity index.
Agreement between each set of criteria and physician judgment of remission in patients with RA
The agreement rates between physician judgment and each set of criteria were in fair agreement (κ = 0.22–0.37); agreement was highest between physician judgment and the CDAI (κ = 0.37 in CDAI). When physician-judged remission was compared with Boolean criteria-judged remission, 78.9% of patients exhibited concordant classification and 21.1% of patients exhibited disconcordant classification between the two sets of criteria. Only 5.5% of all patients satisfied both sets of remission criteria. The rate of patients who satisfied the Boolean remission criteria but who were not judged in remission by physicians was 6.7%, whereas the rate of patients judged in remission by physicians but who did not satisfy the Boolean criteria was 14.4% (Table 1).
Table 1. Agreement between each set of criteria and physician judgment for RA remission.
| Remission criteria | DAS28-CRP | DAS28-ESR | SDAI | CDAI | Boolean criteria | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No remission | Remission | No remission | Remission | No remission | Remission | No remission | Remission | No remission | Remission | ||
| Physician judgment | No remission (%) | 1,533 (47.8) | 1,037 (32.3) | 2,013 (62.7) | 557 (17.4) | 2,286 (71.2) | 284 (8.9) | 2,296 (71.5) | 274 (8.5) | 2,354 (73.4) | 216 (6.7) |
| Remission (%) | 165 (5.1) | 474 (14.8) | 279 (8.7) | 360 (11.2) | 344 (10.7) | 295 (9.2) | 348 (10.8) | 291 (9.1) | 462 (14.4) | 177 (5.5) | |
| Kappa | 0.22 | 0.30 | 0.36 | 0.37 | 0.23 | ||||||
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||
DAS = disease activity score, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, SDAI = simplified disease activity index, CDAI = clinical disease activity index.
Characteristics of patients in remission according to the Boolean remission criteria and/or physician judgment
Patients were classified into three groups according to their classification by the Boolean criteria and physician judgment. Their demographic and clinical characteristics were compared between the following three groups: remission based on the Boolean criteria (n = 216), concordant remission (n = 177), and remission based on physician judgment (n = 462). Patients who satisfied both classification approaches were younger than patients in the other groups (51.6 ± 11.6 years vs. 54.1 ± 13.2 for remission by Boolean criteria and 54.8 ± 11.4 for remission by physician judgement, P = 0.007). Moreover, the proportion of female patients was lower in the group that satisfied both criteria (73.4%) than in the group that satisfied only the Boolean criteria (78.7%) or the group that satisfied only physician judgment (83.1%) (P = 0.020). With respect to laboratory tests, rheumatoid factor (RF) positivity (78.7% vs. 75.7% and 78.1%, P = 0.748) and abnormal ESR were common (44.0% vs. 20.9% and 32.9%, respectively, P < 0.001), while the prevalence of abnormal CRP was lower (8.8% vs. 14.8% and 20.1%, respectively, P = 0.001) in the concordant group than in the two other groups (Table 2).
Table 2. Characteristics of patients in remission according to the Boolean criteria and/or physician judgment.
| Variables | Remission based on the Boolean criteria (n = 216) | Concordant (n = 177) | Remission based on physician judgment (n = 462) | P |
|---|---|---|---|---|
| Demographics | ||||
| Age (years, median, IQR) | 54.5, 46.0, 62.0 | 52.0, 44.0, 59.0 | 55.0, 47.0, 63.0 | 0.007 |
| Female (No., %) | 170 (78.7) | 130 (73.4) | 384 (83.1) | 0.020 |
| Disease duration (years, median, IQR) | 5.1, 1.6, 10.4 | 5.4, 2.2, 10.1 | 5.7, 2.0, 11.2 | 0.345 |
| Education (No., %) | 0.059 | |||
| Less than high school | 80 (37.4) | 50 (28.6) | 191 (41.5) | |
| High school | 79 (34.6) | 74 (42.3) | 159 (34.6) | |
| College | 55 (25.7) | 51 (29.1) | 110 (23.9) | |
| Income level (No., %) | 0.304 | |||
| ≤ $19,999 | 94 (43.7) | 64 (36.4) | 207 (44.8) | |
| $20,000–$49,999 | 87 (40.5) | 76 (43.2) | 170 (36.8) | |
| ≥ $50,000 | 34 (15.8) | 36 (20.5) | 85 (18.4) | |
| BMI (No., %) | 0.297 | |||
| Underweight, < 18.5 | 24 (11.2) | 11 (6.2) | 30 (6.5) | |
| Normal, 18.5–22.9 | 104 (48.4) | 83 (46.9) | 241 (52.3) | |
| Pre-obese, 23–24.9 | 48 (22.3) | 44 (24.9) | 97 (21.0) | |
| Obese, ≥ 25 | 39 (18.1) | 39 (22.0) | 93 (20.2) | |
| Laboratory (No., %) | ||||
| Rheumatoid factor positive | 170 (78.7) | 134 (75.7) | 361 (78.1) | 0.748 |
| CRP positive | 32 (14.8) | 15 (8.5) | 93 (20.1) | 0.001 |
| ESR positive | 95 (44.0) | 37 (20.9) | 152 (32.9) | < 0.001 |
| Medication (No., %) | ||||
| Methotrexate | 186 (86.1) | 151 (85.3) | 364 (78.8) | 0.039 |
| Biologic DMARD | 9 (4.2) | 12 (6.8) | 42 (9.1) | 0.069 |
| Glucocorticoid | 138 (63.9) | 95 (53.7) | 272 (58.9) | 0.122 |
| NSAID | 107 (49.5) | 69 (39.0) | 206 (44.6) | 0.112 |
| Patient outcome (Mean ± SD) | ||||
| Tender joint count | 0.27 ± 0.44 | 0.12 ± 0.32 | 1.62 ± 3.13 | < 0.001 |
| Swollen joint count | 0.19 ± 0.39 | 0.06 ± 0.24 | 0.66 ± 1.75 | < 0.001 |
| HAQ-DI | 0.17 ± 0.28 | 0.09 ± 0.21 | 0.38 ± 0.45 | < 0.001 |
| Fatigue (10 cm VAS) | 1.6 ± 2.04 | 1.42 ± 1.98 | 3.91 ± 2.86 | < 0.001 |
| Sleep disturbance (10 cm VAS) | 0.62 ± 1.39 | 0.50 ± 1.18 | 1.91 ± 2.53 | < 0.010 |
| Pain (10 cm VAS) | 0.75 ± 1.18 | 0.47 ± 0.70 | 2.55 ± 2.33 | < 0.001 |
Concordant: remission by both Boolean criteria and physician judgment, Remission based on the Boolean criteria: remission only by the Boolean criteria, Remission based on physician judgment: remission only by physician judgment.
SD = standard deviation, BMI = body mass index, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, DMRAD = disease modifying anti-rheumatic drug, NSAID = non-steroidal anti-inflammatory disease, HAQ-DI = health assessment questionnaire disability index, VAS = visual analogue scale.
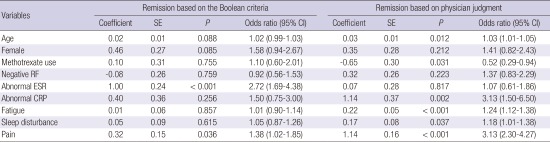
Factors that influence discordance between classification by the Boolean criteria and physician judgment for remission in patients with RA
Next, multinomial logistic regression analysis was performed to identify factors that influence the extent of discordance between classification by the Boolean criteria and physician judgment for remission, with the concordant group as reference. This analysis used variables found to be significant in univariate analysis (P < 0.05), such as age, sex, methotrexate use, RF positivity, abnormality of ESR or CRP, degree of fatigue, degree of sleep disturbance, and degree of pain.
The factors associated with remission only by the Boolean criteria were: abnormal ESR (odds ratio [OR], 2.72; 95% confidence interval [CI], 1.69–4.38) and a high level of pain (OR, 1.38; 95% CI, 1.02–1.85). The factors associated with remission only by physician judgment were: old age (OR, 1.03; 95% CI, 1.01–1.05), abnormal CRP (OR, 3.13; 95% CI, 1.50–6.50), fatigue (OR, 1.24; 95% CI, 1.12–1.38), and a high level of pain (OR, 3.13; 95% CI, 2.30–4.27) (Table 3).
Table 3. Factors that influence discordance between the Boolean criteria and physician judgment for remission* .
| Variables | Remission based on the Boolean criteria | Remission based on physician judgment | ||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | P | Odds ratio (95% CI) | Coefficient | SE | P | Odds ratio (95% CI) | |
| Age | 0.02 | 0.01 | 0.088 | 1.02 (0.99–1.03) | 0.03 | 0.01 | 0.012 | 1.03 (1.01–1.05) |
| Female | 0.46 | 0.27 | 0.085 | 1.58 (0.94–2.67) | 0.35 | 0.28 | 0.212 | 1.41 (0.82–2.43) |
| Methotrexate use | 0.10 | 0.31 | 0.755 | 1.10 (0.60–2.01) | -0.65 | 0.30 | 0.031 | 0.52 (0.29–0.94) |
| Negative RF | -0.08 | 0.26 | 0.759 | 0.92 (0.56–1.53) | 0.32 | 0.26 | 0.223 | 1.37 (0.83–2.29) |
| Abnormal ESR | 1.00 | 0.24 | < 0.001 | 2.72 (1.69–4.38) | 0.07 | 0.28 | 0.817 | 1.07 (0.61–1.86) |
| Abnormal CRP | 0.40 | 0.36 | 0.256 | 1.50 (0.75–3.00) | 1.14 | 0.37 | 0.002 | 3.13 (1.50–6.50) |
| Fatigue | -0.01 | 0.06 | 0.857 | 1.01 (0.90–1.14) | 0.22 | 0.05 | < 0.001 | 1.24 (1.12–1.38) |
| Sleep disturbance | 0.05 | 0.09 | 0.615 | 1.05 (0.87–1.26) | 0.17 | 0.08 | 0.037 | 1.18 (1.01–1.38) |
| Pain | 0.32 | 0.15 | 0.036 | 1.38 (1.02-–1.85) | 1.14 | 0.16 | < 0.001 | 3.13 (2.30–4.27) |
RF = rheumatoid factor, ESR = erythrocyte sedimentation rate, CRP = C-reactive protein.
*The total of 855 includes the concordant group (177 patients) as the reference group.
DISCUSSION
In the present study we found that 12.2% of all patients with RA in routine clinical care achieved remission by the 2011 ACR/EULAR remission criteria (i.e. the Boolean criteria). Compared with the other sets of remission criteria examined in this study (DAS28-ESR, DAS28-CRP, CDAI, SDAI, and physician clinical judgment), the Boolean criteria were the most stringent for identifying patients with RA remission. Poor agreement was observed between all sets of composite criteria and physician judgment for remission; the Boolean criteria showed the lowest level of agreement with physician judgment for remission. Patient subjective symptoms such as pain and fatigue, in addition to laboratory results such as CRP and ESR, were associated with discordance between classification by the Boolean criteria and physician judgment for remission.
In clinical practice, it is crucial to reach a consensus definition for remission in patients with RA, since the current treatment goal for RA is to achieve and maintain this state (3,4,5). Recently, treat-to-target strategies for RA treatment have been widely accepted, and periodic monitoring of disease activity of RA patients has been emphasized (3,4,5). However, despite the compelling evidence supporting this approach, adherence to the treat-to-target strategy in clinical practice is often low. This non-adherence is thought to arise from differences between the various composite measures of disease activity and physician judgment of remission. In the treat-to-target strategy, DAS, DAS28, CDAI, or SDAI should be employed to assess the disease activity of each patient. However, here we showed that the extent of agreement with each of these methods with physician judgment for remission varies widely. The agreement between CDAI and physician judgment was the highest. We hypothesize that this high level of agreement is because the CDAI includes a physician global assessment (0–10 cm) scale for estimating disease activity. In contrast, DAS28-CRP, the Boolean criteria, and physician judgement showed the lowest levels of agreement. This finding can be explained by a different reason; that is, the DAS28-CRP criteria are relatively loose, while the Boolean criteria for remission are more stringent.
Although either set of criteria can be used to define remission in patients with RA, the Boolean criteria may be most useful for predicting maintenance of remission or the possibility of drug discontinuation for patients who are in sustained remission, due to their stringency (14,15). Hence, it is important to understand the factors that affect discordance between the Boolean criteria and physician judgment of remission to decrease the gap between them.
We found that elevated ESR and high levels of subjective pain reported by patients were both associated with remission in patients who satisfied only the Boolean criteria, not physician judgment. Since the Boolean criteria included only CRP (and not ESR) as an inflammatory marker, this result is reasonable. Moreover, subjective patient pain does not always mean high disease activity (16). Therefore, if the pain felt by patients is communicated to physicians, pain can be a factor that influences discordance between the Boolean criteria and physician judgment.
On the other hand, the factors associated with patients in remission by physician judgment but not by the Boolean criteria were increased CRP, old age, and increased pain. We note that the Boolean criteria use a CRP cutoff of 1 mg/dL; however, our normal level in usual practice ranges from 0.3 mg/dL to 0.8 mg/dL at the different hospitals. When the measured CRP level is over the cut-off level at a particular hospital, physicians usually do not assert that such a patient is in remission. The data regarding old age and subjective pain point to another interesting observation, namely, older patients do not easily talk about their disease activity. We speculate that this barrier might influence patient-physician communication. Moreover, if physicians do not ask cautiously about patient feelings or global health, they may tend to judge disease activity of their patients based on objective physician examinations or lab test results. Previous reports have also shown that age and comorbidity can influence self-reported disability or pain; hence, these factors also need to be taken into account when interpreting remission or response rates in RA (17). Pain was associated with both discordances. However, its impact was stronger in the physician judgment classification as opposed to the Boolean criteria (OR, 3.13) than it was in remission in patients who satisfied only the Boolean criteria but not physician judgment (OR, 1.38). This finding indicates that pain has a greater influence on patient perception than on physician judgment. Previous reports have shown that patient-reported global health is influenced by pain, fatigue, and comorbid conditions (18,19,20). These factors may cause some patients to persistently score high on their global assessment components, even though they have low numbers of active joints and normal acute phase reactants. Ultimately, this discrepancy can lead to discordance about remission classification between methods that include patient-reported outcomes vs. physician judgment. Therefore, improving physician-patient communication about disease activity and pain holds promise to resolve this discordance between the Boolean criteria and physician judgment for classifying patients with RA in remission. Through this effort, patient-reported outcomes will be reflected in the decision-making by their physicians.
There are several limitations to our study. First, there is no official consensus about remission by physician judgment. Each physician has different background and experience; thus, physician judgment for remission may vary from person to person. However, it made physicians to define patients in remission advertently. The relatively low proportion of patients in remission by physician judgment can be explained by their stringent tendencies. Therefore, we considered it appropriate to compare two conservative definitions of remission (Boolean criteria vs. physician judgment). Second, in practice, physician judgment is usually based on both the current and past statuses of patients. Thus, it is inevitable that some differences will arise between physician judgment and the Boolean criteria. However, from this perspective, the Boolean criteria are considered to be superior to the other composite indices for identifying true patients in remission, because these criteria do not add individual values or constants to calculate disease activity. Because patient global assessments can reflect both the current and past statuses of disease activity of each patient, we expect that further follow-up studies would allow us to determine the extent of agreement between changes in disease activity and maintenance of remission. Third, we did not analyze the extent of discordance for each disease activity level. Since this study was conducted to compare each set of remission criteria (including the Boolean criteria) with physician judgment, we did not estimate the extent of agreement of each composite index to classify each level of disease activity. Since low disease activity is another aim for RA treatment, further analysis aimed at identifying patients with low disease activity will be helpful for informing decision making in clinical practice.
In conclusion, here we found that the Boolean criteria are more stringent than physician clinical judgment. Moreover, these two approaches have a low extent of agreement. Patient subjective symptoms such as pain and fatigue were associated with discordance between the two approaches.
ACKNOWLEDGMENT
The authors wish to acknowledge the assistance of the following investigators who have enrolled patients to KORONA: Drs. Joong Kyong Ahn, So-Young Bang, Sung Jae Choi, Minyoung Her, Chung-Il Joung, Young Ok Jung, Dong-Yook Kim, Hae-Rim Kim, Hyoun Ah Kim, Seong-Kyu Kim, Jaejoon Lee, Sang-Heon Lee, Sang-Hoon Lee, Seong-Su Nah, Seung-Cheol Shim, Dong Hyuk Sheen, Gwan Gyu Song, Chang-Hee Suh.
The authors gratefully acknowledge the assistance of eWorldEditing, Inc., in editing the manuscript.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R & D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI16C0061).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study design: Bae SC. Data collection and interpretation: Sung YK, Cho SK, Kim D, Yoon BY, Choi CB, Cha HS, Choe JY, Chung WT, Hong SJ, Jun JB, Kang YM, Kim J, Kim TH, Kim TJ, Koh E, Lee CK, Lee J, Lee SS, Lee SW, Lee HS, Lee YA, Park SH, Yoo DH, Yoo WH. Statistical analysis: Sung YK, Cho SK. Writing: Sung YK, Cho SK. Revision of manuscript: Sung YK, Cho SK, Bae SC. Final approval of the manuscript: all authors.
References
- 1.Kapetanovic MC, Lindqvist E, Nilsson JÅ, Geborek P, Saxne T, Eberhardt K. Development of functional impairment and disability in rheumatoid arthritis patients followed for 20 years: relation to disease activity, joint damage, and comorbidity. Arthritis Care Res (Hoboken) 2015;67:340–348. doi: 10.1002/acr.22458. [DOI] [PubMed] [Google Scholar]
- 2.van Nies JA, Krabben A, Schoones JW, Huizinga TW, Kloppenburg M, van der Helm-van Mil AH. What is the evidence for the presence of a therapeutic window of opportunity in rheumatoid arthritis? A systematic literature review. Ann Rheum Dis. 2014;73:861–870. doi: 10.1136/annrheumdis-2012-203130. [DOI] [PubMed] [Google Scholar]
- 3.Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, Combe B, Cutolo M, de Wit M, Dougados M, et al. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010;69:631–637. doi: 10.1136/ard.2009.123919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh JA, Saag KG, Bridges SL, Jr, Akl EA, Bannuru RR, Sullivan MC, Vaysbrot E, McNaughton C, Osani M, Shmerling RH, et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2016;68:1–26. doi: 10.1002/art.39480. [DOI] [PubMed] [Google Scholar]
- 5.Smolen JS, Landewé R, Breedveld FC, Buch M, Burmester G, Dougados M, Emery P, Gaujoux-Viala C, Gossec L, Nam J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis. 2014;73:492–509. doi: 10.1136/annrheumdis-2013-204573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aletaha D, Landewe R, Karonitsch T, Bathon J, Boers M, Bombardier C, Bombardieri S, Choi H, Combe B, Dougados M, et al. Reporting disease activity in clinical trials of patients with rheumatoid arthritis: EULAR/ACR collaborative recommendations. Arthritis Rheum. 2008;59:1371–1377. doi: 10.1002/art.24123. [DOI] [PubMed] [Google Scholar]
- 7.Smolen JS, Aletaha D. The assessment of disease activity in rheumatoid arthritis. Clin Exp Rheumatol. 2010;28:S18–27. [PubMed] [Google Scholar]
- 8.Mierau M, Schoels M, Gonda G, Fuchs J, Aletaha D, Smolen JS. Assessing remission in clinical practice. Rheumatology (Oxford) 2007;46:975–979. doi: 10.1093/rheumatology/kem007. [DOI] [PubMed] [Google Scholar]
- 9.Sokka T, Hetland ML, Mäkinen H, Kautiainen H, Hørslev-Petersen K, Luukkainen RK, Combe B, Badsha H, Drosos AA, Devlin J, et al. Remission and rheumatoid arthritis: data on patients receiving usual care in twenty-four countries. Arthritis Rheum. 2008;58:2642–2651. doi: 10.1002/art.23794. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, Aletaha D, Allaart CF, Bathon J, Bombardieri S, et al. American College of Rheumatology/European League against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis. 2011;70:404–413. doi: 10.1136/ard.2011.149765. [DOI] [PubMed] [Google Scholar]
- 11.Lee YC, Cui J, Lu B, Frits ML, Iannaccone CK, Shadick NA, Weinblatt ME, Solomon DH. Pain persists in DAS28 rheumatoid arthritis remission but not in ACR/EULAR remission: a longitudinal observational study. Arthritis Res Ther. 2011;13:R83. doi: 10.1186/ar3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaver TS, Anderson JD, Weidensaul DN, Shahouri SH, Busch RE, Mikuls TR, Michaud K, Wolfe F. The problem of rheumatoid arthritis disease activity and remission in clinical practice. J Rheumatol. 2008;35:1015–1022. [PubMed] [Google Scholar]
- 13.Sung YK, Cho SK, Choi CB, Park SY, Shim J, Ahn JK, Bang SY, Cha HS, Choe JY, Chung WT, et al. Korean observational study network for arthritis (KORONA): establishment of a prospective multicenter cohort for rheumatoid arthritis in South Korea. Semin Arthritis Rheum. 2012;41:745–751. doi: 10.1016/j.semarthrit.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Klarenbeek NB, Koevoets R, van der Heijde DM, Gerards AH, Ten Wolde S, Kerstens PJ, Huizinga TW, Dijkmans BA, Allaart CF. Association with joint damage and physical functioning of nine composite indices and the 2011 ACR/EULAR remission criteria in rheumatoid arthritis. Ann Rheum Dis. 2011;70:1815–1821. doi: 10.1136/ard.2010.149260. [DOI] [PubMed] [Google Scholar]
- 15.Hoshi D, Nakajima A, Shidara K, Seto Y, Tanaka E, Taniguchi A, Momohara S, Yamanaka H. Disability is the major negative predictor for achievement of Boolean-based remission in patients with rheumatoid arthritis treated with tocilizumab. Mod Rheumatol. 2013;23:1205–1210. doi: 10.1007/s10165-012-0825-4. [DOI] [PubMed] [Google Scholar]
- 16.Wolfe F, Boers M, Felson D, Michaud K, Wells GA. Remission in rheumatoid arthritis: physician and patient perspectives. J Rheumatol. 2009;36:930–933. doi: 10.3899/jrheum.080947. [DOI] [PubMed] [Google Scholar]
- 17.Krishnan E, Häkkinen A, Sokka T, Hannonen P. Impact of age and comorbidities on the criteria for remission and response in rheumatoid arthritis. Ann Rheum Dis. 2005;64:1350–1352. doi: 10.1136/ard.2005.037903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan NA, Spencer HJ, Abda E, Aggarwal A, Alten R, Ancuta C, Andersone D, Bergman M, Craig-Muller J, Detert J, et al. Determinants of discordance in patients’ and physicians’ rating of rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken) 2012;64:206–214. doi: 10.1002/acr.20685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho SK, Sung YK, Choi CB, Bang SY, Cha HS, Choe JY, Chung WT, Hong SJ, Jun JB, Kim J, et al. What factors affect discordance between physicians and patients in the global assessment of disease activity in rheumatoid arthritis? Mod Rheumatol. 2016 doi: 10.1080/14397595.2016.1176310. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 20.van Tuyl LH, Hewlett S, Sadlonova M, Davis B, Flurey C, Hoogland W, Kirwan J, Sanderson T, van Schaardenburg D, Scholte-Voshaar M, et al. The patient perspective on remission in rheumatoid arthritis: ‘You’ve got limits, but you’re back to being you again’. Ann Rheum Dis. 2015;74:1004–1010. doi: 10.1136/annrheumdis-2013-204798. [DOI] [PubMed] [Google Scholar]