Abstract
Various manifestations after bee sting have been described. Local reactions, such as pain, wheal, flare, edema and swelling, are common and generally self-limiting. Uncommonly manifestations like vomiting, diarrhea, dyspnea, generalized edema, acute renal failure, anaphylactic shock, myocardial infarction, hypotension, collapse, pulmonary hemorrhage, acute hemorrhagic pancreatitis, and atrial fibrillation may occur. We report a 59 year-old man who sustained ischemic stroke and multi-organ dysfunction following multiple bee stings.
Keywords: Bee sting, Acute stroke, Emergency department
1. Introduction
Venomous bites and stings from arthropods are a significant worldwide problem.1 Infrequently, a reaction to Hymenoptera venom produces neurologic, cardiovascular and urologic symptoms, with signs of encephalopathy, neuritis, vasculitis, and nephrosis.2 Neurologic manifestations are rare in bee venom poisoning.3, 4, 5, 6, 7, 8 Stroke and multi-organ dysfunction after bee stings are extremely rare.9 To the best of our knowledge this is the second ever case report of stroke after bee sting.
2. Case
A 59 year-old male patient who lives in a rural area was admitted to the closest state hospital after multıple bee stings (an estimated 50 bees) with complaints of mild shortness of breath, swelling, and itching of the lips. After the medical therapy (intramuscular adrenalin 0.5 mg, intravenous pheniramine maleate 45.5 mg and prednisolone 1 mg/kg) complaints of the patient were reduced and the patient was placed under observation. After one hour, the patient experienced a sudden loss of consciousness and was transferred to our hospital.
The patient's vital signs were a temperature of 36.5 °C, blood pressure of 140/90 mmHg, and respiratory rate of 14/min. On the neurological examination, the patient exhibited reduced consciousness with stupor. The patient's papillary light reflexes were bilaterally positive and cranial nerve exam revealed left central facial paralysis. Additionally, the patient had left hemiplegia. Cardiac and respiratory examinations were normal. Swelling was present in the patient's upper lip. His X-ray chest, electrocardiograph, echocardiography, carotid Doppler ultrasonography were normal. Biochemical parameters of the patient were as follows: blood glucose 78 mg/dl, blood urea nitrogen (BUN) 63.9 mg/dl, Creatinine (Cr) 3.80 mg/dl, aspartate aminotransferase (AST) 2362 U/lt, alanine aminotransferase (ALT) 1453 U/lt, sodium (NA) 138 mEq/L, potassium 6.36 mEq/L, creatine phosphokinase (CK) 2981 IU/L, prothrombin time (PT) 48 seconds, partial thromboplastin time (aPTT) 48 seconds, international normalized ratio (INR) 1.8, and troponin I 1.5 μg/lt. Blood gas analysis was normal. The patient's relatives related that the patient had a medical history of hypertension, and a short time ago the advent of a mild allergic reaction due to bee stings.
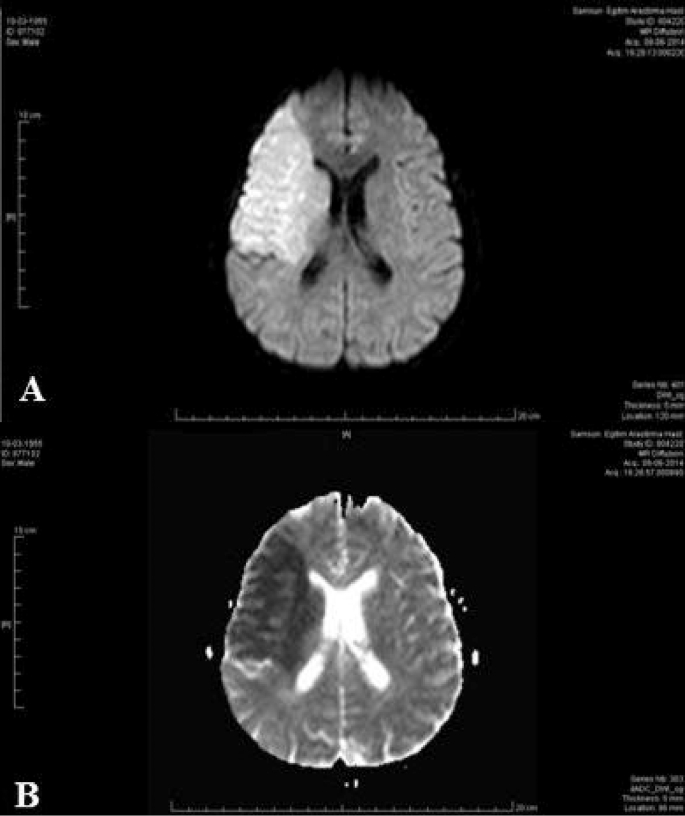
With an initial diagnosis of acute ischemic stroke, the patient was consulted to the neurology department. There were no pathologic findings in the computed tomography of the patient (Fig. 1). On the diffusion magnetic resonance imaging (MRI), an acute infarction was detected extending from the right frontotemporal region to the parietal region (Fig. 2). The patient was transferred to the intensive care unit and medical treatment was started. On the second day of follow-up, the patient experienced ventricular tachycardia, and after electrical cardioversion normal cardiac rhythm was obtained. On the third day of follow-up, the condition of the patient worsened and respiratory failure was developed. The patient was intubated and connected to a mechanical ventilator. On the fourth day of follow-up, cardiac arrest developed. Despite cardiopulmonary resuscitation, normal cardiac rhythm could not be obtained and the patient was announced expired.
Fig. 1.
Axial computerized tomography image of patient. There is no acute changing.
Fig. 2.
Diffusion-weighted MRI imaging shows hyperintensity on rontotemporoparietal region of the brain (a)and apparent diffusion coefficient MRI imaging shows hypointensity on frontotemporoparietal region(b).
3. Discussion
Hymenoptera stings cause local reactions such as immediate pain, wheal and flare reaction, which resolve within a few hours. Stings from accidentally swallowed insects may induce life-threatening edema of the upper airways. Multiple stings can lead to vomiting, diarrhea, generalized edema, dyspnoea, rhabdomyolysis, intravascular hemolysis, and renal failure.8 Neurologic reactions, including stroke after bee stings, are very rare.3, 4, 5, 6, 7, 8
The pathophysiology to explain the stroke after bee sting is unknown. The postulated mechanisms include: 1) Hypotension caused by anaphylaxis may induce cerebral and optic nerve ischaemia(3), 2) Vasoconstriction secondary to mediators released after the sting, aggravated by exogenous adrenaline, and platelet aggregation may contribute to cerebral ischaemia, and 3) Bee venom itself contains histamine, thromboxane, leucotrienes, and other vasoactive and inflammatory mediators leading to cerebral ischaemia. Both thromboxane and leukotrienes have been shown to cause vasoconstriction resulting in cerebral infarction.5 In our patient, we thought that the systemic immune-mediated reaction due to the bee sting caused vasoconstriction and a prothrombotic state with subsequent ischaemia leading to stroke.
Acute renal failure is also an unusual complication of bee stings. Although acute renal failure after bee stings is typically caused by tubular necrosis in the setting of hemolysis or rhabdomyolysis, in some cases, acute renal failure may result from a direct nephrotoxic effect of a hypersensitivity reaction.10 In our opinion, acute renal failure may have resulted from rhabdomyolysis in our patient. Promising markers such as neutrophil gelatinase-associated lipocalin and pro-enkephalin may be useful in these patients to determine both presence and prognosis of renal failure.11, 12
Reported cardiovascular complications of bee stings include acute myocardial infarction in patients with normal and abnormal coronary arteries.13, 14 We suggested that in our patient, ventricular dysrhythmia seems to be related to the release of vasoactive amines and thrombogenic substances that are in the hymenopterans venom, the former able to produce vasospasm, the latter able to ventricular dysrhythmia.
The hepatotoxic effects of bee stings is unknown. The postulated mechanisms are: 1) Venom damages hepatic cellular membranes, and mitochondria are most severely injured,15 and 2) Hypotension caused by anaphylaxis induces liver ischaemia.16 Our patient never had hypotension during his intensive care follow-up period, so the second mechanism does not seem likely. We suggest that hepatotoxic effects seen in our patient were caused by first mechanism.
We believe that tissue damage caused by wasp venom was the possible reason for development of stroke and multi-systemic injury.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
References
- 1.White J. Bites and stings from venomous animals: a global overview. Ther Drug Monit. 2000;22:65–68. doi: 10.1097/00007691-200002000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Jones R.G., Corteling R.L., Bhogal G., Landon J. A novel Fab-based antivenom for the treatment of mass bee attacks. Am J Trop Med Hyg. 1999;61:361–366. doi: 10.4269/ajtmh.1999.61.361. [DOI] [PubMed] [Google Scholar]
- 3.Crawley F., Schon F., Brown M.M. Cerebral infarction: a rare complication of wasp sting. J Neurol Neurosurg Psychiatry. 1999;66:550–551. doi: 10.1136/jnnp.66.4.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sachdev A., Mahapatra M., D'Cruz S., Kumar A., Singh R., Lehl S.S. Wasp sting induced neurological manifestations. Neurol In-dia. 2002;50:319–321. [PubMed] [Google Scholar]
- 5.Riggs J.E., Ketonen L.M., Wymer J.P., Barbano R.L., Valanne L.K., Bodensteiner J.B. Acute and delayed cerebral infarction after wasp sting anaphylaxis. Clin Neuropharmacol. 1994;17:384–388. doi: 10.1097/00002826-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Bilir O., Ersunan G., Kalkan A., Ozmen T., Yigit Y. A different reason for cerebrovascular disease. Am J Emerg Med. 2013;31(891):e5–e6. doi: 10.1016/j.ajem.2012.12.040. [DOI] [PubMed] [Google Scholar]
- 7.An J.Y., Kim J.S., Min J.H., Han K.H., Kang J.H., Lee S.W. Hemicho-rea after multiple bee stings. Am J Emerg Med. 2014;32(196):e1–e2. doi: 10.1016/j.ajem.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Starr J.C., Brasher G.W. Wasp sting anaphylaxis with cerebral infarction. Ann Allergy. 1977;39:431–433. [PubMed] [Google Scholar]
- 9.Wani M., Saleem S., Verma S., Yousuf I., Wani M., Asimi R. Multiple cerebral infarctions with severe multi-organ dys-function following multiple wasp stings. Ann Indian Acad Neurol. 2014;17:125–127. doi: 10.4103/0972-2327.128581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Das R.N., Mukherjee K. Asian wasp envenomation and acute renal failure: a report of two cases. Mcgill J Med. 2008;11:25–28. [PMC free article] [PubMed] [Google Scholar]
- 11.Di Somma S., Magrini L., De Berardinis B., Marino R., Ferri E., Moscatelli P. Additive value of blood neutrophil gelatin-ase-associated lipocalin to clinical judgement in acute kidney injury diagnosis and mortality prediction in patients hospital-ized from the emergency department. Crit Care. 2013;17:R29. doi: 10.1186/cc12510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marino R., Struck J., Hartmann O., Maisel A.S., Rehfeldt M., Magri-ni L. Diagnostic and short-term prognostic utility of plasma pro-enkephalin (pro-ENK) for acute kidney injury in patients admitted with sepsis in the emergency department. J Nephrol. 2015;28:714–724. doi: 10.1007/s40620-014-0163-z. [DOI] [PubMed] [Google Scholar]
- 13.Wagdi P., Mehan V.K., Bürgi H., Salzmann C. Acute myocardial infarction after wasp stings in a patient with normal coronary arteries. Am Heart J. 1994;128:820–823. doi: 10.1016/0002-8703(94)90282-8. [DOI] [PubMed] [Google Scholar]
- 14.Jones E., Joy M. Acute myocardial infarction after a wasp sting. Br Heart J. 1988;59:506–508. doi: 10.1136/hrt.59.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neuman M.G., Ishay J., zimmerman M., Eshchar J. Hepatotox-icity of oriental hornet venom. Article Hebr Harefuah. 1990;118:78–80. [Abstract] [PubMed] [Google Scholar]
- 16.Park S., Chun H.J., Keum B., Seo Y.S., Kim Y.S., Jeen Y.T. Ana-phylactic shock-induced ischemic proctocolitis following bee stings: first case report. Endoscopy. 2010;42(Suppl 2):E153–E154. doi: 10.1055/s-0029-1244101. [DOI] [PubMed] [Google Scholar]