Abstract
Vitamin C is widely used in clinical settings and is well known for its safety. Previous studies have shown the efficacy of intravenous vitamin C; however, intratumoral delivery of vitamin C has yet to be attempted. In the present study, the biological effects of high-dose vitamin C on tumor cells were investigated in vitro by using the MTT assay and flow cytometry. When administered in vitro, high-dose vitamin C inhibited the proliferation of murine colon and breast cancer cells, and induced tumor cell apoptosis. Cytotoxicity of vitamin C was partially reversed by N-acetyl-cysteine at a relatively low dosage. In addition, synergistic anti-tumor effects of vitamin C and cisplatin were observed. In vivo, intratumoral delivery of vitamin C delayed tumor growth in murine solid tumor models. Considering its low toxicity and availability, the present study indicates that vitamin C may be a novel therapeutic method for patients with advanced tumors.
Keywords: vitamin C, tumor, proliferation, apoptosis, N-acetyl-cysteine, chemotherapy
Introduction
Vitamin C, also termed ascorbic acid, has been widely used, orally and parenterally, in clinical settings and is vital to human health. Vitamin C typically functions in the prevention and treatment of the common cold, hypersensitivity and viral infection, and is anti-aging (1–3). Recently, evidence has emerged to suggest that vitamin C has additional functions other than its anti-oxidant ability. Vitamin C activates the Jak-Stat2 signaling pathway and enhances Nanog expression (4), which has been demonstrated to be a direct target of TLR4 (5) and is associated with stem cell properties (6,7). Vitamin C induces the generation of induced pluripotent stem cells (iPSCs) (8) and the transition from pre-iPSCs to iPSCs (9). Vitamin C also inhibits the retinoid acid-induced differentiation of mouse embryonic stem cells (4).
In addition to its use as an auxiliary treatment for patients with cancer, attempts have been made to utilize vitamin C as a more substantial therapeutic agent for patients with cancer. Although vitamin C is an unorthodox therapeutic agent for cancer, previous studies have supported the hypothesis that vitamin C restricts metastatic spread via collagen deposition and hyaluronidase inhibition (10,11). Intravenous ascorbate has been reported to be effective at prolonging patient survival times in terminal human cancer (12). A recent report has shown that high-dose parenteral ascorbate is able to enhance chemosensitivity of carboplatin and paclitaxel in an ovarian cancer model (13). Vitamin C may represent an attractive and innovative therapeutic strategy for patients with cancer. At present, the majority of preclinical studies and clinical trials in this field are investigating the oral or parenteral administration of vitamin C; however, no previous studies have reported local delivery of vitamin C into the tumor microenvironment.
In the present study, the direct tumoricidal effect of vitamin C in murine cancer was assessed. The present study provides a rationale for reexamining vitamin C treatment in patients with cancer.
Materials and methods
Cell lines and reagents
Murine 4T1 breast cancer cells and CT26 colon cancer cells (both American Type Culture Collection, Manassas, VA, USA) were maintained in RPMI-1640 (Gibco-BRL, Carlsbad, CA, USA), supplemented with 10% fetal bovine serum (both Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) in a humidified atmosphere containing 5% CO at 37°C. Cisplatin was obtained from the West China Hospital, Sichuan University (Chengdu, China). NAC and vitamin C and were purchased from Sigma-Aldrich (Merck Millipore, Darmstadt, Germany).
MTT assay
A total of 3,000 tumor cells/well were seeded in 96-well plates. Tumor cells were subsequently exposed to 100 and 200 µg/ml vitamin C the following day. At 0, 24, 48 and 72 h, MTT reagent (Sigma-Aldrich; Merck Millipore) was added to each well and incubated for 4 h at 37°C. Cell supernatant was subsequently removed and formazan precipitates were dissolved in 150 µl dimethyl sulfoxide. Optical density 570 nm was detected and a growth curve was plotted.
Flow cytometry
CT26 tumor cells (5×104) were exposed to 200, 500 and 1,000 µg/ml vitamin C. Following 24 h, tumor cells were stained using an Annexin-V-fluorescein isothiocyanate (FITC) and propidium iodide (PI) kit (Roche Diagnostics GmbH, Mannheim, Germany; cat. no. 11988549001), according to the manufacturer's protocol. For flow cytometry analysis, cells were analyzed with a FACSCalibur flow cytometer and CellQuest software (version 6.0) (both BD Biosciences, San Jose, CA, USA). To assess the synergistic effect of vitamin C and chemotherapy, CT26 tumor cells were exposed to 1 mg/ml cisplatin and 200 µg/ml vitamin C for 48 h. Apoptotic cells were examined by flow cytometry.
Blockade assay
CT26 tumor cells were treated with 200, 500 and 1,000 µg/ml vitamin C for 24 h. To antagonize the cytotoxicity of vitamin C, tumor cells were simultaneously exposed to 2 mM N-acetyl-cysteine. Apoptotic cells were assessed by flow cytometry (BD Biosciences).
Animal models
Animal experiments were approved by the Ethics Committee of Sichuan University (Chengdu, China). Female BALB/c mice (8–10 weeks old; 20±3 g; n=33) were purchased from Vital River Laboratories, Co., Ltd. (Beijing, China). Mice were maintained under pathogen-free conditions at between 21 and 27°C, a humidity of between 40 and 60%, a light/dark cycle of 12 h and ad libitum access to food and water. For subcutaneous tumor models, 1×106 4T1 cells were subcutaneously inoculated into the right flanks of BALB/c mice (n=15). CT26 tumor cells were subcutaneously inoculated into the right flanks of BALB/c mice (n=18). Eight days post-inoculation, when palpable tumors reached ~90 mm3, vitamin C was delivered intratumorally into tumors. Tumor-bearing mice were randomly divided into three groups: Control, 1ow-dose and high-dose groups (4T1, n=5 for each group; CT26, n=6 for each group). Tumor growth was monitored by measuring i) large and ii) short length with a sliding caliper. Tumor volume was calculated as: Tumor volume = a × b2 × 0.52.
Statistical analysis
Statistical analysis was performed using Student's t-test between two groups, and one-way analysis of variance between more than two groups. Results were expressed as the mean ± standard deviation. P<0.05 was considered to indicate a statistically significant difference.
Results
Vitamin C inhibits tumor cells proliferation
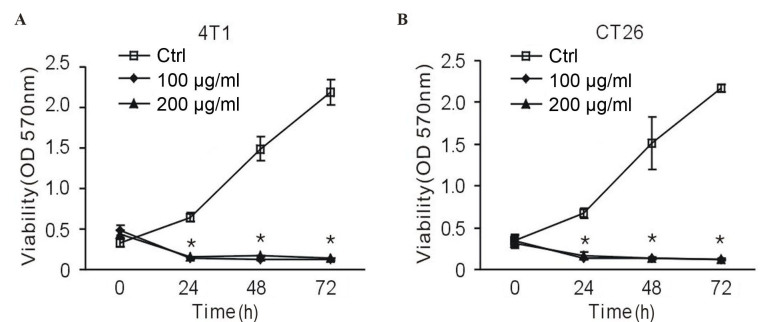
To investigate whether vitamin C influenced the proliferation of tumor cells, an MTT assay was performed. In the presence of vitamin C, 4T1 murine breast cancer cells exhibited a reduced proliferation rate; however, there was no dose-dependent effect. A significant suppressive effect began at 24 h, and persisted over the course of treatment (P<0.01 vs. the control group; Fig. 1A). To demonstrate that vitamin C is universally cytotoxic or cytostatic, it was assessed against additional cells lines. Notably, 100 and 200 µg/ml vitamin C exhibited a significantly suppressive effect on CT26 murine colon cancer cells at 24, 48 and 72 h (P<0.01 vs. the control group; Fig. 1B). This data suggests that high-dose vitamin C inhibits tumor cell proliferation.
Figure 1.
Vitamin C inhibits tumor cell proliferation. (A) Murine 4T1 breast cancer cells and (B) CT26 colon cancer cells were treated with 100 and 200 µg/ml vitamin C for 72 h. MTT assays were performed at 0, 24, 48 and 72 h. Vitamin C significantly inhibited tumor cells proliferation in vitro. *P<0.01 vs. the control group. OD, optical density; ctrl, control.
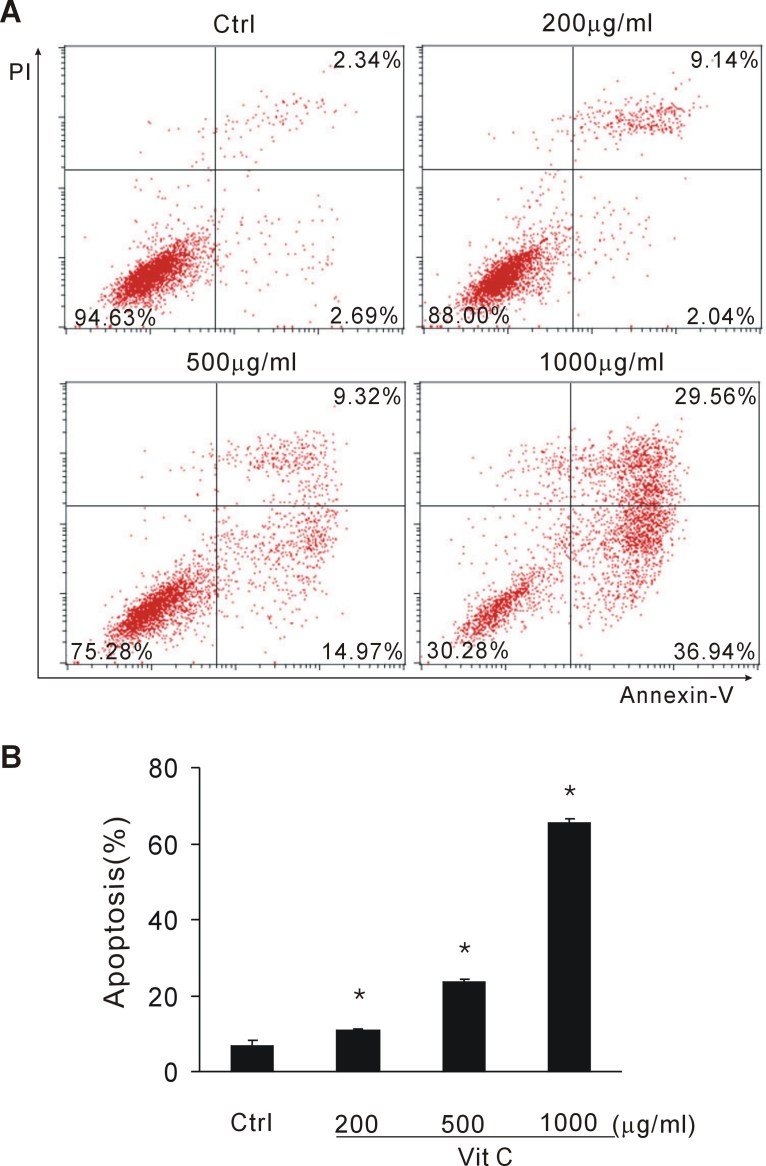
Vitamin C induces apoptosis in vitro
To investigate whether vitamin C induced apoptosis of tumor cells, CT26 tumor cells exposed to vitamin C were stained with Annexin-V and PI. Early and late apoptotic cell fractions were determined by flow cytometry. When exposed to >200 µg/ml vitamin C, tumor cells underwent apparent apoptosis. In the present experiment, 200, 500 and 1,000 µg/ml vitamin C significantly induced tumor cell apoptosis in a dose-dependent manner (P<0.05 vs. the control group; Fig. 2A and B). This data suggests that a large dose of vitamin C induces tumor cell apoptosis.
Figure 2.
Vit C induces tumor cells apoptosis. CT26 tumor cells were exposed to various doses of vitamin C for 24 h. Flow cytometry was performed. (A) Representative flow cytometry of CT26 cells treated with 200 µg/ml vit C; (B) quantification of apoptotic cells following exposure to various doses of vit C. High doses of vit C induced the apoptosis of tumor cells. *P<0.05 vs. the control group. Ctrl, control; vit, vitamin.
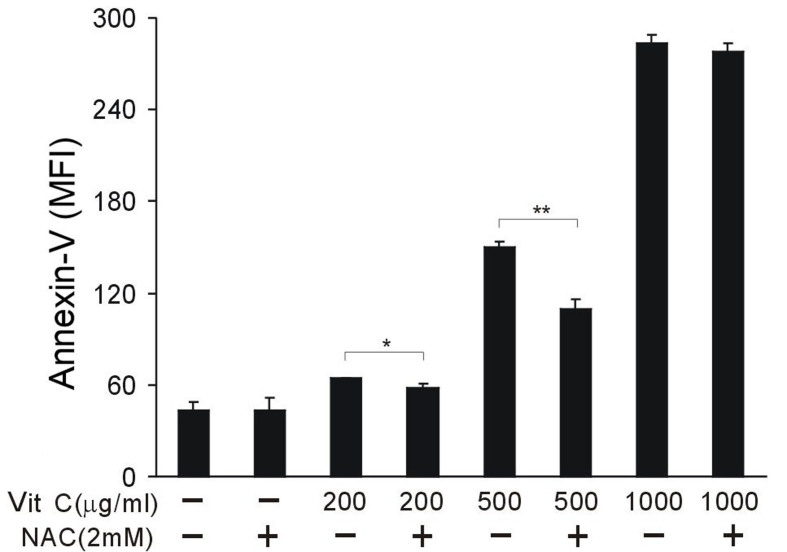
NAC partially antagonizes the tumoricidal effect of vitamin C
To investigate the key mechanism of vitamin C, NAC was used to block the tumoricidal effect of vitamin C. A total of 2 mM NAC was used per sample. NAC did not cause observable toxicity to CT26 cancer cells. NAC was able to partially reverse the effect of vitamin C and protected tumor cells from cell death when vitamin C was administered at 200 and 500 µg/ml; however, NAC was not able to block the cytotoxicity of 1,000 µg/ml vitamin C (P<0.05; Fig. 3). These results indicate that vitamin C function, in this context, may be unrelated to its antioxidant activity, and inversely, oxidative stress suppression may partially antagonize the tumoricidal effect of a relatively low dose of vitamin C.
Figure 3.
NAC partially antagonizes the tumoricidal effect of vit C. CT26 tumor cells were treated with 200, 500 and 1,000 µg/ml vit C for 24 h, and 2 mM NAC was used to block the effect of vit C. Annexin-V-positive apoptotic cells were assessed by flow cytometry. NAC antagonized the cytotoxicity of vitamin C. *P<0.05 vs. (−) NAC group in the presence of 200 µg/ml vit C; **P<0.01 vs. (−) NAC group in the presence of 500 µg/ml vit C. NAC, N-acetyl-cysteine; Vit, vitamin; MFI, mean fluorescence intensity.
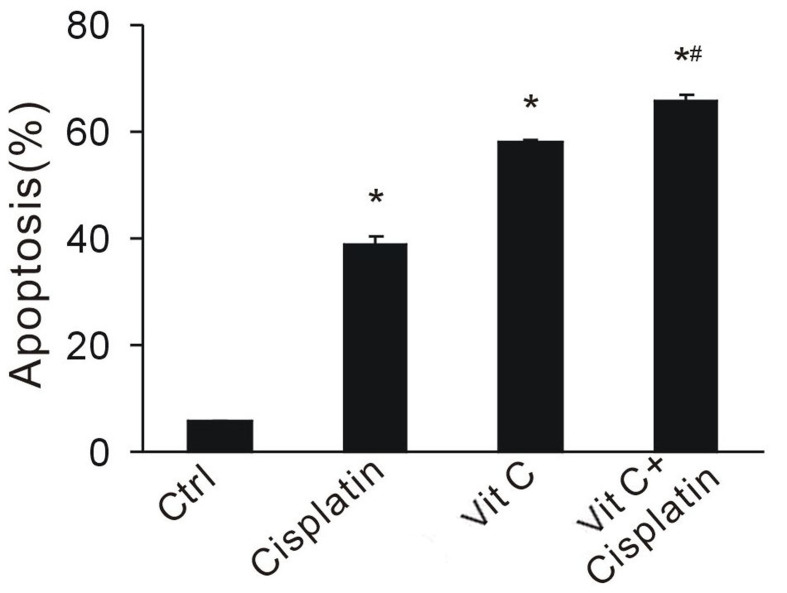
Vitamin C enhances the anti-tumor effect of cisplatin
Various chemotherapeutical agents, such as cisplatin, rely on the redox system to kill cancer cells. To investigate whether vitamin C enhances the anti-tumor effect of chemotherapy, a large dose of vitamin C was administered in combination with cisplatin. Apoptotic cell fractions were determined by flow cytometry. Vitamin C and cisplatin significantly increased cell apoptosis (P<0.05 vs the control group; Fig. 4). CT26 cancer cells exposed to both drugs exhibited the highest apoptotic rates, indicating the synergistic effect of combination treatment (Fig. 4). This data suggests that vitamin C enhances the effect of chemotherapy, and may provide a rationale for combination therapy.
Figure 4.
Vit C enhances the anti-tumor effect of cisplatin. CT26 tumor cells were treated with 1 mg/ml cisplatin and/or 200 µg/ml vit C for 48 h. Flow cytometry was performed to assess the synergistic anti-tumor effect. The addition of vit C enhanced the anti-tumor effect of chemotherapy. *P<0.05 vs. control; #P<0.05 vs. cisplatin or vitamin C single drug. Vit, vitamin; ctrl, control.
Local delivery of vitamin C is effective for cancer treatment
To investigate the anti-tumoral effect of vitamin C in vivo, 4T1 and CT26 tumor-bearing mice were treated intratumorally with dose-escalating vitamin C. Drug schedules were as indicated in Fig. 5A and B. Over the course of treatment, CT26 tumor-bearing BALB/c mice displayed a marked response to vitamin C (Fig. 5C). Tumor volume markedly decreased in the low-dose group, whereas a significant decrease was detected in the high-dose group, indicating a dose-dependent effect (P<0.05 vs. the control group; Fig. 5C). Significant diminution of 4T1 tumor growth was observed following low– and high-dose vitamin C treatment (P<0.05 vs. the control group; Fig. 5D). Therefore, the ability of vitamin C to restrain tumor growth was not limited by the type of tumors being examined. This data indicates that local delivery of vitamin C may be effective for tumor growth retardation.
Figure 5.
Intratumoral delivery of escalating doses of vitamin C retards tumor growth. Scheme of drug administration in (A) CT26 and (B) 4T1 tumor-bearing mice. (C) Mice bearing CT26 cancer cells were treated with vitamin C. Tumor volume was tracked and calculated at the 26th day (n=6). (D) 4T1 tumor-bearing mice were treated with vitamin C. Tumor volume was tracked and calculated at 32nd day (n=5). *P<0.05 vs. control; ctrl, control.
Discussion
The present study investigated the biological effects of large doses of vitamin C on murine tumor cells in vitro and in vivo. This anti-tumoral agent, with a high safety profile, was effective whether used alone or in combination with cisplatin chemotherapy in the present study. In addition, intratumoral delivery of vitamin C significantly retarded tumor growth in murine solid tumor models.
Vitamin C has previously been used as an unorthodox therapy for patients with cancer (14); however, in most clinical settings, vitamin C is used as an auxillary treatment and the dosage is low. Low-dose vitamin C (25–50 µg/ml) does not induce apoptosis; conversely, it is associated with stem cell proliferation and maintenance (4,8). Previous studies have shown that high-dose vitamin C (10 g/day) is effective at treating cancer (12). In the present study, murine CT26 colon cancer cells were used. Low-dose vitamin C (25–50 µg/ml) induced minimal apoptosis. However, the larger dose had a cytotoxic/cytostatic effect and induced marked cell apoptosis. In addition, dose-escalating vitamin C yielded a measurable and significant anti-tumor effect in vivo. These findings provide a rationale for further investigation of this phenomenon to elucidate the association between vitamin C and cancer stem cells.
The mechanism of action of vitamin C for cancer treatment remains unclear. Several hypotheses have been suggested. Vitamin C acts as a cofactor in various reactions driven by dioxygenases, including histone demethylases, hypoxia-inducible factor prolyl hydroxylases and collagen prolyl hydroxylases (15). Vitamin C inhibits the enzymatic activity of hyaluronidase, which otherwise destroys collagen (11); thus through strengthening the collagen structure, vitamin C restrains tumor cell metastasis. In a recent paper, Ma et al (13) suggest that the anti-tumor effect of vitamin C is due to pro-oxidative properties, which activate ATM/AMPK and inhibit the mTOR pathway in ovarian cancer cells. Vitamin C, within pharmacological concentrations, forms ascorbate radicals which produce hydrogen peroxide in extracellular fluid that are cytotoxic to various cancer cells (16). In the present study, NAC, a well-known anti-oxidant agent (17), was demonstrated to antagonize the anti-tumor effect of a relatively low dose of vitamin C (200 and 500 µg/ml). However, NAC was not able to block the cytotoxicity of 1,000 µg/ml vitamin C. Additional studies are required to fully explore the mechanism of vitamin C against cancer cells.
Delivery route influences the effect of vitamin C. Intravenous vitamin C and orally administered vitamin C were demonstrated to induce apoptosis in tumor cells; however, it has previously been demonstrated that the same dose of vitamin C was ineffective when administered orally (18). Furthermore, a previous study has determined that orally administered and intravenous vitamin C have different pharmacokinetics (19). When administered orally, plasma and tissue concentrations of vitamin C are influenced by absorption, tissue transport and renal excretion processes (20); whereas intravenous vitamin C bypasses the absorption process, thus high plasma concentrations are easily maintained. Although intravenous doses as high as 1.5 g/kg vitamin C are tolerated by patients with normal renal function and glucose-6-phosphate dehydrogenase (G6PD) activity (21), the clinical use of vitamin C should be carefully monitored, as G6PD is not commonly detected by clinical tests. Considering these defects, a local delivery strategy may prove most beneficial to the treatment of patients with cancer. In vitro experiments showed the cytotoxic effect of vitamin C; therefore, vitamin C was injected directly into solid tumors. This routine was demonstrated to be safe and effective in tumor-bearing mice.
In conclusion, the present study demonstrated the cytotoxic effect of large dose vitamin C. Considering its low toxicity and high availability, intratumoral delivery of vitamin C may provide a therapeutic option for those with advanced tumors.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (grant no. 81501609) and the Chinese Postdoctoral Science Foundation (grant no. 81301980).
References
- 1.Klenner FR. The treatment of poliomyelitis and other virus diseases with vitamin C. South Med Surg. 1949;111:209–214. [PubMed] [Google Scholar]
- 2.Bansal P, Saw S, Govindaraj D, Arora N. Intranasal administration of a combination of choline chloride, vitamin C, and selenium attenuates the allergic effect in a mouse model of airway disease. Free Radic Biol Med. 2014;73:358–365. doi: 10.1016/j.freeradbiomed.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 3.Padayatty SJ, Sun AY, Chen Q, Espey MG, Drisko J, Levine M. Vitamin C: Intravenous use by complementary and alternative medicine practitioners and adverse effects. PLoS One. 2010;5:e11414. doi: 10.1371/journal.pone.0011414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu H, Wu Y, Ai Z, Yang L, Gao Y, Du J, Guo Z, Zhang Y. Vitamin C enhances Nanog expression via activation of the JAK/STAT signaling pathway. Stem Cells. 2014;32:166–176. doi: 10.1002/stem.1523. [DOI] [PubMed] [Google Scholar]
- 5.Chen CL, Tsukamoto H, Liu JC, Kashiwabara C, Feldman D, Sher L, Dooley S, French SW, Mishra L, Petrovic L, et al. Reciprocal regulation by TLR4 and TGF-β in tumor-initiating stem-like cells. J Clin Invest. 2013;123:2832–2849. doi: 10.1172/JCI65859. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Cavaleri F, Schöler HR. Nanog: A new recruit to the embryonic stem cell orchestra. Cell. 2003;113:551–552. doi: 10.1016/S0092-8674(03)00394-5. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki A, Raya A, Kawakami Y, Morita M, Matsui T, Nakashima K, Gage FH, Rodríguez-Esteban C, Izpisúa Belmonte JC. Nanog binds to Smad1 and blocks bone morphogenetic protein-induced differentiation of embryonic stem cells. Proc Natl Acad Sci USA. 2006;103:10294–10299. doi: 10.1073/pnas.0506945103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esteban MA, Wang T, Qin B, Yang J, Qin D, Cai J, Li W, Weng Z, Chen J, Ni S, et al. Vitamin C enhances the generation of mouse and human induced pluripotent stem cells. Cell Stem Cell. 2010;6:71–79. doi: 10.1016/j.stem.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Silva J, Barrandon O, Nichols J, Kawaguchi J, Theunissen TW, Smith A. Promotion of reprogramming to ground state pluripotency by signal inhibition. PLoS Biol. 2008;6:e253. doi: 10.1371/journal.pbio.0060253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCormick WJ. Cancer: The preconditioning factor in pathogenesis; a new etiologic approach. Arch Pediatr. 1954;71:313–322. [PubMed] [Google Scholar]
- 11.Cameron E, Rotman D. Ascorbic acid, cell proliferation, and cancer. Lancet. 1972;1:542. doi: 10.1016/S0140-6736(72)90215-2. [DOI] [PubMed] [Google Scholar]
- 12.Cameron E, Pauling L. Supplemental ascorbate in the supportive treatment of cancer: Reevaluation of prolongation of survival times in terminal human cancer. Proc Natl Acad Sci USA. 1978;75:4538–4542. doi: 10.1073/pnas.75.9.4538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma Y, Chapman J, Levine M, Polireddy K, Drisko J, Chen Q. High-dose parenteral ascorbate enhanced chemosensitivity of ovarian cancer and reduced toxicity of chemotherapy. Sci Transl Med. 2014;6:222ra18. doi: 10.1126/scitranslmed.3007154. [DOI] [PubMed] [Google Scholar]
- 14.González MJ, Miranda-Massari JR, Mora EM, Guzmán A, Riordan NH, Riordan HD, Casciari JJ, Jackson JA, Román-Franco A. Orthomolecular oncology review: Ascorbic acid and cancer 25 years later. Integr Cancer Ther. 2005;4:32–44. doi: 10.1177/1534735404273861. [DOI] [PubMed] [Google Scholar]
- 15.Shi Y. Histone lysine demethylases: Emerging roles in development, physiology and disease. Nat Rev Genet. 2007;8:829–833. doi: 10.1038/nrg2218. [DOI] [PubMed] [Google Scholar]
- 16.Chen Q, Espey MG, Sun AY, Lee JH, Krishna MC, Shacter E, Choyke PL, Pooput C, Kirk KL, Buettner GR, Levine M. Ascorbate in pharmacologic concentrations selectively generates ascorbate radical and hydrogen peroxide in extracellular fluid in vivo. Proc Natl Acad Sci USA. 2007;104:8749–8754. doi: 10.1073/pnas.0702854104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Supabphol A, Muangman V, Chavasiri W, Supabphol R, Gritsanapan W. N-acetylcysteine inhibits proliferation, adhesion, migration and invasion of human bladder cancer cells. J Med Assoc Thai. 2009;92:1171–1177. [PubMed] [Google Scholar]
- 18.Creagan ET, Moertel CG, O'Fallon JR, Schutt AJ, O'Connell MJ, Rubin J, Frytak S. Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N Engl J Med. 1979;301:687–690. doi: 10.1056/NEJM197909273011303. [DOI] [PubMed] [Google Scholar]
- 19.Padayatty SJ, Sun H, Wang Y, Riordan HD, Hewitt SM, Katz A, Wesley RA, Levine M. Vitamin C pharmacokinetics: Implications for oral and intravenous use. Ann Intern Med. 2004;140:533–537. doi: 10.7326/0003-4819-140-7-200404060-00010. [DOI] [PubMed] [Google Scholar]
- 20.Levine M, Conry-Cantilena C, Wang Y, Welch RW, Washko PW, Dhariwal KR, Park JB, Lazarev A, Graumlich JF, King J, Cantilena LR. Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance. Proc Natl Acad Sci USA. 1996;93:3704–3709. doi: 10.1073/pnas.93.8.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffer LJ, Levine M, Assouline S, Melnychuk D, Padayatty SJ, Rosadiuk K, Rousseau C, Robitaille L, Miller WH., Jr Phase I clinical trial of i.v. ascorbic acid in advanced malignancy. Ann Oncol. 2008;19:1969–1974. doi: 10.1093/annonc/mdn377. [DOI] [PubMed] [Google Scholar]