Abstract
Central pontine myelinolysis (CPM), also known as osmotic demyelination syndrome, is a rare demyelinating disorder characterized by the loss of myelin in the center of the basis pontis. In this case report, an alcoholic patient with CPM and acquired demyelinating lesion of the basis pontis is described. The patient is a 70 year-old woman who presented with intermittent psychiatric symptoms and limb tremors following two months of alcohol abuse. During admission, magnetic resonance imaging (MRI) revealed hyperintensity on T2 weighted images and fluid-attenuated inversion-recovery imaging in the central pons without contrast enhancement. The patient's symptoms gradually improved following conservative treatment with vitamins B1 and B12. The one month follow-up MRI showed a significant reduction of the pontine injury.
Keywords: central pontine myelinolysis, chronic alcoholism, myelinolysis
Introduction
Central pontine myelinolysis (CPM), also known as osmotic demyelination syndrome (ODS), is a rare demyelinating disorder characterized by the loss of myelin in the center of the basis pontis (1). CPM was originally considered to be the result of excessively rapid correction of slowly progressive hyponatremia in patients with chronic medical conditions, such as chronic alcoholism, malnutrition and malignancy (2,3). The proposed mechanism of CPM is that neuronal demyelination begins when osmotically active substances such as sodium are depleted from the serum and free water shifts into the brain (4). However, there have been occasional reports of CPM not accompanied by hyponatremia or drastic changes in serum sodium level (2,3). The exact incidence of CPM is unknown. In a study of 3,000 brains examined postmortem, 15 cases of asymptomatic CPM were evident (5). Kleinschmidt-Demasters et al (6,7) reported that 39.4% of patients of CPM were diagnosed with alcohol poisoning, 21.5% had a history of correcting hyponatremia, and 17.4% received a liver transplantation. Although earlier reports on CPM described very poor outcome with mortality rates as high as 50% in the first 2 weeks after presentation and 90% at 6 months, recent results suggest the decreased mortality mainly due to early diagnosis and improved intensive care treatment (7). Chronic alcoholism is frequently associated with CPM, which can have a variable clinical outcome. In the present case report, a chronic alcoholic patient who suffered from CPM without hyponatremia is described. The patient eventually completely recovered.
Case report
A 70-year-old female with a history of alcohol abuse for two months presented with intermittent psychosis and involuntary tremors at the First Hospital of Jilin University (Jilin, China), in November 2014. The patient's psychiatric symptoms were characterized by auditory and visual hallucinations intermittently. The onset of the symptoms began after two months of alcohol abuse, when she began to drink a half bottle of white spirits per day. The patient denied other substance use, and her vital signs were stable. At the initial neurological examination, the patient was cooperative and her language was intact with no word-finding disorder. The patient was well oriented, her pupils were equal size (3.0 mm) and light reflexes were normal on both sides. The patient did not have extraocular movement limitations or nystagmus, and her motor strength, sensory exam and deep tendon reflexes were normal.
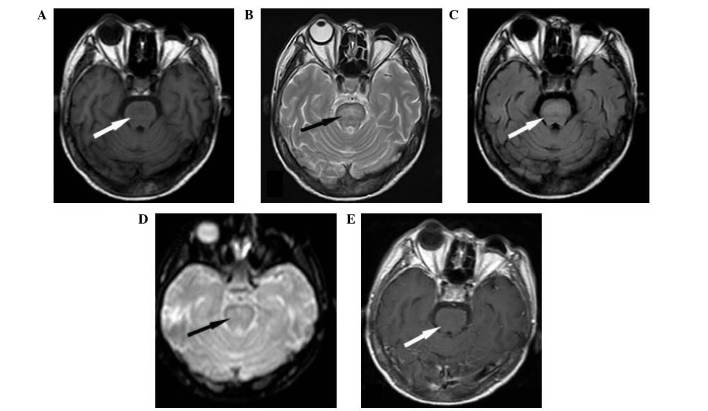
Routine laboratory data showed that the electrolytes and renal and liver function tests were within normal ranges. However, brain magnetic resonance imaging (MRI) identified a central pontine lesion, hyperintense on T2-weighted and fluid-attenuated inversion-recovery (FLAIR) imaging (Fig. 1). An increased signal on diffusion-weighted imaging (DWI) indicated abnormal restricted diffusion. The lesion was hypointense on T1-weighted and non-contrast enhanced imaging. No remarkable changes were detected in the thalamus or mammillary bodies.
Figure 1.
Central pontine myelinolysis on magnetic resonance imaging. (A) T1 weighted imaging (WI) showing a hypointense lesion in the pons in white arrow. (B) T2WI and (C) fluid-attenuated inversion-recovery-weighted imaging showing a hyperintense lesion in the pons in black or white arrow. (D) Diffusion-weighted imaging indicating abnormal restricted diffusion manifested by increased signal in black arrow. (E) T1WI without contrast enhancement in white arrow.
The patient's symptoms gradually improved after one week of supplementation with vitamin B1 (300 mg/day) and vitamin B12 (1,000 µg/day), and the intermittent mental symptoms and tremor of the limbs soon disappeared. The patient fully recovered to a normal mental and physical state, and was discharged after two weeks. The MRI at the one month follow-up visit showed a reduction in the hyperintensity and extent of the pontine lesion evident on the FLAIR and T2 weighted images. Written informed consent was obtained from the patient prior to their inclusion in the present study.
Discussion
Underlying chronic diseases may be central to the development of CPM, such as chronic alcoholism, malnutrition and liver transplantation. CPM can develop in the absence of serum sodium fluctuations, with more than one predisposing factor. Chronic alcoholism is the most common reason for developing CPM (6). However, only a small number of cases of CPM following alcohol withdrawal have been reported (8,9); the majority of the cases are associated with normonatremia (10). In the present report, the patient with chronic alcoholism developed CPM following alcohol abuse for two months. Laboratory examination revealed normal blood sodium levels.
The clinical presentation of CPM includes a range of neurological severity, between asymptomatic presentation and quadriparesis and coma, depending on the distribution of demyelination in the pontine (1,11). Symptoms typically begin with weakness, confusion and dysarthria, and may progress to pseudobulbar palsy and locked-in-syndrome. Psychotic symptoms have rarely been described in association with CPM. However, one previously reported case described an alcoholic patient who developed psychotic symptoms during alcohol withdrawal (9). This patient presented with limb tremors and intermittent mental abnormalities following heavy drinking, and was in accordance with the clinical presentation of CPM.
Diagnosis of CPM is based on a clinical neurologic examination and is confirmed by imaging studies. MRI is the primary method for diagnosis, and is superior to computed tomography (12,13). Besides hypointense T1- and hyperintense T2-weighted lesions on MRI (14), DWI can be useful in diagnosing and predicting the prognosis of ODS. The lesions identified in patients with CPM may appear between days and weeks after the onset of symptoms and may resolve completely over a period of months, and the majority of patients have a good prognosis with supportive treatment (14). In the present case report, a brain MRI of the patient confirmed the characteristic of CPM.
The prognosis of CPM is typically poor, and may result in permanent neurological sequelae or mortality (11). Currently, no effective treatment is available for CPM; however, with supportive care, spontaneous recovery is possible. In the current case report, the patient developed CPM following heavy drinking, rather than from withdrawal. Laboratory examination did not indicate the presence of hyponatremia, and the patient's symptoms were uncommon; however, MRI confirmed CPM. In conclusion, it is apparent that physicians should pay attention to the development of CPM in alcoholic patients.
References
- 1.Adams RD, Victor M, Mancall EL. Central pontine myelinolysis: A hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Arch Neurol Psychiatry. 1959;81:154–172. doi: 10.1001/archneurpsyc.1959.02340140020004. [DOI] [PubMed] [Google Scholar]
- 2.Lampl C, Yazdi K. Central pontine myelinolysis. Eur Neurol. 2002;47:3–10. doi: 10.1159/000047939. [DOI] [PubMed] [Google Scholar]
- 3.Lupato A, Fazio P, Fainardi E, Cesnik E, Casetta I, Granieri E. A case of asymptomatic pontine myelinolysis. Neurol Sci. 2001;31:361–364. doi: 10.1007/s10072-009-0215-7. [DOI] [PubMed] [Google Scholar]
- 4.Laureno R, Karp BI. Myelinolysis after correction of hyponatremia. Ann Intern Med. 1997;126:57–62. doi: 10.7326/0003-4819-126-1-199701010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Newell KL, Kleinschmidt-DeMasters BK. Central pontine myelinolysis at autopsy; a twelve year retrospective analysis. J Neurol Sci. 1996;142:134–139. doi: 10.1016/0022-510X(96)00175-X. [DOI] [PubMed] [Google Scholar]
- 6.Huang WY, Weng WC, Peng TI, Ro LS, Yang CW, Chen KH. Central pontine and extrapontine myelinolysis after rapid correction of hyponatremia by hemodialysis in a uremic patient. Ren Fail. 2007;29:635–638. doi: 10.1080/08860220701392314. [DOI] [PubMed] [Google Scholar]
- 7.Kleinschmidt-Demasters BK, Rojiani AM, Filley CM. Central and extrapontine myelinolysis: Then. and now. J Neuropathol Exp Neurol. 2006;65:1–11. doi: 10.1097/01.jnen.0000196131.72302.68. [DOI] [PubMed] [Google Scholar]
- 8.Korn-Lubetzki I, Virozub Y, Orbach H. Central pontine myelinolysis after alcohol withdrawal. Isr Med Assoc J. 2002;4:656. [PubMed] [Google Scholar]
- 9.Yoon B, Shim YS, Chung SW. Central pontine and extrapontine myelinolysis after alcohol withdrawal. Alcohol Alcohol. 2008;43:647–649. doi: 10.1093/alcalc/agn050. [DOI] [PubMed] [Google Scholar]
- 10.Martin RJ. Central pontine and extrapontine myelinolysis: The osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004;75(Suppl 3):iii22–iii28. doi: 10.1136/jnnp.2004.045906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mochizuki H, Masaki T, Miyakawa T, Nakane J, Yokoyama A, Nakamura Y, Okuyama K, Kamakura K, Motoyoshi K, Matsushita S, Higuchi S. Benign type of central pontine myelinolysis in alcoholism-clinical, neuroradiological and electrophysiological findings. J Neurol. 2003;250:1077–1083. doi: 10.1007/s00415-003-0157-6. [DOI] [PubMed] [Google Scholar]
- 12.Kwon HG, Jang SH. Motor recovery mechanism in a quadriplegic patient with locked-in syndrome. NeuroRehabilitation. 2012;30:113–117. doi: 10.3233/NRE-2012-0734. [DOI] [PubMed] [Google Scholar]
- 13.Rippe DJ, Edwards MK, D'Amour PG, Holden RW, Roos KL. MR imaging of central pontine myelinolysis. J Comput Assist Tomogr. 1987;11:724–726. doi: 10.1097/00004728-198707000-00037. [DOI] [PubMed] [Google Scholar]
- 14.Menger H, Jörg J. Outcome of central pontine and extrapontine myelinolysis (n=44) J Neurol. 1999;246:700–705. doi: 10.1007/s004150050435. [DOI] [PubMed] [Google Scholar]