Abstract
Background
The United States military considers tourniquets to be effective for controlling bleeding from major limb trauma. The purpose of this study was to assess whether tourniquets are safely applied to the appropriate civilian patient with major limb trauma of any etiology.
Methods
Following IRB approval, patients arriving to a level-1 trauma center between October 2008 and May 2013 with a prehospital (PH) or emergency department (ED) tourniquet were reviewed. Cases were assigned the following designations: absolute indication (operation within 2 hours for limb injury, vascular injury requiring repair/ligation, or traumatic amputation); relative indication (major musculoskeletal/soft-tissue injury requiring operation 2–8 hours after arrival, documented large blood loss); and non-indicated. Patients with absolute or relative indications for tourniquet placement were defined as indicated, while the remaining were designated as non-indicated. Complications potentially associated with tourniquets, including amputation, acute renal failure, compartment syndrome, nerve palsies, and venous thromboembolic events, were adjudicated by orthopedic, hand or trauma surgical staff. Univariate analysis was performed to compare patients with indicated versus non-indicated tourniquet placement.
Results
A total of 105 patients received a tourniquet for injuries sustained via sharp objects, i.e., glass or knives (32%), motor vehicle collisions (30%), or other mechanisms (38%). A total of 94 patients (90%) had indicated tourniquet placement; 41 (44%) of which had a vascular injury. Demographics, mechanism, transport, and vitals were similar between patients that had indicated or non-indicated tourniquet placement. 48% of the indicated tourniquets placed PH were removed in the ED, compared to 100% of the non-indicated tourniquets (p < 0.01). The amputation rate was 32% among patients with indicated tourniquet placement (vs. 0%; p = 0.03). Acute renal failure (3.2 vs. 0%, p = 0.72), compartment syndrome (2.1 vs. 0%, p = 0.80), nerve palsies (5.3 vs. 0%; p = 0.57), and venous thromboembolic events (9.1 vs. 8.5%; p = 0.65) and were similar in patients that had indicated compared to non-indicated tourniquet placement. After adjudication, no complication was a result of tourniquet use.
Conclusion
The current study suggests that PH and ED tourniquets are used safely and appropriately in civilians with major limb trauma that occur via blunt and penetrating mechanisms.
Keywords: Tourniquet, extremity hemorrhage, civilian, trauma, safety
Introduction
Trauma is the leading cause of death in individuals 46 and younger.1 The majority of potentially preventable deaths from civilian trauma are a result of hemorrhage; a third of these fatal hemorrhages occur in the extremity.2 The Committee on Tactical Combat Casualty Care (TCCC) first recommended tourniquet use for control of bleeding from major limb trauma, and subsequent studies following this implementation have demonstrated an associated improvement in survival with a low incidence of complications in the military setting.3–5 Following the model developed by TCCC, The Civilian Tactical Emergency Casualty Care (TECC) guidelines advocate for the use of tourniquets by medical and non-medical first responders (police officers), as it recognizes that non-medical first responders and bystanders are often the nearest to casualty, especially in the case of hostile incidents.4, 6–8
The National Association of Emergency Medical Technicians (NAEMT) has developed several different courses, some in conjunction with the American College of Surgeons Committee on Trauma (ACS-COT), to teach the use of tourniquet application in civilians to basic life support providers, law enforcement officers and lay persons. The use of tourniquets in the civilian population has been met with controversy, however, as some argue that their use is not warranted or necessary due different patterns of injury sustained by civilians, the shortened transport times of mature trauma systems and the capability of prehospital providers to dedicate effort to manual compression.9–12
As a result, the authorities that address civilian use of tourniquets range from not recommending use,13 not addressing prehospital use,14–15 recommending use only in specific injuries (i.e., penetrating lower extremity),15 addressing use only in tactical or hostile scenarios,16–18 or recommending the judicious use by medical and nonmedical first responders for control of bleeding from a limb.16, 19 As a consequence, there is no clear and uniform recommendation for tourniquet application for upper or lower limb bleeding (regardless of mechanism) in either the prehospital (PH) or emergency department (ED) in civilians.
The purpose of this study was to examine the injuries resulting in major limb trauma sustained by civilians. We hypothesized that appropriately trained PH and in-hospital civilian personnel could safely and appropriately apply tourniquets in patients with major limb trauma from common mechanisms of injury sustained by civilians, including motor vehicle collisions, single stab wounds and gunshot wounds.
Methods
Study Setting
The University of Texas Health Science Center at Houston and the Memorial Hermann Hospital Institutional Review Boards approved this study. The Texas Trauma Institute at Memorial Hermann Hospital is an American College of Surgeons-accredited Level I trauma center that is the primary teaching hospital for the University of Texas Health Science Center at Houston. Memorial Hermann is one of only two Level 1 trauma centers in Houston, Texas, the fourth largest city in the United States. The hospital is an 800+ bed facility within the Texas Medical Center and is also home to the John S. Dunn Helistop, the busiest heliport for its size in the United States. The trauma center admits more than 6,000 trauma patients annually with the most severely injured cared for in the 23-bed shock trauma intensive care unit.
Selection of Participants
This was a single-center, retrospective cohort study of patients arriving Memorial Hermann Hospital with a trauma activation, identified using the institution’s Trauma Registry of the American College of Surgeons database. All patients admitted between October 2008 and May 2013 with a tourniquet listed as a treatment were included in the study. Patients were excluded from the study if no documentation of tourniquet placement could be corroborated on review of prehospital and hospital medical records. All tourniquets were official-issued Combat Application Tourniquets (CAT, Composite Resources, Rock Hill, SC), a type of windlass tourniquet. CATs were distributed first to the aeromedical flight nurses in 2008, and then ground Emergency Medical Services in 2011. Formal education for tourniquet application was conducted for all aeromedical flight nurses and basic life support providers in a peer to peer fashion, under the supervision of the Emergency Medical Services (EMS) Director. The aeromedical and county EMS services purchase these CATs independently.
Definitions
Tourniquet placement was designated as indicated if an absolute or relative indication could be identified via review of patient hospital record. For the purpose of this study, absolute and relative indications were defined a priori. An absolute indication included a traumatic amputation, an emergent or urgent operation for limb injury within two hours of hospital arrival, or a vascular injury requiring repair or ligation. A relative indication included a documented significant blood loss at the scene or a major musculoskeletal/soft tissue injury requiring a non-emergent or urgent operation (between 2 and 8 hours of hospital arrival). The tourniquet was designated as non-indicated if there was no absolute or relative indication identified.
Outcomes
Patients were evaluated by indicated or non-indicated tourniquet placement. The primary outcome evaluated was the presence of a complication potentially due to the tourniquet, including amputation, acute renal failure, compartment syndrome, nerve palsy, or venous thromboembolism (VTE). Secondary outcomes included removal, replacement or addition of a tourniquet in the ED, operative procedures including amputation, revascularization, vascular ligation, exploration/fixation of the extremity and fasciotomy, mortality and resuscitation. These outcomes were determined by a combination of Trauma Registry data and electronic health record review. Patient demographics, injury mechanism, Injury Severity Score (ISS), Abbreviated Injury Scale (AIS) Scores, length of hospital stay (days), intensive care unit stay (days), prehospital (PH) and Emergency Department (ED) vital signs (systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), Glasgow Coma Score (GCS), shock index (SI, defined as the ratio of SBP to HR) and temperature), admission labs (hemoglobin, hematocrit, lactate, base deficit, platelet count, international normalized ratio, pH, bicarbonate), total volume of crystalloid administered, total units of blood transfused, and mortality were determined from the Trauma Registry. Trauma Registry staff calculated ISS and AIS after discharge or death of each patient. To account for evolving transfusion practices and a trend towards less crystalloid/increased blood product administration for resuscitation of hemorrhagic shock at our institution during the study period, a Resuscitation Intensity was calculated as previously described by Rahbar and colleagues20 with the sum of all fluid given with the ratio of 1 unit of resuscitation = 1000 mL crystalloid = 500 mL colloid = 1 unit of red blood cells (RBC), plasma or platelets. The PH or ED application of a tourniquet and associated injuries were extracted from the prehospital and in-hospital electronic health record. As our electronic health record does not collect tourniquet time in a standard fashion, transport time was used as a surrogate for tourniquet time and was calculated as the difference from scene arrival to hospital arrival time. Type of vascular injury, need for revascularization, need and reason for amputation, need for fasciotomy, and need for emergent/urgent musculoskeletal stabilization were confirmed on review of operative reports. Rate of complications, including amputation due to tourniquet use, acute renal failure, compartment syndrome, nerve palsy, and VTE, were extracted from the trauma registry and adjudicated by orthopedic, hand or trauma or surgical faculty via operative reports. Nerve palsies were only considered in the absence of an identified transected nerve as identified by the Trauma Registry. To account for the role of tourniquet application contributing to complications in patients in the extremes of age, a subgroup analysis was conducted comparing patients aged 18–49 years to those outside of that range.
Statistical Analysis
Continuous data are presented as medians and interquartile range (IQR). Comparisons between groups are performed using the Wilcoxon rank-sum (Mann-Whitney U test). Categorical data are reported as proportions and, where appropriate, tested for significance using Chi-square or Fisher’s exact tests. STATA Statistical software (version 13.1, College Station, TX) was used for the analysis.
Results
Between October 2008 and May 2013, 107 patients arrived as a trauma activation and were identified by the Trauma Registry as having a tourniquet placed either PH, in the ED, or in both settings. After review of patient records, documentation of tourniquet placement could not be identified for two patients and they were excluded from the study, leaving 105 patients for analysis.
Tourniquet Use
One hundred and twenty one tourniquets were applied to 54 upper and 52 lower limbs. All of the patients had a CAT placed, however, 2 patients also had an improvised tourniquet placed by bystanders in the field prior to CAT placement. One of these patients had a CAT placed by PH providers and additionally in the ED while the other had a CAT placed after arrival to the ED. The median number of tourniquets per patient was 1 (1, 1), which was similar whether they were placed PH or in the ED (p = 0.16).
Indication for Tourniquet Placement
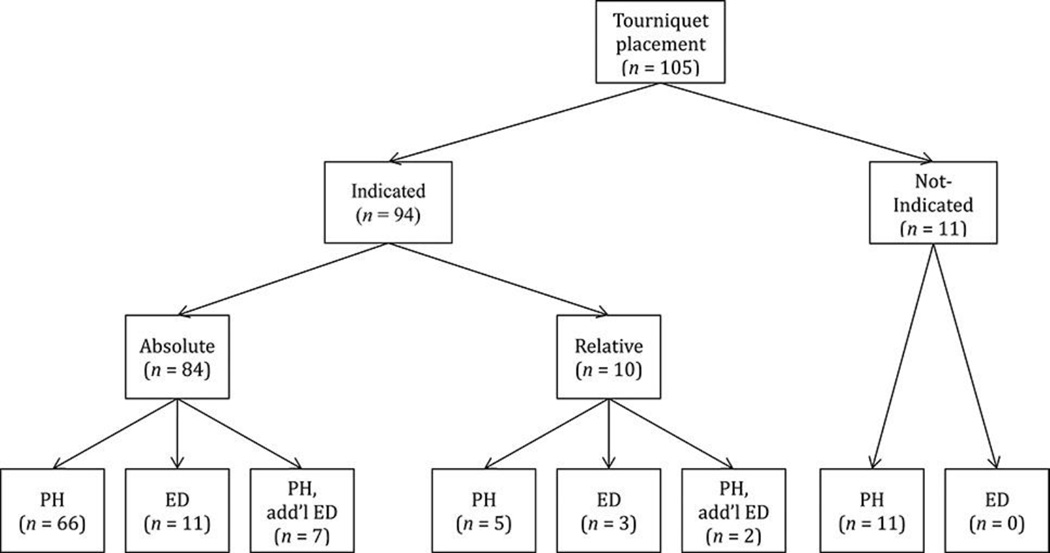
Of the 105 patients that received tourniquets, 82 (78%) patients had tourniquets placed PH, 14 (13%) patients had a de novo tourniquet placed in the ED, and 9 (9%) patients had a tourniquet placed PH and then an additional tourniquet placed after arriving to the ED. Ninety-four (90%) patients met the definition for indicated tourniquet placement. Of these 94 with indicated tourniquet placement, 84 (89%) had an absolute indication for tourniquet placement and 10 (11%) had a relative indication for tourniquet placement. Eleven (10%) patients were found to have a non-indicated tourniquet placement. The distribution of PH or ED indicated or non-indicated tourniquet placement is displayed in Figure 1. There were zero non-indicated tourniquets placed in the ED.
Figure 1.
Distribution of patients and location of indicated or not-indicated tourniquet placement. PH = prehospital; ED = emergency department; PH add’l ED = PH tourniquet applied, additional tourniquet applied in ED.
Mechanism of Injury
Blunt and penetrating injuries were equal in the population (49.5% each mechanism) and this distribution remained similar despite indicated or non-indicated tourniquet placement (p = 0.53) (Table 1). One patient arrived as a trauma activation, however was found to have bleeding from a disrupted arteriovenous fistula. Table 1 additionally shows the type of blunt and penetrating injuries sustained by this patient population and their equal distribution between indicated or non-indicated tourniquet placements. Motor vehicle collisions were the most common source of blunt injuries associated with tourniquet placement, irrespective of whether it was indicated (30%) or non-indicated (36%, p = 1.0). Lacerations sustained via stab wounds, broken glass or other sharp objects (35% vs. 9%, p = 0.10) and gunshot wounds (6% vs. 27%, p = 0.07) were the predominant penetrating injuries associated with indicated or non-indicated tourniquet placement.
Table 1.
Mechanism of injury in patients that had by Indicated or Non-indicated tourniquet placement
| Indicated | Non-indicated | All patients | ||
|---|---|---|---|---|
| (n = 94) | (n = 11) | (n = 105) | P value | |
| Blunt | 45 (48%) | 7 (64%) | 5 (49.5%) | 0.53 |
| MVC/MCC | 28 (30%) | 4 (36%) | 32 (30%) | 1.00 |
| Crush | 5 (5%) | 1 (9%) | 6 (6%) | 0.53 |
| Auto pedestrian | 3 (3%) | 1 (9%) | 4 (4%) | 0.39 |
| Water Vehicle | 3 (3%) | 0 | 3 (3%) | 1.00 |
| Explosion | 1 (1%) | 0 | 1 (1%) | 1.00 |
| Industrial | 5 (5%) | 1 (9%) | 6 (6%) | 0.53 |
| Penetrating | 48 (51%) | 4 (36%) | 52 (49.5%) | 0.53 |
| GSW | 6 (6%) | 3 (27%) | 9 (9%) | 0.07 |
| Stab/Plate Glass/Sharp Object | 33 (35%) | 1 (9%) | 34 (32%) | 0.10 |
| Saw | 8 (9%) | 0 | 8 (8%) | 0.60 |
| Animal Bite | 1(1%) | 0 | 1 (1%) | 1.00 |
| Othera | 1(1%) | 0 | 1 (1%) | 1.00 |
Note. MVC = motor vehicle collision; MCC = motorcycle collision; GSW = gunshot wound. Values are expressed as n (precentage).
disruption of arteriovenous graft
Injuries Associated with Tourniquet Placement
Injuries associated with tourniquet placement included limb laceration (40%), traumatic amputation (29%), open fracture (16%), mangled/multiply-injured limb (9%), gunshot wounds (3%), soft tissue defect (2%), and arteriovenous fistula blowout (1%). With the exception of traumatic amputations, as it was one of the indications for tourniquet placement, there were no differences in the distribution of injuries associated with indicated or non-indicated tourniquet placement (p = 0.27).
Patient and Injury Demographics/Physiology
Patients that had a tourniquet placed were a median age of 34 years (25, 46) years, 88% were male, 64% were transported by air with a median ISS of 9 (4, 16), AIS of the extremity of 3 (2, 3), and LOS of 7 days (2, 16) days and ICU stay of 1 (0, 5) days. A total of 17% of patients had a severe injury (AIS ≥ 3) to another body region (head, face/neck, chest, abdomen, or external surface). These demographic values were similar for indicated and non-indicated tourniquet placement (Table 2). Transport time, available for 80 of the 105 patients, occupied 31 (23, 39) minutes and was similar in patients that had indicated or non-indicated tourniquet placement (p = 0.47). Transport time was available for similar proportions of patients with indicated or non-indicated tourniquet placement (76% vs. 82%, p = 0.49).
Table 2.
Demographic, prehospital, and physiologic parameters in patients with Indicated versus Non-indicated tourniquet placement
| Indicated (n = 94) | Non-indicated (n = 11) | All patients (n = 105) | P value | |
|---|---|---|---|---|
| Age, years | 34 (26, 46) | 35 (19, 57) | 34 (25, 46) | 0.88 |
| Age <18, ≥50 years (%) | 18 | 36 | 20 | 0.22 |
| Gender (%) | 87 | 91 | 88 | 0.64 |
| BMI kg/m2 | 27 (24, 30) | 29 (27, 33) | 27 (24, 30) | 0.11 |
| ISS | 9 (4, 16) | 5 (4, 9) | 9 (4, 16) | 0.33 |
| AIS Extremity | 3 (2, 3) | 2 (1, 3) | 3 (2, 3) | 0.32 |
| AIS not-Extremity ≥3 (%) | 17 | 18 | 17 | 1.00 |
| PH Vital Signs | ||||
| SBP, mmHg | 110 (91, 134) | 110 (101, 126) | 110 (91, 132) | 0.95 |
| HR, bpm | 96 (80, 120) | 85 (68, 104) | 96 (80, 114) | 0.15 |
| GCS | 15 (14, 15) | 15 (15, 15) | 15 (14, 15) | 0.31 |
| Shock Index | 0.85 (0.68, 1.2) | 0.72 (0.64, 0.83) | 0.82 (0.65, 1.2) | 0.22 |
| ED Vital Signs | ||||
| SBP, mmHg | 124 (99, 146) | 116 (101, 155) | 124 (99, 147) | 0.90 |
| Ä SBP, mmHg | 24.5 (0, 118) | 80 (−8, 155) | 27 (−3, 121) | 0.68 |
| HR, bpm | 97 (82, 113) | 99 (69, 107) | 98 (82, 112) | 0.37 |
| GCS | 15 (13, 15) | 15 (15, 15) | 15 (13, 15) | 0.28 |
| Shock Index | 0.8 (0.6, 1.1) | 0.8 (0.6, 0.9) | 0.8 (0.6, 1.1) | 0.53 |
| Labs on Admission | ||||
| pH | 7.31 (7.23, 7.34) | 7.32 (7.27, 7.32) | 7.31 (7.23, 7.34) | 0.98 |
| Base Deficit, mEq/L | 4 (2, 8) | 4 (3, 5) | 4 (2, 8) | 0.73 |
| Lactate, mg/dL | 2.1 (0, 3.4) | 2.3 (2.2, 2.3) | 2.2 (0, 3.4) | 0.89 |
| Hemoglobin, mg/dL | 12.9 (10.4, 14.1) | 12.7 (11.7, 13.2) | 12.9 (10.6, 14.1) | 0.72 |
| Platelet count (x109/L) | 215 (162, 269) | 268 (159, 315) | 219 (162, 270) | 0.27 |
| INR | 1.1 (1.03, 1.32) | 1.09 (0.97, 1.20) | 1.10 (1.02, 1.3) | 0.41 |
| PT | 14 (13.4, 15.3) | 13.7 (13.0, 14.2) | 14.0 (13.2, 15.1) | 0.39 |
| PTT | 26.5 (23.4, 31.3) | 25.4 (24.1, 27.1) | 25.9 (23.6, 30.9) | 0.70 |
| Transport time (minutes) | 21 (23, 39) | 27 (23, 35) | 21 (23, 39) | 0.48 |
Note. 11 SBP defined as change in SBP from PH to ED. Transport time calculated as (hospital arrival–scene arrival). Values are expressed as median with 25th, 75th percentiles, or percentages. ISS = Injury Severity Score; AIS = Abbreviated Injury Score; PH = prehospital; ED = emergency department; SBP = systolic blood pressure; HR = heart rate; GCS = Glasgow Coma Score.
These patients presented with a median SBP of 125 (99, 147) mmHg, HR of 98 (82, 112) bpm, shock index of 0.76 (0.6, 1.06), pH of 7.31 (7.23, 7.34), and base deficit of 4 (2, 8). There were no clinically relevant differences in PH or ED vital signs or labs on admission between patient that had an indicated and non-indicated tourniquet placement (Table 2).
Vascular Injuries
Of the 94 patients that had an indicated tourniquet placement, 41 (44%) had a vascular injury; by definitions created a priori, all of these patients had an absolute indication for tourniquet placement. There were more isolated arterial injuries compared to isolated venous or combined arterial and venous injuries (68% vs. 7% vs. 24%, p = 0.03). The radial artery was most the most commonly injured structure, irrespective of mechanism (27% overall, 14% blunt, 29% penetrating, p = 0.65). The distribution of injuries to specific named structures is outlined in Table 3. Patients with a blunt mechanism of injury sustained less vascular injuries overall (13% compared to 65%, p < 0.001). Patients that had a non-indicated tourniquet placement did not have a vascular injury.
Table 3.
Site of vascular injury in patients with Absolute Indication for tourniquet placement
| Anatomic Site of | All patients with vascular injury |
Blunt | Penetrating | |
|---|---|---|---|---|
| Injury | (n = 41) | (n = 7) | (n = 34) | p value |
| Brachial Artery | 4 (10%) | 0 | 4 (12%) | 1.00 |
| Brachial Artery and Vein | 3 (7%) | 0 | 3 (9%) | 1.00 |
| Cephalic/Basilic Vein | 3 (7%) | 1 (14%) | 2 (6%) | 0.44 |
| Digital Artery | 1 (2%) | 0 | 1 (3%) | 1.00 |
| Femoral Artery | 3 (7%) | 1 (14%) | 2 (6%) | 0.44 |
| Femoral Artery and Vein | 4 (10%) | 1 (14%) | 3 (9%) | 0.54 |
| Multiple Upper Extremity Combineda |
3 (7%) | 0 | 3 (9%) | 1.00 |
| Peroneal Artery | 1 (2%) | 1 (14%) | 0 | 0.17 |
| Radial Artery | 6 (15%) | 1 (14%) | 5 (15%) | 1.00 |
| Radial and Ulnar Artery | 5 (12%) | 0 | 5 (15%) | 0.57 |
| Tibial Artery | 4 (10%) | 1 (14%) | 3 (9%) | 0.54 |
| Ulnar Artery | 4 (10%) | 1 (14%) | 3 (9%) | 0.54 |
Multiple upper extremity combined includes patients that had a combination of injuries to the cephalic or basilic vein and brachial artery (n = 1), ulnar artery (n = 1), or both (n = 1). Values are expressed as n (proportion).
Primary Outcome
The majority (82%) of patients did not have a complication potentially associated with the use of a tourniquet, including amputation, acute renal failure, compartment syndrome, nerve palsy, or VTE (Table 4). Of the 105 patients with a tourniquet, 30 patients (29%) underwent amputations. The reasons for amputation included traumatic amputation (n = 14), a non-salvageable limb (n = 14), and completion of a partial amputation (n = 2). Tourniquets placed for the a priori indication of amputation were not considered a complication unless judged by the adjudicating panel. As such, there were no amputations due to indicated tourniquet placement, and there were no amputations in patients with non-indicated tourniquet placement.
Table 4.
Potential complications by Indicated or Non-indicated tourniquet placement
| Indicated | Non-indicated | All patients | ||
|---|---|---|---|---|
| (n = 94) | (n = 11) | (n = 105) | P value | |
| Total Complications | 18 (19.1%) | 1 (9.1%) | 19 (18%) | 0.68 |
| Amputationa | 0 | 0 | 0 | 1.00 |
| Acute Renal Failure | 3 (3.2%) | 0 | 3 (2.9%) | 0.72 |
| Compartment Syndrome |
2 (2.1%) | 0 | 2 (1.9%) | 0.80 |
| Nerve Palsy | 5 (5.3%) | 0 | 5 (4.8%) | 0.57 |
| VTE | 8 (8.5%) | 1 (9.1%) | 9 (8.6%) | 0.65 |
| None | 76 (81%) | 10 (91%) | 86 (82%) | 0.68 |
Note.
Traumatic amputation was included in the a priori definition of indicated tourniquet placement. Values are expressed as n (percentage). VTE = venous thromboembolism.
In the 94 patients that had an indicated tourniquet placement, 3 (3.2%) developed acute renal failure, 2 (2.1%) developed compartment syndrome, 5 (5.3%) had nerve palsies, and 8 (8.5%) had VTEs. The only potential complication that occurred in patients with a non-indicated tourniquet placement was a VTE (pulmonary embolism, n = 1).
Acute Renal Failure
Three patients developed acute renal failure during their hospitalization. No cases of renal failure were from rhabdomyolysis. There were no cases of acute renal failure in patients with non-indicated tourniquet placement.
Compartment Syndrome
Two patients with indicated tourniquet placement developed compartment syndrome. One was a 31-year-old male that transected the brachial artery after punching his right arm through a window. He went into cardiac arrest and underwent subsequent ACLS with return of spontaneous circulation and tourniquet placement at an outside facility. He was transferred to our center four hours after injury. While the tourniquet could have contributed to the development of compartment syndrome, it is more likely that this was due to cardiac arrest from exsanguination, delay in transfer and restoration of vascular flow to the distal limb than tourniquet use. The other patient was a 51-year-old male who sustained a degloving injury to his right arm distal to the elbow from a motor vehicle accident. A tourniquet was placed PH and was removed upon evaluation in the ED, which revealed an arm that was neurovascularly intact with radius and ulna fractures and soft compartments. His arm was splinted and when it was re-evaluated prior to operative fixation of the fractures six hours later, the volar compartment was noted to be tight with Stryker pressures exceeding 90 mmHg in the mobile wad. In this case, all clinicians involved in his care felt the splint application resulted in the development of compartment syndrome rather than the tourniquet. There were no cases of compartment syndrome in patients with non-indicated tourniquet placement.
Nerve Palsy
All five nerve palsies occurred in patients with indicated tourniquet placement. All nerve palsies were attributed to the injury itself and not tourniquet placement. Four of the patients sustained open fractures and/or mangled lower limbs that ultimately required a formal amputation. One patient was injured with a chainsaw to his left arm; he presented with decreased wrist extension that was secondary to pain from muscular damage from the traumatic injury. There were no cases of nerve palsies in patients with non-indicated tourniquet placement.
Venous Thromboembolism
Nine patients developed a VTE during their hospitalization. Only one developed a deep venous thrombosis in the same limb that was injured, and this patient had a traumatic amputation of that limb.
The rate of VTE between patients with indicated and non-indicated tourniquet placement was similar. Of the 11 patients with non-indicated tourniquet placement, 1 patient had a pulmonary embolism without evidence of a deep venous thrombosis in the injured limb.
As displayed in Table 4, the distribution of all complications potentially associated indicated or non-indicated tourniquet placement was similar.
Complications in Extremes of Age
Twenty-one patients (20%) were either younger than 18 or older than 49, and this age distribution was the same between indicated or non-indicated tourniquet placement (p = 0.22; Table 2). As observed in the overall cohort, no amputations were deemed by the adjudicating panel to be due to tourniquet use, but the rate of amputation (29% vs. 29%, p = 1.0) was equally distributed between the two age groups. The rates of compartment syndrome (2.4 vs. 0.0%, p = 0.64), nerve palsies (4.8 vs. 4.8%, p = 0.68), and VTE (9.5 vs. 4.8%, p = 0.43) were similar in patients 18–49 compared to those outside of that range. There was a trend for a lower rate of acute renal failure in those 18–49 years of age (1.2 vs. 9.5%, p = 0.10). No patients with a non-indicated tourniquet placement that were younger than 18 or older than 49 had a complication potentially associated with tourniquet placement. The rates of potential complications between patients with an indicated (n = 17) versus non-indicated (n = 4) tourniquet placement were similar in this age range (compartment syndrome: 0% vs. 0%; nerve palsy 5.8% vs. 0%, p = 0.81; VTE: 5.8% vs. 0%, p = 0.81; renal failure 12% vs. 0%, p = 0.65).
Secondary Outcomes
Removal/replacement of tourniquets in the ED
Twenty-three patients had tourniquets placed in the ED; all were indicated. Fourteen patients had an original tourniquet placed in the ED; the remaining 9 had an additional tourniquet placed after arrival to the ED. The predominant reason for requiring an additional tourniquet was failure of the PH tourniquet to adequately control bleeding (4 out of 9 patients, 44%), followed by replacement of improvised tourniquet (22%). The remainder additional ED tourniquets (n = 3) were placed for reasons not obvious in the patient’s medical record, despite the indicated PH placement. The 11 non-indicated patients all had their tourniquets placed PH and all were removed upon arrival to the ED; none were replaced. A total of 48% of indicated tourniquets placed PH were removed in the ED, compared to 100% of the non-indicated tourniquets (p < 0.01).
Operative Procedures
Eighty-nine of the 105 patients (71%) underwent at least one operative procedure for their limb injury, with a total of 187 limb operations performed in the 105 patients. The operative procedures were for exploration/fixation of the limb (54%), direct vascular repair (34%), amputation (29%), vascular ligation (16%), fasciotomy (15%), and interposition graft or shunt (10%).
Patients that had a procedure for revascularization, amputation, or vascular ligation all had indicated tourniquet placement. A total of 46 patients underwent procedures for revascularization, either by direct vascular repair, interposition graft or shunt placement. Subsequently, none of these patients later underwent a limb amputation because of a failure of the revascularization procedure. Thirty patients (29%) underwent amputations. The reasons for amputation included traumatic amputation (n = 14), a non-salvageable limb (n = 14), and completion of a partial amputation (n = 2). There were no amputations as a result of a complication from tourniquet placement.
The rates of operative limb exploration/fixation (62% vs, 86%, p = 0.41) and fasciotomy (18% vs. 14%, p = 1.0) were similar in patients that had an indicated or non-indicated tourniquet placement. Fasciotomies were performed predominantly for prophylactic reasons and not for the treatment of compartment syndrome, as only 2 patients developed compartment syndrome.
Mortality
Seven out of the 105 patients (14%) succumbed to their injuries. One patient was dead upon arrival after he was found down in a parking lot with a single gunshot wound to the left thigh. Two patients with traumatic amputations died in the ED. One had tourniquet placed to the bilateral lower limbs PH and another had both upper and lower limb tourniquets placed in the ED after losing pulses. The remaining four patients died in-hospital with a median LOS of 1.5 (0.75–22) days.
There was no difference in mortality between patients that had indicated compared to non-indicated tourniquet placement (6% vs. 9%, p = 0.75).
Resuscitation
All patients received a total of 1.4 (0, 3.5) liters of crystalloid, 2 (0, 6) units of red blood cells (RBCs), and 3 (0, 10) units of plasma. As displayed in Table 5, patients that had indicated tourniquet placement received more units of RBCs and fresh plasma in the first 24 hours compared with those with non-indicated tourniquet placement [RBCs: 3 (0, 7) vs. 0 (0, 0), p = 0.02; plasma: (4 (0, 12) vs. 0 (0, 3), p = 0.01]. There were no differences in crystalloid administration. However, patients with indicated tourniquet placement had a higher ED and 24-hour Resuscitation Intensity than those in with non-indicated tourniquet placement [ED: 2 (0, 4) vs. 0 (0, 1), p = 0.01; 24-hour (5 (1, 14) vs. 1 (0, 4), p = 0.05].
Table 5.
Resuscitation by Indicated or Non-indicated tourniquet placement
| Indicated | Non-indicated | All patients | ||
|---|---|---|---|---|
| (n = 94) | (n = 11) | (n = 105) | P value | |
| Blood Transfusion (units) | ||||
| 24-hour RBC | 3 (0, 7) | 0 (0, 0) | 2 (0, 6) | 0.02 |
| 24-hour plasma | 4 (0, 12) | 0 (0, 0) | 3 (0, 10) | 0.01 |
| 24-hour platelet | 0 (0, 2) | 0 (0, 0) | 0 (0, 1.5) | 0.05 |
| Crystalloid (liters) | ||||
| Prehospital | 0 (0, 0.6) | 0.1 (0, 0.3) | 0 (0, 0.6) | 0.71 |
| Emergency Department | 0 (0, 1.0) | 0 (0, 1.0) | 0 (0, 1.0) | 0.88 |
| Operating Room | 0.5 (0, 2.0) | 1.3 (0, 2.4) | 0.6 (0, 2.0) | 0.57 |
| 24-hour | 1.4 (0, 3.5) | 1.1 (0, 4.0) | 1.4 (0, 3.5) | 0.79 |
| Resuscitation Intensity | ||||
| Prehospital | 0.6 (0, 3.5) | 0 (0, 0.3) | 0.4 (0, 3.0) | 0.08 |
| Emergency Department | 2.0 (0, 4.0) | 0 (0, 1.0) | 2.0 (0, 4.0) | 0.01 |
| Operating Room | 0.8 (0, 8.3) | 0.8 (0, 3.0) | 0.8 (0, 7.0) | 0.60 |
| 24-hour | 4.5 (1.0, 14.0) | 1.1 (0, 4.1) | 4.1 (1.0, 11.8) | 0.04 |
Note. Resuscitation intensity calculated as previously demonstrated by Rahbar et al.20 Values are expressed as median with 25th or 75th percentiles. RBC = red blood cells; PH = prehospital; ED = emergency department; OR = operating room.
Discussion
The purpose of this study was to demonstrate that tourniquets could be used safely and appropriately in civilians who sustain traumatic major limb trauma by any mechanism. For the evaluation of safety, we used the rate of potential tourniquet-associated complications and judged the contribution of the tourniquet to the development of these complications. For the evaluation of appropriateness, we used a priori definitions of absolute or relative indications and applied them to this retrospective study. We have described the use of tourniquets in 105 civilians with predominately isolated major limb trauma with a potential complication rate of 18% and, following adjudication, a 0% complication rate attributed to the use of a tourniquet (regardless of indicated or non-indicated placement). A total of 90% of the tourniquets were indicated. However, it is reasonable to assume that all of the tourniquets were applied with the intent to control hemorrhage, so deeming the 11 non-indicated tourniquets as “inappropriate” is difficult to judge in this retrospective study. In addition, the predominant injuries associated with tourniquet application in patients that had a non-indicated placement were lacerations (23%) and open fractures (31%), which can bleed considerably from the soft tissue, even in the absence of a vascular injury. Previous studies have demonstrated that the placement of a tourniquet is based on the appearance of a wound21and have theorized that its use serves as a “threat-to-life” indicator.22 The patients with indicated tourniquet placement did require more resuscitation (either by transfusion of blood products or resuscitation intensity), consistent with the a priori definitions of indicated, which included a vascular injury.
Several studies in the military setting have demonstrated that tourniquets are effective for hemorrhage control,5, 23 improve survival overall,3 especially when applied before the onset of shock,4 can achieve survival rates similar to those without a tourniquet despite arriving with worse indices of shock (base deficit, hemoglobin, pulse rate, ISS, transfusion units),22 and that PH personnel can apply tourniquets without significant adverse effects.21 However, the use in civilian trauma, while increasing since 2008, is not uniform. A 2014 survey of 151 prehospital care providers in the Midwestern United States revealed that only 25 had previously used a tourniquet, with the majority not understanding the mechanics of tourniquet application (91%), the harm of venous occlusion without arterial occlusion (69%), and 37% did not know the correct location of application.24 Additionally, the majority respondents from a 2015 survey of Trauma Medical Directors at predominately American College of Surgeons-verified trauma centers indicated less than 20% of patients who could have benefited from a tourniquet arrived with one in place. A total of 49% of these respondents cited the lack of concomitant civilian research as a barrier to translation from military to civilian use.25
In the current state, guidelines regarding tourniquet use for civilian major limb trauma are conflicting and accompanied with caveats. The 2011 Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage does not recommend the use of tourniquets due to the paucity of evidence in civilian population, the variance of use amongst EMS systems and the possibility for overuse.13 Advanced Trauma Life Support (ATLS) guidelines support the use of a tourniquet when direct pressure fails to control arterial limb hemorrhage, however, only in the context that an intentional possible choice of life over limb has been made.14 This language suggests that many still believe that tourniquet use equals amputation. Our study conversely displayed 30 patients with amputations, all of which were a direct consequence of the injury and none were a complication of tourniquet use. This is consistent with evaluation of the National Trauma Databank, which displayed amputation was more common with blunt, distal vascular injuries.26 In addition, as ATLS is intended for physician providers that are normally located within a hospital, there is no actual recommendation by ATLS with regards to PH application of tourniquets. The Eastern Association for the Association of Trauma (EAST) guidelines are often cited as an entity recommending the use of tourniquets in the civilian population, however it should be emphasized that these guidelines refer to individuals with penetrating arterial injuries to the leg not controlled via manual compression or a compression dressing.15 Our population was approximately 50% blunt, with 56 arm injuries to 25 arterial structures. The most commonly injured vascular structure in the limbs was the radial artery, which has been previously reported and is not unique to this patient population.27
Therefore, while the EAST guidelines do not apply to the majority of the population that we have presented, these patients still had an indication for tourniquet placement. In addition, an analysis of the National Trauma Databank has demonstrated a higher association of blunt (not penetrating) injury with lower limb arterial injury, which had a higher rate of mortality and amputation.28
Following recent terrorist and mass-casualty events in Aurora, CO; Tucson, AZ; Boston, MA; Newtown, CT; and other areas, The Hartford Consensus presented a call to action that no one should die from uncontrolled bleeding.29 The recommendations formed from these meetings advocate for providing all EMS, fire, police, and concerned citizens with individual first aid kits. These kits, which include a hemostatic dressing, tourniquet, and gloves, are recommended to be placed in public places and be as readily available as automated external defibrillators. However, as these recommendation statements were formed initially in response to active shooter and mass casualty events, there is a resounding implication that tourniquets should be applied to civilians in tactical or hazard situations where the scene cannot be secured for EMS to enter or dedication to direct pressure is not safe. The most recent Hartford Consensus IV, released in March 2016, now includes the use of tourniquets for hemorrhage control from any etiology, including motor vehicle collisions. Additionally, an evaluation of limb exsanguination control protocols in the United States revealed that 84% of states had a protocol in place, but only 36% include specific guidance with respect to type, indication, technique and safety.30 Therefore, it is evident this recommendation is still developing.
The NAEMT, which provides education for medical and nonmedical first responders via Prehospital Trauma Life Support (PHTLS), Law Enforcement and First Response Tactical Casualty Care (LEFR-TCC), Bleeding Control for the Injured (BCon), and TECC, does teach the use of tourniquets in the prehospital setting. Each of these courses has a different intended audience and scene. PHTLS is intended for EMS practitioners caring for patients that sustain traumatic injury by any mechanism, and teaches tourniquet placement when direct pressure fails to control bleeding.31 LEFR-TCC, intended specifically for public safety first responders responding to tactical scenarios, teaches early tourniquet application for life-threatening limb bleeding.16 BCon (formed out of collaboration between NAEMT and ACS-COT), created for non-tactical lay bystanders (i.e., law enforcement officers, security personnel, teachers, civilians) responding to any traumatic incident, similarly teaches early tourniquet application for major limb trauma in an abbreviated (2–3 hour) course.16 Finally, TECC, which promotes a chain of survival similar to TCCC, is intended for all-hazard (tactical, active shooter, mass casualty) scenarios.6, 8 The TECC advocates for tourniquet use for all (including pediatric) major limb trauma by medical and nonmedical first responders, recognizing that in hostile situations, first responders may not be able to access the wounded until after the scene is clear.6–8, 16, 31
This concept became a reality following the 2013 Boston Marathon bombing, as improvised tourniquets were predominately used by bystanders and first responders to control bleeding limbs.33 Finally, the International Liaison Committee on Resuscitation suggests the use of a tourniquet by first aid providers when direct pressure and/or a pressure dressing fails to control hemorrhage, however still cites this as a weak recommendation with low-quality evidence.34
In summary, while PH civilian tourniquet use may be increasing, the current landscape offers no clear consensus on the appropriate setting (PH or after arrival to the ED), mechanism of injury or even anatomic location where tourniquets are appropriate for civilian use.35 This is due in part to the lack of a randomized, controlled trial assessing the safety and efficacy of civilian tourniquet use, despite the unlikely occurrence that one ever will exist.
Animal models have demonstrated the lethality of femoral artery transection following tourniquet release, despite the application of direct pressure with a polymeric hemostatic agent.36 Several retrospective studies of civilians with major limb trauma have demonstrated a potential benefit to tourniquet use in civilians. Passos et al.37conducted a retrospective review comparing 8 patients with isolated major limb bleeding that had either a PH or ED tourniquet placed with 6 patients that did not have a tourniquet and died. The group that did receive a tourniquet and died were more likely to have received a massive transfusion, suggesting that early tourniquet use would have prevented exsanguination. Dorlac et al.38 conducted a retrospective review of 14 patients who died from isolated penetrating limb trauma and no effective PH control of bleeding from these wounds. There was a 100% mortality for this group, with almost 60% graded as being potentially preventable deaths (had control of hemorrhage had been obtained), suggesting that limb tourniquets could have been life-saving.
Additionally, recent publications have described the experience of civilian tourniquet use. Schroll and colleagues39 conducted a multi-institution study of 197 patients with PH tourniquets (both improvised tourniquets and commercially manufactured ones) and concluded that PH personnel can safely and effectively apply tourniquets. A survival benefit was difficult to appreciate as the mortality for the group was low (3%). Inaba and colleagues40 evaluated 87, young patients with predominant penetrating, isolated major limb trauma with improvised, CAT and pneumatic tourniquets placed in the field, ED or operating room. The investigators reported an overall vascular injury rate of 80% with an associated complication rate of 8% and amputation rate of 17% (only one of which was attributed to the actual tourniquet). The authors concluded that the potential benefit of using tourniquets in civilians outweighs the low associated complication rate. Ode and colleagues41additionally conducted a retrospective analysis of 24 patients that received either CAT or improvised tourniquets with zero complications despite imperfect patient selection (21% unindicated). The Boston EMS system also described their experience with PH surgical tubing tourniquets (not CAT), in which 50% were applied by basic life support providers. 92% of these tourniquets were successful in controlling bleeding and 2 of 95 cases had a complication potentially associated with the tourniquet application.42 Finally, Callaway et al.32 described a case report of tourniquet application to four patients by law enforcement officers, 3 of which had a vascular injury, all patients survived to hospital discharge, and no patients suffered any tourniquet-related complications.
Therefore, the body of literature supporting the concept that civilians sustain life-threatening, limb trauma which is amenable to control via a tourniquet with a low complication rate is growing, and our study additionally augments this claim. This is the largest single-center study to date that reports the use of tourniquets for civilians with major limb trauma. Similar to military21, 23, 43, 44 and new civilian studies41 we have demonstrated a low complication rate with none attributed to tourniquet use despite imperfect selection for tourniquet application. In addition, we have displayed use in a population that is injured predominately via single lacerations or multiply injured in motor vehicle collisions. Bulger and colleagues45 previously noted that the military literature could not address the safety of tourniquets in elderly and pediatric patients. We have demonstrated safety across various age groups, with patients as young as four and old as 91 years of age.
This study is limited due to its single-center and retrospective nature. As a result, tourniquet times could not be abstracted from the patient record. Assuming that tourniquet and transport times are nearly equivalent, our recorded transport times took 31 (23, 39) minutes, which is considerably shorter than the 2 hours used for tourniquets in the operating room.45, 46 However, it is difficult to conclude that the limited observation of complications would be observed regardless of tourniquet time or in a setting with an immature trauma system with prolonged transport times. The retrospective nature of this study additionally limited the abstraction of specific information regarding location of the five nerve palsies in relation to the level of the tourniquet. Likewise, the specific criteria for the limb ischemia component of the Mangled Extremity Severity Score (MESS; reduced pulse but normal perfusion/pulseless, paresthesia, slow capillary refill/cool, paralysis, numb/insensate) could not be accurately extracted from retrospective records. Finally, as the mortality of this cohort was low (7%), and as there was no comparison group, it is difficult to comment on the mortality benefit of tourniquet use in the civilian setting. When identifying the limitations of this study, several areas for improvement regarding documentation of tourniquet use were identified. Specifically, documentation of actual tourniquet time, the reason for and level of tourniquet placement, the adequacy of tourniquet placement, level of any nerve palsy in relation to tourniquet placement and a formal MESS assessed in real-time by the clinicians evaluating the injury would have improved the quality of this study.
Conclusion
Our study displays that in civilians sustaining major limb trauma, prehospital and in-hospital personnel are capable of applying tourniquets to the appropriate patient. After adjudication, there were no complications due to tourniquet use, even in pediatric and elderly patients, deeming them safe for use in civilians with major upper or lower limb trauma via blunt or penetrating mechanisms of any etiology.
Acknowledgments
Funding for Dr. Scerbo was provided through NIH Grant 5T32GM008792.
Footnotes
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Rhee P, Joseph B, Pandit V, et al. Increasing trauma deaths in the United States. Ann Surg. 2014;260:13–21. doi: 10.1097/SLA.0000000000000600. [DOI] [PubMed] [Google Scholar]
- 2.Davis JS, Satahoo SS, Butler FK, et al. An analysis of prehospital deaths: Who can we save? J Trauma Acute Care Surg. 2014;77:213–218. doi: 10.1097/TA.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 3.Eastridge BJ, Mabry RL, Seguin P, et al. Death on the battlefield (2001–2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73:S431–S437. doi: 10.1097/TA.0b013e3182755dcc. [DOI] [PubMed] [Google Scholar]
- 4.Kragh JF, Jr, Walters TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249:1–7. doi: 10.1097/SLA.0b013e31818842ba. [DOI] [PubMed] [Google Scholar]
- 5.Kragh JF, Jr, Walters TJ, Baer DG, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J. Trauma. 2008;64:S38–S50. doi: 10.1097/TA.0b013e31816086b1. [DOI] [PubMed] [Google Scholar]
- 6.Smith R, Callaway DW. Tactical emergency casualty care. The need for & evolution of civilian high threat medical guidelines. JEMS. 2014;(Suppl):10–15. [PubMed] [Google Scholar]
- 7.Cannon M. Law enforcement and the long gun: do we need a new face in the fight? J Emeg Med. 2013;45:710–713. doi: 10.1016/j.jemermed.2013.01.026. [DOI] [PubMed] [Google Scholar]
- 8.Callaway DW, Smith ER, Cain J, et al. Tactical emergency casualty care (TECC): guidelines for the provision of prehospital trauma care in high threat environments. J Spec Oper Med. 2011;11:104–122. doi: 10.55460/8BUM-KREB. [DOI] [PubMed] [Google Scholar]
- 9.Welling DR, Burris DG, Hutton JE, Minken SL, Rich NM. A balanced approach to tourniquet use: lessons learned and relearned. J Am Coll Surg. 2006;203:106–115. doi: 10.1016/j.jamcollsurg.2006.02.034. [DOI] [PubMed] [Google Scholar]
- 10.Husum H, Gilbert M, Wisborg T, Pillgram-Larsen J. Prehospital tourniquets: there should be no controversy. J Trauma. 2004;56:214–215. doi: 10.1097/01.TA.0000104494.62175.2F. [DOI] [PubMed] [Google Scholar]
- 11.Lee C, Porter KM, Hodgetts TJ. Tourniquet use in the civilian prehospital setting. Emerg Med J. 2007;24:584–587. doi: 10.1136/emj.2007.046359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doyle GS, Taillac PP. Tourniquets: a review of current use with proposals for expanded prehospital use. Prehosp Emerg Care. 2008;12:241–256. doi: 10.1080/10903120801907570. [DOI] [PubMed] [Google Scholar]
- 13.Sasser SM, Hunt RC, Faul M, et al. Centers for Disease Control; Prevention (CDC) Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm. Rep. 2012;61:1–20. [PubMed] [Google Scholar]
- 14.ATLS Subcommittee, American College of Surgeons’ Committee on Trauma … International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2012;74:1363–1366. doi: 10.1097/TA.0b013e31828b82f5. [DOI] [PubMed] [Google Scholar]
- 15.Fox N, Rajani RR, Bokhari F, et al. Eastern Association for the Surgery of Trauma. Evaluation and management of penetrating lower extremity arterial trauma: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S315–S320. doi: 10.1097/TA.0b013e31827018e4. [DOI] [PubMed] [Google Scholar]
- 16.Pons PT, Jerome J, McMullen J, Manson J, Robinson J, Chapleau W. The Hartford Consensus on Active Shooters: implementing the continuum of prehospital trauma response. J Emerg Med. 2015;49:878–885. doi: 10.1016/j.jemermed.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Fisher AD, Callaway DW, Robertson JN, Hardwick SA, Bobko JP, Kotwal RS. The Ranger First Responder Program and Tactical Emergency Casualty Care Implementation: a whole-community approach to reducing mortality from active violent incidents. J Spec Oper Med. 2015;15:46–53. doi: 10.55460/J3TF-9EKV. [DOI] [PubMed] [Google Scholar]
- 18.Bobko J, Lai TT, Smith ER, et al. Tactical emergency casualty care? Pediatric appendix: novel guidelines for the care of the pediatric casualty in the high-threat, prehospital environment. J Spec Oper Med. 2013;13:94–107. doi: 10.55460/EF77-LDYW. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs LM and the Joint Committee to Create a National Policy to Enhance Survivability from Mass Casualty Shooting Events. The Hartford Consensus IV: a call for increased national resilience. Bull Am Coll Surg. 2016;101:25–32. [Google Scholar]
- 20.Rahbar E, Fox EE, del Junco DJ, et al. PROMMTT Study Group. Early resuscitation intensity as a surrogate for bleeding severity and early mortality in the PROMMTT study. J Trauma Acute Care Surg. 2013;75:S16–S23. doi: 10.1097/TA.0b013e31828fa535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beekley AC, Sebesta JA, Blackbourne LH, et al. 31st Combat Support Hospital Research Group. Prehospital tourniquet use in Operation Iraqi Freedom: effect on hemorrhage control and outcomes. J Trauma. 2008;64:S28–S37. doi: 10.1097/TA.0b013e318160937e. [DOI] [PubMed] [Google Scholar]
- 22.Kragh JF, Jr, Nam JJ, Berry KA, et al. Transfusion for shock in US military war casualties with and without tourniquet use. Ann Emerg Med. 2015;65:290–296. doi: 10.1016/j.annemergmed.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 23.Lakstein D, Blumenfeld A, Sokolov T, et al. Tourniquets for hemorrhage control on the battlefield: a 4-year accumulated experience. J Trauma. 2003;54:S221–S225. doi: 10.1097/01.TA.0000047227.33395.49. [DOI] [PubMed] [Google Scholar]
- 24.Wall PL, Welander JD, Smith HL, Buising CM, Sahr SM. What do the people who transport trauma patients know about tourniquets? J Trauma Acute Care Surg. 2014;77:734–742. doi: 10.1097/TA.0000000000000433. [DOI] [PubMed] [Google Scholar]
- 25.Haider AH, Piper LC, Zogg CK, et al. Military-to-civilian translation of battlefield innovations in operative trauma care. Surgery. 2015;158:1686–1695. doi: 10.1016/j.surg.2015.06.026. [DOI] [PubMed] [Google Scholar]
- 26.Kauvar DS, Sarfati MR, Kraiss LW. National trauma databank analysis of mortality and limb loss in isolated lower extremity vascular trauma. J Vasc Surg. 2011;53:1598–1603. doi: 10.1016/j.jvs.2011.01.056. [DOI] [PubMed] [Google Scholar]
- 27.Franz RW, Skytta CK, Shah KJ, Hartman JF, Wright ML. A five-year review of management of upper-extremity arterial injuries at an urban level I trauma center. Ann Vasc Surg. 2012;26:655–664. doi: 10.1016/j.avsg.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 28.Tan TW, Joglar FL, Hamburg NM, et al. Limb outcome and mortality in lower and upper extremity arterial injury: a comparison using the National Trauma Data Bank. Vasc Endovascular Surg. 2011;45:592–597. doi: 10.1177/1538574411415125. [DOI] [PubMed] [Google Scholar]
- 29.Jacobs LM, McSwain N, Rotondo M, et al. Joint Committee to Create a National Policy to Enhance Survivability from Mass Casualty Shooting Events. Improving survival from active shooter events: the Hartford Consensus. Bull Am Coll Surg. 2013;98:14–16. [PubMed] [Google Scholar]
- 30.Ramly EP, Runyan G, King DR. The state of the union: Nationwide absence of uniform guidelines for the pre-hospital use of tourniquets to control extremity exsanguination. J Trauma Acute Care Surg. 2016 Feb 16; doi: 10.1097/TA.0000000000000988. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Butler FK, Giebner SD, McSwain N, Pons P. Prehospital Trauma Life Support Manual; Eighth Edition - Military Version. 2014 [Google Scholar]
- 32.Callaway DW, Robertson J, Sztajnkrycer MD. Law enforcement-applied tourniquets: a case series of life-saving interventions. Prehosp Emerg Care. 2015;19:320–327. doi: 10.3109/10903127.2014.964893. [DOI] [PubMed] [Google Scholar]
- 33.King DR, Larentzakis A, Ramly EP Boston Trauma Collaborative. Tourniquet Use at the Boston Marathon bombing: Lost in translation. J Trauma Acute Care Surg. 2015;78:594–599. doi: 10.1097/TA.0000000000000561. [DOI] [PubMed] [Google Scholar]
- 34.American Heart Association and American Red Cross. Web-based Integrated Guidelines for First Aid. [Accessed March 11, 2016];© 2015 American Heart Association, Inc., and The American National Red Cross. Available at: firstaidguidelines.heart.org.
- 35.Kragh JF, Jr, Aden JK, 3rd, Walters TJ, et al. In reply. Ann Emerg Med. 2015;66:340–341. doi: 10.1016/j.annemergmed.2015.04.024. [DOI] [PubMed] [Google Scholar]
- 36.Walters T, Baer DG, Kauvar DS. A large animal fatal extremity hemorrhage model and evaluation of a polymeric dressing (fatal extremity hemorrhage) J Traum. 2006;61:1107–1112. doi: 10.1097/01.ta.0000195655.30837.29. [DOI] [PubMed] [Google Scholar]
- 37.Passos E, Dingley B, Smith A, et al. Canadian Trauma Trials Collaborative. Tourniquet use for peripheral vascular injuries in the civilian setting. Injury. 2014;45:573–577. doi: 10.1016/j.injury.2013.11.031. [DOI] [PubMed] [Google Scholar]
- 38.Dorlac WC, DeBakey ME, Holcomb JB, et al. Mortality from isolated civilian penetrating extremity injury. J Trauma. 2005;59:217–222. doi: 10.1097/01.ta.0000173699.71652.ba. [DOI] [PubMed] [Google Scholar]
- 39.Schroll R, Smith A, McSwain NE, Jr, et al. A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg. 2015;79:10–14. doi: 10.1097/TA.0000000000000689. [DOI] [PubMed] [Google Scholar]
- 40.Inaba K, Siboni S, Resnick S, et al. Tourniquet use for civilian extremity trauma. J Trauma Acute Care Surg. 2015;79:232–237. doi: 10.1097/TA.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 41.Ode G, Studnek J, Seymour R, Bosse MJ, Hsu JR. Emergency tourniquets for civilians: Can military lessons in extremity hemorrhage be translated? J Trauma Acute Care Surg. 2015;79:586–591. doi: 10.1097/TA.0000000000000815. [DOI] [PubMed] [Google Scholar]
- 42.Kue RC, Temin ES, Weiner SG, et al. Tourniquet use in a civilian emergency medical services setting: a descriptive analysis of the Boston EMS experience. Prehosp Emerg Care. 2015;19:399–404. doi: 10.3109/10903127.2014.995842. [DOI] [PubMed] [Google Scholar]
- 43.Kue RC, Temin ES, Weiner SG, et al. Tourniquet use in a civilian emergency medical services setting: a descriptive analysis of the Boston EMS experience. Prehosp Emerg Care. 2015;19:399–404. doi: 10.3109/10903127.2014.995842. [DOI] [PubMed] [Google Scholar]
- 44.Kragh JF, Jr, Littrel ML, Jones JA, et al. Battle casualty survival with emergency tourniquet use to stop limb bleeding. J Emerg Med. 2011;41:590–597. doi: 10.1016/j.jemermed.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 45.Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18:163–173. doi: 10.3109/10903127.2014.896962. [DOI] [PubMed] [Google Scholar]
- 46.Fitzgibbons PG, Digiovanni C, Hares S, Akelman E. Safe tourniquet use: a review of the evidence. J Am Acad Orthop Surg. 2012;20:310–319. doi: 10.5435/JAAOS-20-05-310. [DOI] [PubMed] [Google Scholar]