Abstract
Background
Vascular access failure is a huge burden for patients undergoing hemodialysis. Many efforts have been made to maintain vascular access patency, including pharmacotherapy. Angiotensin converting enzyme inhibitor (ACE-I), angiotensin receptor blocker (ARB), and calcium channel blocker (CCB) are known for their antihypertensive and cardio-protective effects, however, their effects on long-term vascular access patency are still inconclusive.
Design, setting, participants and measurements
We retrospectively enrolled patients commencing maintenance hemodialysis between January 1, 2000, and December 31, 2006 by using National Health Insurance Research Database in Taiwan. Primary patency was defined as the date of first arteriovenous fistula (AVF) or arteriovenous graft (AVG) creation to the time of access thrombosis or any intervention aimed to maintain or re-establish vascular access patency. Cox proportional hazards models were used to adjust the influences of patient characteristics, co-morbidities and medications.
Results
Total 42244 patients were enrolled in this study, 37771 (89.4%) used AVF, 4473 (10.6%) used AVG as their first long term dialysis access. ACE-I, ARB, and CCB use were all associated with prolonged primary patency of AVF [hazard ratio (HR) 0.586, 95% confidence interval (CI) 0.557–0.616 for ACE-I use; HR 0.532, CI 0.508–0.556 for ARB use; HR 0.485, CI 0.470–0.501 for CCB use] and AVG (HR 0.557, CI 0.482–0.643 for ACE-I use, HR 0.536, CI 0.467–0.614 for ARB use, HR 0.482, CI 0.442–0.526 for CCB use).
Conclusions
In our analysis, ACE-I, ARB, and CCB were strongly associated with prolonged primary patency of both AVF and AVG. Further prospective randomized studies are still warranted to prove the causality.
Introduction
Vascular access is crucial for patients on maintenance hemodialysis. A functional long-term vascular access is associated better life quality [1], less mortality [2–4] and hospitalization [5]. However, vascular access occlusion is still a major cause of hospitalization in patients undergoing hemodialysis [6]. And the cost for vascular access failure is still high in recent years.
Many strategies have been surveyed in order to prolong vascular access patency, including meticulous pre-operative planning [7], newer design of vascular access [8], stent implantation [9,10], far infrared therapy [11], and pharmacotherapy [12–16]. Among pharmacotherapy, some cardioprotective antihypertensive agents have drawn attention recently, including angiotensin converting enzyme inhibitor (ACE-I), angiotensin receptor blocker (ARB) and calcium channel blocker (CCB). Theoretically, ACE-I, ARB and CCB could increase vascular access patency through inhibiting venous neointimal hyperplasia, an important mechanism of arteriovenous fistula (AVF) and arteriovenous graft (AVG) failure [17–21]. However, the results of these drugs on clinical studies were still controversial [12,13,16,22–24]. The aim of this study is to evaluate whether ACE-I, ARB, and CCB could have impact on long-term vascular access patency.
Materials and Methods
Database
The National Health Insurance (NHI) program has provided compulsory universal health insurance in Taiwan since 1995. With the exception of prison inmates, all citizens have been enrolled in the program. All contracted medical institutions must submit standard computerized claim documents for medical expenses. Patients with End stage renal disease (ESRD) are eligible for any type of renal replacement therapy free of any charge; all maintenance dialysis patients are covered by NHI.
Data were obtained from the National Health Insurance Research Database (NHIRD) [Bureau of National Health Insurance. Available at: www.doh.gov.tw/statistic/index.htm [In Chinese] (accessed September 25, 2011); http://www.doh.gov.tw/EN2006/index_EN.aspx [In English]] and released for research by the Taiwan National Health Research Institute. The NHIRD covers nearly all (99%) inpatient and outpatient medical benefit claims for Taiwan’s 23 million residents, is one of the largest and most comprehensive databases in the world, and has been used extensively in various studies. Patient identification numbers, gender, birthday, dates of admission and discharge, medical institutions providing the services, the ICD-9-CM (International Classification of Diseases, 9th Revision, Clinical Modification) diagnostic and procedure codes, and outcomes are encrypted. We used the NHIRD for ambulatory care claims, all inpatient claims, and the updated registry for beneficiaries for this study. All datasets can be interlinked through each individual’s unique personal identification number.
Patient selection and definition
Incident adult ESRD patients (≥18 years old) who began maintenance hemodialysis between January 1, 2000, and December 31, 2006 were included in this study. ESRD patients on maintenance hemodialysis were defined as having undergone hemodialysis for more than 90 days. All incident patients with first payment and operation code for AVF (procedure code 69032C) or AVG (procedure code 69034C) between January 1, 1998, and December 31, 2008 were identified to analyze. A total of 42244 incident dialysis patients were analyzed in this study.
The definition of primary patency was the time from the first reported date of vascular access creation to the date of access thrombosis or any intervention aimed to maintain or re-establish vascular access patency. Patients were followed during the period of primary patency. Patient who died or discontinuing dialysis, or whose vascular access remained patent during hemodialysis after December 31, 2008 were censored. Vascular access dysfunction was identified based on the diagnostic code for vascular thrombosis (ICD-9-CM 996.73, other complications due to renal dialysis device implant and graft) and operative procedures for vascular thrombotic occlusion (thrombectomy, procedure code 38.0; reconstruction of access, procedure code, 69032C; embolectomy, arterial, 69001B; embolectomy, arterial catheter, 69002B; thrombectomy, venous, 69003B) at a subsequent admission or outpatient visit. Vascular access related intervention [percutaneous transluminal angiography (PTA), revision or removal of vascular access] were identify either by NHI' s procedure code or by disease code.
Ascertaining the demographic and comorbid variables
We linked to the diagnostic codes through the inpatient and outpatient claims databases of the NHI. We included patient demographics, and baseline comorbidities. Baseline comorbidities—including diabetes mellitus (DM), hypertension (HTN), coronary artery disease (CAD), ischemic cerebrovascular disease, deep venous thrombosis (DVT), peripheral artery disease (PAD), dyslipidemia, hyperuricemia, chronic liver disease—were analyzed. In addition, the use of ACE-I, ARB, or CCB for more than 3 months after creation of AVF or AVG was also identified by the codes specified for those drugs. The drugs evaluated in the study were listed in Table 1.
Table 1. Drugs included in the study.
| Angiotensin converting enzyme inhibitor | Angiotensin receptor blocker |
| Benazepril | Candesartan |
| Enalapril | Losartan |
| Lisinopril | Irbesartan |
| Quinapril | Valsartan |
| Captopril | Olmesartan |
| Fosinopril | Calcium channel blocker |
| Ramipril | Amlodipine |
| Verapamil | Felodipine |
| Cilazapril | Nifedipine |
| Verapamil | |
| Diltiazem | |
| Isradipine | |
| Nicardipine |
Statistical analysis
Parametric Pearson’s chi square test is utilized to compare each variable in the groups of patients with using AVF and AVG. Age was entered as a categorical variable (18 to 44, 45 to 64, and 65 years or older). Significance was set at p < 0.05. The cumulative incidences of vascular dysfunction after vascular access creation were calculated using the Kaplan-Meier method. The log rank test was used to analyze significance. Cox proportional hazards models were used to identify the risk factors of vascular access dysfunction after vascular access creation. Hazard ratios (HR) and 95% confidence intervals (CI) were derived from Cox proportional hazards models. Cox models met the assumption of proportionality of risks. To adjust for potential confounding in the relationship between variables and the vascular access dysfunction, multivariate analyses were used. All statistical operations were performed using the Statistical Package for Social Sciences for Windows 17.0 (SPSS Inc; Chicago, IL, USA).
Results
Patient characteristics
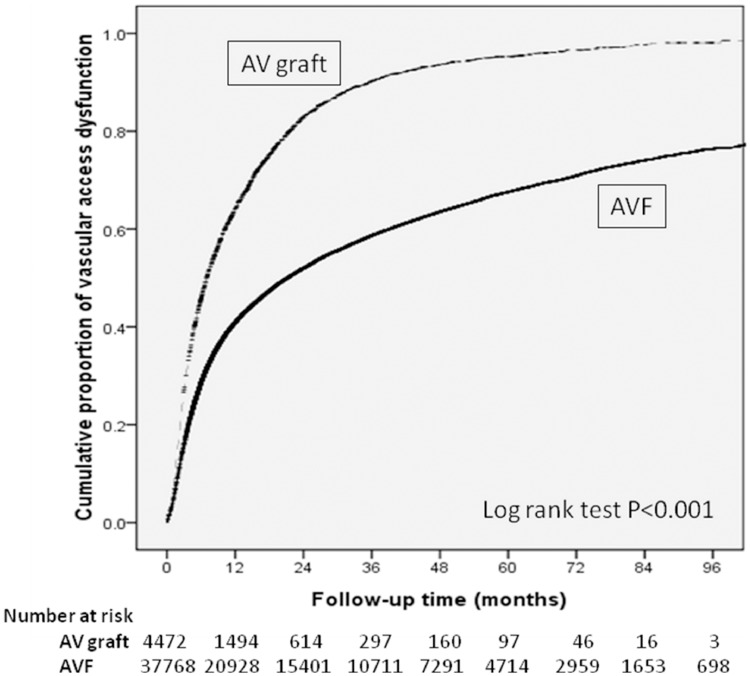
Total 42244 patients were enrolled in this study. 37771 (89.4%) used AVF, 4473 (10.6%) used AVG as their first long term dialysis access (Table 2). Patients using AVF were male predominant, older, and they had lower prevalence of diabetes mellitus (p < 0.001), coronary artery disease (p < 0.001), ischemic cerebrovascular disease (p < 0.001), peripheral artery disease (p = 0.005), and deep vein thrombosis (p = 0.039). AVF group also had higher rate of using renin-angiotensin blockage and CCB. Compared with patients using AVF, those using AVG had higher frequency of creation of vascular access before dialysis (75.9% V.S 68.8%). The cumulative patency of primary AVG and AVF was 35.9% and 59.2% at the end of year 1, but only 4.7% and 32.5% at the end of year 5 respectively. The incidence of primary patency was significantly higher in AVF group both in univariate and multivariate analysis (Fig 1).
Table 2. Patient characteristics and association with using arteriovenous fistula and arteriovenous graft among end-stage renal disease hemodialysis patients.
| Patients Using an AVF (n = 37771) | Patients Using an AVG (n = 4473) | P value | |||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Sex | <0.001 | ||||
| Female | 18327 | (86.6) | 2841 | (13.4) | |
| Male | 19444 | (92.3) | 1632 | (7.7) | |
| Age (years) | <0.001 | ||||
| 18–44 | 5058 | (94.5) | 296 | (5.5) | |
| 45–64 | 17446 | (91.3) | 1671 | (8.7) | |
| ≥ 65 | 15267 | (85.9) | 2506 | (14.1) | |
| Time of vascular access creation | <0.001 | ||||
| After initiating dialysis | 13214 | (91.6) | 1209 | (8.4) | |
| 0–1 month before dialysis | 13323 | (87.8) | 1843 | (12.2) | |
| ≥ 1 month before dialysis | 11234 | (88.8) | 1421 | (11.2) | |
| Diabetic mellitus | <0.001 | ||||
| No | 18943 | (90.6) | 1954 | (9.4) | |
| Yes | 18828 | (88.2) | 2519 | (11.8) | |
| Hypertension | 0.232 | ||||
| No | 7144 | (89.8) | 813 | (10.2) | |
| Yes | 30627 | (89.3) | 3660 | (10.7) | |
| Coronary artery disease | <0.001 | ||||
| No | 29122 | (90.1) | 3204 | (9.9) | |
| Yes | 8649 | (87.2) | 1269 | (12.8) | |
| Ischemic cerebrovascular disease | <0.001 | ||||
| No | 35791 | (89.6) | 4139 | (10.4) | |
| Yes | 1980 | (85.6) | 334 | (14.4) | |
| Deep venous thrombosis | 0.039 | ||||
| No | 37533 | (89.4) | 4433 | (10.6) | |
| Yes | 238 | (85.6) | 40 | (14.4) | |
| Peripheral artery disease | 0.005 | ||||
| No | 36654 | (89.5) | 4307 | (10.5) | |
| Yes | 1117 | (87.1) | 166 | (12.9) | |
| Dyslipidemia | 0.427 | ||||
| No | 31310 | (89.4) | 3729 | (10.6) | |
| Yes | 6461 | (89.7) | 744 | (10.3) | |
| Hyperuricemia | 0.129 | ||||
| No | 32371 | (89.3) | 3871 | (10.7) | |
| Yes | 5400 | (90.0) | 602 | (10) | |
| Chronic liver disease | 0.131 | ||||
| No | 34431 | (89.5) | 4047 | (10.5) | |
| Yes | 3340 | (88.7) | 426 | (11.3) | |
| Drug Usage (%) | |||||
| ACE-I | 10.7% | 6.2% | <0.001 | ||
| ARB | 15.0% | 7.1% | <0.001 | ||
| CCB | 32.2% | 20.6% | <0.001 | ||
AVF: arteriovenous fistula; AVG: arteriovenous graft; ACE-I: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; CCB: calcium channel blocker.
Fig 1. Cumulative incidence of vascular access dysfunction.
Patient characteristics associated with AVF and AVG dysfunction
Tables 3 and 4 showed the factors associated with vascular access dysfunction. In patients with AVF, patient characteristics relating to more access dysfunction in multivariate analysis were female sex (HR 0.964, CI 0.939–0.990), age (HR 1.177, CI 1.129–1.228 in those aged 45–64, HR 1.329, CI 1.272–1.387 in those aged ≥ 65, comparing to reference group aged 18–44), diabetes mellitus (HR 1.264, CI 1.229–1.300), hypertension (HR 1.149, CI 1.110–1.189), coronary artery disease (HR 1.109, CI 1.074–1.144), deep venous thrombosis (HR 1.267, CI 1.087–1.476), peripheral artery disease (HR 1.195, CI 1.111–1.285), dyslipidemia (HR 1.101, CI 1.063–1.140). Early AVF creation was associated with less AVF dysfunction. Comparing to reference group who received AVF creation after commencing hemodialysis, there’s a HR 0.969, CI 0.940–0.999 in group whose AVF created 0-1 month before, and a HR 0.948, CI 0.917–0.979 in group whose AVF created more than 1 month before commencing hemodialysis.
Table 3. Risk factors for arteriovenous fistula dysfunction among maintenance hemodialysis patients.
| Covariate | Univariate analysis | Multivariate analysis |
|---|---|---|
| HR (95% CI) | HR (95% CI) | |
| Sex (Male vs. Female) | 0.939 (0.916–0.963)* | 0.964 (0.939–0.99)* |
| Age at initiation of Dialysis | ||
| 18–44 (Reference) | 1 | 1 |
| 45–64 | 1.251 (1.201–1.304)* | 1.177 (1.129–1.228)* |
| ≥ 65 | 1.512 (1.451–1.577)* | 1.329 (1.272–1.387)* |
| Time of vascular access creation | ||
| After initiating dialysis (Reference) | 1 | 1 |
| 0–1 month before dialysis | 0.951 (0.922–0.980)* | 0.969 (0.940–0.999)* |
| More than 1 month before dialysis | 0.839 (0.812–0.866)* | 0.948 (0.917–0.979)* |
| Comorbidities | ||
| Diabetic Mellitus (yes vs. no) | 1.228 (1.197–1.260)* | 1.264 (1.229–1.300)* |
| Hypertension (yes vs. no) | 1.083 (1.048–1.119)* | 1.149 (1.110–1.189)* |
| Coronary Artery Disease (yes vs. no) | 1.175 (1.140–1.211)* | 1.109 (1.074–1.144)* |
| Ischemic Cerebrovascular disease (yes vs. no) | 1.142 (1.079–1.209)* | 1.045 (0.986–1.107) |
| Deep venous thrombosis (yes vs. no) | 1.410 (1.210–1.642)* | 1.267 (1.087–1.476)* |
| Peripheral artery disease (yes vs. no) | 1.266 (1.178–1.361)* | 1.195 (1.111–1.285)* |
| Dyslipidemia (yes vs. no) | 1.083 (1.047–1.120)* | 1.101 (1.063–1.140)* |
| Hyperuricemia (yes vs. no) | 1.005 (0.696–1.042) | 1.031 (0.993–1.071) |
| Chronic liver disease (yes vs. no) | 0.950 (0.907–0.995)* | 1.003 (0.970–1.036) |
| Drug Usage | ||
| ACE-I (yes vs. no) | 0.428 (0.407–0.449)* | 0.586 (0.557–0.616)* |
| ARB (yes vs. no) | 0.386(0.370–0.404)* | 0.532 (0.508–0.556)* |
| CCB (yes vs. no) | 0.405 (0.393–0.417)* | 0.485 (0.470–0.501)* |
ACE-I: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; CCB: calcium channel blocker.
*indicates a significant difference (p<0.05).
Table 4. Risk factors for arteriovenous graft dysfunction among maintenance hemodialysis patients.
| Covariate | Univariate analysis | Multivariate analysis |
|---|---|---|
| HR (95% CI) | HR (95% CI) | |
| Sex (Male v Female) | 1.010 (0.947–1.078) | 0.989 (0.925–1.056) |
| Age at initiation of Dialysis | ||
| 18–44 (Reference) | 1 | 1 |
| 45–64 | 1.056 (0.927–1.202) | 1.126 (0.988–1.285) |
| ≥ 65 | 1.137 (1.002–1.290)* | 1.207 (1.061–1.373)* |
| Time of vascular access creation | ||
| After initiating dialysis (Reference) | 1 | 1 |
| 0–1 month before dialysis | 0.923 (0.855–0.997)* | 0.966 (0.894–1.044) |
| More than 1 month before dialysis | 0.766 (0.706–0.831)* | 0.857 (0.789–0.931)* |
| Comorbidities | ||
| Diabetic Mellitus (yes vs. no) | 1.072 (1.006–1.141)* | 1.143 (1.068–1.223)* |
| Hypertension (yes vs. no) | 0.974 (0.898–1.055) | 1.064 (0.977–1.159) |
| Coronary Artery Disease (yes vs. no) | 1.000 (0.933–1.072) | 1.018 (0.947–1.093)* |
| Ischemic Cerebrovascular disease (yes vs. no) | 1.079 (0.957–1.217) | 1.073 (0.950–1.212) |
| Deep venous thrombosis (yes vs. no) | 1.339 (0.973–1.743) | 1.374 (0.998–1.863) |
| Peripheral artery disease (yes vs. no) | 1.058 (0.896–1.480) | 1.047 (0.886–1.237) |
| Dyslipidemia (yes vs. no) | 0.979 (0.900–1.065) | 1.038 (0.952–1.132) |
| Hyperuricemia (yes vs. no) | 1.024 (0.935–1.121) | 1.081 (0.984–1.187) |
| Chronic liver disease (yes vs. no) | 0.954 (0.857–1.061) | 1.010 (0.931–1.096) |
| Drug Usage | ||
| ACE-I (yes vs. no) | 0.407 (0.354–0.468)* | 0.557 (0.482–0.643)* |
| ARB (yes vs. no) | 0.396 (0.347–0.452)* | 0.536 (0.467–0.614)* |
| CCB (yes vs. no) | 0.400 (0.369–0.434)* | 0.482 (0.442–0.526)* |
ACE-I: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; CCB: calcium channel blocker.
*indicates a significant difference (p<0.05).
Patient characteristics associated with more AVG dysfunction in multivariate analysis were older age (HR1.207, CI 1.061–1.373 in group aged ≥ 65, but no significance in those aged 45–64, comparing with reference group aged 18–44), diabetes mellitus (HR 1.143, CI 1.068–1.223), and coronary artery disease (HR 1.018, CI 0.947–1.093). AVG created more than 1 month before hemodialysis was associated with less AVG dysfunction comparing with AVG created after hemodialysis(HR 0.857, CI 0.789–0.931), but there’s no difference in AVG created 0–1 month before HD comparing with the reference group(HR 0.966, CI 0.894–1.044).
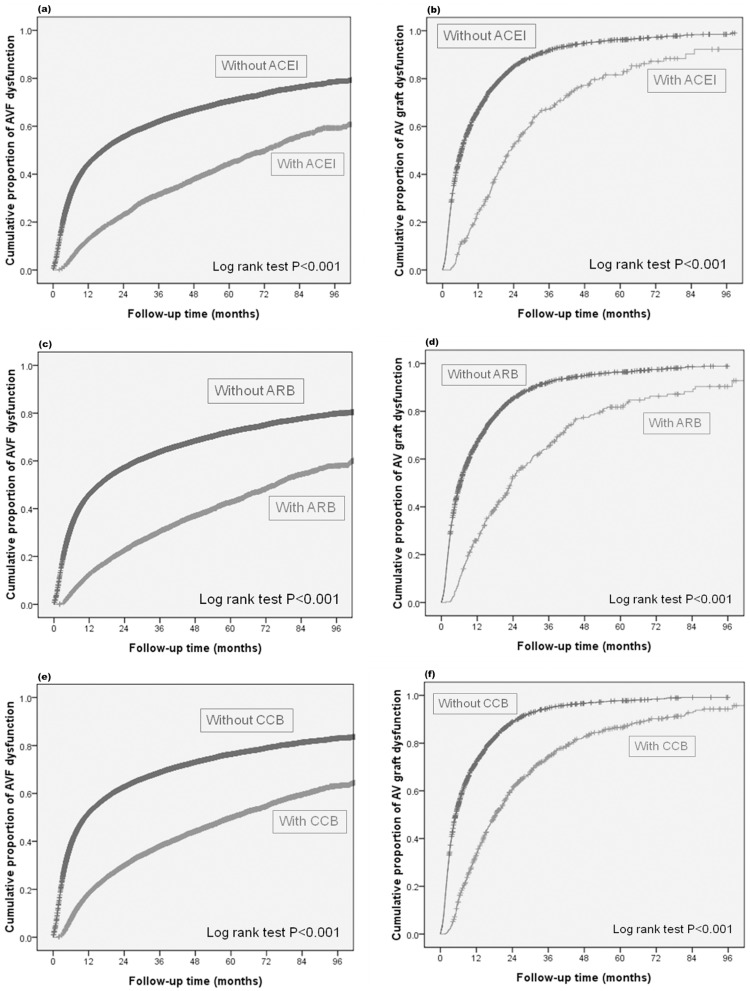
Medications and AVF and AVG dysfunction
Fig 2 showed Kaplan-Meier curve of medication use and cumulative incidences of vascular access dysfunction. All three kinds of medications were related to less AVF dysfunction in multivariate analysis, including ACE-I (HR 0.586, CI 0.557–0.616), ARB (HR 0.532, CI 0.508–0.556) and CCB (HR 0.485, CI 0.470–0.501). These medications were also associated with less AVG dysfunction by multivariate analysis [ACE-I (HR 0.557, CI 0.482–0.643), ARB (HR 0.536, CI 0.467–0.614), CCB (HR 0.482, CI 0.442–0.526)].
Fig 2. Cumulative incidence of vascular access dysfunction stratified by drugs.
(a) ACEI & AVF (b) ACEI & AVG (c) ARB & AVF (d) ARB & AVG (e) CCB & AVF (f) CCB & AVG.
Discussion
The objective of the study was to evaluate the relationship between anti-hypertensive drugs and primary patency of long-term vascular access. Our analysis revealed that ACE-I, ARB, and CCB were all associated with decreased risk of AVF and AVG dysfunction. For AVF, the relative risk reduction in ACE-I, ARB, and CCB user were 41%, 47%, and 51%. For AVG, the relative risk reduction associated with ACE-I, ARB, and CCB user were 44%, 46%, and 52%.
There were researches aimed for ACE-I and vascular access patency. Gradzki [23] et al. found that ACE-I was associated with higher AVG patency. Saran [13] et al. also reported that ACE-I was related to prolonged secondary patency of AVF. Our study also showed ACE-I was associated with prolonged primary patency in both AVG and AVG groups.
The association between vascular access patency and use of ARB is controversial. Jackson et al reported that ARB prolongs primary patency in both AVF and AVG groups [12], whereas the DOPPS study [13] showed that there’s no relationship between ARB and vascular access patency, neither in AVF or AVG. However, there is a relatively low rate of ARB use in the DOPPS population (3.8% in AVG group, and 4.1% in AVF group). The rates of using ARB in our AVF and AVG groups were 15.0% and 7.1%, respectively. This turned out to be about 5666 and 318 patients using ARB in our AVF and AVG group, which may increase the statistical power. Moreover, the subjects included in our study were somewhat different from those in DOPPS:Our study focused on the patients whose long-term vascular access was first created, most of them were incident ESRD patients; Whereas the DOPPS enrolled all eligible patients with newly created vascular access, including those with previous permanent accesses. The rate of incident ESRD patients in AVF and AVG groups in DOPPS study were 46.4% and 32.5%, respectively. DOPPS revealed higher numbers of previous access is a risk factor for vascular access failure, which may indicate that long-term dialysis provokes atherosclerosis and arteriosclerosis and overwhelms the effect of vascular access protection of ARB.
Our study also revealed a significant relationship between CCB and prolongation of primary patency in both AVF and AVG group. Animal [18] and human [25] studies had proved that CCB could inhibit vascular neointimal hyperplasia, which is a major characteristic of vascular access stenosis. In clinical studies, CCB was associated with increasing maturation rate of newly created AVF [16]. Doi et al also reported that CCB significantly decreased restenosis rate of AVF after percutaneous transluminal angioplasty [24]. Although this effect was not significant in their AVG group, which may be ascribed to a relatively small number of subjects, there was a trend toward benefit. DOPPS study showed that CCB was associated with increased primary patency rate of AVG, but not AVF.
Our study had several limitations. First, the definition of users of the specified anti-hypertensive agent were those who had used this specified medicine for more than 3 months after the creation of their first AVF or AVG. Some patients who used the medicine for a period shorter than 3 months would be classified as non-users, and those who classified as users may have poor drug compliance. These may weaken the relationship between these medications and vascular access patency in the analysis. Second, this is a retrospective observational study, we could find the relationship between medications and vascular access patency, but the causality cannot be proved. Third, the study is based on NHI claim database, thus some factors, including patient’s laboratory data, smoking history, the control of blood pressure, severity of comorbid diseases, and the location of AVFs or AVGs, could not be identified. The control of blood pressure is of especial importance because ACEI, ARB, and CCB are anti-hypertensive agents. Although ACEI, ARB, and CCB were still significantly associated with increased primary patency after adjusting hypertension in multivariate analysis, poor control of blood pressure may still interfere with the result. Fourth, the original indications of these medications should be mostly used for control of blood pressure rather than prevention of vascular access dysfunction. Whether the study results could be extrapolated to normotensive or hypotensive patients still remains to be determined.
There were also some notable points of our study. Our claim database derived from a nationwide, universal coverage health system, which diminished the possibility of selection bias and provided a considerable amount of eligible subjects. Besides, although randomized, placebo-controlled trials provide evidence of highest level for medical practice. Sometimes it might be limited by ethical problems. In our study, medications such as ACE-I, ARB, and CCB had been proved for its cardioprotective effect in patients undergoing dialysis, which makes it difficult to prohibit their use in a randomized controlled study. Our database study in nature obviated this problem and could provide information for the design of further randomized controlled trials.
In conclusion, our study suggests that ACE-I, ARB, and CCB are associated with increased primary patency of first created AVF and AVG. This large observational, nationwide claim database study may be helpful in clinical practice for patient with newly created vascular access and also serves as a guide for further prospective, randomized, controlled studies.
Acknowledgments
We are grateful to all research staffs participated in this study.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by intramural grants (V100C1-050, V101C-188, V102C-060, V102E2-001, V103C-043, V104C-026, V105C-075) from Taipei Veterans General Hospital, and grants from the National Science Council (NSC101-2314-B-010-024-MY3) and the Ministry of Science and Technology (MOST 104-2314-B-010 -032 -MY3) in Taiwan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wasse H, Kutner N, Zhang R, Huang Y. Association of initial hemodialysis vascular access with patient-reported health status and quality of life. Clin J Am Soc Nephrol 2007; 2(4):708–14. 10.2215/CJN.00170107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J. Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 2005; 16(5):1449–55. 10.1681/ASN.2004090748 [DOI] [PubMed] [Google Scholar]
- 3.Ravani P, Palmer SC, Oliver MJ, Quinn RR, MacRae JM, Tai DJ, et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol 2013; 24(3):465–73. 10.1681/ASN.2012070643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ocak G, Rotmans JI, Vossen CY, Rosendaal FR, Krediet RT, Boeschoten EW, et al. Type of arteriovenous vascular access and association with patency and mortality. BMC Nephrol 2013; 14:79 10.1186/1471-2369-14-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng LJ, Chen F, Pisoni RL, Krishnan M, Mapes D, Keen M, et al. Hospitalization risks related to vascular access type among incident US hemodialysis patients. Nephrol Dial Transplant 2011; 26(11):3659–66. 10.1093/ndt/gfr063 [DOI] [PubMed] [Google Scholar]
- 6.USRDS. United States Renal Data System, 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2014.
- 7.Mihmanli I, Besirli K, Kurugoglu S, Atakir K, Haider S, Ogut G, et al. Cephalic vein and hemodialysis fistula: surgeon's observation versus color Doppler ultrasonographic findings. J Ultrasound Med 2001; 20(3):217–22. [DOI] [PubMed] [Google Scholar]
- 8.Hung YN, Ko PJ, Ng YY, Wu SC. The longevity of arteriovenous graft for hemodialysis patients—externally supported or nonsupported. Clin J Am Soc Nephrol 2010; 5(6):1029–35. 10.2215/CJN.08181109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolmatch BL. Stent graft versus balloon angioplasty for failing dialysis access grafts: a long-awaited advance in the treatment of permanent hemodialysis access. J Vasc Access 2010; 11(2):89–91. [DOI] [PubMed] [Google Scholar]
- 10.Haskal ZJ, Trerotola S, Dolmatch B, Schuman E, Altman S, Mietling S, et al. Stent graft versus balloon angioplasty for failing dialysis-access grafts. N Engl J Med 2010; 362(6):494–503. 10.1056/NEJMoa0902045 [DOI] [PubMed] [Google Scholar]
- 11.Lin CC, Chang CF, Lai MY, Chen TW, Lee PC, Yang WC. Far-infrared therapy: a novel treatment to improve access blood flow and unassisted patency of arteriovenous fistula in hemodialysis patients. J Am Soc Nephrol 2007; 18(3):985–92. 10.1681/ASN.2006050534 [DOI] [PubMed] [Google Scholar]
- 12.Jackson RS, Sidawy AN, Amdur RL, Khetarpal A, Macsata RA. Angiotensin receptor blockers and antiplatelet agents are associated with improved primary patency after arteriovenous hemodialysis access placement. J Vasc Surg 2011; 54(6):1706–12. 10.1016/j.jvs.2011.06.028 [DOI] [PubMed] [Google Scholar]
- 13.Saran R, Dykstra DM, Wolfe RA, Gillespie B, Held PJ, Young EW. Association between vascular access failure and the use of specific drugs: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis 2002; 40(6):1255–63. 10.1053/ajkd.2002.36895 [DOI] [PubMed] [Google Scholar]
- 14.Dixon BS, Beck GJ, Vazquez MA, Greenberg A, Delmez JA, Allon M, et al. Effect of dipyridamole plus aspirin on hemodialysis graft patency. N Engl J Med 2009; 360(21):2191–201. 10.1056/NEJMoa0805840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osborn G, Escofet X, Da Silva A. Medical adjuvant treatment to increase patency of arteriovenous fistulae and grafts. Cochrane Database Syst Rev 2008; (4):CD002786 10.1002/14651858.CD002786.pub2 [DOI] [PubMed] [Google Scholar]
- 16.Bashar K, Zafar A, Elsheikh S, Healy DA, Clarke-Moloney M, Casserly L, et al. Predictive parameters of arteriovenous fistula functional maturation in a population of patients with end-stage renal disease. PLoS One 2015; 10(3):e0119958 10.1371/journal.pone.0119958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brauner R, Laks H, Drinkwater DC Jr., Chaudhuri G, Shvarts O, Drake T, et al. Controlled periadventitial administration of verapamil inhibits neointimal smooth muscle cell proliferation and ameliorates vasomotor abnormalities in experimental vein bypass grafts. J Thorac Cardiovasc Surg 1997; 114(1):53–63. 10.1016/S0022-5223(97)70117-X [DOI] [PubMed] [Google Scholar]
- 18.Huang P, Hawthorne WJ, Peng A, Angeli GL, Medbury HJ, Fletcher JP. Calcium channel antagonist verapamil inhibits neointimal formation and enhances apoptosis in a vascular graft model. Am J Surg 2001; 181(6):492–8. [DOI] [PubMed] [Google Scholar]
- 19.Yamada T, Kondo T, Numaguchi Y, Tsuzuki M, Matsubara T, Manabe I, et al. Angiotensin II receptor blocker inhibits neointimal hyperplasia through regulation of smooth muscle-like progenitor cells. Arterioscler Thromb Vasc Biol 2007; 27(11):2363–9. 10.1161/ATVBAHA.107.147124 [DOI] [PubMed] [Google Scholar]
- 20.O'Donohoe MK, Schwartz LB, Radic ZS, Mikat EM, McCann RL, Hagen PO. Chronic ACE inhibition reduces intimal hyperplasia in experimental vein grafts. Ann Surg 1991; 214(6):727–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yagi S, Morita T, Katayama S. Combined treatment with an AT1 receptor blocker and angiotensin converting enzyme inhibitor has an additive effect on inhibiting neointima formation via improvement of nitric oxide production and suppression of oxidative stress. Hypertens Res 2004; 27(2):129–35. [DOI] [PubMed] [Google Scholar]
- 22.Sajgure A, Choudhury A, Ahmed Z, Choudhury D. Angiotensin converting enzyme inhibitors maintain polytetrafluroethylene graft patency. Nephrol Dial Transplant 2007; 22(5):1390–8. 10.1093/ndt/gfl821 [DOI] [PubMed] [Google Scholar]
- 23.Gradzki R, Dhingra RK, Port FK, Roys E, Weitzel WF, Messana JM. Use of ACE inhibitors is associated with prolonged survival of arteriovenous grafts. Am J Kidney Dis 2001; 38(6):1240–4. 10.1053/ajkd.2001.29220 [DOI] [PubMed] [Google Scholar]
- 24.Doi S, Masaki T, Shigemoto K, Harada S, Yorioka N. Calcium channel antagonists reduce restenosis after percutaneous transluminal angioplasty of an arteriovenous fistula in hemodialysis patients. Ther Apher Dial 2008; 12(3):232–6. 10.1111/j.1744-9987.2008.00579.x [DOI] [PubMed] [Google Scholar]
- 25.Taber TE, Maikranz PS, Haag BW, Gaylord GM, Dilley RS, Ehrman KO, et al. Maintenance of adequate hemodialysis access. Prevention of neointimal hyperplasia. ASAIO J 1995; 41(4):842–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.