Abstract
Sleepwalking is thought to be a common arousal disorder; however, the epidemiology of this disorder has not yet been systematically examined. A systematic search of MEDLINE, CINAHL, EMBASE, PsycINFO, PubMed, and ScienceDirect was conducted for ‘sleepwalking’ OR ‘somnambulism’ in any field, to identify studies that reported the epidemiology of sleepwalking or sleepwalking disorders. Fifty-one studies assessed the prevalence rates of sleepwalking in a total sample of 100 490. The meta-analysis showed the estimated lifetime prevalence of sleepwalking was 6.9% (95% CI 4.6%–10.3%). The current prevalence rate of sleepwalking—within the last 12 months—was significantly higher in children 5.0% (95% CI 3.8%–6.5%) than adults 1.5% (95% CI 1.0%–2.3%). There was no evidence of developmental trends in sleepwalking across childhood. The significant risk of bias across all studies suggests these results should be used cautiously. Further epidemiological research that addresses methodological problems found in studies of sleepwalking to date is needed.
Introduction
Sleepwalking is a behavior characterized by partial arousal during slow wave sleep (N4) [1]. The potential adverse health outcomes of sleepwalking are injury to the sleepwalker themselves or to others as a result of impaired perception, characteristic of sleepwalking. The most sensationalized of these adverse events come to the public’s attention (e.g.[2]), otherwise sleepwalking largely goes unnoticed and may not get routinely reported to any health service. An absence of sleepwalking being recorded as a cause of significant injury requiring hospitalization or death (e.g.[3, 4–6]) may be: 1) indicative of very low prevalence rates of sleepwalking; 2) a reflection of the low rates of adverse events from sleepwalking; and/or 3) represent inadequate identification, reporting, or assessment of sleepwalking as the cause of injuries. Understanding the epidemiology of sleepwalking is important to public health, individual decision-making and clinical management. It can inform optimal allocation of health resources for this largely neglected behavior. General population screening is needed to understand the potential health implications [7].
Challenges in epidemiological research for sleepwalking
The definition of sleepwalking varies considerably within the literature. The behavioral event is similar to the proverbial tree falling in the forest—if it is not observed, did it make a noise? Studies of children frequently rely on observation, typically using parent-report that their child sleepwalks, as the operationalization of sleepwalking. This reduces prevalence rates to those where the child captures the parents attention (e.g. such as by leaving their bedroom), are observed by parents, and the episode is later recalled by the parent. Some studies with older children use self-report, as do studies with adults. These are used to obtain lifetime and point prevalence rates, despite amnesia for the event being a common feature of the behavior. The classification of sleepwalking as a disorder rather than just a behavior, requires recurrent episodes, contact with others during the event, and amnesia for the event [8]. The American Psychiatric Association classifies sleepwalking as a mental illness if, in addition to the ICD-10 CM [8] characteristics, the events cause clinically significant distress or impairment in social, occupational or other important areas of functioning [9]. The increasing complexity of the definitions would be expected to result in decreasing prevalence rates, with sleepwalking behavior being the more prevalent and the mental illness of sleepwalking least likely to occur.
These differing levels of operationalizing sleepwalking necessarily result in different measurement strategies. Polysomnography (PSG) is the only measure that can accurately confirm the neurological event of sleepwalking—demonstrated by ambulant behavior during a maintained sleep state. However, PSG can be impractical to do on a large scale and may miss sleepwalking episodes that are usually infrequent. Fallible measures of sleepwalking include actigraphy, video monitoring, direct observation, self-report, and significant other report. Actigraphy is sensitive in detecting unique sleep patterns associated with specific sleep disorders [10]. It can provide an objective measure of sleep fragmentation due to movement, as a proxy measure of nocturnal wandering. Immediate parent-report relies on the child being observable to parents. Self-report relies on at least partial awareness of the event by the individual, or being told about their sleepwalking by someone who has observed it. Given that amnesia is a common feature of sleepwalking, sleepwalkers who are observed (e.g. children) would be more likely to be aware of sleepwalking than those who live alone. This most likely explains higher rates of sleepwalking in adults who are married compared with those who are single [11].
Retrospective recall is reliant on encoding the event as significant and long-term recall of the episode [12]. Distinctively different sleepwalking experiences would be more likely to be remembered by both sleepwalkers and their family members [13]. The distinctiveness of the episode constrains processing at the time of recall and thus reduces the incidence of false recall [14]. The measurement of the incidence of sleepwalking is likely to be more accurate than period prevalence, as a new experience of sleepwalking would be more distinctive to both parents/significant others and sleepwalkers than historical occurrences. Self-report could be based on memory for the event, distinctive features of an event such as injury or waking somewhere unusual, or reliant on what others have told the sleepwalker—each contains inherent measurement error. There is also the potential that individuals and observers could incorrectly classify all nocturnal wandering as sleepwalking.
Partially validated datasets are recommended in cases where the outcome variable is difficult or costly to measure [15], as in the case of sleepwalking. This involves all data points being classified by fallible tests and some of the data points being validated by also being classified by an accurate gold-standard test. To accurately assess the prevalence of sleepwalking, this would involve all participants being classified by fallible tests (such as self-, and parent-reports, actigraphy, or video monitoring) and some data points being validated by polysomnography. A partially validated dataset enables the systematic error that is included in each fallible measure to be quantified and taken into account in determining the true prevalence of sleepwalking.
Prevalence rates of sleepwalking frequented quoted in the literature typically relate to a single study (e.g. [16] or provide no reference at all e.g. [17, 18]). The operationalization of sleepwalking is rarely mentioned. By combining studies, taking into account the differing conceptualization and measurement of sleepwalking and assigning the individual studies different weights according to their sample size, the potentially troublesome role of individual studies is minimized. The aim of this study is to systematically examine the epidemiology of sleepwalking in general population samples of children and adults.
Method
This study was registered with PROSPERO (#CRD42016036296). PRISMA guidelines were followed in conducting and reporting the results of this systematic review and meta-analysis [19].
Search strategy
The following databases were included in the identification of relevant studies: MEDLINE, CINAHL, EMBASE, PsycINFO, PubMed, and ScienceDirect. Search terms were ‘sleepwalking’ OR ‘somnambulism’ in any field (e.g. PubMed search terms (sleepwalk*) OR somnambulism). The combined lists were screened for relevant titles and abstracts and full texts of all potentially relevant titles were examined. Studies were included if: 1) they reported the prevalence or incidence of sleepwalking; and 2) they were submitted to a peer-reviewed publication. All ages were included. The search was conducted in English; however, studies identified in other languages were included. Studies were excluded if: a) sleepwalking incidence or prevalence was not reported separately from other sleep disorders; b) participants were forensic cases or sleep-clinic samples; c) the study included drug-induced sleepwalking; or d) adults participants were psychiatric patients. Adult psychiatric patients were excluded because sleepwalking has been identified as a potential side-effect of psychotropic medications [20]. We identified other pertinent studies through citation tracking, review of reference lists in retrieved articles, Google Scholar, and our knowledge of the literature. The searches were from the beginning of each database through to 15 March 2016. All initial searches were conducted by the first author. The articles were then independently examined by the second author—there were no disagreements between authors.
Data extraction
Data were extracted independently by both authors. For each paper, we documented authors, year, country, study design (e.g. cross-sectional, longitudinal), setting (e.g. school, general population), participants (e.g. adults, children), sample size, response rate, age range, data collection procedure, sleepwalking measure, and results.
Data evaluation
We applied published guidelines for evaluating prevalence studies [21], using eight critical appraisal criteria across three domains, sampling, measurement, and data analysis. These are consistent with STROBE guidelines for the reporting observational studies in epidemiology [22]. Sampling items assessed whether the survey design yielded a sample of respondents’ representative of a defined target population. The items were whether: 1) the target population was clearly defined; 2) probability sampling was used to identify potential respondents; and 3) the characteristics of the respondents matched the target population. Measurement items assessed whether survey instruments yielded reliable and valid measures of sleepwalking. The items were whether: 4) the data collection methods were standardized; 5) the instruments were reliable; and 6) the instruments were valid. Data analysis assessed whether special features of the sampling design were accounted for in the analysis (Criterion 7). Confidence intervals, essential to produce frequency estimates within the population overall, were calculated for each study (Criterion 8). Evaluations was conducted independently by each author.
Analyses
The prevalence of sleepwalking was calculated for each study with the number of reported sleepwalkers in the sample as the numerator and the total sample size as the denominator. All rates were calculated as the rate of sleepwalkers per 100 people, with the total sample being the summation of sleepwalker and non-sleepwalkers. An aggregate effect size, weighted by sample size, was computed to provide an overall effect size across the studies to identify the lifetime and current prevalence rates in children and adults. A random-effects model was used to aggregate individual effect sizes to create a pooled prevalence of sleepwalking. Random-effects models are based on the assumption that the true effect could vary between studies [23].
Homogeneity across studies was tested with the I2 index, which provides the percentage of variation in prevalence attributable to between-study heterogeneity. An I2 value of >75% is interpreted as high heterogeneity [24]. Post-hoc sensitivity analyses were conducted for the different study populations (child and adult) and measures (sleepwalking behavior and sleepwalking diagnoses) to investigate possible sources of heterogeneity. A forest plot was created to illustrate the prevalence of each study or current and lifetime sleepwalking, with 95% confidence intervals that contributed to the analysis along with the pooled prevalence estimate. Meta-regression was used to identify any developmental trends in current sleepwalking rates across childhood. Funnel plots [25] and Egger’s test of asymmetry [26] were used to formally detect bias within the results. All analyses were performed with Comprehensive Meta-Analysis Version 3 [27].
Description of studies
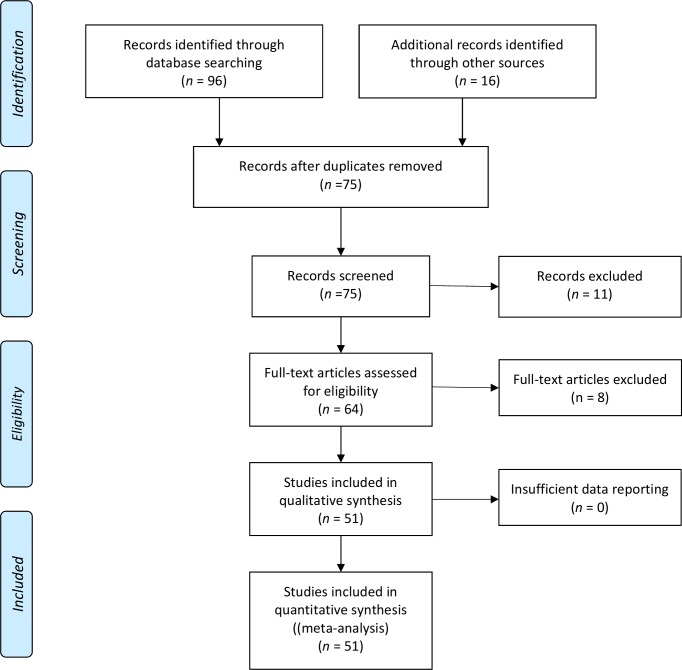
A total of 801 hits were produced in the database search. Review of titles resulted in 96 potentially relevant papers that were reviewed. Fig 1 displays the flow of information through the different phases of the systematic review and meta-analysis. From the original 64 sourced papers, 56 papers describing 51 studies met the inclusion criteria and were subsequently included for review. The eight full-text papers that were excluded were for the following reasons: not an empirical study (n = 1), not a general population sample (n = 5), not measuring sleepwalking epidemiology (n = 1), and not reporting sleepwalking separately from other sleep problems (n = 1).
Fig 1. PRISMA flow of information through the different phases of the systematic review.
A summary of the participant characteristics from the included studies is shown in Tables 1 and 2. They span more than seven decades of research and include 20 countries—representing an international and cross-cultural sample. There were 15 studies of adults comprising 31 108 participants and 36 pediatric samples comprising 69 382 children. Sample sizes ranged from 100 to 15 929 participants. All used an observational study design using questionnaires or interviews. The majority of studies measured sleepwalking behavior (n = 43). Eight studies measured sleepwalking using a diagnosis—five using DSM-IV [28] and three ICSD [29]. Several studies reported assessing ICD [30] and DSM diagnoses; however, as DSM has an additional criterion compared with ICD, that is ‘episodes cause clinically significant distress or impairment’ ([9]; p. 399) and only one result is reported in all studies, it is assumed the result refers to DSM. With child samples, six used child self-report and 26 used parent-report of sleepwalking behavior. Where children were asked to complete questionnaires with their parents, the results are included as parent-report.
Table 1. Characteristics of Included Studies of Children listed by Measurement Type.
| Citation | Country | Design | Age Range | N | Response Rate % | Prevalence Outcomes | Criteria | Results % |
|---|---|---|---|---|---|---|---|---|
| Self-reported behavior | ||||||||
| Abdel-Khalek [37] | Kuwait | Cross-sectional | 14–18 | 2574 | ns | 1 month | ‘much’ and ‘very much’ response on 5-point scale (no, a little, moderate, much, very much) | 10.0 |
| Ghalebandi et al [38] | Iran | Cross-sectional | 5–10+ | 4309 | 71.82 | ns | ‘almost always’ and ‘frequently’ response on 5-point scale (almost always, frequently, occasionally, rarely, never) | 0.39 |
| Ipsiroglu et al [39] | Austria | Cross-sectional | 10–15 | 332 | 99.70 | Lifetime | ‘very often’ and ‘occasionally’ on 3-point scale (never, occasionally, very often) | 15.10 |
| Stallman et al [40] | Australia | Cross-sectional | 17–18 | 532 | ns | 1 month | How frequently in previous month not during the past month’, ‘less than once a week’, ‘once or twice a week’, ‘three or more times a week’ | 2.90 |
| Wiechers et al [31] | Germany | Cross-sectional | M = 9.6 | 1144 | 65.00 | Current | ‘sometimes’ or ‘often’ on 3-point scale (never/rarely, sometimes, often) | 4.80 |
| Yang et al [41] | China | Cross-sectional | 12–18 | 846 | ns | 6 months | At least one experience | 4.00 |
| Parent-reported behavior | ||||||||
| Abe [42] | Japan | Cross-sectional | 3 | 342 | 55.97 | Lifetime | Yes/no | 4.58 |
| Abe et al [43] | Japan | Longitudinal | 8 | 363 | 50.14 | Lifetime | ns | 4.13 |
| Agargun et al [44] | Turkey | Cross-sectional | 7–11 | 971 | 86.60 | 6 months | ‘frequently/always’ response on 4-point scale (never, rarely, occasionally, frequently/always) | 1.2 |
| Archbold et al [45] | USA | Cross-sectional | 2–14 | 1038 | 74.14 | Lifetime | Yes/no | 14.8 |
| Bharti et al [46] | India | Cross-sectional | 3–10 | 103 | ns | ns | ns | 1.90 |
| Blader et al [47] | USA | Cross-sectional | 5–12 | 987 | 59.82 | 6 months | Any response greater than ‘none’ on 4-point scale (none, <1 night per month, 1–2 nights per week, >3 nights per week) | 9.80 |
| Buhler & Largo [48] | Switzerland | Cross-sectional | 6–18 | 320 | ns | Lifetime | ns | 5.00 |
| Cai et al [49] | China | Cross-sectional | 2–12 | 3756 | ns | Lifetime | ns | 0.90 |
| Fisher & Wilson [50] | Canada | Cross-sectional | 5–18 | 1695 | 40.03 | 12 months | “At least once” | 21.00 |
| Current | “Still sleepwalking” | 14.00 | ||||||
| Goodwin et al [51] a Furet et al [52] | USA | Longitudinal | 6–11 | 480 | 6.80 | Current | more than three times/month on 4-point scale (Never, less than three times per month, three to five times per month, or more than five times per month) | 3.50 |
| 9–17 | 350 | 4.96 | 1 month | 1.40 | ||||
| Greene et al [53] | UK | Longitudinal | 5 | 7830 | 45.53 | Lifetime | ‘mild’ and ‘severe’ response on 3-point scale (non, mild, severe) | 24.19 |
| Kilincaslan et al [32] | Turkey | Cross-sectional | M = 16.09 | 3485 | 92.20 | 6 months | Above median number of occurrences in cohort | 5.70 |
| Klackenberg [54–56] | Sweden | Longitudinal | 8 16 | 194 180 | 97.34 85.00 | Lifetime | ‘seldom’ response or more on 5-point scale (never, seldom, sometimes, often, always) | 6.29 40.0 |
| Laberge [57] | Canada | Longitudinal | 13 | 1353 | 67.65 | Lifetime | Presence of sleepwalking | 5.80 |
| Lehmkuhl et al [58] | Germany | Cross-sectional | M = 5.52 | 4793 | 28.9653.30 | Current | ‘sometimes’ or ‘often’ response on 3-point scale (never, sometimes, often) | 3.3 |
| Liu et al [59] | China | Cross-sectional | 7–13 | 517 | 91.50 | 1 week | Yes/no | 6.00 |
| Liu et al [60] | China | Cross-sectional | 2–12 | 5979 | 90.59 | 6 months | Yes/no | 0.60 |
| Neveus et al [33] | Sweden | Cross-sectional | 6–11 | 1413 | 74.00 | Current | At least once per month or more on 5-point scale (daily, every week, every month, less than monthly, at an earlier age) | 7.20 |
| Petit et al [61, 62] | Canada | Longitudinal | 2–6 13 | 14921011 | 55.77 37.79 | 12 months | ‘sometimes’ or ‘frequently’ response on 4-point scale (never, seldom, sometimes, frequently) | 14.50 12.80 |
| Simonds & Parraga [63] | USA | Cross-sectional | 5–18 | 309 | 83.74 | 6 months | At least one episode | 10.03 |
| Smedje et al [64, 65] | Sweden | Longitudinal | 5–7 6–8 | 1844635 | 83.25 34.44 | 6 months | Any response greater than ‘never’ on 5-point scale (never, occasionally, once or twice per week, 3 or 4 days per week, at least 5 days per week) | 8.30 |
| Stallman et al [66] | Australia | Cross-sectional | 5–10 | 1814 | 25.2 | 1 week | at least once; 4-point scale (never, rarely, sometimes, usually | 10.5 |
| Steinsbekk et al [67, 68] | Norway | Longitudinal | 4 | 995 | 79.60 | 3 months | Anders criteria[69] | 0.70 |
| 6 | 795 | 63.60 | 3.50 | |||||
| Tomás Vila et al [70] | Spain | Cross-sectional | 6–17 | 887 | 68.75 | Lifetime | Yes/no | 12.50 |
| Vaher et al [71] | Estonia | Cross-sectional | 8–9 | 703 | 66.00 | Current6 months | Yes/no | 28.59 |
| Wiechers et al [31] | Germany | Cross-sectional | M = 9.6 | 1144 | 65.00 | Current | ‘sometimes’ or ‘often’ on 3-point scale (never/rarely, sometimes, often) | 9.20 |
| Xiong et al [72] | China | Cross-sectional | b | 2848 | b | b | b | 2.84 |
| Diagnosis | ||||||||
| Fisher et al [73] | UK | Longitudinal | 12 | 6796 | 46.23 | 6 months | DSM-IV | 12.55 |
| Ozgun, et al [74] | Turkey | Cross-sectional | 6–18 | 4144 | 83.7 | Current | ICSD-2 | 4.20 |
| Ramírez et al [75] | Columbia | Cross-sectional | 5–12 | 296 | 91.60 | ns | DSM-IV | 7.40 |
| Shang et al [76] | Taiwan | Cross-sectional | 4–9 | 1391 | 91.60 | Lifetime | Yes/no DSM-IV | 8.60 |
| 1 month | 1.00 | |||||||
ns = not specified
aexact data reported in a second paper is not included in this paper
bfull paper not accessible
Table 2. Characteristics of Included Studies of Adults listed by Measurement Type.
| Citation | Country | Design | Age | N | Response Rate % | Prevalence Outcomes | Results % | |
|---|---|---|---|---|---|---|---|---|
| Self-reported behaviour | ||||||||
| Bixler et al [77] | USA | Cross-sectional | 18–80 | 1006 | ns | Lifetime | Yes/no | 2.5 |
| Current | 0.4 | |||||||
| Bjorvatn et al [78] | Norway | Cross-sectional | 18–96 | 1000 | 25.38 | Lifetime | At least once during past 3 months from 6-point scale (never, less than once per month, less than once per week, 1–2 days per week, 3–5 days per week, daily/almost daily) | 22.40 |
| 3 month | 1.70 | |||||||
| Davis [79] | England | Cross-sectional | ns | 100 | ns | Lifetime | Yes/no | 3.0 |
| Hirotsu et al [80] | Brazil | Cross-sectional | 16–60+ | 2017 | 99.95 | Current | Yes/no | 1.00 |
| Mume [11] | Nigeria | Cross-sectional | 18–60 | 228 | 91.20 | Lifetime | Yes/no | 7.00 |
| Orme [81] | UK | Cross-sectional | ns | 151 | ns | Lifetime | Yes/no | 13.91 |
| Panda et al.[82] | India | Cross-sectional | 16–55 | 1050 | >95 | 1 month | ns | .60 |
| Stepansky et al [83] | Austria | Cross-sectional | ns | 1000 | ns | ns | ns | .004 |
| Thomas & Pederson [84] | USA | Cross-sectional | 19–34+ | 1116 | 88.35 | Current | ns | 2.24 |
| Vela-Bueno et al [85] | Spain | Cross-sectional | 18–65+ | 1131 | 75.40 | Lifetime | Yes/no | 1.10 |
| Zeitlhofer et al (2010) | Austria | Cross-sectional | 14 = 50+ | 1000 | 82.10 | Current | ns | 2.00 |
| Diagnosis | ||||||||
| Frauscher et al [86] | Austria | Cross-sectional | 19–77 | 100 | 27.50 | Lifetime | non-bothersome sleepwalking < 2 times per week ICSD-2 | 12 |
| Oluwole [87] | Nigeria | Cross-sectional | 19–35 | 276 | 30.84 | Lifetime | Yes/no ICSD | 4.35 |
| 2 weeks | 1.45 | |||||||
| Ohayon [88] | UK | Cross-sectional | 15–100 | 4972 | 79.60 | Current | DSM-IV | 2.00 |
| Ohayon et al [89] | USA | Cross-sectional | 18–102 | 15 929 | 83.2 | 12 months | DSM-IV | 3.6 |
| Childhood | 25.7 | |||||||
Risk of bias
The risk of bias analyses are presented in Table 3. There were no studies without risk of bias and all failed to control for bias across multiple criterion.
Table 3. Summary of Risk of Bias in Included Studies.
| Target Population | Probability sampling | Selection bias | Standardized data collection | Measurement Reliability | Measurement Validity | Analyses accounts for sampling design | Period Assessed | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Abdel-Khalek (2001) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | Current | 8.9–11.2 |
| Agargun et al (2004) | 0 | 0 | 2 | 0 | 1 | 1 | 1 | Current | 0.6–2.0 |
| Bharti et al (2006) | 0 | 1 | 2 | 0 | 1 | 1 | 1 | Current | 0.5–7.4 |
| Bixler et al (1979) | 0 | 0 | 2 | 0 | 1 | 1 | 1 | Current | 0.2–1.1 |
| Lifetime | 1.7–3.7 | ||||||||
| Bjorvatn et al (2010) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 4.7–9.2 |
| Lifetime | 19.9–25.1 | ||||||||
| Blader et al (1997) | 0 | 2 | 1 | 0 | 1 | 1 | 1 | Current | 8.1–11.8 |
| Cai et al (2008) | 0 | 2 | 2 | 2 | 1 | 1 | 2 | Current | 0.6–1.3 |
| Fisher & Wilson (1987) | 0 | 0 | 1 | 1 | 1 | 1 | 1 | Current | 19.1–23.0 |
| Fisher et al (2014) | 0 | 0 | 1 | 1 | 1 | 1 | 1 | Current | 11.8–13.4 |
| Furet et al (2011) | 0 | 2 | 2 | 2 | 1 | 1 | 2 | Current | 0.06–3.3 |
| Ghalebandi et al (2011) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 3.4–4.5 |
| Goodwin et al (2012) | 0 | 2 | 2 | 2 | 1 | 1 | 2 | Current | 2.2–5.6 |
| Hirotsu (2014) | 0 | 0 | 1 | 0 | 1 | 1 | 0 | Current | .06–1.5 |
| Kilincaslan et al (2014) | 0 | 0 | 1 | 2 | 1 | 1 | 0 | Current | 5.0–6.5 |
| Lehmkuhl et al (2008) | 0 | 0 | 1 | 0 | 1 | 1 | 1 | Current | 2.8–3.8 |
| Lui (2003) | 0 | 0 | 0 | 2 | 1 | 1 | 0 | Current | 4.3–8.4 |
| Lui (2005) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 0.4–0.8 |
| Mume (2010) | 0 | 0 | 0 | 2 | 1 | 1 | 1 | Current | 6.7–7.3 |
| Neveus et al (2001) | 0 | 0 | 0 | 2 | 1 | 1 | 1 | Current | 6.1–8.4 |
| Ohayon et al (1999) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 1.6–2.4 |
| Ohayon et al (2012) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 3.3–3.9 |
| Lifetime | 25.0–26.4 | ||||||||
| Ozgun et al (2013) | 0 | 2 | 0 | 2 | 1 | 1 | 1 | Current | 3.6–4.9 |
| Panda (2012) | 0 | 1 | 2 | 0 | 1 | 1 | 1 | Current | 0.3–1.3 |
| Ramírez et al (2008) | 0 | 2 | 2 | 2 | 1 | 1 | 2 | Current | 4.9–11.0 |
| Shang et al (2006) | 0 | 0 | 1 | 0 | 1 | 1 | 1 | Current | .06–1.7 |
| Lifetime | 7.2–10.2 | ||||||||
| Simonds & Parraga (1982) | 0 | 2 | 1 | 2 | 1 | 1 | 1 | Current | 7.6–14.6 |
| Smedje et al (1999; 2001) | 0 | 0 | 1 | 2 | 1 | 1 | 1 | Current | 7.1–9.6 |
| Stallman et al (2016b) | 0 | 0 | 2 | 0 | 1 | 1 | 2 | Current | 9.2–12.0 |
| Stallman et al (2016a) | 0 | 0 | 0 | 0 | 1 | 1 | 1 | Current | 1.8–4.7 |
| Steinsbekk et al (2013, 2015) | 0 | 1 | 1 | 0 | 1 | 1 | 0 | Current | 0.3–1.5 |
| Current | 2.4–5.0 | ||||||||
| Stepansky et al (1999) | 0 | 0 | 2 | 2 | 1 | 1 | 2 | ns | 0–100 |
| Thomas & Pederson (1963) | 0 | 1 | 0 | 0 | 1 | 1 | 1 | Current | 1.6–3.4 |
| Tomás Vila et al (2008) | 0 | 0 | 1 | 2 | 1 | 1 | 2 | Current | 10.5–14.8 |
| Vaher et al (2013) | 1 | 2 | 2 | 0 | 1 | 1 | 1 | Current | 25.4–32.0 |
| Wiechers et al (2011) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 7.7–11.0 |
| Xiong et al (2008) | 0 | 0 | 2 | 2 | 1 | 1 | 2 | Current | 2.3–3.5 |
| Yang et al (1987) | 0 | 1 | 2 | 2 | 1 | 1 | 1 | Current | 2.9–5.6 |
| Zeitlhofer et al (2010) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Current | 7.5–8.0 |
| Abe (1966) | 0 | 0 | 2 | 0 | 1 | 1 | 1 | Lifetime | 2.8–6 |
| Abe et al (1982) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | Lifetime | 2.9–7.3 |
| Archbold et al (2002) | 1 | 1 | 0 | 0 | 1 | 1 | 1 | Lifetime | 12.8–17.1 |
| Buhler (1981) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | Lifetime | 3.1–8.0 |
| Davis (1942) | 1 | 1 | 2 | 2 | 1 | 1 | 1 | Lifetime | 1.0–8.9 |
| Frauscher et al (2014) | 0 | 0 | 2 | 0 | 1 | 1 | 2 | Lifetime | 35.1–36.9 |
| Greene et al (2015) | 0 | 1 | 1 | 0 | 1 | 1 | 1 | Lifetime | 22.3–25.2 |
| Ipsiroglu et al (2002) | 0 | 1 | 2 | 0 | 1 | 1 | 0 | Lifetime | 11.6–19.4 |
| Klackenberg (1971, 1982, 1987) | 0 | 2 | 2 | 1 | 1 | 1 | 1 | Lifetime | 33.1–47.3 |
| Laberge et al (2000) | 0 | 0 | 1 | 2 | 1 | 1 | 1 | Lifetime | 4.7–7.2 |
| Oluwole (2010) | 0 | 1 | 2 | 2 | 1 | 1 | 1 | Lifetime | 1.1–5.5 |
| Orme (1967) | 1 | 1 | 2 | 2 | 1 | 1 | 1 | Lifetime | 9.2–20.4 |
| Petit et al (2007, 2015) | 0 | 0 | 1 | 0 | 1 | 1 | 0 | Lifetime | 12.8–16.4 |
| Vela-Bueno et al (1999) | 2 | 2 | 1 | 2 | 1 | 1 | 2 | Lifetime | 0.6–1.9 |
Note. 0 = no risk of bias
1 = risk of bias
2 = unclear risk of bias
ns = not specified
Sampling
Criterion 1—Target population clearly defined: The majority of studies defined their target population (n = 44), six had risk of bias and one was unclear. Criterion 2 -Probability sampling used to identify potential respondents: More than half of the studies used probability sampling (n = 30), 12 had clear risk of bias, and 9 had an unclear risk. Criterion 3—Representativeness of the sample: There was significant heterogeneity in regards to how representative the samples were. For studies that reported or provided data to calculate response rates (n = 44), they ranged from 4.96% to 99.95%. Twenty-three studies met the minimum criteria of 70% response rate to be considered representative of the population [21]. Overall, only 15 papers had no risk of bias for sampling, 17 had risk of bias and 19 had unclear risk.
Measurement
Criterion 4—Standardized data collection procedures: More than half of the studies had no risk of bias related to data collection procedures (n = 29), three had risk of bias, 19 had unclear risk. Criterion 5—Reliable measurement: No studies reported the reliability of the measure they used to assess sleepwalking. Criterion 6—Valid measurement: No measures of sleepwalking used in any study have been validated. Measurement of sleepwalking varied considerably between studies. All studies used interview or questionnaires to measure sleepwalking—no studies included objective measures. Questions ranged from a single question to diagnostic interviews. Studies used either self-reported behavior (n = 15), or parent report of behavior (n = 27), self-report to form a diagnosis (n = 4), or parent-report diagnosis (n = 4), One study used more than one assessment measure of sleepwalking, collecting both parent and child reports [31]. Three studies encouraged participants to consult with a parent or family member, but did not assess or report the extent that was done [11, 32, 33].
Analyses
Criterion 7—Sampling design accounted for in the analysis: Thirteen studies has no risk of bias, 28 had risk of bias and 10 had unclear risk. Criterion 8—Confidence intervals for statistical estimates: The confidence intervals were calculated for each study and are summarized in Table 3.
As a result of the significant risk of bias in all studies and the great variations between studies including definitions of sleepwalking, data collection, measuring and reporting of results, a series of a priori decisions were made with respect to combining data. All studies were included and no sensitivity analyses were able to be conducted. For lifetime prevalence, the highest rate reported in a study was used as the lifetime prevalence rate. As the true lifetime prevalence rate cannot decrease over time, differences at different time points in the one study are likely to reflect attrition and/or recall bias. Period prevalence rates varied considerably between studies—previous week, previous one month, 3 months, 6 months, 12 months, or period not specified. The small sample size for any given period and the significant risk of bias within studies make it problematic to ascertain the prevalence at each point. Consequently the studies that reported period prevalence rates between one week and 12 months were combined to provide an estimate of the current prevalence of sleepwalking, defined here as sleepwalking within the past year. Where studies reported multiple time points within the previous 12 months, the highest rate is taken to reflect the greatest proportion of participants sleepwalking within the previous 12 months. Where multiple papers for a single study reported the current prevalence rate at different ages, all that did not overlap in the age range were included in the calculation of current prevalence rate. When studies reported that parents and children completed interviews or questionnaires together, these were recorded as parent-reported prevalence rates.
Current prevalence of sleepwalking
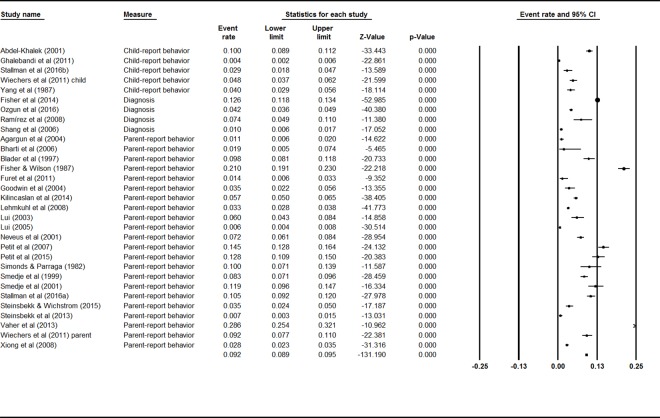
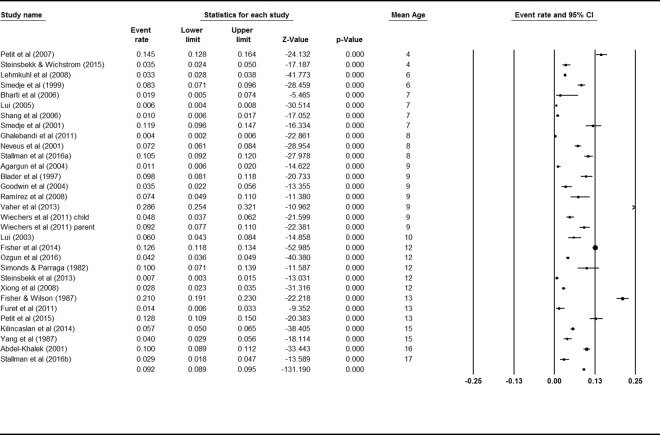
Mixed effects analysis showed a significant difference between the current prevalence rates for adult and child samples, Q = 22.25, p < .001, indicating the need to consider these populations separately. Thirty-one studies reported rates for various periods to provide current prevalence rates for sleepwalking behavior in children. A mixed effects analysis showed no significant difference between studies using child self-report behavior, parent-report behavior, and sleepwalking diagnoses, Q = 1.49, p = .48, indicating that they could be analyzed together. The event rates and 95% confidence interval across ages are shown in Fig 2. The combined effect for the current prevalence of sleepwalking during childhood was 5.0% (95% CI 3.8–6.5). There was high and significant heterogeneity between studies (I2 = 98%; Q value = 969.45, p < .001), indicating great variability in effect size estimates.
Fig 2. Forest plot for Current Sleepwalking in Children.
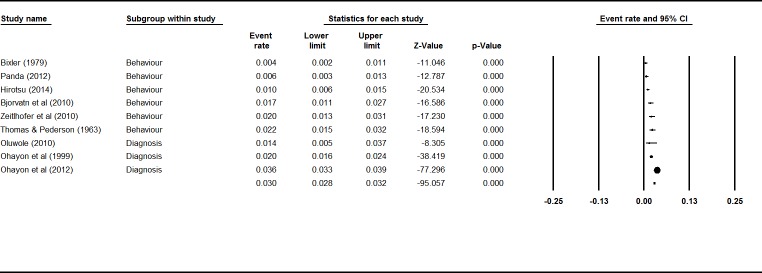
A mixed effects analysis showed no significant difference between self-reported sleepwalking behavior and diagnoses in adult studies (Q = 3.57, p = .06). The event rates and 95% confidence interval across ages are shown in Fig 3. The combined effect for the current prevalence rate of sleepwalking in adults from nine studies was 1.5% (95% CI 1.0%–2.3%). There was high and significant heterogeneity between studies (I2 = 93%; Q value = 108.65, p < .001), indicating great variability in effect size estimates.
Fig 3. Forest plot for Current Sleepwalking in Adults.
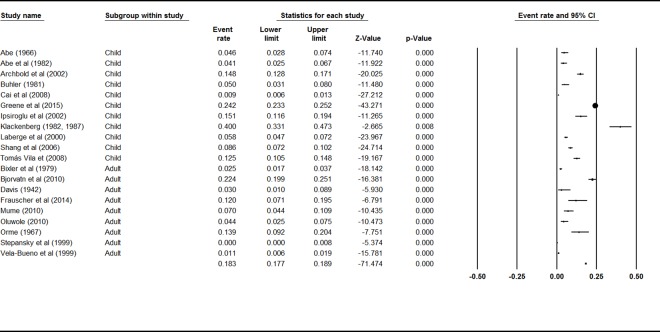
Lifetime prevalence of sleepwalking
There was no significant difference for lifetime prevalence rates of sleepwalking between adults and children, Q = 1.65 p = .20, indicating that the 20 studies could be analyzed together. The event rates and 95% confidence interval across ages are shown in Fig 4. The combined effect for lifetime prevalence of sleepwalking was 6.9% (95% CI 4.6%–10.3%). There was high and significant heterogeneity between studies (I2 = 98%; Q value = 1238.95, p < .001), indicating great variability in effect size estimates.
Fig 4. Forest plot for Lifetime Sleepwalking.
Developmental trends in sleepwalking
Pediatric studies of sleepwalking in childhood included children aged between two and 18 years. The ages varied considerably between studies. The reporting of prevalence rates was diverse and included prevalence at a given age, prevalence within the sample’s age range and only reporting the mean age of the sample and a prevalence rate. In order to assess the developmental trend of sleepwalking across childhood, the mean age for each sample was calculated for each study. The event rates and 95% confidence interval across ages are shown in Fig 5. Meta-regression showed no significant relationship between the mean age of children reported in studies and the current prevalence rate of sleepwalking (Q value = 0.34, p = .56, R2 = 0). There was high and significant heterogeneity between studies (I2 = 98%; Q value = 1943, p < .001) indicating great variability in effect size estimates.
Fig 5. Forest Plot for child current sleepwalking prevalence ordered by mean sample age.
Bias and heterogeneity
Inspection of the funnel plots showed significant bias with positive skew for both current and lifetime prevalence rates. The Egger’s test was significant for bias for current child (t (29) = -8.66, p < .001) and adult analyses (t (7) = -4.36, p < .001) and lifetime analyses (t (18) = -7.99, p < .001). The Classic fail-safe N shows no evidence of publication bias with 4247 missing lifetime studies needed to bring p-value to non-significance, 8 010 adult current and 8 707 child current studies.
Discussion
This systematic review included more than 100 000 people from 51 studies to identify the prevalence rate of sleepwalking in adults and children. Sleepwalking has been reported in children as young as two years and throughout adulthood. The lifetime prevalence for sleepwalking was 6.9% (95% CI 4.6%–10.3%). This does not vary significantly between childhood and adulthood, suggesting that relatively few people start sleepwalking later in life. This is consistent with adult onset of sleepwalking being associated with medications [20] and neurodegenerative diseases (e.g.[34]). This finding highlights the importance for detailed clinical evaluations of patients presenting with sleepwalking for the first time in adulthood. The current rate of sleepwalking was higher in children than adults 5.0% (95% CI 3.8–6.5) than in adults 1.5% (95% CI 1.0%– 2.3%). This difference may be the result of methodological issues or the decrease in slow wave sleep evident between childhood and adulthood [35].
The strengths of this study are its large sample size, both for children and adults, and the large number of studies included in the analyses. The limitations relate to the methodological problems within studies that are reflected in the high risk of bias across all studies and the consequent high heterogeneity across all analyses. Sleepwalking research is hampered by the very nature of the phenomenon. It occurs at night while the individual is sleeping. No studies included in this review used objective measures of sleepwalking; all relying on self- or parent-reports of sleepwalking behavior. Sleepwalkers typically have poor memory of sleepwalking episodes, because like other NREM dreams, sleepwalking actions appear less bizarre and novel than REM dreams [36]. The identification of sleepwalking episodes is therefore heavily dependent on the behavior being observed by others or the sleepwalker suspecting it because of injuries or other occurrences, such as noticing that things in the house have been moved, when they awaken. This is supported by research that included relationship status, showing that sleepwalking is more prevalent in married people than single people [11]. It may also mean that the significant difference in current sleepwalking rates between children and adults is an artifact of not being observed, rather than a true effect. It is important that future research measure who participants live with and how they or the informant know the person has been sleepwalking, and then control for these factors when determining prevalence rates. When using parent-report in older children, it would be important to ascertain whether parents are awake and able to observe adolescents sleepwalking in order to better determine the validity of the measure.
Reliability and validity have not been evaluated for self-, or parent-report measures of sleepwalking. This likely accounts for the very high heterogeneity in the results of this study. Because the definition of sleepwalking varied considerably across studies, random effects modelling was used in this study as it does not assume one underlying true effect across measures. In contrast, clinical diagnostic measures, such as the DSM, have diagnostic criteria that include recurrent episodes, observed sleepwalking behavior with impaired functioning [9]. Prevalence rates would have therefore been expected to be lower than for sleepwalking behavior. However, this was not evident in the current study, likely due to the enormous heterogeneity in the sample. It is recommended that single behaviors, in addition to frequency or recurrent sleepwalking be assessed in future epidemiological studies to overcome this problem. The presence of impairment or distress is a consequence of sleepwalking behavior and should not be used to calculate prevalence rates. Few studies that assessed current period prevalence of sleepwalking, assessed incidence. This is an important component for future studies to include in order to be able to understand the developmental trajectory of sleepwalking.
There was also inconsistency across studies in recall periods. It would be sensible for future research to use the last 12 months to capture current sleepwalking, in addition to a recent period—such as previous two weeks—that is less affected by recall bias. Previous year period prevalence and incidence measurement would also readily enable the developmental trajectory of sleepwalking to be better observed. Other periods such as one, three and six months do not add anything of importance to our understanding of sleepwalking.
Conclusion
Prevalence rates of sleepwalking are challenging to measure due to methodological limitations in identifying and accurately measuring the behavior. These include: a) the event happening during sleep when an individual is least likely to be witnessed; b) the individual having little or no memory for the event; c) reliance on recall of retrospective events by the sleepwalker or the informant; and d) differences in the conceptual understanding and measurement of the behavior. Any estimates, therefore, are likely to underestimate the true prevalence rates and represent episodes that are known to either caregivers (in relation to child studies) or the participant (in the case of adult studies). The summary prevalence rates reported here have significant limitations associated with systematic measurement error and should be used cautiously. The combined child and adult data supports the notion that sleepwalking behavior is a relatively common occurrence sometime during the lifespan. This review highlights the need for further epidemiological research to accurately explore the prevalence and incidence of sleepwalking across the lifespan. Outcomes would be strengthened by methodologies that: a) concurrently assess sleepwalking behavior and sleepwalking disorders; b) triangulate results using subjective and objective measures; c) assess how individuals know they sleepwalk; and d) assess injuries to sleepwalker and others.
Supporting Information
(DOC)
Data Availability
As this is a systematic review, all data is listed in the publication.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Broughton RJ. Sleep disorders: Disorders of arousal? Enuresis, somnambulism, and nightmares occur in confusional states of arousal, not in "dreaming sleep". Science. 1968;159(3819):1070–8. 10.1126/science.159.3819.1070 [DOI] [PubMed] [Google Scholar]
- 2.Xie Q. Naked sleepwalker found in Manchester city centre at 4am by police—who returned him to his hotel after posing for a selfie. Daily Mail Australia. 2016;Monday, May 30th 2016.
- 3.Australian Bureau of Statistics. 3303.0—Causes of Death, Australia, 2013, Table 1. Underlying cause of death, All causes, Australia, 2013, ata cube: Excel spreadsheet, viewed 7 September 2015, http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3303.02013?OpenDocument. 2015.
- 4.Australian Bureau of Statistics. 3303.0—Causes of Death, Australia, 2010, Table 1. Underlying cause of death, All causes, Australia, 2010, ata cube: Excel spreadsheet, viewed 7 September 2015, http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3303.02010?OpenDocument. 2012.
- 5.Australian Bureau of Statistics. 3303.0—Causes of Death, Australia, 2012, Table 1. Underlying cause of death, All causes, Australia, 2012, ata cube: Excel spreadsheet, viewed 7 September 2015, http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3303.02012?OpenDocument. 2014.
- 6.Australian Bureau of Statistics. 3303.0—Causes of Death, Australia, 2011, Table 1. Underlying cause of death, All causes, Australia, 2011, ata cube: Excel spreadsheet, viewed 7 September 2015, http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3303.02011?OpenDocument. 2013.
- 7.Woodward M. Epidemiology: study design and data analysis 3rd ed. Boca Raton: Taylor & Francis; 2014. [Google Scholar]
- 8.American Academy of Sleep Medicine. International classification of sleep disorders–Third Edition (ICSD-3) 3rd ed. Westchester, IL: AASM; 2014. [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Washington, D.C.: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Sadeh A. The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev. 2011;15(4):259–67. 10.1016/j.smrv.2010.10.001 [DOI] [PubMed] [Google Scholar]
- 11.Mume CO. Prevalence of sleepwalking in an adult population. Libyan J Med. 2010;5(1):1–4. 10.4176/090907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baddeley A, Eysenck MW, Anderson MC. Memory. 2nd ed. London: Psychology Press; 2015. [Google Scholar]
- 13.Eysenck MW. Depth, elaboration, and distinctiveness In: Cermack LS, Craik FIM, editors. Levels of processing in human memory. Hillsdale, NJ: Lawrence Erlbaum Associates; 1979. [Google Scholar]
- 14.Hunt RR, Smith RE, Dunlap KD. How does distinctive processing reduce false memory? Journal of Memory and Language. 2011;65(4):378–89. 10.1016/j.jml.2011.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qui S-F, Poon W-Y, Tang M-L. Sample size determination for disease prevalence studies with partially validated data. Stat Methods Med Res. 2012;0(0):1–27. 10.1177/0962280212439576 [DOI] [PubMed] [Google Scholar]
- 16.Koch HJ, Stiller O. Diurnal variation of physiological rhythms in a patient with sleepwalking. Biol Rhythm Res. 2015;46(2):287–9. 10.1080/09291016.2014.994856 [DOI] [Google Scholar]
- 17.Wilson S, Nutt D. Sleep Disorders. Oxford: Oxford University Press; 2008. [Google Scholar]
- 18.Sheldon SH. Disorders of development and maturation of sleep, and sleep disorders in infancy, childhood, and cerebral palsy In: Culebras A, editor. Sleep Disorders and Neurological Disease. Hoboken: Informa Healthcare; 2007. p. 59–82. [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stallman HM, Kohler M, White J. Medication induced sleepwalking: A systematic review. Sleep Med Rev. in press. [DOI] [PubMed] [Google Scholar]
- 21.Boyle MH. Guidelines for evaluating prevalence studies. Evidence-Based Mental Health. 1998;1(2):37–9. 10.1136/ebmh.1.2.37 [DOI] [Google Scholar]
- 22.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–35. 10.1097/EDE.0b013e3181577511 [DOI] [PubMed] [Google Scholar]
- 23.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis Chichester, UK: John Wiley & Sons Ltd; 2009. [Google Scholar]
- 24.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in metaanalyses. BMJ. 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Light RJ, Pillemer DB. Summing up: The Science of Reviewing Research. Cambridge, Massachusetts: Harvard University Press; 1984. [Google Scholar]
- 26.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borenstein M, Hedges L, Higgins JPT, Rothstein HR. Comprehensive meta-analysis version 3 Englewood NJ: Biostat, Inc; 2005. [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, TR). Washington, DC: Author; 2000. [Google Scholar]
- 29.American Academy of Sleep Medicine. The International Classification of Sleep Disorders, Second Edition (ICSD-2). Darien, IL: Author; 2005. [Google Scholar]
- 30.World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Version 2016 Geneva: World Health Organization; 1992. [Google Scholar]
- 31.Wiechers S, Schlarb AA, Urschitz MS, Eggebrecht E, Schlaud M, Poets CF. Sleep problems and poor academic performance in primary school children. Somnologie. 2011;15(4):243–8. [Google Scholar]
- 32.Kilincaslan A, Yilmaz K, Oflaz SB, Aydin N. Epidemiological study of self-reported sleep problems in Turkish high school adolescents. Pediatr Int. 2014;56(4):594–600. 10.1111/ped.12287 [DOI] [PubMed] [Google Scholar]
- 33.Neveus T, Cnattingius S, Olsson U, Hetta J. Sleep habits and sleep problems among a community sample of schoolchildren. Acta Paediatr. 2001;90(12):1450–5. [DOI] [PubMed] [Google Scholar]
- 34.Poryazova R, Waldvogel D, Bassetti CL. Sleepwalking in patients with Parkinson disease. Arch Neurol. 2007;64(10):1524–7. 10.1001/archneur.64.10.1524 [DOI] [PubMed] [Google Scholar]
- 35.Colrain IM, Baker FC. Changes in sleep as a function of adolescent development. Neuropsychol Rev. 2011;21(1):5–21. 10.1007/s11065-010-9155-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Llewellyn S. Such stuff as NREM dreams are made on? The Behavioral and Brain Sciences. 2013;36(6):611–2. 10.1017/S0140525X12003135 [DOI] [PubMed] [Google Scholar]
- 37.Abdel-Khalek AM. Epidemiologic study of sleep disorders in Kuwaiti adolescents. Percept Mot Skills. 2001;93(3):901–10. 10.2466/pms.2001.93.3.901 [DOI] [PubMed] [Google Scholar]
- 38.Ghalebandi M, Salehi M, Rasoulain M, Shooshtari MH, Naserbakht M, Salarifar MH. Prevalence of parasomnia in school aged children in Tehran. Iran Journal of Psychiatry. 2011;6(2):75–9. [PMC free article] [PubMed] [Google Scholar]
- 39.Ipsiroglu OS, Fatemi A, Werner I, Paditz E, Schwarz B. Self-reported organic and nonorganic sleep problems in schoolchildren aged 11 to 15 years in Vienna. J Adolesc Health. 2002;31(5):436–42. 10.1016/S1054-139X(02)00423-8 [DOI] [PubMed] [Google Scholar]
- 40.Stallman HM, Kohler M, Wilson A, Biggs S, Dollman J, Martin AJ, et al. Self-reported sleepwalking in Australian senior secondary school students. Sleep Medicine. 2016;25:1–3. 10.1016/j.sleep.2016.06.024 [DOI] [PubMed] [Google Scholar]
- 41.Yang L, Zuo C, Eaton LF. Research note: Sleep problems of normal Chinese adolescents. J Child Psychol Psychiatry. 1987;28(1):167–72. [DOI] [PubMed] [Google Scholar]
- 42.Abe KK. Predisposition to sleep-walking. Psychiatr Neurol (Basel). 1966;152(5):30. [DOI] [PubMed] [Google Scholar]
- 43.Abe K, Ohta M, Amatomi M, Oda N. Persistence and predictive value of behaviours of 3-yr-olds: A follow-up study at 8 years. Acta Paedopsychiatr. 1982;48(4):185–91. [PubMed] [Google Scholar]
- 44.Agargun MY, Cilli AS, Sener S, Bilici M, Ozer OAO, Selvi Y, et al. The prevalence of parasomnias in preadolescent school-aged children: a Turkish sample. Sleep. 2004;27(4):701–5. [DOI] [PubMed] [Google Scholar]
- 45.Archbold KH, Pituch KJ, Panahi P, Chervin RD. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr. 2002;140(1):97–102. Epub 2002/01/30. 10.1067/mpd.2002.119990 [DOI] [PubMed] [Google Scholar]
- 46.Bharti B, Malhi P, Kashyap S. Patterns and problems of sleep in school going children. Indian Pediatr. 2006;43(1):35–8. Epub 2006/02/09. [PubMed] [Google Scholar]
- 47.Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children: A community survey. Arch Pediatr Adolesc Med. 1997;151(5):473–80. 10.1001/archpedi.1997.02170420043007 [DOI] [PubMed] [Google Scholar]
- 48.Buhler M, Largo RH. Sleeping behavior between the ages of 2 and 18. Longitudinal study. Helvetica paediatrica acta. 1981;36(6):533–41. Epub 1981/01/01. . [PubMed] [Google Scholar]
- 49.Cai YM, Yi ZW, Huang H, Li JM, Luo XM. Epidemiological investigation of sleep disorders for children at ages of 2–12 years in Changsha City. Chinese Journal of Contemporary Pediatrics. 2008;10(3):353–6. [PubMed] [Google Scholar]
- 50.Fisher BE, Wilson AE. Selected sleep disturbances in school children reported by parents: Prevalence, interrelationships, behavioral correlates and parental attributions. Percept Mot Skills. 1987;64(3 II):1147–57. [DOI] [PubMed] [Google Scholar]
- 51.Goodwin JL, Kaemingk KL, Fregosi RF, Rosen GM, Morgan WJ, Smith T, et al. Parasomnias and sleep disordered breathing in Caucasian and Hispanic children–the Tucson children's assessment of sleep apnea study. BMC Med. 2004;2(1). 10.1186/1741-7015-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Furet OA, Goodwin J, Quan SF. Incidence and remission of parasomnias among adolescent children in the Tucson Children’s Assessment of Sleep Apnea (TuCASA) Study:. Southwest Journal of Pulmonary and Critical Care. 2011;2:93–101. [PMC free article] [PubMed] [Google Scholar]
- 53.Greene G, Gregory AM, Fone D, White J. Childhood sleeping difficulties and depression in adulthood: The 1970 British Cohort Study. J Sleep Res. 2015;24(1):19–23. 10.1111/jsr.12200 [DOI] [PubMed] [Google Scholar]
- 54.Klackenberg G. A prospective longitudinal study of children. Acta Paediatr Scand. 1971;Supp 224:1–239. [PubMed] [Google Scholar]
- 55.Klackenberg G. Somnambulism in childhood: prevalence, course and behavioral correlations A prospective longitudinal study (6–16 years). Acta Paediatr. 1982;71(3):495–9. 10.1111/j.1651-2227.1982.tb09458.x [DOI] [PubMed] [Google Scholar]
- 56.Klackenberg G. Incidence of parasomnias in children in a general population In: Guilleminault C, editor. Sleep and its disorders in children. New York: Raven Press; 1987. p. 99–113. [Google Scholar]
- 57.Laberge L, Tremblay RE, Vitaro F, Montplaisir J. Development of parasomnias childhood to early adolescence. Pediatrics. 2000;106(1 I):67–74. [DOI] [PubMed] [Google Scholar]
- 58.Lehmkuhl G, Wiater A, Mitschke A, Fricke-Oerkermann L. Sleep disorders in children beginning school: Their causes and effects. Deutsches Ärzteblatt International. 2008;105(47):809–14. 10.3238/arztebl.2008.0809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu X, Liu LL, Wang R. Bed Sharing, sleep habits, and sleep problems among chinese school-aged children. Sleep. 2003;26(7). [DOI] [PubMed] [Google Scholar]
- 60.Liu X, Ma Y, Wang Y, Jiang Q, Rao X, Lu X, et al. Brief report: An epidemiologic survey of the prevalence of sleep disorders among children 2 to 12 years old in Beijing, China. Pediatrics. 2005;115(1 Suppl):266–8. Epub 2005/05/04. 10.1542/peds.2004-0815I [DOI] [PubMed] [Google Scholar]
- 61.Petit D, Touchette E, Tremblay RE, Boivin M, Montplaisir J. Dyssomnias and parasomnias in early childhood. Pediatrics. 2007;119(5):1016–25. 10.1542/peds.2006-2132 [DOI] [PubMed] [Google Scholar]
- 62.Petit D, Pennestri MH, Paquet J, Desautels A, Zadra A, Vitaro F, et al. Childhood Sleepwalking and Sleep Terrors: A Longitudinal Study of Prevalence and Familial Aggregation. JAMA pediatrics. 2015;169(7):653–8. Epub 2015/05/06. 10.1001/jamapediatrics.2015.127 . [DOI] [PubMed] [Google Scholar]
- 63.Simonds JF, Parraga H. Prevalence of sleep disorders and sleep behaviors in children and adolescents. J Am Acad Child Psychiatry. 1982;21(4):383–8. 10.1016/S0002-7138(09)60942-0 [DOI] [PubMed] [Google Scholar]
- 64.Smedje H, Broman JE, Hetta J. Parents' reports of disturbed sleep in 5-7-year-old Swedish children. Acta Paediatr. 1999;88(8):858–65. Epub 1999/09/30. [DOI] [PubMed] [Google Scholar]
- 65.Smedje H, Broman JE, Hetta J. Associations between disturbed sleep and behavioural difficulties in 635 children aged six to eight years: A study based on parents' perceptions. Eur Child Adolesc Psychiatry. 2001;10(1):1–9. 10.1007/s007870170041 [DOI] [PubMed] [Google Scholar]
- 66.Stallman HM, Kohler M, Biggs S, Lushington K, Kennedy D, Martin AJ. Childhood sleepwalking and its relationship to daytime and sleep related behaviors. Sleep and Hypnosis. 2016:Advance online publication. 10.5350/Sleep.Hypn.2016.18.0122 [DOI] [Google Scholar]
- 67.Steinsbekk S, Berg-Nielsen TS, Wichstrom L. Sleep disorders in preschoolers: prevalence and comorbidity with psychiatric symptoms. J Dev Behav Pediatr. 2013;34(9):633–41. 10.1097/01.dbp.0000437636.33306.49 [DOI] [PubMed] [Google Scholar]
- 68.Steinsbekk S, Wichstrom L. Stability of sleep disorders from preschool to first grade and their bidirectional relationship with psychiatric symptoms. J Dev Behav Pediatr. 2015;36(4):243–51. Epub 2015/02/05. 10.1097/dbp.0000000000000134 [DOI] [PubMed] [Google Scholar]
- 69.Anders TF, Eiben L. Sleep Disorders In: Zeanah C, editor. Handbook of infant mental health. New York: The Guilford Press; 2000. [Google Scholar]
- 70.Tomás Vila M, Miralles Torres A, Beseler Soto B, Revert Gomar M, Sala Langa Ma S, Uribelarrea Sierra AI. Sleep patterns and sleep disturbances among schoolchildren in the town of Gandia. Anales de Pediatria. 2008;68(3):250–6. [DOI] [PubMed] [Google Scholar]
- 71.Vaher H, Kasenõmm P, Vasar V, Veldi M. A survey of parentally reported sleep health disorders in estonian 8–9 year old children. BMC Pediatrics. 2013;13:200 10.1186/1471-2431-13-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xiong F, Yang F, Mao M, Yang HM, Wang J. Sleep problems among school age children in Chengdu. Journal of Sichuan University (Medical Science Edition). 2008;39(6):1014–7. [PubMed] [Google Scholar]
- 73.Fisher HL, Lereya ST, Thompson A, Lewis G, Zammit S, Wolke D. Childhood parasomnias and psychotic experiences at age 12 years in a United Kingdom birth cohort. Sleep. 2014;37(3):475–82. 10.5665/sleep.3478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ozgun N, Sonmez FM, Can G, Topbas M. Insomnia and parasomnia frequency and affecting factors in school children. Pediatr Int. 2016. 10.1111/ped.12954 [DOI] [PubMed] [Google Scholar]
- 75.Ramírez MMC, Martínez LCM, Velásquez MCN, Peña Á MA, Carmona JL, Ochoa WC. Prevalence of sleep disorders in school children from Sabaneta, Colombia 2005. Iatreia. 2008;21(2):113–20. [Google Scholar]
- 76.Shang C-Y, Gau SS-F, Soong WT. Association between childhood sleep problems and perinatal factors, parental mental distress and behavioral problems. J Sleep Res. 2006;15(1):63– 10.1111/j.1365-2869.2006.00492.x [DOI] [PubMed] [Google Scholar]
- 77.Bixler EO, Kales A, Soldatos CR, Kales JD, Healey S. Prevalence of sleep disorders in the Los Angeles metropolitan area. Am J Psychiatry. 1979;136(10):1257–62. 10.1176/ajp.136.10.1257 [DOI] [PubMed] [Google Scholar]
- 78.Bjorvatn B, Grønli J, Pallesen S. Prevalence of different parasomnias in the general population. Sleep Med. 2010;11(10):1031–4. 10.1016/j.sleep.2010.07.011 [DOI] [PubMed] [Google Scholar]
- 79.Davis EM. Somnambulism. The Lancet. 1942;1:186. [Google Scholar]
- 80.Hirotsu C, Bittencourt L, Garbuio S, Andersen ML, Tufik S. Sleep complaints in the Brazilian population: Impact of socioeconomic factors. Sleep Science. 2014;7(3):135–42. 10.1016/j.slsci.2014.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Orme JE. The incidence of sleepwalking in various groups. Acta Psychiatr Scand. 1967;43(3):279–81. 10.1111/j.1600-0447.1967.tb05764.x [DOI] [PubMed] [Google Scholar]
- 82.Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India. 2012;60(1):68–74. 10.4103/0028-3886.93601 [DOI] [PubMed] [Google Scholar]
- 83.Stepansky R, Schmeiser-Rieder A, Holzinger B, Saletu B, Bolitschek J, Zeitlhofer J. Self reported prevalence of parasomnias and bedtime restless legs. Somnologie. 1999;3(2):78–82. 10.1007/s11818-999-0014-7 [DOI] [Google Scholar]
- 84.Thomas CB, Pederson LA. Psychobiological studies. II. Sleep habits of healthy young adults with observations on levels of cholesterol and circulating eosinophils. Journal of Chronic Disease. 1963;16:1099. [DOI] [PubMed] [Google Scholar]
- 85.Vela-Bueno A, De Iceta M, Fernandez C. Prevalence of sleep disorders in Madrid, Spain. Gac Sanit. 1999;13(6):441–8. Epub 2000/01/05. [DOI] [PubMed] [Google Scholar]
- 86.Frauscher B, Mitterling T, Bode A, Ehrmann L, Gabelia D, Biermayr M, et al. A prospective questionnaire study in 100 healthy sleepers: non-bothersome forms of recognizable sleep disorders are still present. J Clin Sleep Med. 2014;10(6):623–9. 10.5664/jcsm.3784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Oluwole OSA. Lifetime prevalence and incidence of parasomnias in a population of young adult Nigerians. J Neurol. 2010;257(7):1141–7. 10.1007/s00415-010-5479-6 [DOI] [PubMed] [Google Scholar]
- 88.Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry. 1999;60(4):268 [DOI] [PubMed] [Google Scholar]
- 89.Ohayon MM, Mahowald MW, Dauvilliers Y, Krystal AD, Leger D. Prevalence and comorbidity of nocturnal wandering in the U.S. adult general population. Neurology. 2012;78(20):1583–9. Epub 2012/05/16. 10.1212/WNL.0b013e3182563be5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
As this is a systematic review, all data is listed in the publication.