Abstract
Objectives. To understand the effect of unintentional injuries (e.g., drug overdose), suicide, and homicide on pregnancy-associated death (death during or within 1 year of pregnancy).
Methods. We analyzed all cases of pregnancy-associated death among Philadelphia, Pennsylvania, residents from 2010 to 2014, examining cause of death, contributing factors, and history of health care use.
Results. Approximately half (49%; 42 of 85) of pregnancy-associated deaths were from unintentional injuries (n = 31), homicide (n = 8), or suicide (n = 3); drug overdose was the leading cause (n = 18). Substance use was noted during or around events leading to death in 46% (31 of 67) of nonoverdose deaths. A history of serious mental illness was noted in 39% (32 of 82) of nonsuicide deaths. History of intimate partner violence (IPV) was documented in 19% (15 of 77) of nonhomicide deaths. Regardless of cause of death, approximately half of all decedents had an unscheduled hospital visit documented within a month of death.
Conclusions. Unintentional injury, homicide, and suicide contribute to many deaths among pregnant and recently pregnant women. Interventions focused on substance use, mental health, and IPV may reduce pregnancy-associated and pregnancy-related deaths.
Maternal mortality is increasing in the United States.1 Maternal mortality traditionally includes deaths from medical causes directly related to pregnancy (e.g., hemorrhage, thromboembolism, and hypertensive disease). Although substance use, serious mental illness, and intimate partner violence (IPV) also are exacerbated by pregnancy and are known to worsen perinatal outcomes,2–4 deaths involving these causes are not included in current definitions of US maternal mortality.5 Failure to record and analyze these deaths may lead to missed opportunities to prevent death during a critical period when women are likely to seek health care services.
Examining a larger group of pregnancy-associated deaths—or those occurring during or within 1 year of pregnancy from any cause—may elucidate the full scope of causes of maternal mortality. To address this gap, we used data obtained by the Philadelphia Maternal Mortality Review (MMR) team to examine causes of death, contributing factors, and hospital use patterns in Philadelphia, Pennsylvania, in all identified residents with pregnancy-associated death between 2010 and 2014.
METHODS
The Philadelphia MMR reviews all identified cases of pregnancy-associated death. Cases are identified through International Classification of Diseases, 10th Revision,6 codes on the death certificate and through linkage analysis between maternal death certificate and infant birth certificate. A physician or medical examiner determines cause and manner of death for the death certificate; manner of death is classified as accident, homicide, natural (referred to in this analysis as medical), suicide, or undetermined. A nurse abstractor summarizes available health and social service records for each decedent, and a social worker attempts to interview close decedent contacts such as a partner or family member for supplementary information.7
We extracted cause and manner of death, demographics, comorbidities, and history of care use from case summaries and performed descriptive analysis with Stata version 13.1 (StataCorp LP, College Station, TX).
RESULTS
The Philadelphia MMR reviewed all 85 identified cases of pregnancy-associated death (i.e., deaths occurring during or within a year of pregnancy from any cause; Table 1) occurring from 2010 to 2014 in Philadelphia. Of all deaths, 51% (43 of 85) were from medical causes, and 49% (42 of 85) were from injuries or nonmedical causes. These included unintentional injuries (e.g., drug overdose), suicide, and homicide.
TABLE 1—
Characteristics of Women (n = 85) Who Died During or Within 1 Year of Pregnancy: Philadelphia, PA, 2010–2014
| Characteristic | Median (Range) or No. (%) |
| Demographics | |
| Age, y | 27 (24–33) |
| Race/ethnicity | |
| Non-Hispanic Black | 49 (58) |
| Non-Hispanic White | 27 (32) |
| Hispanic/Latina (of any race) | 8 (9) |
| Non-Hispanic Asian/Pacific Islander | 1 (1) |
| Insurancea | |
| Medicaid | 63 (84) |
| Private | 5 (7) |
| Uninsured | 7 (9) |
| Total no. of pregnanciesb | |
| 1 | 18 (21) |
| 2 | 14 (16) |
| 3 or 4 | 27 (32) |
| ≥ 5 | 26 (31) |
| Timing of death | |
| During pregnancy | 26 (31) |
| Delivery to 6 wks postpartum | 16 (19) |
| 6 wks to 1 y postpartum | 43 (51) |
| Manner/cause of death | |
| Medical | 43 (51) |
| Hemorrhage or obstetric complicationc | 7 (16) |
| Cardiovascular | 22 (51) |
| Infection | 6 (14) |
| Other medical (e.g., cancer) | 8 (19) |
| Unintentional injury | 31 (36) |
| Drug overdose | 18 (58) |
| Motor vehicle crash | 9 (29) |
| Other (e.g., fire, fall) | 4 (13) |
| Suicide | 3 (4) |
| Homicide | |
| Overall | 8 (9) |
| Committed by intimate partner | 4 (50) |
Insurance status was known for 88% (75 of 85) of decedents.
Includes the index pregnancy (i.e., the pregnancy during or within 1 year of which the woman died).
Percentages of specific causes of death (e.g., hemorrhage or obstetric complication, drug overdose, homicide by intimate partner) are column percentages (i.e., as a percentage of all medical/natural deaths, unintentional injuries, or homicides, respectively). These deaths are presented in aggregate to protect case confidentiality.
Among unintentional injuries (n = 31), drug overdose was the leading direct cause of death (58%; 18 of 31). Among suicides (n = 3), all had a history of serious mental illness prior to death based on recorded diagnoses in medical records. Finally, among homicides (n = 8), 50% (4 of 8) were committed by intimate partners; all of these women had a documented history of IPV based on provider and agency records before their death.
We also identified substance use, serious mental illness, and IPV during or around the events leading to death in women who died of other causes. Recent or current drug or alcohol use was noted in 46% (31 of 67) of nonoverdose deaths. A history of serious mental illness was noted in 39% (32 of 82) of nonsuicide deaths. A history of IPV was documented in 19% (15 of 77) of nonhomicide deaths.
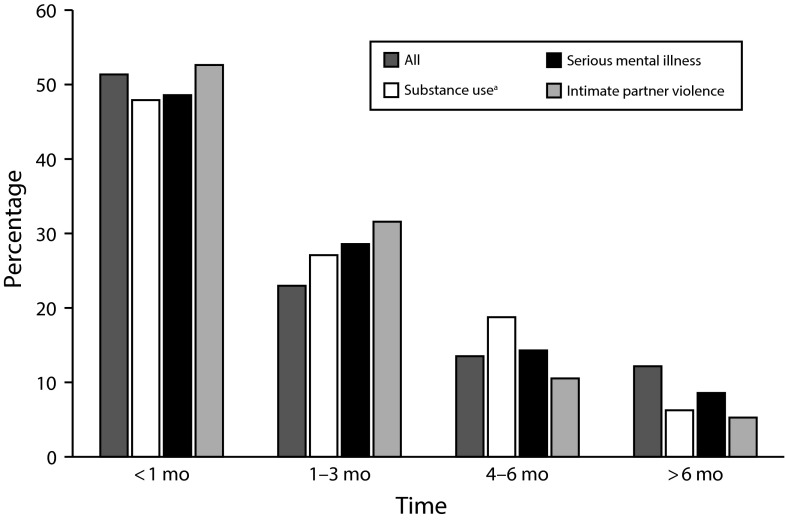
Of decedents with available records, 51% (38 of 74) were documented to have sought unscheduled medical care in an emergency department or hospital within 1 month of their death. This percentage was similar for women in whom substance use (48%), mental illness (49%), and IPV (53%) played a direct or indirect role in their death (Figure 1).
FIGURE 1—
Time Since Last Health System Contact Among Women Who Died During or Within 1 Year of Pregnancy: Philadelphia, PA, 2010–2014
Note. Data exclude terminal hospitalization (i.e., the hospitalization during which death occurred, if applicable).
aSubstance use, serious mental illness (i.e., schizophrenia, other psychotic disorders, bipolar disorder, or major depressive disorder), or intimate partner violence was noted during or around the events leading to death. Categories are not mutually exclusive.
DISCUSSION
In Philadelphia, approximately half of all women who died during or within 1 year of pregnancy died of unintentional injuries, suicide, or homicide. Of all deaths, more than half were directly or indirectly associated with substance use, more than 40% were associated with serious mental illness, and more than 20% were associated with IPV. These percentages are comparable to those reported previously in other US cities and reflect a higher prevalence of these conditions in pregnant women compared with all reproductive-aged women.8–10 We found that approximately half of all decedents had a recorded unscheduled hospital visit within a month of death, suggesting significant missed opportunities for prevention.
A recently published report noted that the rate of pregnancy-related deaths in Philadelphia residents exceeded national rates (27.0 vs 16.0 of 100 000). Of these deaths, only 1 was thought to be “preventable” by health system intervention based on standard review procedures. Efforts to define the preventable maternal death in Philadelphia date back to the city’s first reports on maternal mortality in the 1930s, which posited that deaths were preventable if an individual physician or hospital’s management could have altered the outcome.7
The findings from our analysis of hospital contacts prior to pregnancy-associated death suggest that more deaths may be truly preventable through efforts of modern health systems and institutions of public health. Like other medical diseases, the trajectories of substance use disorder, serious mental illness, and IPV can be altered by pregnancy. One recent analysis of national vital records suggested an increased risk of homicide and a reduced risk of suicide during pregnancy and the postpartum period; findings were limited by a high proportion of missing and potentially misclassified data.11 Our use of a local review allowed for exploration of these causes of death with more granular data.
Regardless of whether a risk factor is specifically related to pregnancy, health system contact during pregnancy presents a unique opportunity to identify vulnerabilities and alter outcomes. Proven interventions exist to help address morbidity and mortality resulting from substance use disorder, serious mental illness, and IPV during pregnancy. For example, interdisciplinary perinatal management of substance use disorder with medication-assisted treatment and behavioral health management has been extensively described.2 Home visitation and integrated psychobehavioral interventions can reduce the risk of recurrent episodes of IPV during pregnancy and the postpartum period.12 Efforts to improve the quality of medical and obstetric care for pregnant and postpartum women should be broadened to incorporate such services at the point of scheduled and unscheduled care.
We recommend the direct involvement of health systems and providers in building the functional, community-engaged systems for referral, treatment, communication, and support required to address complex issues such as substance use disorder, mental illness, and IPV during pregnancy. For example, the creation of health information exchanges may allow for sharing of information about clinical and behavioral treatment across facilities, settings, and providers. Second, providers and agencies can engage first responders and emergency providers to implement professionally mandated universal screening for substance use disorder, mental illness, and IPV during pregnancy. Third, those with unmet needs can be immediately linked to evidence-based care, case management, and social support models.7 Pilot programs and trials in these areas have shown promise, but emerging obstetric safety “bundles” created to improve outcomes focus only on medical contributors to death.13
PUBLIC HEALTH IMPLICATIONS
Our findings suggest that a narrow focus on the medical causes of maternal mortality is inadequate. This has been recognized in part by the World Health Organization in a 2012 recommendation that suicide deaths be included in maternal mortality. Even women who died from medical causes frequently had histories of substance use disorder, serious mental illness, or IPV—hidden potential contributors to maternal mortality. An approach that relies on a broader framework to define the “preventable” pregnancy-associated death and leverage health system contact is vital to addressing the US maternal health crisis.
ACKNOWLEDGMENTS
The authors would like to thank the entire Philadelphia Maternal Mortality Review Team and the Philadelphia Department of Public Health.
HUMAN PARTICIPANT PROTECTION
We obtained institutional review board approval from the Philadelphia Department of Public Health and the University of Pennsylvania.
REFERENCES
- 1.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125(1):5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 2.ACOG Committee on Health Care for Underserved Women; American Society of Addiction Medicine. ACOG Committee Opinion No. 524: Opioid abuse, dependence, and addiction in pregnancy. Obstet Gynecol. 2012;119(5):1070–1076. doi: 10.1097/AOG.0b013e318256496e. [DOI] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women. ACOG Committee Opinion No. 343: Psychosocial risk factors: perinatal screening and intervention. Obstet Gynecol. 2006;108(2):469–477. doi: 10.1097/00006250-200608000-00046. [DOI] [PubMed] [Google Scholar]
- 4.Brownridge DA, Taillieu TL, Tyler KA, Tiwari A, Ko Ling C, Santos SC. Pregnancy and intimate partner violence: risk factors, severity, and health effects. Violence Against Women. 2011;17(7):858–881. doi: 10.1177/1077801211412547. [DOI] [PubMed] [Google Scholar]
- 5.Creanga AA, Berg CJ, Ko JY et al. Maternal mortality and morbidity in the United States: where are we now? J Womens Health (Larchmt) 2014;23(1):3–9. doi: 10.1089/jwh.2013.4617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.International Classification of Diseases, 10th Revision. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 7.Philadelphia Department of Public Health Medical Examiner’s Office. Maternal Mortality in Philadelphia: 2010-2012. May 2015. Available at: http://www.phila.gov/health/pdfs/MMR%202010-12%20Report%20-%20final%20060115.pdf. Accessed May 15, 2015.
- 8.Hardt N, Wong TD, Burt MJ, Harrison R, Winter W, Roth J. Prevalence of prescription and illicit drugs in pregnancy-associated non-natural deaths of Florida mothers, 1999-2005. J Forensic Sci. 2013;58(6):1536–1541. doi: 10.1111/1556-4029.12219. [DOI] [PubMed] [Google Scholar]
- 9.Massachusetts Department of Public Health. Pregnancy-associated injury deaths: violence, substance abuse and motor vehicle collisions, 1990-1999. May 2002. Available at: http://www.mass.gov/eohhs/docs/dph/com-health/prego-newborn/safe-mom-preg2002-report.doc. Accessed June 1, 2015.
- 10.Cheng D, Horon IL. Intimate-partner homicide among pregnant and postpartum women. Obstet Gynecol. 2010;115(6):1181–1186. doi: 10.1097/AOG.0b013e3181de0194. [DOI] [PubMed] [Google Scholar]
- 11.Wallace ME, Hoyert D, Williams C, Mendola P. Pregnancy-associated homicide and suicide in 37 US states with enhanced pregnancy surveillance. Am J Obstet Gynecol. 2016;215(3):364.e1–364.e10. doi: 10.1016/j.ajog.2016.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Parys AS, Verhamme A, Temmerman M, Verstraelen H. Intimate partner violence and pregnancy: a systematic review of interventions. PLoS One. 2014;9(1):e85084. doi: 10.1371/journal.pone.0085084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D’Alton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol. 2014;123(5):973–977. doi: 10.1097/AOG.0000000000000219. [DOI] [PubMed] [Google Scholar]