Abstract
Until now, known as the demure cousin of dengue virus (DENV) inhabiting Africa, Zika virus (ZIKV) has reinvented itself to cause explosive epidemics captivating the Western hemisphere. The outbreak causing potential for ZIKV was realized when it made its way from Africa to Yap Island Micronesia in 2007, and in French Polynesia in 2013. From there, it moved on to Brazil in 2015. Now ZIKV has infected people in more than 33 countries in Central and South America and the Caribbean. Moreover the epidemiological and subsequent virological association with microcephaly cases in Brazil has prompted the World Health Organization to declare a public health emergency of International Concern. ZIKV shares not only its vector Aedes aegypti with dengue and chikungunya but also the geographic distribution and clinical features, which makes the laboratory confirmation mandatory for definitive diagnosis. The serological cross-reactivity with other Flavivirus, particularly with DENV makes laboratory confirmation challenging and will place additional burden on health systems to establish molecular diagnostic facilities. The evidence of additional nonvector modes of transmission, such as perinatal, sexual as well as transfusion has made preventative strategies more difficult. As ZIKV disease continues to mystify us with several unanswered questions, it calls for coordinated effort of global scientific community to address the ever growing arboviral threat to mankind.
KEY WORDS: Aedes aegypti, chikungunya, dengue, microcephaly, Zika virus
Introduction
An unexpected upsurge in infants born with microcephaly in Brazil and a possible association with the emergence of Zika virus (ZIKV) within the region has put the International health authorities on high alert. In May 2015, autochthonous cases of suspected ZIKV disease were identified in Brazil and by December 2015, 440,000–1,300,000 suspected cases of ZIKV disease were reported too in Brazil.[1] In January 2016, the US Centers for Disease Control and Prevention (CDC) issued travel guidance on affected countries, which included the use of enhanced precautions and considering postponing travel, besides guidelines for pregnant women.[2,3] The rapid spread of ZIKV, previously restricted to remote ecologic niches in Africa and Asia, throughout South America, Central America, the Caribbean, and the United States, underscores its huge pandemic potential and reinforces the need for better public health strategies to control arbovirus spread.
The Virus
ZIKV is a mosquito-borne Flavivirus related to yellow fever virus, dengue virus (DENV), and West Nile virus. The virus is a member of the spondweni serocomplex of genus Flavivirus and family Flaviviridae. Like other viruses in this family, ZIKV is an enveloped virus with icosahedral symmetry. The genome is single-stranded, nonsegmented, positive-sense RNA genome (10,794-nt genome) and is closely related to the Spondweni virus. The genome contains two untranslated regions at 5′ and 3′, flanking a single open reading frame that encodes a polyprotein which gets cleaved into three structural proteins (capsid [C], premembrane/membrane, and envelope [E]) and seven nonstructural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5). Based on the nucleotide sequences derived from the NS5 gene, two major ZIKV lineages have been described: African, and Asian.[4] The African lineages have further been subdivided into East African and West African clades, suggestive of two independent ZIKV introductions.[5] There are different hypotheses regarding the origin, phylogenetic relationships between the major ZIKV lineages.[5] Although the Asian lineage is believed to have originated from the African lineage by some investigators, the other hypothesis suggests of both ZIKV lineages having parallel evolution from a common ancestor.[5]
The virological factors possibly associated with the sudden increase in the epidemic potential as well as increased pathogenicity are poorly understood. A comparative genomic analysis of representative preepidemic and epidemic ZIKV strains has revealed phylogenetic clustering of the epidemic strains with the Asian lineage with additional presence of a fragment of genetic recombination at NS2B with that of Spondweni virus.[6] Fifteen amino acid substitutions have been found in the epidemic strains when compared with the preepidemic strains.[6] Further studies are needed to ascertain the biological significance of these genomic changes.
Disease Background
ZIKV was originally isolated in 1947 from a rhesus monkey kept for a surveillance study of YFV in the Zika forest, near Kampala, Uganda, and subsequently from a pool of Aedes africanus mosquitos at the same site in 1948.[7] ZIKV was first isolated from human cases in Nigeria in 1968.[8] Prior to 2007, when the first large-scale ZIKV outbreak was reported from Yap Island in Micronesia, serologic evidence of human ZIKV infection was also reported from several African countries such as Uganda, Tanzania, Egypt, Central African Republic, Sierra Leone, and Gabon, as well as in parts of Asia including India, Malaysia, the Philippines, Thailand, Vietnam, and Indonesia but only 14 human cases were reported.[9] The 2007 Yap Island outbreak (49 confirmed cases, 73% of the residents with serologic evidence for recent ZIKV infection), was the first time that ZIKV was detected from outside of Africa and Asia in an unexpected magnitude.[10,11] The second large-scale epidemic was reported in 2013 from French Polynesia (FP) with an estimated 28,000 cases (approximately 11% of the population).[12] These large-scale epidemics in Yap Island in Micronesia, and FP occurred concomitantly with circulation of DENVs and were initially misdiagnosed as dengue. An unusual increase in the incidence of Guillain–Barre syndrome (GBS) and congenital neurological malformations was noticed in the FP outbreak.[12] These outbreaks showcased the potential of ZIKV to cross its territory to new geographic locales, capable of causing large scale epidemics as well as possibility of more serious disease symptoms, previously not attributed to the virus.
Current Outbreak
In the early 2015, ZIKV was found as the causative agent of an outbreak of dengue and chikungunya like illnesses in the North-Eastern Brazil. This was the first evidence of autochthonous transmission of ZIKV in the Americas.[1] Currently, the ZIKV epidemic continues to spread at an alarming speed in the Americas. As of April 4, 2016, autochthonous cases of ZIKV infection were reported from 33 countries or territories in America in the past 2 months.[13] Apart from its unusual rate of spread, in the current Brazilian outbreak, health authorities have reported an apparent 20-fold increase in microcephaly cases, in comparison with the previous year rates (4300 cases have been recorded as Mid-February 2016).[14] The ongoing ZIKV is also notable because, for the first time any arbovirus is directly linked to adverse fetal outcome. Initially, the high rates of microcephaly among infants born to mothers with proven antecedent ZIKV had provided a suspicion linking ZIKV to microcephaly. The subsequent finding of ZIKV RNA in the amniotic fluid of fetuses with microcephaly as well as in the brain tissue of fetuses and infants with microcephaly has provided strong evidence linking maternal ZIKV to microcephaly.[15,16] The World Health Organization (WHO) has declared the spread of ZIKV and the associated birth defects an International Public Health Emergency on February 1, 2016.[17]
Transmission
Vector-borne transmission
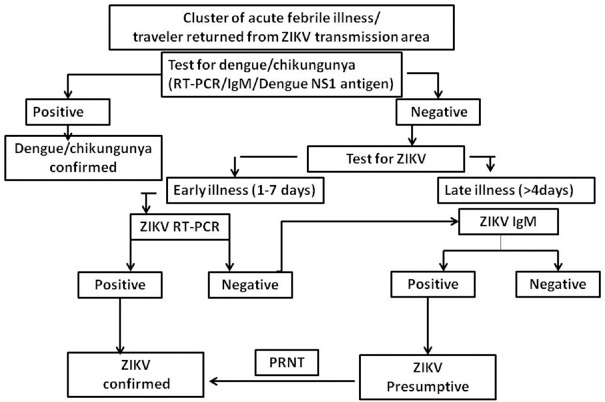
ZIKV was originally isolated from a pool of A. africanus mosquitoes in 1947 in the Zika forest, near Kampala, Uganda.[7] The virus is maintained in nature in a sylvatic cycle involving nonhuman primates and A. africanus mosquitoes with cyclic epizootics in monkeys reported in Uganda.[7] In the sylvatic transmission cycle, humans likely serve as incidental hosts. ZIKV has been isolated notably from Aedes aegypti, and other Aedes mosquitoes such as Aedes polynesinensis, Aedes luteocephalus, Aedes vittatus, Aedes (Stegomyia) apicoargenteus, Aedes furcifer.[18] Aedes hensilli were the predominant mosquito species in the Yap outbreak.[12] Man–Mosquito–Man was the major mode of transmission during Yap outbreak.[12] It is also being hypothesized that ZIKV may follow the footsteps of yellow fever, dengue, and chikungunya viruses and establish an entirely new maintenance cycles of human A. aegypti human transmission with A. aegypti being the common vectors for Zika as well as chikungunya and dengue [Figure 1].[19] Since the first description of A. albopictus as a potential vector of ZIKA in 2007 by Wong et al., other reports have also suggested the possibility of ZIKV adapting to a sustainable transmission cycle involving A. albopictus.[20] This could be responsible for the emergence of new ZIKA infection epidemics in urban areas.
Figure 1.
Modes of transmission of Zika virus
Nonvector-borne Zika virus transmission
Several nonvector-borne ZIKV transmission routes are also described [Figure 1]. Direct interhuman transmission, most likely by sexual intercourse, has been described.[21] Perinatal transmission via trans placental route and breast milk has been reported during the outbreak in FP.[22] The detection of ZIKV RNA in the amniotic fluid of affected newborns in the ongoing Brazil epidemic together with a precipitous surge in infants born with microcephaly, further substantiates trans placental route of transmission.[23] The isolation of ZIKV from 3% of blood donors in FP has already raised the potential for transmission via blood transfusion.[24]
Clinical features
Until ZIKV outbreak occurred in FP clinical features of ZIKV was restricted only to mild illnesses similar to other arboviral infections like dengue and chikungunya. Fever, rash, conjunctivitis, and arthralgia are the common manifestations in various reported ZIKV cases including Yap island outbreak where 1/3 population was affected.[10,11] Myalgia, retro-orbital pain, anorexia, vomiting, diarrhea, constipation, abdominal pain are among the less common manifestations.[10,11]
The association of ZIKV with neurological manifestations was noted for the first time during 2013–2014 outbreak in FP.[12] The outbreak reported 8750 suspected cases with 383 confirmed cases. Seventy-four cases were documented with neurological symptoms or autoimmune syndromes which had symptoms consistent with ZIKV infection within previous few days. Of these majority (42/74) were diagnosed to be GBS.[25] The current outbreak in Brazil, recorded 76 cases with neurological manifestations, with GBS being the most prevalent (42/76). Other South American countries also reported similar observation.[17] Meningitis, meningoencephalitis, and myelitis are among the other neurological syndromes reported during FP outbreak.[26]
The association of ZIKV with congenital neural malformations though noticed for the first time in FP, the association was proved during the current Brazil outbreak.[15,16] The ZIKV etiology in microcephaly was first suspected in Brazil when a number of microcephaly per 1000 live births were found to be alarmingly high during 2015 in comparison with previous years (20 times high).[14] Microcephaly is a clinical condition where size of head is small as per the gestational age. After the recent emergence of possible link of microcephaly with ZIKV infection, the CDC has recommended microcephaly to be defined as occipitofrontal circumference less than third percentile for gestational age and sex.[14] Presence of ZIKV RNA by reverse transcription-polymerase chain reaction (RT-PCR) in amniotic fluid of pregnant women with fetal microcephaly who had symptoms consistent of ZIKV during gestation, in fetal amniotic fluid of microcephaly children and finally detection of viral genome in tissues of four cases of congenital malformation by RT-PCR confirmed the ZIKV infection in microcephalic babies and trans placental transmission.[15,16]
Zika virus and pregnancy
During pregnancy, ZIKV can infect in any trimester. The rate of infection in pregnant women and the risk of congenital infection are presently not known. Current evidence does not indicate higher susceptibility or severity of ZIKV infection in pregnant women.[2] However, evidence from the recent epidemics indicates the risk of congenital malformation like microcephaly appears to be more if the infection occurs during the first trimester.[27]
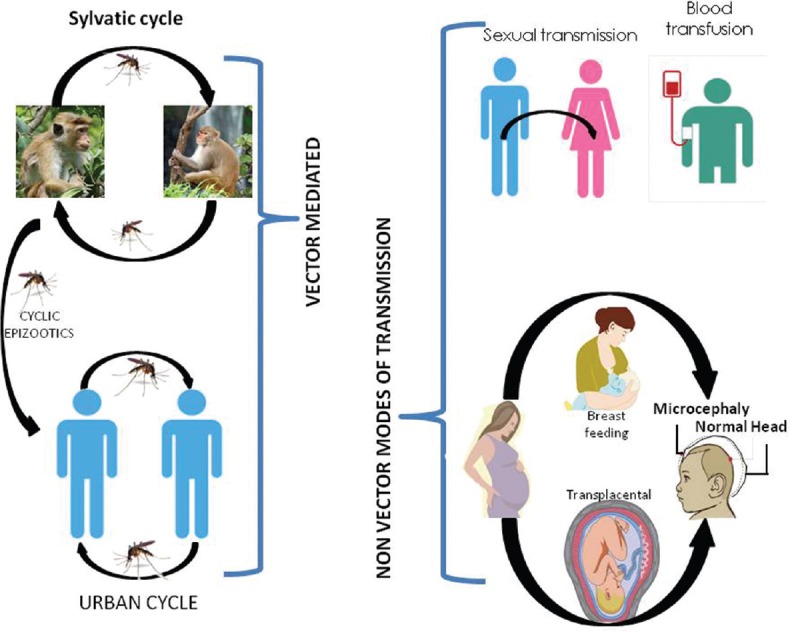
Laboratory diagnosis
Diagnosis of ZIKV should be considered after ruling out the possibility of dengue and chikungunya viral infections. Detection of viral RNA or IgM antibody in serum samples can be employed for both the viral infections, whereas for dengue infection, NS1 antigen enzyme-linked immunosorbent assay can also be done.[28]
During the acute phase of illness (before 5 days of illness) ZIKV is commonly diagnosed by detection of viral RNA in serum of the patients by RT-PCR. Saliva and urine samples also have been used for this.[29,30] The rate of positivity and viral load has been reported to be higher in urine sample as compared to serum. RNA positivity in urine has also been detected up to 15 days as compared to 5 days in serum.[30]
Virus specific IgM may be positive as early as day 3 of illness. However, if the serum sample is negative within 7 days of illness, the test should be repeated with convalescent sample to check for sero-conversion. Strong cross-reactivity with other Flaviviruses, more so with DENV, is a common reason of false positive serological test.[31]
During the late phase of illness (7–8th postillness), sample should be subjected for virus specific IgM antibody detection and IgM positive samples should further be confirmed by plaque reduction neutralization test (PRNT) to measure virus specific neutralizing antibodies. Four-fold rise in antibody titer between acute and convalescent samples is taken as confirmatory for primary infection. However, PRNT still suffers from cross-reactivity for secondary Flavivirus infection.[31] Figure 2 depicts the practical approach to diagnose suspected ZIKV infection in dengue and chikungunya endemic settings.
Figure 2.
Zika virus diagnosis algorithm in dengue/chikungunya endemic setting
All samples of suspected ZIKV infection should be handled in Biosafety level-2 laboratories.
Treatment and prevention
Presently there is no specific antiviral available for ZIKV and supportive treatment is the main stay of patient management. Due to the absence of specific treatment and vaccine, the role of prevention is of paramount importance particularly for the pregnant women. CDC has advised ZIKV testing and fetal ultrasound to detect microcephaly or intra-cranial calcification in pregnant women returning from Zika transmission area or to defer travel to those countries if possible.[2] Considering the mild and asymptomatic nature of the infection in most of the cases, CDC has also advised the men who are residing in or have returned from the Zika transmission area and have pregnant partner, to refrain from sexual activity or to use condom for the duration of pregnancy. The same is also advised to the men having nonpregnant partner to avoid sexual transmission.[32]
For others who are planning to travel to Zika transmission areas are also advised to prevent mosquito bite, keeping in mind the fact that the mosquitoes responsible for transmission of ZIKV bite mostly during the day time both indoors and outdoors. The WHO has advised to all its member countries to set up the surveillance for detection of first case where A. aegypti mosquitoes are circulating.
Zika virus in the Indian context
India, being endemic for dengue and chikungunya viruses and harboring A. aegypti, is ecologically conducive for ZIKV transmission. The important similarities and differences between dengue, chikungunya and ZIKV are enlisted in Table 1.
Table 1.
| Chikungunya | Dengue | Zika | |
|---|---|---|---|
| Virus family | Togaviridae | Flaviviridae | Flaviviridae |
| Mode of transmission | Man–mosquito–man | Man–mosquito–man | Man–mosquito–man And man to man |
| Principal vector |
A. aegypti (Mc) A. albopictus |
A. aegypti (Mc) A. albopictus |
A. aegypti |
| Nonvector modes | Rare | Rare | Yes |
| Sexual | No | No | Yes |
| Breast feeding | No | No | Possible |
| Blood transfusion | Rare | Possible | Possible |
| Incubation period | 3–7 days | 3–14 days | Few days to a week |
| Asymptomatic: Case (%) | 3–30 | 50–75 | ~80 |
| Signs and symptoms | Fever, arthralgia | Fever, maculopapular rash, thrombocytopenia, retro-orbital pain DHF and DSS in severe cases |
Mild febrile illness, conjunctivitis, joint pain and muscle ache |
| Neurologic and autoimmune complications | Infrequent | Infrequent | GBS |
| Congenital malformation | Infrequent | infrequent | Microcephaly |
| Lab diagnosis | IgM antibody by MAC ELISA- after 5-7 days RT-PCR (1st week) | Early phase (1st 5 days)- Ns1 Ag IgM antibody by MAC ELISA- after 5-7 days RT-PCR (1st week) | IgM antibody by MAC ELISA- after 5-7 days (high degree of cross reaction) RT-PCR (1st week) |
| Treatment | No antiviral Supportive | No antiviral Supportive | No antiviral Supportive |
| Vaccine | Not available | Available (CYD-TDV) | Not available |
DHF: Dengue hemorrhagic fever, DSS: Dengue shock syndrome, GBS: Guillain–Barre syndrome, A. aegypti: Aedes aegypti, TDV: Tetravalent dengue vaccine, RT-PCR: Reverse transcription-polymerase chain reaction
The Ministry of Health and Family Welfare, Government of India has issued a guideline on ZIKV disease to track clustering of febrile illness, microcephaly among newborns and GBS.[37] The two apex laboratories of the country, National CDC, Delhi and National Institute of Virology, Pune are equipped to provide the diagnostic facilities for ZIKV RT-PCR in suspected cases, where as 10 more labs are getting geared up to cater the entire country.
Conclusion
For the first time, an arbovirus has been associated with a severe congenital malformation. The world is already facing the challenge of mosquito-borne diseases such as dengue and chikungunya due to the increasing geographic range of the vector Aedes, and of malaria due to increasing drug resistance. In addition to this existing burden, the new entity of serious congenital malformation with another mosquito-borne virus has posed a huge challenge to the global health authorities to handle the mosquito menace. The reason for expansion of clinical spectrum and severe neural involvement by a previously innocuous virus should be sought into with a serious note. The presence of virus in various body fluids, particularly semen and saliva which can play role in virus transmission, needs extensive research. Finally in the absence of antivirals, possibility of vaccine in near future provides some hope to tackle the emergency. The transformation of ZIKV from a benign to a frightening virus has made the world to believe the unbelievable and remain prepared to face the challenge.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zanluca C, Melo VC, Mosimann AL, Santos GI, Santos CN, Luz K. First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz. 2015;110:569–72. doi: 10.1590/0074-02760150192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen EE, Staples JE, Meaney-Delman D, Fischer M, Ellington SR, Callaghan WM, et al. Interim guidelines for pregnant women during a Zika virus outbreak – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:30–3. doi: 10.15585/mmwr.mm6502e1. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 1600 Clifton Road Atlanta, GA 30329-4027 USA. CDC Issues Interim Travel Guidance Related to Zika Virus for 14 Countries and Territories in Central and South America and the Caribbean. [About 4 Screens] [Last updated on 2016 Jan 17; Last cited on 2016 Jan 17]. Available from: http://www.cdc.gov/media/releases/2016/s0315-zika-virus-travel.html .
- 4.Haddow AD, Schuh AJ, Yasuda CY, Kasper MR, Heang V, Huy R, et al. Genetic characterization of Zika virus strains: Geographic expansion of the Asian lineage. PLoS Negl Trop Dis. 2012;6:e1477. doi: 10.1371/journal.pntd.0001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faye O, Freire CC, Iamarino A, Faye O, de Oliveira JV, Diallo M, et al. Molecular evolution of Zika virus during its emergence in the 20(th) century. PLoS Negl Trop Dis. 2014;8:e2636. doi: 10.1371/journal.pntd.0002636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu Z, Chan JF, Tee KM, Choi GK, Lau SK, Woo PC, et al. Comparative genomic analysis of pre-epidemic and epidemic Zika virus strains for virological factors potentially associated with the rapidly expanding epidemic. Emerg Microbes Infect. 2016;5:e22. doi: 10.1038/emi.2016.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dick GW, Kitchen SF, Haddow AJ. Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46:509–20. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- 8.Moore DL, Causey OR, Carey DE, Reddy S, Cooke AR, Akinkugbe FM, et al. Arthropod-borne viral infections of man in Nigeria, 1964-1970. Ann Trop Med Parasitol. 1975;69:49–64. doi: 10.1080/00034983.1975.11686983. [DOI] [PubMed] [Google Scholar]
- 9.Hayes EB. Zika virus outside Africa. Emerg Infect Dis. 2009;15:1347–50. doi: 10.3201/eid1509.090442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, et al. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232–9. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS, et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009;360:2536–43. doi: 10.1056/NEJMoa0805715. [DOI] [PubMed] [Google Scholar]
- 12.Cao-Lormeau VM, Roche C, Teissier A, Robin E, Berry AL, Mallet HP, et al. Zika virus, French polynesia, South pacific, 2013. Emerg Infect Dis. 2014;20:1085–6. doi: 10.3201/eid2006.140138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. 1600 Clifton Road Atlanta, GA 30329.4027 USA. All Countries and Territories with Active Zika Virus Transmission. [About 2 Screens] [Last updated on 2016 May 02; Last cited on 2016 Feb 03]. Available from: http://www.cdc.gov/zika/geo/active-countries.html .
- 14.Victora CG, Schuler-Faccini L, Matijasevich A, Ribeiro E, Pessoa A, Barros FC. Microcephaly in Brazil: How to interpret reported numbers? Lancet. 2016;387:621–4. doi: 10.1016/S0140-6736(16)00273-7. [DOI] [PubMed] [Google Scholar]
- 15.Calvet G, Aguiar RS, Melo AS, Sampaio SA, de Filippis I, Fabri A, et al. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: A case study. Lancet Infect Dis. 2016 doi: 10.1016/S1473-3099(16)00095-5. pii: S1473-309900095-5. [DOI] [PubMed] [Google Scholar]
- 16.Martines RB, Bhatnagar J, Keating MK, Silva-Flannery L, Muehlenbachs A, Gary J, et al. Notes from the field: Evidence of Zika virus infection in brain and placental tissues from two congenitally infected newborns and two fetal losses – Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:159–60. doi: 10.15585/mmwr.mm6506e1. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. WHO Statement on the First Meeting of the International Health Regulations (2005) Emergency Committee on Zika Virus and Observed Increase in Neurological Disorders and Neonatal Malformations. [About 2 Screens] [Last updated on 2016 Feb 01; Last cited on 2016 Feb 01]. Available from: http://www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/en/
- 18.Marcondes CB, Ximenes Mde F. Zika virus in Brazil and the danger of infestation by Aedes (Stegomyia) mosquitoes. Rev Soc Bras Med Trop. 2016;49:4–10. doi: 10.1590/0037-8682-0220-2015. [DOI] [PubMed] [Google Scholar]
- 19.Fauci AS, Morens DM. Zika virus in the Americas – Yet another arbovirus threat. N Engl J Med. 2016;374:601–4. doi: 10.1056/NEJMp1600297. [DOI] [PubMed] [Google Scholar]
- 20.Wong PS, Li MZ, Chong CS, Ng LC, Tan CH. Aedes (Stegomyia) albopictus (Skuse): A potential vector of Zika virus in Singapore. PLoS Negl Trop Dis. 2013;7:e2348. doi: 10.1371/journal.pntd.0002348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foy BD, Kobylinski KC, Chilson Foy JL, Blitvich BJ, Travassos da Rosa A, Haddow AD, et al. Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg Infect Dis. 2011;17:880–2. doi: 10.3201/eid1705.101939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Besnard M, Lastere S, Teissier A, Cao-Lormeau V, Musso D. Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill. 2014;19 pii: 20751. [PubMed] [Google Scholar]
- 23.Washington, D.C: PAHO/WHO; 2016. [Last updated on 2016 Jan 17; Last cited on 2016 Jan 17]. Pan American Health Organization/World Health Organization. Epidemiological update: Neurological syndrome, congenital anomalies and Zika virus infection. About 8 Pages. Available from: http://www.paho.org/hq/index.php?option=com_docman and task=doc_view and Itemid=270 and gid=32879 and lang=en . [Google Scholar]
- 24.Musso D, Nhan T, Robin E, Roche C, Bierlaire D, Zisou K, et al. Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill. 2014;19 doi: 10.2807/1560-7917.es2014.19.14.20761. pii: 20761. [DOI] [PubMed] [Google Scholar]
- 25.European Centre for Disease Prevention and Control. Rapid risk assessment: Zika virus infection outbreak, Brazil and the Pacific region. 25 May 2015. Stockholm: ECDC; 2015. [Last updated on 2015 May 25; Last cited on 2016 May 25]. About 8 pages. Available from: http://www.ecdc.europa.eu/en/publications/Publications/rapid-risk-assessment-Zika?20virus-south-america-Brazil-2015.pdf . [Google Scholar]
- 26.European Centre for Disease Prevention and Control. Rapid risk assessment: Zika virus epidemic in the Americas: Potential association with microcephaly and Guillain. Barre syndrome. 10 December 2015. Stockholm: ECDC; 2015. [Last updated on 2015 Dec 10; Last cited on 2015 Dec 10]. About 14 pages. Available from: http://www.ecdc.europa.eu/en/publications/Publications/zika-virus-americas-association-with-microcephaly-rapid-risk-assessment.pdf . [Google Scholar]
- 27.Petersen LR, Jamieson DJ, Powers AM, Honein MA. Zika virus. N Engl J Med. 2016;374:1552–63. doi: 10.1056/NEJMra1602113. [DOI] [PubMed] [Google Scholar]
- 28.Pan American Health Organization. Zika virus (ZIKV) Surveillance in the Americas: Interim Guidance for Laboratory Detection and Diagnosis. 29 June, 2015 Algorithm for Detecting Zika Virus (ZIKV) 2015. [Last updated on 2016 March 3; Last cited on 2015 May 13]. Available from: http://www.paho.org/hq/index.php?option=com_docman and task=doc_view and ltemid=270 and gid=30176 and lang=en .
- 29.Musso D, Roche C, Nhan TX, Robin E, Teissier A, Cao-Lormeau VM. Detection of Zika virus in saliva. J Clin Virol. 2015;68:53–5. doi: 10.1016/j.jcv.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 30.Gourinat AC, O'Connor O, Calvez E, Goarant C, Dupont-Rouzeyrol M. Detection of Zika virus in urine. Emerg Infect Dis. 2015;21:84–6. doi: 10.3201/eid2101.140894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Division of Vector-Borne Diseases, Arboviral Diseases and Dengue Branches. 1600 Clifton Road Atlanta, GA 30329-4027 USA. CDC Arboviral Diseases and Dengue Branches Memorandum. Updated Diagnostic Testing for Zika, Chikungunya, and Dengue Viruses in US Public Health Laboratories. [Last updated on 2016 Jan 13; Last cited on 2016 Jan 13]. Available from: http://www.aphl.org/Materials/CDCMemo_Zika_Chik_Deng_Testing_011916.pdf .
- 32.Oster AM, Brooks JT, Stryker JE, Kachur RE, Mead P, Pesik NT, et al. Interim guidelines for prevention of sexual transmission of Zika virus – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:120–1. doi: 10.15585/mmwr.mm6505e1. [DOI] [PubMed] [Google Scholar]
- 33.Christofferson RC. Zika Virus Emergence and Expansion: Lessons Learned from Dengue and Chikungunya may Not Provide All the Answers. Am J Trop Med Hyg. 2016;95:15–8. doi: 10.4269/ajtmh.15-0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cecilia D. Current status of dengue and chikungunya in India. WHO South-East Asia J Public Health. 2014;3:22–7. doi: 10.4103/2224-3151.206879. [DOI] [PubMed] [Google Scholar]
- 35.Moulin E, Selby K, Cherpillod P, Kaiser L, Boillat-Blanco N. Simultaneous outbreaks of dengue, chikungunya and Zika virus infections: Diagnosis challenge in a returning traveller with nonspecific febrile illness. New Microbes New Infect. 2016;11:6–7. doi: 10.1016/j.nmni.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Halstead S. Critique of WHO Approval of a Dengue Vaccine. J Infect Dis. 2016 doi: 10.1093/infdis/jiw340. pii: jiw340. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 37.Government of India. Ministry of Health and Family Welfare. Directorate General of Health Services. Guidelines on Zika Virus Disease following Epidemic in Brazil and Other Countries of America. [About 5 pages] [Last accessed on 2016 April 8]. Available from: http://www.mohfw.nic.in/showfile.php?lid=3705 .