Abstract
Objective:
To compare the diagnostic accuracy of multi-slice computed tomography (MSCT) angiography with conventional angiography in patients undergoing major noncoronary cardiac surgeries.
Materials and Methods:
We studied fifty major noncoronary cardiac surgery patients scheduled for invasive coronary angiography, 29 (58%) female and 21 (42%) male. Inclusion criteria of the study were age of the patients ≥40 years, having low or intermediate probability of coronary artery disease (CAD), left ventricular ejection fraction (LVEF) >35%, and patient giving informed consent for undergoing MSCT and conventional coronary angiography. The patients with LVEF <35%, high pretest probability of CAD, and hemodynamically unstable were excluded from the study.
Results:
The diagnostic accuracy of CT coronary angiography was evaluated regarding true positive, true negative values. The overall sensitivity and specificity of CT angiography technique was 100% (95% confidence interval [CI]: 39.76%–100%) and 91.30% (95% CI: 79.21%–97.58%). The positive (50%; 95% CI: 15.70%–84.30%) and negative predictive values (100%; 95% CI: 91.59%–100%) of CT angiography were also fairly high in these patients.
Conclusion:
Our study suggests that this non-invasive technique may improve perioperative risk stratification in patients undegoing non-cardiac surgery.
Key words: Computed tomography angiography, conventional angiography, major noncoronary cardiac surgery
INTRODUCTION
Coronary artery disease (CAD) is the emerging cause of morbidity and mortality in developing world. Conventional coronary angiography has been the gold standard investigation for the diagnosis of CAD. It provides an excellent resolution for visualization of the coronary arteries for catheter-based or operating interventions.[1] Although the association of this technique with major complications such as mortality is highly uncommon, it is frequently associated with various cardiac and noncardiac complications.[2]
Computed tomography (CT) coronary angiography is a promising technique for the evaluation of CAD noninvasively.[3] It assesses disease within the coronary artery and provides qualitative and quantitative information about nonobstructive atherosclerotic plaque burden within the vessel wall. Thus, CT angiography-based disease evaluation may provide clinically more significant information than conventional angiography. The introduction of multi-slice computed tomography (MSCT) technology such as 64-slice, 128-slice, 256-slice, and now 320-slice MSCT has produced a high diagnostic accuracy of CT coronary angiography.[4] It has consistently showed to have a very high negative predictive value (well above 90%) in ruling out patients with significant CAD defined as coronary luminal stenosis of >50%.[5,6]
The American College of Cardiology/American Heart Association recommends that coronary angiography should be performed before valve surgery in men aged >40 years, women aged >35 years with coronary risk factors and in postmenopausal women.[7] The prevalence of CAD in patients undergoing valve replacement is 20–40% in developed countries. In the previous studies, the incidence of angiographically proven CAD in acquired valvular diseases has been shown to vary widely from 9% to 41%.[8] In aortic stenosis, the incidence of CAD was reported to be as high as 37%.[9] Hence, the accurate diagnosis of CAD in valvular patients holds high clinical importance.
We aimed to report the diagnostic performance of 128-slice CT coronary angiography in 50 patients undergoing for major noncoronary cardiac surgery referred for diagnostic invasive coronary angiography to assess the extent and severity of coronary stenosis.
MATERIALS AND METHODS
During January 2013 to December 2014, we enrolled fifty major noncoronary cardiac surgery patients scheduled for invasive coronary angiography who fulfilled the following inclusion criteria of age ≥40 years, having low or intermediate probability of CAD, left ventricular ejection fraction (LVEF) >35%, and patient giving informed consent for undergoing MSCT and conventional coronary angiography. Those having any contraindication for contrast injection, LVEF <35%, high pretest probability of CAD, and hemodynamic instability were excluded from the study. Patients with heart rates of >70 bpm received (unless they had known overt heart failure or electrocardiogram (ECG) atrioventricular conduction abnormalities) a single oral dose of 100 mg metoprolol 45 min before the scan. Patients with heart rates of >80 bpm received an additional oral dose of metoprolol if not contraindicated. If the patient was anxious, then lorazepam was used if not contraindicated.
All patients were scanned with a 128-slice CT scanner (Siemens, somatom definition AS) equipped with a new feature in MSCT technology, so-called z-axis flying-focus technology. The central 32 detector rows acquire 0.6-mm slices, and the flying-focus spot switches back and forth between 2 z positions between each reading. Two slices per detector row are acquired, which results in a higher oversampling rate in the z-axis, thereby reducing artifacts related to the spiral acquisition and improving spatial resolution down to 0.4 mm. A bolus of 65–80 mL contrast material (omnipaque) was injected through an arm vein at a flow rate of 5 mL/s. A bolus tracking technique was used to synchronize the arrival of contrast in the coronary arteries with the initiation of the scan. To monitor the arrival of contrast material, axial scans were obtained at the level of the ascending aorta with a delay of 10 s after the start of the contrast injection. The scan was automatically started when a threshold of 150 Hounsfield units was reached in a region of interest positioned in the ascending aorta. Images were reconstructed with ECG gating to obtain optimal, motion-free image quality.
Conventional coronary angiography evaluation
All scans were performed within 2 weeks of the MSCT coronary diagnostic angiogram. A single observer unaware of the multi-slice CT results identified coronary lesion as a single vessel, double vessel, or triple vessel disease. All lesion, regardless of size, were included for comparison with CT coronary angiography. Lesions were classified as having nonsignificant disease (luminal irregularities or <50% stenosis) or as having significant stenosis. Stenosis was evaluated in two orthogonal views and classified as significant if the mean lumen diameter reduction was 50% using a validated quantitative coronary angiography (QCA).[10]
Computed tomography coronary angiography evaluation
All scans were analyzed independently by a radiologist and a cardiologist who were unaware of the results of conventional coronary angiography. Total calcium scores of all patients were calculated with dedicated software and expressed as Agatston scores. The Agatston score is a commonly used scoring method that calculates the total amount of calcium on the basis of the number, areas, and peak Hounsfield units of the detected calcified lesions. All available coronary segments were visually scored for the presence of > 50% considered as significant stenosis. Maximum intensity projections were used to identify coronary lesions and (curved) multiplanar reconstructions to classify lesions as significant or nonsignificant. Disagreement between observers was resolved by consensus.
Statistical analysis
Data were analyzed using statistical system SPSS version 20 software (Chicago, IL, USA). The diagnostic performance of CT coronary angiography for the detection of significant lesions in coronary arteries with QCA as the standard of reference is presented as sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios with the corresponding exact 95% of confidence interval (CIs). Comparison between CT and conventional coronary angiography was performed on the two level vessel by vessel (no or any disease per vessel), and patient by patient (no or any disease per patient).
RESULTS
In this study, 29 (58%) subjects were female, and 21 (42%) were male showing an average age of 50.36 ± 8.39 years. The overall prevalence of CAD in the study population was 8%. Of fifty patients 24 (48%), 13 (26%), eight (16%), and five (10%) underwent mitral valve replacement, double valve replacement (DVR), aortic valve replacement, and other surgeries, respectively. High distribution of CAD risk factors such as hypertension (24%), smoking (22%), and dyslipidemia (18%) was observed in the study group. The mean creatinine level was 0.766 ± 0.17 and average dye used in conventional angiography was 48.5 ± 26.6 whereas for CT angiography it was 72.8 ± 6.32. Average radiation dose in conventional coronary angiography and MSCT coronary angiography was 5.2 mSv and 9.2 mSv, respectively.
The majority of the patients had sinus rhythm (68%), whereas atrial fibrillation was found in 32% of the subjects. Patients included in the study had low to intermediate probability of CAD. In this study, three patients had complications after conventional angiography. Complications were of local site hematoma, acute kidney injury managed conservatively, and acute heart failure. A patient who developed hematoma was obese female patients with body mass index >30 kg/m2. The patient suffered from pseudoaneurysm, had hospitalized for 9 days, which leads to increased morbidity and cost of hospital stay. None of the patients had a complication after CT coronary angiography. One patient needed repeat CT angiography due improper scan.
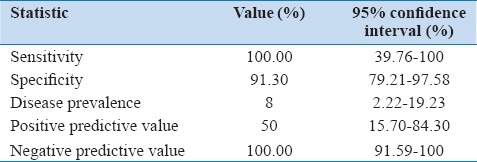
The diagnostic accuracy of CT coronary angiography was evaluated regarding true positive, true negative values and is presented in Table 1. The overall sensitivity and specificity of CT angiography technique was 100% (95% CI: 39.76%–100%) and 91.30% (95% CI: 79.21%–97.58%), respectively [Table 2]. The positive predictive value (50%; 95% CI: 15.70%–84.30%) and negative predictive value (100%; 95% CI: 91.59%–100%) of CT angiography were also fairly high in these patients.
Table 1.
Diagnostic test evaluation
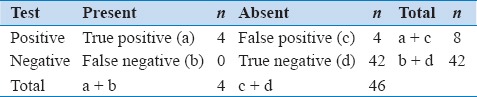
Table 2.
Diagnostic accuracy of computed tomography angiography according to sensitivity and specificity
DISCUSSION
Recent reports from multiple studies demonstrated that recent-generation MSCT scanners showed promise for noninvasive detection of coronary stenosis[11,12,13,14] However, until now no studies were found regarding the clinical efficacy or prognostic value of 128-slice CT coronary angiography versus conventional invasive coronary angiography in the diagnosis of patients planned for major noncoronary surgeries such as DVR, Bentall, atrial septal defect closure, etc.[15,16] In our study, we reported 8% CAD prevalence in patients planned for major noncoronary cardiac surgery. We performed conventional and MSCT coronary angiography in all patients and the results showed that CT coronary angiography with invasive coronary angiography as the reference standard had a considerably high sensitivity (100%) and specificity (95.65%).
The health economic model using invasive coronary angiography as the reference standard showed that at a pretest probability of CAD of 70% or lower, CT coronary angiography resulted in lower cost per patient with a true positive diagnosis. At a pretest probability of CAD of 70% or higher, invasive coronary angiography was associated with a lower cost per patient with a true positive diagnosis.[17]
In our study population, two patients developed local site complications in the form of hematoma and pseudoaneurysm after conventional angiography. None of the patients developed drug complication after MSCT coronary angiography. Hence, MSCT coronary angiography will be more favorable in female obese patients with intermediate likelihood of CAD. Hence, MSCT coronary angiography will be cost-effective in patients of valvular heart diseases.[18]
However, CT angiography suffers from a drawback that average amount of dye used in MSCT coronary angiography were 72.8 ± 6.32 ml which is higher than average amount of dye required for conventional angiography (48.6 ± 26.6 ml). Hence, the use of CT coronary angiography could not be used in patients with known renal dysfunction, where reduction of contrast dye load is highly advocated.
CONCLUSION
Our results show that 128-slice CT coronary angiography is a reliable technique to detect coronary stenosis in patients planned for noncoronary cardiac surgery. Although there has been important technological progress in the development of CT coronary angiography, its clinical application remains limited. A study wth large numbers of patients is required for the recommendation of only CT coronary angiography for the coronary evaluation in major non-cardiac surgeries.
Financial support and sponsorship
U.N. Mehta Institute of Cardiology and Research Center (Affiliated to BJ Medical College, Ahmedabad, Gujarat, India).
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kohsaka S, Makaryus AN. Coronary angiography using noninvasive imaging techniques of cardiac CT and MRI. Curr Cardiol Rev. 2008;4:323–30. doi: 10.2174/157340308786349444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tavakol M, Ashraf S, Brener SJ. Risks and complications of coronary angiography: A comprehensive review. Glob J Health Sci. 2012;4:65–93. doi: 10.5539/gjhs.v4n1p65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O'Gara P, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2010;56:1864–94. doi: 10.1016/j.jacc.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Otero HJ, Steigner ML, Rybicki FJ. The “post-64” era of coronary CT angiography: Understanding new technology from physical principles. Radiol Clin North Am. 2009;47:79–90. doi: 10.1016/j.rcl.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Achenbach S, Ulzheimer S, Baum U, Kachelriess M, Ropers D, Giesler T, et al. Noninvasive coronary angiography by retrospectively ECG-gated multislice spiral CT. Circulation. 2000;102:2823–8. doi: 10.1161/01.cir.102.23.2823. [DOI] [PubMed] [Google Scholar]
- 6.Zou KH, O'Malley AJ, Mauri L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation. 2007;115:654–7. doi: 10.1161/CIRCULATIONAHA.105.594929. [DOI] [PubMed] [Google Scholar]
- 7.Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, 3rd, Guyton RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:e57–185. doi: 10.1016/j.jacc.2014.02.536. [DOI] [PubMed] [Google Scholar]
- 8.Bozbas H, Yildirir A, Küçük MA, Ozgül A, Atar I, Sezgin A, et al. Prevalence of coronary artery disease in patients undergoing valvular operation due to rheumatic involvement. Anadolu Kardiyol Derg. 2004;4:223–6. [PubMed] [Google Scholar]
- 9.Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, et al. ACC/AHA guidelines for coronary angiography: Executive summary and recommendations. A report of the American college of cardiology/American heart association task force on practice guidelines (committee on coronary angiography) developed in collaboration with the society for cardiac angiography and interventions. Circulation. 1999;99:2345–57. doi: 10.1161/01.cir.99.17.2345. [DOI] [PubMed] [Google Scholar]
- 10.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol. 2008;52:1724–32. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 11.Nieman K, Rensing BJ, van Geuns RJ, Vos J, Pattynama PM, Krestin GP, et al. Non-invasive coronary angiography with multislice spiral computed tomography: Impact of heart rate. Heart. 2002;88:470–4. doi: 10.1136/heart.88.5.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mollet NR, Cademartiri F, Krestin GP, McFadden EP, Arampatzis CA, Serruys PW, et al. Improved diagnostic accuracy with 16-row multi-slice computed tomography coronary angiography. J Am Coll Cardiol. 2005;45:128–32. doi: 10.1016/j.jacc.2004.09.074. [DOI] [PubMed] [Google Scholar]
- 13.Sharma RK, Voelker DJ, Sharma RK, Singh VN, Bhatt G, Moazazi M, et al. Coronary computed tomographic angiography (CCTA) in community hospitals: Current and emerging role. Vasc Health Risk Manag. 2010;6:307–16. doi: 10.2147/vhrm.s9108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sun Z, Choo GH, Ng KH. Coronary CT angiography: Current status and continuing challenges. Br J Radiol. 2012;85:495–510. doi: 10.1259/bjr/15296170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia MJ, Lessick J, Hoffmann MH. CATSCAN Study Investigators. Accuracy of 16-row multidetector computed tomography for the assessment of coronary artery stenosis. JAMA. 2006;296:403–11. doi: 10.1001/jama.296.4.403. [DOI] [PubMed] [Google Scholar]
- 16.Tempe DK, Virmani S, Gupta R, Datt V, Joshi C, Dhingra A, et al. Incidence and implications of coronary artery disease in patients undergoing valvular heart surgery: The Indian scenario. Ann Card Anaesth. 2013;16:86–91. doi: 10.4103/0971-9784.109732. [DOI] [PubMed] [Google Scholar]
- 17.Meijboom WB, van Mieghem CA, Mollet NR, Pugliese F, Weustink AC, van Pelt N, et al. 64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery disease. J Am Coll Cardiol. 2007;50:1469–75. doi: 10.1016/j.jacc.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al. Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease. Health Technol Assess. 2008;12:1–164. doi: 10.3310/hta12170. [DOI] [PubMed] [Google Scholar]


