Abstract
Objectives:
The study was aimed to capture the effect of using injection pads as a tool in educating the diabetic patients who were on insulin. The attitude and practice of the patients in storage of insulin vials and disposal of insulin syringes were also assessed.
Materials and Methods:
A facility based Quasi-experimental study was carried out among the diabetic patients on insulin, attending diabetic clinic in endocrinology OPD in a tertiary care hospital, Puducherry. One to one intervention was given to the study participants or their attendants (who were involved in injecting insulin), by a trained investigator regarding all the steps of insulin administration. The insulin administration practices before and immediately after the intervention was assessed using a checklist.
Results:
In total 91 patients were included for the study with mean (SD) age of 53.9 (10.6) years and of them 76% were females. The attitude and practices of the study participants, such as hand washing before handling insulin, checking the expiry date, storage of insulin, inspection of injection site, rolling and cleaning the vial, withdrawal of the syringe up to the required dose, pushing the plunger after inserting the syringe into the vial, checking and removal of air bubbles, cleaning the injection site and allow to dry and injection technique improved significantly after the intervention (P < 0.05).
Conclusion:
This study findings shows that using injection pads for educating patients helps them to practise better insulin administration. The findings from the study can be applied in routine care and has to be explored further in diabetic patient management.
Key words: Effectiveness, insulin injection practice, insulin pad
INTRODUCTION
Diabetes has reached epidemic proportions worldwide.[1] Nearly, 347 million people suffer from diabetes worldwide,[2] and India is the host of 17.6% of them.[3] India leads the world with the largest number of diabetic patients earning the dubious distinction of being termed the “diabetes capital of the world.”[3] India, with one of the largest and most diverse populations of people living with diabetes, experiences significant barriers in successful diabetes care. In India, around 35–49% of the cases were detected to have diabetes after developing micro- and macrovascular complications related to diabetes.[4] For majority of these people, insulin becomes the mode of treatment. Insulin therapy is the mainstay of diabetes management,[1] and approximately 1.2 million Indians inject insulin. If injection technique is incorrect, there is a high risk of poor glycemic control. If needles are reused or used improperly, it can result in pain with bleeding and bruising, chances of breaking off and lodging under the skin, risk of contamination, infection, dosage inaccuracy, and lipodystrophy. Hence, injection technique is an important part of insulin therapy.[5] Limitations in appropriate and timely use of insulin impede the achievement of good glycemic control. Diseases such as diabetes need lifelong commitment from providers as well as patients. Even among the literate patient groups, readiness to follow insulin self-administration is very low. Some of the Indian studies revealed very poor adherence to treatment regimens due to poor attitude toward the disease and poor health literacy among the general public. Because the vast majority of day-to-day care in diabetes is handled by patients and/or families, there is an important need for reliable and valid measures for self-management of diabetes.[6]
Patient- and physician-targeted programs to enhance awareness in various aspects of diabetes care must be initiated across all levels of health care ensuring uniformity of information.[5] The barriers could be related to the patient, physician, or the health system. Some of them are fear of injections, excessive traveling, lack of knowledge of proper injection technique, and overburdened health-care providers. It could also be psychological factors related to poor self-efficacy or social stigma and in some cases due to dexterity problems or cognitive impairment.[7,8,9] Out of these, one of the important remediable barriers is the limited training provided to patients related to administration of insulin. Health education interventions were found to improve the knowledge and attitude domains profoundly; however, the improvement in the practice domain was relatively less.[10] One of the reasons could be that most patient education interventions did not provide hands-on training to the patient.
Most of the educational institutions use injection pads or equivalent alternatives to train medical and paramedical students about injection practices. A novel method of training the patient would be to use these for patient education and practice. Hence, we decided to study the effect of the use of injection pads on insulin administration practices of patients on treatment with insulin attending tertiary care teaching hospital. An additional effort was also made to capture the attitude and practice related to storage of insulin vials and disposal of used syringes among the patients.
METHODOLOGY
Study design and study setting
A facility-based quasi-experimental study (before and after type of interventional study) was carried out among the diabetic patients on insulin, attending diabetic clinic in endocrinology outpatient department (OPD) in a tertiary care hospital, Puducherry. The clinic is conducted biweekly and on an average 100 diabetic patients on insulin attends the clinic over a month. The OPD is manned by consultants and resident doctors from endocrinology department, along with nursing personnel and medical social worker trained for Diabetes Education programme.
Sample size and sampling technique
Assuming an additional 30% of patients could follow appropriate insulin administration techniques after training the minimum sample size required was calculated as 90 using OpenEpi software (Atlanta, US).[11] Every alternate patients attending were approached for participation in the study.
Study procedure and data collection
The data were collected during the month of August–September 2015. The investigator contacted the study participants after their consultation with their multidisciplinary team and explained the study purpose. Informed consent from patients was obtained, and patient details such as sociodemography, economic status, and history related to diabetes were captured using a semi-structured questionnaire. A checklist was prepared for the domains related to insulin storage, drawing appropriate dose from insulin vial, insulin administration, and disposal based on consensus guidelines issued by society of diabetes. Items in the checklist were developed from guidelines proposed by the Forum for Injection Technique, India.[5] The diabetic injection pad was used for the demonstration of injection practices. The pad simulates skin in color and texture, and it can be worn at any part of the body using adjustable straps [Figure 1].
Figure 1.

Insulin pad used for the demonstration of injection practices
Intervention
Step 1: Preintervention assessment of insulin administration practices
The patient was provided with a vial of insulin, alcohol swab, disposable syringe, and a diabetic injection pad and instructed to demonstrate insulin administration practices as they followed routinely at home. The investigator used a checklist to score the insulin administration practices based on the accepted guidelines for Indians.[6]
Step 2: Patient education intervention
The trained investigator demonstrated the study participants all the steps of insulin administration from storage, cleaning the vial, preparation of local site, withdrawal of correct dose, selection of appropriate site, administration using an insulin injection pad, and disposal of syringe for 10 min duration. The session was held separately for each participant to improve their participation. The patient and the attendant who is involved in injecting insulin were also included in the session.
Step 3: Immediate postintervention assessment of insulin administration practices
Ten minutes after the educational intervention, the patient was again assessed for the postintervention knowledge using the same method as described in Step 1 [Figure 2].
Figure 2.
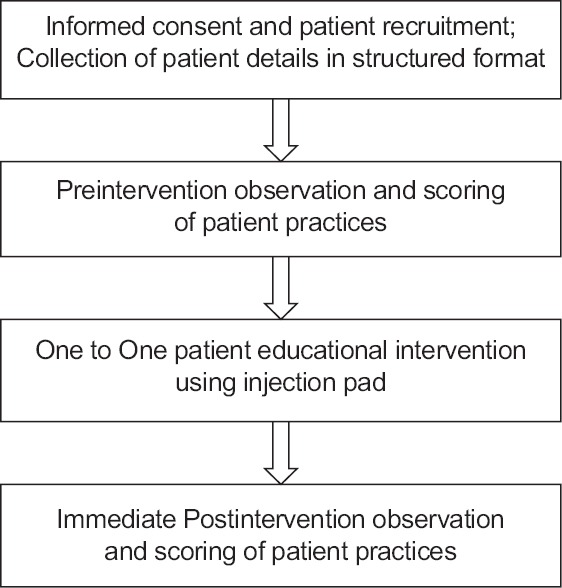
Flowchart explaining the study procedure
The study protocol was reviewed and approved by the Human Institute Ethics Committee of Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
Data entry and analysis
The data were entered in EpiData 3.0 and analyzed using EpiData analysis software (The EpiData Association, Odense M, Denmark, Europe).[12] The change in proportion of patients with good insulin administration practice in each item from pre- and post-intervention was done using McNemar Chi-square test. Items which were framed in a negative manner (e.g., storage of insulin in freezer) were recorded in the reverse direction to calculate cumulative score. Each item with good practice was scored as 1, otherwise 0. Finally, cumulative score was calculated using all these 17 items. Hence, the total score could range from 0 to 17. Similarly, cumulative score was calculated for the after intervention. Patients or relatives who administer insulin were categorized as following appropriate insulin administration practices if they obtained at least 70% in the overall score.
OBSERVATION AND RESULTS
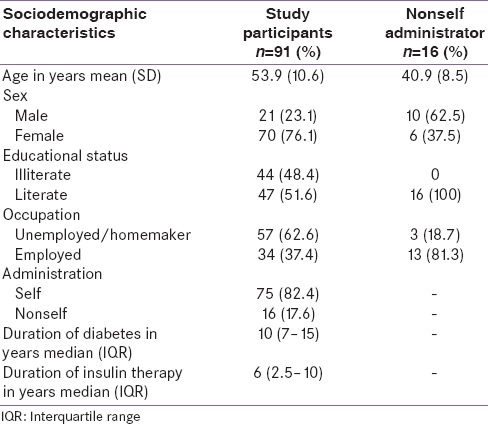
A total of 91 patients were included in the study with a mean (standard deviation) age of 53.9 (10.6) years. Around 80% of the participants were self-administering insulin and almost half of the participants were illiterate [Table 1]. For 16 participants, insulin injection was given by their relatives; majority by son (50%), followed by daughter (18.7%) and husband (12.5%), almost 20% of the participants reported storing insulin vials in mud pots containing water.
Table 1.
Sociodemographic characteristics of study participants
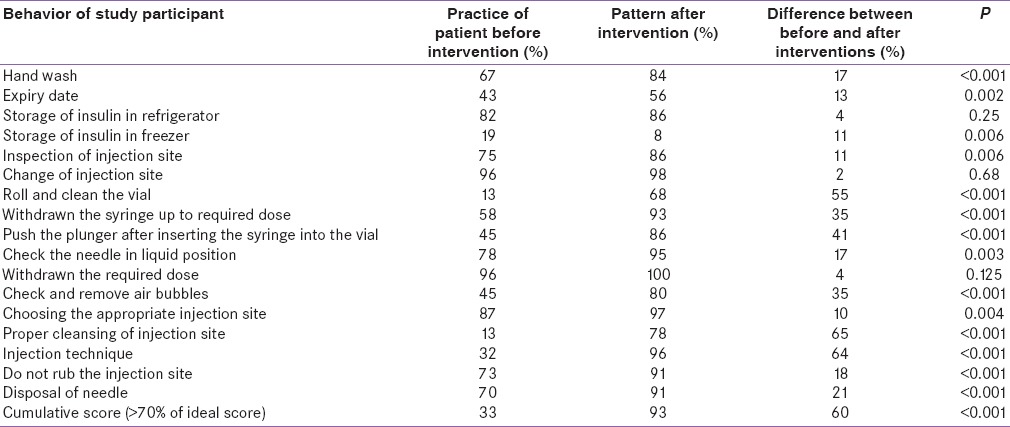
After intervention, a significant difference was seen in the manner, in which patients roll and clean the vial, withdrawal of the syringe up to the required dose, pushing the plunger after inserting the syringe into the vial, checking and removal of air bubbles, cleaning the injection site and allow to dry and injection technique. At the end of the demonstration, significantly more proportions of participants were able to show the best insulin administration practices (proportion of patients with more than 70% of ideal score: Preintervention: 33.0% vs. postintervention: 93.4%, P ≤ 0.001) [Table 2].
Table 2.
Distribution of change in insulin administration practice before and after the intervention by items among diabetes patients (n=91)
DISCUSSION
This study shows that educational intervention plays a significant positive impact on knowledge related to insulin use among diabetes patients using insulin. The preintervention knowledge was poor in almost two-third of the participants. This study shows that one to one counseling and demonstration using an injection pad model will result in substantial improvement in patient's knowledge which is considered a precursor of practice. Studies conducted in South India reported that there is a poor knowledge on insulin use among the diabetes patients who were on insulin.[10,13] Injection technique is critical to the therapeutic success of insulin and is highly operator-dependent. The correct administration technique will help in reducing the HbA1c levels.
This study has few implications in clinical practice. Faulty insulin administration practices were more commonly observed in following aseptic precautions, withdrawal of insulin from the vial and administration to the site. Poor knowledge in these steps may eventually lead to inadvertent high or low dose of insulin administration. Moreover, the lack of aseptic procedures will lead to life-threatening infections in already susceptible diabetic populations for local infections. Health-care providers should identify the patient level barriers in the administration of this technique. Accordingly, patients who could not follow these techniques on their own should be guided to nearest 24 × 7 primary health centers for further support. Repeated demonstration of this technique by grassroots workers can help these patients to learn this technique. Medical social worker and other staffs can be trained in patient-specific education and demonstration of insulin injection practices. In resource-constrained settings, the OPD waiting time of the patient can also be utilized by showing insulin injection-related videos, which may encourage patient's behavior change on insulin injection practices. Involvement of family members in such activities is critical, as insulin will be administered by family members too.
The study has few strengths. First, one to one intervention increased patient participation and understanding. Second, the intervention was focused not only on the patient but also on the insulin administrators including family members. Third, the injection pad was used in this study for demonstration, which can be tied anywhere in the patient's body, according to their injection practice. The texture of the insulin pad also mimics such as skin. Practice of insulin administration through this pad gives the participants exactly like a real-time experience there by confidence to administer on their own even if they are away from their health-care provider. The study has few limitations: The short-term impact of the intervention was only assessed. Whether the patient would be able to follow the same level of appropriate administration techniques in the long run should be confirmed from future studies. This study is based on one to one intervention. In resource-poor settings, where majority of the noncommunicable diseases (NCDs) are treated through NCD special clinics whether the group level demonstration or peer group discussion will lead to the same level of impact also needs to be explored from future studies. Long-term retention of the knowledge from the intervention was not evaluated.
CONCLUSIONS
The study conducted among the diabetic patients on insulin reported marked improvement in insulin administration knowledge and practice. Therapeutic modalities should incorporate these kinds of patient-centric paradigms of diabetes care and monitoring of patients’ adherence to therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The study was conducted as a part of the Short-term Studentship Project supported by ICMR, New Delhi.
REFERENCES
- 1.Mohan V, John M, Baruah M, Bhansali A. Addressing barriers to effective basal insulin therapy. J Assoc Physicians India. 2014;62(1 Suppl):10–4. [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva: Diabetes – Factsheet. 2015. [Last cited on 2015 Jan 19]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
- 3.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 4.Sosale A, Prasanna Kumar KM, Sadikot SM, Nigam A, Bajaj S, Zargar AH, et al. Chronic complications in newly diagnosed patients with type 2 diabetes mellitus in India. Indian J Endocrinol Metab. 2014;18:355–60. doi: 10.4103/2230-8210.131184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalra S, Balhara YP, Baruah MP, Chadha M, Chandalia HB, Chowdhury S, et al. Forum for injection techniques, India: The first Indian recommendations for best practice in insulin injection technique. Indian J Endocrinol Metab. 2012;16:876–85. doi: 10.4103/2230-8210.102929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12:14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: A review from the patient's perspective. Ther Clin Risk Manag. 2008;4:269–86. doi: 10.2147/tcrm.s1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piñeiro F, Gil V, Donis M, Torres MT, Orozco D, Merino J. Factors involved in noncompliance with drug treatment in non-insulin dependent diabetes mellitus. Aten Primaria. 1997;20:415–20. [PubMed] [Google Scholar]
- 9.Siminerio L. Strategies for Insulin Injection Therapy in Diabetes Self-Management. American Association of Diabetic Educators. 2011. [Last cited on 2016 Aug 24]. Available from: https://www.diabeteseducator.org/docs/default-source/legacy-docs/_resources/pdf/research/aade_meded.pdf?sfvrsn=2 .
- 10.Vimalavathini R, Agarwal SM, Gitanjali B. Educational program for patients with type-1 diabetes mellitus receiving free monthly supplies of insulin improves knowledge and attitude, but not adherence. Int J Diabetes Dev Ctries. 2008;28:86–90. doi: 10.4103/0973-3930.44079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health. [Last updated on 2013 Apr 06, Last accessed on 2016 Oct 24]. Available from: http://www.OpenEpi.com .
- 12.EpiData Software. Denmark. 2006-10. [Last cited on 2016 Jan 13]. Available from: http://www.epidata.dk/
- 13.Surendranath A, Nagaraju B, Padmavathi GV, Anand SC, Fayaz P, Balachandra G. A study to assess the knowledge and practice of insulin self-administration among patients with diabetes mellitus. Asian J Pharm Clin Res. 2012;5:63–6. [Google Scholar]


