Abstract
Aims:
To determine the prevalence of subclinical and overt hypothyroidism in diabetic kidney disease (DKD) and effect of thyroid hormone replacement on progression of DKD.
Materials and Methods:
A prospective cohort study on 41 adult DKD patients who were screened for hypothyroidism. Hypothyroid DKD patients were started on levothyroxine replacement and were reviewed after 3 and 6 months.
Results:
Of the total population, 14 (34.1%) cases were hypothyroid, among whom 12 (29.3%) cases were subclinical, and 2 (4.8%) were overt hypothyroidism. Prevalence of hypothyroidism and mean thyroid stimulating hormone levels increased with increasing severity of DKD. There were 2 (14.3%) hypothyroid cases in stage 3b, 4 (28.5%) cases in stage 4, and 8 (57.2%) in stage 5 DKD. The mean estimate glomerular filtration rate (ml/min/1.73 m2) at baseline was 13.6 ± 13.3 which increased to 16.4 ± 14.5 and 21.2 ± 15.3 after 3 and 6 months of thyroid hormone replacement therapy (THRT), respectively (P < 0.001).
Conclusions:
Hypothyroidism is commonly associated with DKD. Prevalence of hypothyroidism increased with declining renal function. THRT significantly improved renal function in DKD patients with hypothyroidism after 3 and 6 months of therapy.
Key words: Diabetic kidney disease, estimate glomerular filtration rate, hypothyroidism
INTRODUCTION
Thyroid hormones have significant impact on kidney disease, so it is important to consider the physiological association of thyroid dysfunction in relation to chronic kidney disease (CKD). CKD has been known to affect the pituitary-thyroid axis and the peripheral metabolism of thyroid hormones.[1] Primary hypothyroidism (nonautoimmune) is commonly observed in CKD patients. Especially, the prevalence of SCH Subclinical Hypothyroidism increases consistently with decline in estimated glomerular filtration rate (eGFR).[2]
The earliest and the most common thyroid function abnormality in CKD patients is a “low T3 syndrome” which occurs due to several reasons. However, the free T4 levels vary from being low to normal in CKD. This is primarily because of an impaired protein binding of T4 in CKD. The thyroid profile is similar to that observed in several nonthyroidal illnesses (NTIs) such as severe infections, heart failure, malignancies, and in several hospitalized patients without renal disease. This led to the consideration of a “sick euthyroid state” in CKD, which is now called “NTI.” However, unlike other NTI states, there is no increase in total rT3 levels in CKD.[3] Another difference from other NTIs is that the thyroid stimulating hormone (TSH) levels are elevated in CKD.
Thus, CKD patients have low T3 and normal or reduced T4 levels, and consequently elevated TSH and the attendant increase in thyroid gland volume.[3,4] The reduced T3 levels and associated complications without an increase in rT3, the reduced free T4 levels along with an elevated TSH, and hyporesponsiveness of TSH to thyrotropin-releasing hormone question the “euthyroid” state and raise the possibility of benefit from thyroid supplementation in CKD. There is still a lack of consensus in current guidelines on whether to treat SCH or not. In particular, little is known about the effect of thyroid hormone replacement on the changes in glomerular filtration rate in CKD patients with SH. Only one previous study has examined the prevalence of hypothyroidism among patients with CKD not requiring dialysis. Among a small group of patients with diabetic (n = 32) and nondiabetic (n = 31) nephropathy (defined by urinary protein excretion >0.5 g/day), 24% of study subjects had overt or subclinical (nonautoimmune) hypothyroidism, with a higher prevalence among patients with diabetes.[5] Though diabetes remains the most common cause of CKD globally, the prevalence and impact of treatment of hypothyroidism on diabetic kidney disease (DKD).
MATERIALS AND METHODS
With the permission of the institutional ethics committee, a prospective cohort study was conducted on adult (age ≥18 years) CKD patients (confirmed as per kidney disease outcomes quality initiative guidelines) attending outpatient and inpatient department of our tertiary care center at Allahabad, India. Patients with known thyroid dysfunction or subjects who were receiving concurrent treatment with drugs that could contribute to hypothyroidism (lithium, amiodarone, or iodine) were excluded. Demographic data were recorded, and a detailed history was taken from each patient including history of hypertension, diabetes mellitus, and previous episodes of acute kidney injury and symptoms of uremia. Clinical examination and baseline investigations were done for enrolled patients, which included complete blood count, serum electrolytes, serum urea, and creatinine (simultaneously, eGFR was calculated using MDRD* equation [GFR (mL/min/1.73 m2) = 186 × (serum creatinine [mg/dL])−1.154 × (age [years])−0.203 × (0.742 if female)),[6] Serum protein and albumin, thyroid function tests (fT3, fT4, TSH, anti-thyroperoxidase (TPO) antibody), serum intact parathyroid hormone, 24 h urine protein and fasting and prandial blood sugars. Hypothyroidism was defined as a TSH level >4 mU/l. Subclinical hypothyroidism was defined by a TSH >4 mU/l with normal fT3 level. The normal reference range for TPO antibody was <0.5 IU/mL.[7,8] The American Diabetes Association criteria 2015 were used for diagnosis of diabetes mellitus.[9] Furthermore, all patients had an ultrasonography of abdomen for renal size, echogenicity, and corticomedullary differentiation.
A total of 41 DKD patients who were not known hypothyroidism, were enrolled and screened for hypothyroidism. Patients diagnosed with hypothyroidism, both OH and SCH (qualifying the treatment recommendations)[7] were started on thyroid hormone replacement therapy (THRT) with levothyroxine in a dose of 1.6 µg/kg body weight (dose adjusted according to comorbidities) in both the above groups; and reassessment of eGFR was done after 3 and 6 months. Data were compiled and analyzed using GraphPad Prism Software Inc. version 6.0 with the level of significance being 0.05. Numerical data were analyzed using paired and unpaired Student's t-test while z-test for proportions and Chi-square test was used for nonparametric data. Repeated measures ANOVA were used to determine significant improvement in eGFR before and after THRT.
RESULTS
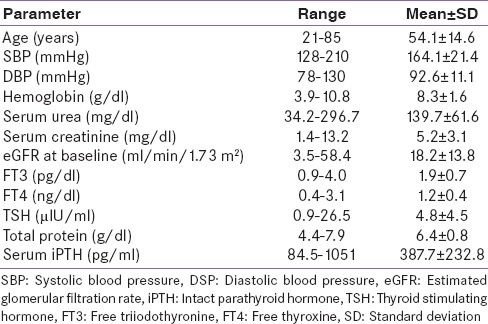
Mean age of study population was 54.12 ± 14.6 years with 70.7% patients being males. The demographic, clinical, and biochemical data of the study population at the time of commencement of thyroid hormone (baseline) are listed in Table 1.
Table 1.
Baseline characteristics of patients
A total of 41 DKD patients were enrolled, out of whom 14 (34.14%) patients were hypothyroid. 12 (29.3%) patients had subclinical hypothyroidism while 2 (4.8%) patients had overt hypothyroidism. Among these 14 patients, 9 patients were started on thyroxine replacement and were reviewed after 3 months and 6 months of thyroxine replacement. Prevalence of hypothyroidism increased with the declining renal function. There were 2 (14.3%), 4 (28.6%), and 8 (57.1%) patients with hypothyroidism in stage 3b, stage 4, and stage 5 of DKD, respectively.
Mean TSH levels also increased with declining renal function. There was a weak negative correlation between eGFR and serum TSH levels across various stages of DKD (r = −0.3801).
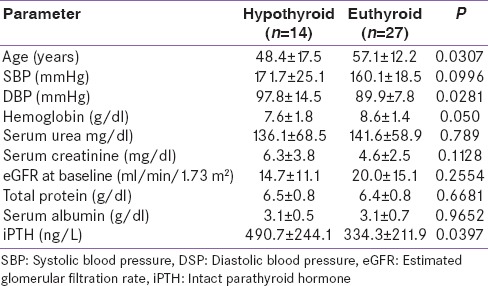
Table 2 shows a comparison of baseline parameters between hypothyroid and euthyroid DKD patients.
Table 2.
Comparison of baseline parameters between hypothyroid and euthyroid diabetic kidney disease
The eGFR (ml/min/1.73 m2) at baseline of DKD patients started on THRT was 13.67 ± 13.32 which increased to 16.38 ± 14.48 after 3 months of THRT and 21.24 ± 15.32 after 6 months of THRT (P = 0.0005).
DISCUSSION
Even though previous studies have demonstrated that restoration of euthyroidism has beneficial effects on cardiac dysfunction in patients with subclinical hypothyroidism [10] the impact of THRT on renal function has not been extensively explored in these patients. The results of this study show that thyroid hormone treatment significantly abrogated the decrease in eGFR in DKD patients with SCH and OH.
In this study, increased prevalence of SCH and OH was found in DKD (29.3% subclinical and 4.8% overt). Previous studies also confirm that subclinical hypothyroidism is not a rare disorder in CKD patients [2,11,12] The data of 14,623 adult participants from the third National Health and Nutrition Examination Survey, a nationally representative sample of the United States population, revealed that the prevalence of hypothyroidism increased with lower levels of GFR, occurring in 10.9% of patients with stage 2 CKD, 21.0% with stage 3 CKD, and 23.1% with stage 4 or 5 CKD.[2] Moreover, Chonchol et al.[13] showed that the prevalence of SCH increased from 7% at an eGFR 90 mL/min/1.73 m2–17.9% at an eGFR <60 mL/min/1.73 m2 in 3089 unselected outpatient adults. Similarly, in our study, the prevalence of hypothyroidism increased with declining levels of eGFR occurring in 2 (14.3%), 4 (28.6%), and 8 (57.1%) patients with hypothyroidism in Stage 3b, Stage 4, and Stage 5 of DKD, respectively. In the current study, we determined mean TSH levels across various stages of DKD to find a significant negative correlation (r = −0.3801) between eGFR and TSH concentrations, which was in accordance with previous studies.[14,15] The incidence of hypothyroidism is up to 4/1000 women and 1/1000 men and prevalence of overt hypothyroidism increases with age. SCH is found in 6–8% of women (10% over the age of 60 years) and 3% of men.[16] This clearly demonstrates the higher prevalence of hypothyroidism in patients with chronic renal dysfunction.
The effect of thyroid hormone, replacement on renal function, has not been widely investigated in hypothyroid DKD patients, especially in SCH. A recent study by Shin et al.[5] demonstrated that thyroid hormone treatment not only preserved renal function but was also an independent predictor of renal outcome. However, they compared changes in eGFR in two different study populations. Thus, to clarify the direct impact of thyroid hormone treatment on the decline in renal function, it was imperative to compare decline in eGFR before and after L-thyroxine replacement in the same patient. The results of this study showed that THRT significantly improved the renal function as evidenced by mean eGFR (ml/min/1.73 m2) which increased from 13.6 ± 13.3 to 16.4 ± 14.5 and 21.2 ± 15.3 after 3 and 6 months of THRT, respectively (P < 0.001).
CONCLUSIONS
Hypothyroidism is a prevalent condition in DKD with 34.14% of patients being hypothyroid in this study. Furthermore, the prevalence of hypothyroidism increases with declining renal function. Hypothyroid DKD patients were significantly younger in age as compared to euthyroid DKD patients. In our study, we found a significant improvement in renal function (evident by improvement in eGFR) in DKD patients with subclinical as well as overt hypothyroidism after THRT. Thus, we advocate thyroxine replacement in all DKD patients with hypothyroidism, both subclinical and overt.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kaptein EM. Thyroid function in renal failure. Contrib Nephrol. 1986;50:64–72. doi: 10.1159/000412989. [DOI] [PubMed] [Google Scholar]
- 2.Lo JC, Chertow GM, Go AS, Hsu CY. Increased prevalence of subclinical and clinical hypothyroidism in persons with chronic kidney disease. Kidney Int. 2005;67:1047–52. doi: 10.1111/j.1523-1755.2005.00169.x. [DOI] [PubMed] [Google Scholar]
- 3.Basu G, Mohapatra A. Interactions between thyroid disorders and kidney disease. Indian J Endocrinol Metab. 2012;16:204–13. doi: 10.4103/2230-8210.93737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh PA, Bobby Z, Selvaraj N, Vinayagamoorthi R. An evaluation of thyroid hormone status and oxidative stress in undialyzed chronic renal failure patients. Indian J Physiol Pharmacol. 2006;50:279–84. [PubMed] [Google Scholar]
- 5.Shin DH, Lee MJ, Lee HS, Oh HJ, Ko KI, Kim CH, et al. Thyroid hormone replacement therapy attenuates the decline of renal function in chronic kidney disease patients with subclinical hypothyroidism. Thyroid. 2013;23:654–61. doi: 10.1089/thy.2012.0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 7.Simon HS, Pearce A. ETA guideline: Management of subclinical hypothyroidism. Eur Thyroid J. 2013;2:215–28. doi: 10.1159/000356507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Thyroid Association ATA/AACE Guidelines for Hypothyroidism in Adults, Endocr Pract. 2012;18:988–1028. doi: 10.4158/EP12280.GL. [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association. Standard of medical care in diabetes. Diabetes Care. 2015;38(Suppl 1):S1–2. [Google Scholar]
- 10.Kaptein EM, Quion-Verde H, Chooljian CJ, Tang WW, Friedman PE, Rodriquez HJ, et al. The thyroid in end-stage renal disease. Medicine (Baltimore) 1988;67:187–97. doi: 10.1097/00005792-198805000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Haddow JE, Palomaki GE, Allan WC, Williams JR, Knight GJ, Gagnon J, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Eng J Med. 1999;341:549–55. doi: 10.1056/NEJM199908193410801. [DOI] [PubMed] [Google Scholar]
- 12.Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008;29:76–131. doi: 10.1210/er.2006-0043. [DOI] [PubMed] [Google Scholar]
- 13.Hardy MJ, Ragbeer SS, Nascimento L. Pituitary-thyroid function in chronic renal failure assessed by a highly sensitive thyrotropin assay. J Clin Endocrinol Metab. 1988;66:233–6. doi: 10.1210/jcem-66-1-233. [DOI] [PubMed] [Google Scholar]
- 14.Asvold BO, Bjøro T, Vatten LJ. Association of thyroid function with estimated glomerular filtration rate in a population-based study: The HUNT study. Eur J Endocrinol. 2011;164:101–5. doi: 10.1530/EJE-10-0705. [DOI] [PubMed] [Google Scholar]
- 15.Saini V, Yadav A, Arora MK, Arora S, Singh R, Bhattacharjee J. Correlation of creatinine with TSH levels in overt hypothyroidism - A requirement for monitoring of renal function in hypothyroid patients? Clin Biochem. 2012;45:212–4. doi: 10.1016/j.clinbiochem.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 16.Longo LD, Fauci AS. Harrison's Principles of Internal Medicine. 18th ed. Vol. 341. McGraw-Hill Companies; 2015. pp. 2918–9. [Google Scholar]


