Sir,
Primary hyperparathyroidism is a highly morbid condition and remains a disease curable by surgery in the vast majority of patients. Historically, bilateral neck exploration has been used as a method for surgical removal. However, since the Majority of patients have only one of the parathyroid glands enlarged, more focused minimally invasive parathyroidectomy is more commonly done.
This surgery requires very good presurgical parathyroid localization to be realized. Nuclear medicine studies have been at the forefront of parathyroid lesion localization for a very long time. Currently among the single-photon emission computed tomography (SPECT) tracers, the data supporting dual-phase technetium-99m (99m Tc)-sestamibi scintigraphy with early SPECT/CT is the most compelling. This technique has shown the highest sensitivity with good specificity and excellent histopathological correlation.[1,2]
Various studies have reported the sensitivity of this technique between 77% and 89%.[3,4] However, this technique also suffers from various shortcomings. These include a significant drop in sensitivity of the technique in very small parathyroid lesions, in postoperative patients, with thyroid adenomas and in certain adenomas with unusually fast sestamibi washout.[5,6,7]
Thus, In certain patients 99mTc-Sestamibi dual phase with early SPECT/CT may be unable to localize parathyroid adenomas. Consequently, there has been a search for tracers which may potentially be able to improve upon the weaknesses of current investigations. Investigations such as 11C-methionine positron emission tomography/CT (PET/CT) have shown good results.[8] In addition, radiological investigations such as ultrasonography and more recently four-dimensional computed tomography have been used for good effect in the preoperative localization of parathyroid lesions.
The most recent nuclear medicine technique to be used for this indication is 18F-fluorocholine PET/CT. Initial studies with his tracer have yielded extremely promising results in research papers.[9,10]
Even at our own institution, use of 18F-fluorocholine PET/CT has been yielding encouraging results showing excellent correlation with final surgical histopathology findings.
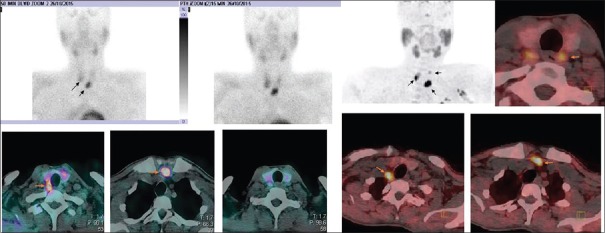
A 58-year-old male patient with a nonsestamibi concentrating lesion on SPECT/CT and planar images underwent 18F-fluorocholine PET/CT. On the PET images, the lesion was well localized and showed good radiotracer concentration. Subsequent surgical resection proved the lesion to be a parathyroid adenoma [Figure 1].
Figure 1.
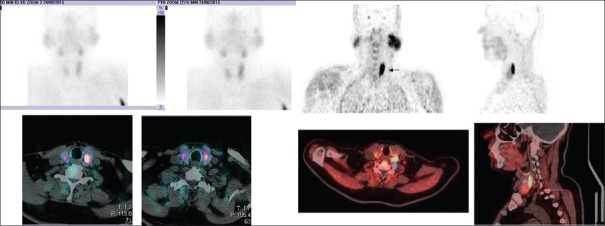
A 38-year-old patient of multiple endocrine neoplasia syndrome with two parathyroid lesions localized on technetium-99m-Sestamibi scan with early single-photon emission computed tomography/computed tomography. 18F-choline positron emission tomography/computed tomography of the same patient identified an additional parathyroid adenoma
In addition, in another 38-year-old male patient with multiple endocrine neoplasia syndrome, 99mTc-sestamibi localized two parathyroid lesions and 18F-fluorocholine PET/CT localized three lesions. Subsequent surgical pathology showed all three lesions to be parathyroid adenomas [Figure 2].
Figure 2.
A 58-year-old male with suspected primary hyperparathyroidism underwent a technetium-99m-sestamibi scan with early single-photon emission computed tomography/computed tomography, with no definite localization of adenoma. 18F-choline positron emission tomography/computed tomography of the same patient localized the parathyroid adenoma
These two cases exemplify the potential utility of this new investigation in primary hyperparathyroidism. This investigation may not just be useful in patients with the negative 99mTc-sestamibi scan, but may even add regarding additional lesion detection in patients with already positive 99mTc-sestamibi scans.
To conclude, 18F-fluorocholine PET/CT scans may have a potential role as a frontline investigation for localizing parathyroid adenomas and need further investigation in this role.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lavely WC, Goetze S, Friedman KP, Leal JP, Zhang Z, Garret-Mayer E, et al. Comparison of SPECT/CT, SPECT, and planar imaging with single-and dual-phase (99m) Tc-sestamibi parathyroid scintigraphy. J Nucl Med. 2007;48:1084–9. doi: 10.2967/jnumed.107.040428. [DOI] [PubMed] [Google Scholar]
- 2.Slater A, Gleeson FV. Increased sensitivity and confidence of SPECT over planar imaging in dual-phase sestamibi for parathyroid adenoma detection. Clin Nucl Med. 2005;30:1–3. doi: 10.1097/00003072-200501000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Gayed IW, Kim EE, Broussard WF, Evans D, Lee J, Broemeling LD, et al. The value of 99mTc-sestamibi SPECT/CT over conventional SPECT in the evaluation of parathyroid adenomas or hyperplasia. J Nucl Med. 2005;46:248–52. [PubMed] [Google Scholar]
- 4.Shafiei B, Hoseinzadeh S, Fotouhi F, Malek H, Azizi F, Jahed A, et al. Preoperative 99 mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism and concomitant nodular goiter: Comparison of SPECT-CT, SPECT, and planar imaging. Nucl Med Commun. 2012;33:1070–6. doi: 10.1097/MNM.0b013e32835710b6. [DOI] [PubMed] [Google Scholar]
- 5.Nichols KJ, Tomas MB, Tronco GG, Palestro CJ. Sestamibi parathyroid scintigraphy in multigland disease. Nucl Med Commun. 2012;33:43–50. doi: 10.1097/MNM.0b013e32834bfeb1. [DOI] [PubMed] [Google Scholar]
- 6.Witteveen JE, Kievit J, Stokkel MP, Morreau H, Romijn JA, Hamdy NA. Limitations of Tc99m-MIBI-SPECT imaging scans in persistent primary hyperparathyroidism. World J Surg. 2011;35:128–39. doi: 10.1007/s00268-010-0818-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta Y, Ahmed R, Happerfield L, Pinder SE, Balan KK, Wishart GC. P-glycoprotein expression is associated with sestamibi washout in primary hyperparathyroidism. Br J Surg. 2007;94:1491–5. doi: 10.1002/bjs.5882. [DOI] [PubMed] [Google Scholar]
- 8.Sundin A, Johansson C, Hellman P, Bergström M, Ahlström H, Jacobson GB, et al. PET and parathyroid L-[carbon-11]methionine accumulation in hyperparathyroidism. J Nucl Med. 1996;37:1766–70. [PubMed] [Google Scholar]
- 9.Michaud L, Balogova S, Burgess A, Ohnona J, Huchet V, Kerrou K, et al. A pilot comparison of 18F-fluorocholine PET/CT, ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: Influence of thyroid anomalies. Medicine (Baltimore) 2015;94:e1701. doi: 10.1097/MD.0000000000001701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lezaic L, Rep S, Sever MJ, Kocjan T, Hocevar M, Fettich J. 18 F-Fluorocholine PET/CT for localization of hyperfunctioning parathyroid tissue in primary hyperparathyroidism: A pilot study. Eur J Nucl Med Mol Imaging. 2014;41:2083–9. doi: 10.1007/s00259-014-2837-0. [DOI] [PubMed] [Google Scholar]