Abstract
Background
The purpose of this study was to identify potential health system solutions to suboptimal use of antihypertensive therapy in a diverse cohort of newly treated patients.
Methods
Using a hypertension registry at Kaiser Permanente Northern California, we conducted a retrospective cohort study of 44,167 adults (≥18 years) with hypertension who were new users of antihypertensive therapy in 2008. We used multivariate logistic regression analysis to model the relationships between race/ethnicity, specific health system factors and early non-persistence (failing to refill the first prescription within 90 days) and non-adherence (at least 80% of days covered during the 12 months following start of treatment), respectively, controlling for socio-demographic and clinical risk factors.
Results
More than 30% of patients were early non-persistent and one in five were non-adherent to therapy. Non-whites were more likely to exhibit both types of suboptimal medication taking behavior. In logistic regression models adjusting for sociodemographic, clinical and health system factors, non-white race was associated with both early non-persistence [Black Odds Ratio:1.56 (95% Confidence Interval: 1.43, 1.70); Asian OR: 1.40 (95% CI:1.29,1.51); Hispanic OR: 1.46 (95% CI:1.35,1.57)] and non-adherence, [Black Odds Ratio:1.54 (95% CI: 1.35, 1.75); Asian OR: 1.13 (95% CI:1.00,1.28); Hispanic OR: 1.48 (95% CI:1.33,1.65). However, the likelihood of early non-persistence among Asians and Hispanics varied by choice of first line therapy. In addition, racial and ethnic differences in non-adherence were appreciably attenuated when medication copay and mail order pharmacy use were accounted for in the models.
Conclusions
Racial and ethnic differences in medication taking behavior occur early in the course of treatment. However, health systems strategies designed to reduce patient copays, ease access to medications and optimize the choice of initial therapy may be effective tools in narrowing persistent gaps in the use of these and other clinically effective therapies.
Heart disease is the leading cause of death in the U.S., and costs more than $315 billion each year in health care costs and loss in productivity.1,2 Hypertension is a leading risk factor for heart disease and modest reductions in blood pressure have been associated with significant reductions in the risk of adverse cardiovascular events such as stroke, coronary heart disease and death.3 Despite the widespread availability of clinically efficacious medications for treating hypertension, fewer than one third of patients with hypertension achieve recommended levels of blood pressure control.4
Some racial and ethnic subgroups may be at higher risk for inadequate blood pressure control and lower rates of antihypertensive adherence, even in settings with somewhat equal access to care.5–9 Suboptimal use of antihypertensives can occur at any stage in the process, from picking up the first prescription to making adherence a part of everyday life.4 However, because long term adherence is dependent upon persistence with therapy at an early stage of treatment, early non-persistence may present a critical opportunity for identifying practices and policies with the potential to reduce disparities in cardiovascular outcomes.
The purpose of this study is to identify potential health system solutions to suboptimal adherence and persistence with antihypertensive medications at an early stage of treatment among a diverse cohort of hypertension patients with equal access to health insurance. Identifying potentially modifiable health system-level determinants of appropriate medication use across racial and ethnic groups could inform the development of interventions designed to reduce disparities in hypertension control.
Methods
Setting and Study Population
This retrospective cohort study was conducted at Kaiser Permanente Northern California (KPNC), an integrated health care delivery system serving more than 3.3 million people. From a hypertension registry including nearly 1.3 million patients from the year 2000 through 2009 identified through a complex algorithm including diagnosis codes and consecutive blood pressure measurements,10 we included 44,167 adults (≥18 years) who were new users of antihypertensive therapy (defined as no evidence of an antihypertensive drug dispensing during the previous eight-year period) in 2008. We excluded 7,818 (13.9%) patients who were not continuously enrolled and who did not have an active drug benefit on the date therapy was started and for at least 250 days following the therapy start date to ensure adequate follow up. We allowed for gaps in drug coverage of no more than 60 days. We also excluded 4,288 (7.6%)patients who were hospitalized at any point in that same time period.
Data Sources
The hypertension registry included clinical databases extracted from integrated electronic medical records at KPNC. Ambulatory pharmacy data included the date of prescription of medications and refill information. In this closed pharmacy system, patients have a strong financial incentive to fill prescriptions at a health plan pharmacy, with more than 95% of members obtaining prescription medications in-house.11,12
Definition of Outcome Measures
We identified three stages of suboptimal medication taking behavior among newly treated patients: primary non-adherence, early non-persistence, and non-adherence. Primary non-adherence was defined as being prescribed a new antihypertensive medication, but failing to fill the prescription within two months of the date it was ordered. Early non-persistence was defined as filling the first prescription, but failing to refill of an antihypertensive medication within 90 days of the date of the first filled prescription for that medication. Patients who switched medications within the first 90 days of initiating therapy were not included in the calculation of primary non-adherence or early non-persistence.
Non-adherence was defined as not having medication available for 20% or more of days during the 12 months following initiation of therapy. This measure was only calculated for patients continuously enrolled for at least 12 months following initiation of antihypertensive medication with at least one refill within the first 90 days (i.e., excluding patients with early non-persistence). Continuous gap measures are refill-based measures of non-adherence demonstrating high reliability and validity, particularly when both prescribing and dispensing data are used.13–15
As a secondary outcome we examined systolic blood pressure (SBP), a highly reliable measure of blood pressure control across age groups,16–20 taken within 90 days prior to the 12 month anniversary of the date of therapy start. Good control was defined as 140 mm Hg (< 130 mm Hg if diabetes or chronic kidney disease was present).
Key Covariates
Race and ethnicity are key covariates in this analysis and were available from both administrative sources and self-report. We classified patients as white (non-Hispanic) (37%), black (non-Hispanic) (6.9%), Asian (non-Hispanic) (8.8%), Hispanic (10.1%), and other or unknown (37.2%). The majority (99%) of patients who were categorized as other or unknown had missing race or ethnicity data.
We created three measures to represent potentially modifiable system level determinants of suboptimal medication taking behavior. First, we identified the level of expected co-payment for generic medications ($0–5, $6–10, more than $10 per prescription) for each patient. More than 95% of all prescribed antihypertensive agents were generics. We also assessed voluntary enrollment in a mail order pharmacy program, which included a financial incentive in the form of reduced copays for approximately 30% of patients. Mail order pharmacy was considered as a predictor of non-adherence only because enrollment in the program ruled out the possibility of early non-persistence (i.e., failure to refill the first prescription).
While the choice of initial antihypertensive therapy is influenced by patient and provider characteristics and preferences, therapeutic choice is also influenced by health system factors such as clinical guidelines and preferred drug lists. Therefore, we included the medication used in initiating therapy (diuretics, angiotensin-converting-enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta blockers, calcium channel blockers, and other agents, including alpha 1 adrenergic blockers, alpha 2 adrenergic agonists, and peripheral vasodilators) as a third factor that is potentially modifiable through health system intervention. Patients initiating on more than one agent (24%) were assigned to the agent listed first in the pharmacy record.
We further adjusted for factors that may be correlated with race and ethnicity including patient age and gender. We also created categorical variables representing the median household income (less than $40,000, $40,000–74,999, greater than or equal to $75,000) and average educational attainment (less than 10% with a college degree, 10–19%, 20–29%, or 30% or more) for each patient’s US Census 2000 block group of residence.
To control for severity of hypertension, we included the most recent SBP reading (<140mmHg, 140–149, 150–159, ≥160) recorded prior to the initiation of antihypertensive treatment, which was available for 93.4% of the study population. Patient reported smoking status (yes/no) and clinically assessed body mass index were also included.
We also included indicators for competing health care needs21 including several medical (cardiovascular disease, chronic kidney disease, diabetes) and mental health comorbidities (schizophrenia, bipolar disorder, anxiety, depression). We used the International Classification of Diseases, Ninth Edition (ICD-9)22 to identify conditions based on one inpatient or two outpatient diagnoses observed between 2000 and the date of initiation of antihypertensive therapy. Given challenges in identifying depression using medical records,23 we only counted depression diagnoses that occurred during the 12 month period prior to the initiation of antihypertensive medication and used dispensing of select antidepressant classes (tricyclics, serotonin reuptake inhibitors, norepinephrine reuptake inhibitors) to identify patients with possible depression.
We further controlled for variation in health services utilization by including a count of the number of medical office visits during the 12 months prior to starting antihypertensive therapy.
Statistical Analysis
We used logistic regression with time-dependent covariates to estimate early nonpersistence and non-adherence, respectively, among patients with hypertension who were new users of antihypertensive therapy. We first estimated the association between race and ethnicity and the primary outcomes controlling only for age and gender. To evaluate whether health system factors acted as potential mediators of the relationship between race/ethnicity and medication use, we sequentially added groups of covariates representing cardiovascular risk factors, socioeconomic status, medical comorbidity, psychiatric comorbidity, number of medical visits, and finally, the three key health system factors to the model and observed the effect on the coefficient for race/ethnicity. A relative change in the coefficient of 10% or greater was considered strong evidence of a mediating or explanatory factor.
We also tested for interactions between race/ethnicity and health system factors to test for possible effect modification using the log likelihood statistic. To facilitate the interpretation of statistically significant interactions, we used the estimates generated by the model with interaction terms to calculate predicted probabilities for each of the main outcomes for important racial/ethnic and medication subgroups. For this calculation, we set the remaining covariates to match the distribution of these factors among white patients and then graphically compared the resulting subgroups of interest. We used multiple imputation to address missing values for body mass index (28.2% missing) and baseline systolic blood pressure (6.6% missing)24 and compared the model results with and without imputed values.
Finally, we visually compared changes in SBP over time, stratifying by race/ethnicity and mediation persistence. All statistical analysis were conducted in SAS Version 9.1.25 This study was approved by the Institutional Review Board at Kaiser Foundation Research Institute.
Results
At the time they initiated therapy, systolic blood pressure was similar across racial and ethnic subgroups. [Table 1] Black and Hispanic patients were younger, more likely to be obese, and to have lower household income and educational attainment compared to other subgroups. Black and white patients were more likely to be active smokers. Rates of medical and psychiatric comorbidity were fairly similar by race and ethnicity.
Table 1.
Characteristics of Kaiser Permanente Northern California Enrollees Newly Initiated on Antihypertensive Medications in 2008 (N=44,167)
| ALL | White | Black | Asian | Hispanic | Other/Unknown | ||
|---|---|---|---|---|---|---|---|
| Total | 44,167 | 16,343 (37.0) | 3,036 (6.9) | 3,893 (8.8) | 4,479 (10.1) | 16,416 (37.2) | |
| Age | <50 | 18,122 (41.0) | 5,205 (31.9) | 1,650 (54.4) | 1,681 (43.2) | 2,330 (52.0) | 7,256 (44.2) |
| 50–64 | 18,817 (42.6) | 7,176 (43.9) | 1,112 (36.6) | 1,574 (40.4) | 1,584 (35.4) | 7,371 (44.9) | |
| 65–74 | 4,966 (11.2) | 2,506 (15.3) | 192 (6.3) | 462 (11.9) | 402 (9.0) | 1,404 (8.6) | |
| 75+ | 2,262 (5.1) | 1,456 (8.9) | 82 (2.7) | 176 (4.5) | 163 (3.6) | 385 (2.4) | |
| Gender | Male | 22,371 (50.7) | 7,870 (48.2) | 1,247 (41.1) | 1,590 (40.8) | 2,034 (45.4) | 9,630 (58.7) |
| Female | 21,796 (49.4) | 8,473 (51.8) | 1,789 (58.9) | 2,303 (59.2) | 2,445 (54.6) | 6,786 (41.3) | |
| Current Smoker | Yes | 4,653 (10.5) | 2,014 (12.3) | 473 (15.6) | 275 (7.1) | 409 (9.1) | 1,482 (9.0) |
| No | 39,514 (89.5) | 14,329 (87.7) | 2,563 (84.4) | 3,618 (92.9) | 4,070 (90.9) | 14,934 (91.0) | |
| BMI (kg/m2)* | <18.5 | 179 (0.6) | 86 (0.7) | <10 (0.2) | 39 (1.3) | 14 (0.4) | 35 (0.4) |
| 18.5–24.99 | 5,959 (18.8) | 2,522 (19.4) | 247 (10.6) | 1,083 (36.5) | 358 (9.9) | 1,749 (17.8) | |
| 25–29.99 | 10,893 (34.4) | 4,464 (34.4) | 634 (27.3) | 1,164 (39.3) | 1,093 (30.2) | 3,538 (36.1) | |
| ≥30 | 14,668 (46.3) | 5,922 (45.6) | 1,436 (61.8) | 679 (22.9) | 2,151 (59.5) | 4,480 (45.7) | |
| Missing (%) | 12,468 (28.2) | 3,349 (20.5) | 714 (23.5) | 928 (23.8) | 863 (19.3) | 6,614 (40.3) | |
| Household income | < $40K | 8304 (18.9) | 2553 (15.7) | 1158 (38.4) | 441 (11.4) | 1089 (24.5) | 3063 (18.8) |
| $40–74,999 | 24487 (55.7) | 9206 (56.6) | 1521 (50.4) | 2154 (55.6) | 2653 (59.6) | 8953 (54.9) | |
| ≥$75K | 11146 (25.4) | 4517 (27.8) | 339 (11.2) | 1280 (33.0) | 708 (15.9) | 4302 (26.4) | |
| Missing (%) | 230 (0.5) | 67 (0.4) | 18 (0.6) | 18 (0.5) | 29 (0.7) | 98 (0.6) | |
| College Degree | <10% | 9316 (21.2%) | 2708 (16.6%) | 1019 (33.7%) | 505 (13.0%) | 1599 (35.9%) | 3485 (21.4%) |
| 10–19% | 14960 (33.4%) | 5362 (32.9%) | 1032 (34.2%) | 1234 (31.9%) | 1643 (36.9%) | 5419 (33.2%) | |
| 20–29% | 11973 (27.5%) | 4778 (29.4%) | 681 (22.6%) | 1270 (32.8%) | 860 (19.3%) | 4384 (26.9%) | |
| ≥30% | 7955 (18.1%) | 3428 (21.1%) | 286 (9.5%) | 866 (22.4%) | 347 (7.8%) | 3028 (18.6%) | |
| Missing (%) | 353 (0.5%) | 67 (0.4%) | 18 (0.6%) | 18 (0.5%) | 30 (0.7%) | 100 (0.6%) | |
| Drug Copay: | $0–5 | 13833 (31.6) | 5126 (31.6) | 1346 (44.6) | 1303 (33.8) | 1348 (30.2) | 4710 (28.9) |
| $6–10 | 24434 (55.8) | 8495 (52.4) | 1413 (46.8) | 2107 (54.6) | 2568 (57.6) | 9851 (60.5) | |
| > $10 | 5547 (12.7) | 2581 (15.9) | 261 (8.6) | 447 (11.6) | 545 (12.2) | 1713 (10.5) | |
| Missing (%) | 353 (0.8) | 141 (0.9) | 16 (0.5) | 36 (0.9) | 18 (0.4) | 142\(0.9) | |
| Mail Order Pharmacy | 9856 (34.4) | 4704 (42.8) | 305 (18.4) | 626 (26.7) | 511 (20.2) | 3710 (33.4) | |
| Comorbid Conditions | Diabetes | 3,152 (7.1) | 1,239 (7.6) | 247 (8.1) | 348 (8.9) | 513 (11.5) | 805 (4.9) |
| Prior Cardiovascular Disease | 959 (2.2) | 638 (3.9) | 55 (1.8) | 73 (1.9) | 92 (2.1) | 101 (0.6) | |
| Chronic Kidney Disease | 909 (2.1) | 588 (3.6) | 49 (1.6) | 63 (1.6) | 88 (2.0) | 121 (0.7) | |
| Schizophrenia | 147 (0.3) | 69 (0.4) | 20 (0.7) | 14 (0.4) | 20 (0.5) | 24 (0.2) | |
| Bipolar Disorder | 338 (0.8) | 229 (1.4) | 17 (0.6) | <10 (0.2) | 27 (0.6) | 56 (0.3) | |
| Anxiety | 2,641 (6.0) | 1,386 (8.5) | 194 (6.4) | 195 (5.0) | 392 (8.8) | 474 (2.9) | |
| Depression | 1,484 (3.4) | 705 (4.3) | 104 (3.4) | 102 (2.6) | 183 (4.1) | 390 (2.4) | |
| Total outpatient visits† | 5.9 (10.2) | 8.0 (12.3) | 7.1 (11.8) | 6.3 (9.4) | 7.6 (11.8) | 2.9 (5.2) | |
| Mean SBP (sd)‡ | 144.3 (17.1) | 144.0 (17.0) | 145.1 (16.3) | 142.9 (17.2) | 143.5 (16.4) | 145.1 (17.5) | |
| Drug Class | Diuretics | 12320 (27.9) | 4441 (27.2) | 1176 (38.7) | 1098 (28.2) | 1207 (27.0) | 4398 (26.8) |
| Ace-Inhibitors | 19013 (43.1) | 6706 (41.0) | 1087 (35.8) | 1552 (39.9) | 2040 (45.6) | 7628 (46.5) | |
| ARBs | 1258 (2.9) | 365 (2.2) | 55 (1.8) | 139 (3.6) | 85 (1.9) | 614 (3.7) | |
| Beta Blockers | 7635 (17.3) | 3132 (19.2) | 431 (14.2) | 750 (19.3) | 763 (17.0) | 2559 (15.6) | |
| Calcium Channel Blockers | 32462 (5.6) | 910 (5.6) | 197 (6.5) | 227 (5.8) | 215 (4.8%) | 913 (5.6%) | |
| Others | 1479 (3.4) | 789 (4.8) | 90 (3.0) | 127 (3.3) | 169 (3.8) | 304 (1.9) |
BMI-Body Mass Index;
All outpatient visits during the 12 months prior to initiation of antihypertensive medication.;
Most recent blood pressure reading prior to initiation of antihypertensive medication.
ARBs-angiotensin II receptor blocker, Other category included: alpha 1 adrenergic blockers, alpha 2 adrenergic agonists, and peripheral vasodilators
Primary non-adherence (failing to fill a prescription) was generally low, affecting fewer than 5% of all patients and was similar across racial and ethnic subgroups [not shown]. Unadjusted prevalence of early non-persistence (Table 2, column 2) was 30.6% for whites, 42.5% for blacks, 38.1% for Asians, 41.1% for Hispanics, and 11.3 for patients with other or unknown race/ethnicity. Unadjusted prevalence of non-adherence (Tale 2, column 5) was highest for blacks (28.1%) and Hispanics (27.3%), compared with Asians (20.7%), patients of other or unknown race (19.2%) and whites (17.1%).
Table 2.
Log Odds of Non-Persistence and Non-Adherence among Kaiser Permanente Northern California Members Newly Treated with Antihypertensive Agents in 2008
| Early Non-Persistence | Non-Adherence | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Characteristics | Unadjusted Proportion | Age-Gender Adjusted | Fully Adjusted | Unadjusted Proportion | Age-Sex Adjusted | Fully Adjusted |
| White (ref) | 30.6 | -- | -- | 17.1 | -- | -- |
| Black | 42.5 | 1.59 (1.46 – 1.73) | 1.56 (1.43 – 1.70) | 28.1 | 1.74 (1.53 – 1.97) | 1.55 (1.37 – 1.77) |
| Asian | 38.1 | 1.36 (1.26 – 1.47) | 1.40 (1.29 – 1.51) | 20.7 | 1.20 (1.07 – 1.35) | 1.13 (1.00 – 1.28) |
| Hispanic | 41.1 | 1.48 (1.37 – 1.58) | 1.46 (1.35 – 1.57) | 27.3 | 1.67 (1.51 – 1.86) | 1.46 (1.31 – 1.63) |
| Other/Missing | 11.3 | 0.97 (0.92 – 1.02) | 1.07 (1.01 – 1.13) | 19.2 | 1.06 (0.99 – 1.15) | 1.01 (0.93 – 1.09) |
| Age<50, y (ref) | 39.1 | -- | -- | 24.8 | -- | -- |
| 50–64 | 28.7 | 0.66 (0.63 – 0.69) | 0.67 (0.64 – 0.70) | 17.5 | 0.64 (0.60 – 0.69) | 0.66 (0.62 – 0.71) |
| 65–74 | 28.1 | 0.64 (0.59 – 0.69) | 0.65 (0.60 – 0.71) | 15.2 | 0.56 (0.50 – 0.62) | 0.54 (0.48 – 0.61) |
| 75+ | 31.1 | 0.75 (0.68 – 0.83) | 0.75 (0.67 – 0.84) | 13.4 | 0.50 (0.42 – 0.59) | 0.48 (0.40 – 0.57) |
| Male (ref) | 33.1 | -- | -- | 20.4 | -- | -- |
| Female | 32.8 | 0.96 (0.92 – 1.00) | 0.94 (0.90 – 0.98) | 19.1 | 0.91 (0.85 – 0.97) | 0.95 (0.89 – 1.01) |
| Non Smoker (ref) | 32.3 | -- | 19.6 | -- | ||
| Smoker | 38.8 | 1.16 (1.09 – 1.24) | 21.0 | 1.02 (0.92 – 1.13) | ||
| Body Mass Index <24.99, kg/m2 (ref) | 37.3 | -- | 16.9 | -- | ||
| Overweight (25–29.99) | 35.7 | 0.90 (0.84 – 0.96) | 17.8 | 0.99 (0.89 – 1.11) | ||
| Obese (≥30) | 36.2 | 0.84 (0.78 – 0.90) | 21.1 | 1.08 (0.97 – 1.20) | ||
| Missing | 24.8 | 0.66 (0.60 – 0.72) | 21.0 | 1.10 (0.97 – 1.25) | ||
| Systolic blood pressure<140 (ref) | 33.5 | -- | 20.2 | -- | ||
| 140 – 149 | 36.4 | 1.06 (1.01 – 1.12) | 19.7 | 0.98 (0.90 – 1.06) | ||
| 150 – 159 | 33.3 | 0.96 (0.90 – 1.02) | 19.0 | 0.94 (0.86 – 1.03) | ||
| 160+ | 32.2 | 0.99 (0.93 – 1.06) | 18.5 | 0.92 (0.84 – 1.01) | ||
| Household Income< $40K | 35.9 | -- | 22.4 | -- | ||
| $40K – $ 74.9K | 33 | 0.92 (0.87 – 0.98) | 20.0 | 0.99 (0.91 – 1.09) | ||
| ≥ $75K | 30.9 | 0.91 (0.84 – 0.99) | 17.1 | 0.95 (0.84 – 1.07) | ||
| Bachelor’s Degree <10% | 36 | 22.8 | ||||
| 10–19% | 33.4 | 0.96 (0.90–1.02) | 20.7 | 1.00 (0.91–1.09) | ||
| 20–29% | 31.9 | 0.92 (0.86–0.99) | 18.3 | 0.95 (0.85–1.05) | ||
| ≥30% | 30.5 | 0.91 (0.83–0.99) | 16.7 | 0.90 (0.80–1.02) | ||
| No Diabetes | 32.6 | -- | 19.7 | -- | ||
| Diabetes | 37.9 | 1.11 (1.02 – 1.20) | 20.1 | 1.00 (0.88–1.13) | ||
| No Chronic Kidney Disease (CKD) | 33 | -- | 19.8 | -- | ||
| CKD | 33.6 | 1.01 (0.87 – 1.18) | 18.2 | 1.18 (0.93–1.48) | ||
| No Prior Cardiovascular | 33 | -- | 19.8 | -- | ||
| Disease (CVD) Prior CVD | 31.8 | 0.96 (0.82 – 1.11) | 16.8 | 1.06 (0.85–1.32) | ||
| No Concurrent Depression (ref) | 32.8 | -- | 19.7 | -- | ||
| Concurrent Depression | 38.4 | 1.09 (0.97 – 1.22) | 20.6 | 1.07 (0.90–1.28) | ||
| No Schizophrenia (ref) | 33 | -- | 19.8 | -- | ||
| Ever Schizophrenia | 32.4 | 0.76 (0.52 – 1.10) | 14.6 | 0.62 (0.34–1.14) | ||
| No Bipolar Disorder (ref) | 33 | -- | 19.7 | -- | ||
| Ever Bipolar Disorder | 38.1 | 1.05 (0.83 – 1.34) | 20.5 | 1.03 (0.71–1.50) | ||
| No Anxiety (ref) | 32.6 | -- | 19.7 | -- | ||
| Ever Anxiety | 38.9 | 1.10 (1.00 – 1.20) | 21.0 | 1.05 (0.91–1.20) | ||
| Medical Visits=0 (ref) | 27.7 | -- | 20.6 | -- | ||
| 1 to 2 | 34.6 | 1.03 (0.96 – 1.09) | 19.2 | 0.97 (0.89–1.07) | ||
| 3 to 5 | 36.3 | 1.08 (1.01 – 1.17) | 18.6 | 0.95 (0.85–1.06) | ||
| 6 to 15 | 40.9 | 1.29 (1.18 – 1.41) | 20.0 | 1.00 (0.87–1.15) | ||
| Medication Copay<$6 | 32.9 | -- | 18.3 | -- | ||
| $6–10 | 33.9 | 1.06 (1.01 – 1.11) | 20.8 | 1.19 (1.11–1.28) | ||
| $11+ | 29.1 | 0.96 (0.88 – 1.04) | 18.7 | 1.35 (1.20–1.52) | ||
| Drug Class Diuretic | 36.7 | 19.1 | ||||
| ACE Inhibitor | 32.8 | 0.88 (0.83–0.93) | 19.6 | 1.03 (0.95–1.11) | ||
| ARB | 17.3 | 0.48 (0.40–0.57) | 22.7 | 1.27 (1.04–1.55) | ||
| Beta blocker | 29.8 | 0.78 (0.73–0.83) | 20.1 | 1.09 (0.99–1.20) | ||
| Calcium Channel Blocker | 26 | 0.66 (0.60–0.74) | 19.9 | 1.09 (0.95–1.26) | ||
| Other | 45.1 | 1.49 (1.33–1.69 | 22 | 1.43 (1.18–1.73) | ||
| No Mail Order Pharmacy Use | NA* | NA | 23.0 | -- | ||
| Mail Order Pharmacy Use | NA | NA | 13.5 | 0.57 (0.53–0.61) | ||
By definition, patients who use mail order pharmacy received at least two refills and therefore cannot achieve the outcome of early non-persistence.
The modeling results for early non-persistence are presented in Table 2, columns 3 and 4. Adjusting for age and gender only (column 3), blacks (OR:1.59; (95% CI:1.46–1.73)), Asians (OR: 1.36 (1.26–1.47)), Hispanics (OR: 1.48 (1.37–1.58)), and patients of other or unknown race/ethnicity (OR:0.97 (0.92–1.02)) all had higher odds of early nonpersistence compared with whites. Sequential adjustment for cardiovascular risk factors, socioeconomic status, medical and psychiatric comorbidity, the frequency of medical visits, and health system factors did not attenuate the associations between race/ethnicity and early non-persistence (Table 2, Column 4)..
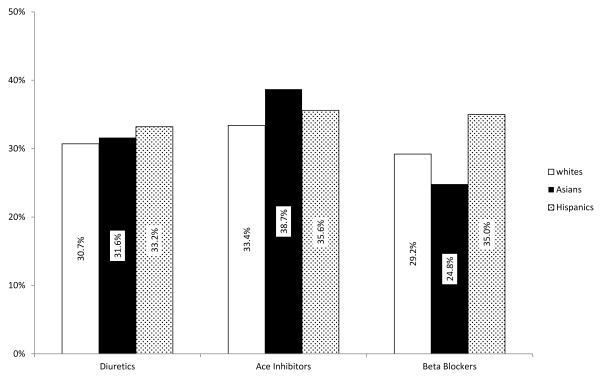
Medication copay and the choice of antihypertensive therapy were independently associated with early non-persistence. A copay of $6–10 was marginally associated with higher odds of early non-persistence relative to a copay under $6 [OR: 1.06 (1.01–1.11)]. Patients initiating on ARBs had a dramatically lower likelihood of early nonpersistence compared to patients initiating diuretics [OR:0.48 (0.40–0.57)]. Tests of interactions between race/ethnicity and these health system factors revealed modification of the race/ethnicity effect by type of medication used (Figure 1). Specifically, Asians using ACE-inhibitors had higher likelihood of early non-persistence (estimated proportion: 38.7%; interaction p value=0.0043) as did Hispanics who initiated on beta blockers (35%; p=0.0592). In contrast, Asians who initiated on beta blockers (24.8%; p=0.0015) had lower odds of early non-persistence with antihypertensive therapy.
Figure 1. Adjusted Proportion of Patients with Early Non-Persistence by Type of Antihypertensive Drug Class and Race and Ethnicity.
Table 2 Early Non-Persistence=Failure to refill a prescription within 90 days; Statistically significant interactions between race/ethnic categories and type of medication prescribed, where all other characteristics are set to the distribution for whites
Several sociodemographic and clinical factors were associated with early nonpersistence including younger age, male gender, smoking, having a BMI of less than 25, baseline SBP between 140 and 149, lower income (<$40,000), lower educational attainment (<10% bachelor’s degree), having diabetes, and having three or more medical visits during the 12 months prior to initiation of therapy. The results were robust to the inclusion of imputed values for BMI and baseline SBP.
Table 2, columns 6 and 7, show the results of the models predicting antihypertensive non-adherence. Adjusting for age and gender (column 6), race and ethnicity were associated with non-adherence, with Black (OR:1.74;95% CI:1.53–1.97), Asian (OR: 1.20 (1.07–1.35)) and Hispanic patients (OR: 1.67 (1.51–1.86)) all having higher odds of non-adherence compared with whites.
Medication copay, type of medication initiated and enrollment in mail order pharmacy were all associated with non-adherence. Copays of $6–10 [OR: 1.19 (1.11–1.28)] and $11 or more [OR:1.35 (1.20–1.52)] were associated with higher odds of non-adherence during the first year of therapy. Patients initiating on ARBs [OR:1.27 (1.04–1.55)] and other less commonly prescribed medications [OR:1.43 (1.18–1.73)] had higher odds of non-adherence compared to patients using diuretics. Enrollment in mail order pharmacy was associated with reduced odds of non-adherence [OR: 0.57 (0.53–0.61)].
The association between race/ethnicity and non-adherence was attenuated by the inclusion of information about copay status and mail order pharmacy use. After inclusion of these covariates, the associated between race/ethnicity and non-adherence was as follows: blacks OR:1.55 (1.37–1.77)], Asians OR:1.13 (1.00–1.28), Hispanics OR:1.46 (1.31–1.63)] and other/unknown OR:1.01 (0.93–1.09)]. We found no evidence of an interaction between health systems factors and race or ethnicity.
Results were robust to the inclusion of imputed BMI and baseline SBP. After adjustment for all covariates, the estimated proportion of patients who were non-adherent by race and ethnicity were as follows: Whites (16.7%), Blacks (28%), Asians (20.3%), Hispanics (26.9%), and other or unknown (18.9%).
Twelve months after starting therapy, blood pressure control improved for all patients. Fewer than 20% of patients were in poor control compared to more than 60% at baseline. Blacks who exhibited non-persistence with antihypertensive agents had the highest proportion of patients who were not in control at the end of follow up (28.2%). In contrast, Asians who were adherent to therapy had the lowest proportion of patients not in control after 12 months (14.1%). [data not shown]
Discussion
In this setting, we found higher rates of blood pressure control and lower rates of primary non-adherence compared to previous studies.26,27 Good blood pressure control in this setting have been cited previously and may be related to early detection, as well as payment mechanisms that financially reward physician groups based in part on the proportion of patients with good blood pressure control.28
Our finding of racial and ethnic differences in both early non-persistence and non-adherence are consistent with prior evidence.8,9,26,27 However, the interaction between race/ethnicity and medication type as predictors of early non-persistence is novel and may reflect unmeasured clinical factors, contraindications or treatment preferences that vary across racial and ethnic groups. 29–34 Whether variation in early non-persistence can be reduce through the use of decision tools and other strategies designed to better match patients with therapy deserves further exploration.
Our finding regarding the importance of mail order pharmacy as a potential policy level mechanism for improving adherence is consistent with previous studies in this and other settings.35–39 This study provides additional evidence that exposure to mail order pharmacy across racial and ethnic subgroups, rather than differential response to this practice, contributes to disparities in adherence.36 However, it is important to note that all patients using mail order pharmacy in this setting also had access to telephone based counseling from pharmacists and approximately one-third also received a financial incentive (i.e., lower copays) for participating in the program.36 Moreover, integrated electronic medical records may facilitate patient monitoring and continuity of care for patients receiving medications by mail. Future research is needed to explore the specific mechanisms by which mail order pharmacy may influence adherence across diverse care settings.
This study has some limitations that deserve consideration. First, we could not control for unmeasured physiological, behavioral and psychosocial factors that may explain some of the observed relationships between race/ethnicity and behavior. Also, we may have misclassified some patients based on inaccurate or missing race/ethnicity data and do not have sufficient information to hypothesize about differences among patients with missing demographic data. In addition, while the use of pharmacy records to estimate adherence is well-supported, we did not directly observe patient behavior. Therefore, to the extent that there is greater variation in actual versus estimated adherence, our findings may be biased. While it is possible that we misclassified some patients as having hypertension who did not have the condition, we believe that this possibility was reduced through the application of a complex algorithm for identify patients with hypertension in order to reduce any potential bias or noise relating to misdiagnosis.10
Evidence from recent disparities focused interventions in cardiovascular disease indicates that multi-faceted interventions to address barriers to self-management may be particularly effective, but provide little guidance as to which barriers are most amenable to change through health system intervention.40–45 Our findings suggest that health systems factors have the potential to reduce racial and ethnic differences in both early persistence and ongoing adherence to antihypertensive therapy. Medication cost and ease of access may be universally important modifiable determinants of ongoing adherence, suggesting that medication cost assistance may be a critical component of interventions to reduce cardiovascular related disparities. Importantly, these findings suggest that the strategies employed to reduce disparities in medication use should be tailored to the stage of treatment, recognizing that the relative importance of health system factors are likely to change over time as patients move from initiation of therapy to making adherence a part of their everyday lives.
We found evidence that health systems factors may play important roles as both mediators and modifiers of racial and ethnic differences in medication taking behavior. Unlike socioeconomic and psychosocial determinants that can be difficult to change, medication choice, copay and access are potentially modifiable through system level intervention and have the potential to reduce non-adherence, a well-known and especially challenging aspect of hypertension management in high risk populations.
Acknowledgments
This study was funded by [3U19HL091179-04S1] the National Heart, Lung, and Blood Institute and the National Institute for Mental Health as a supplement to the HMO Research Network Cardiovascular Disease Network. Additional support for Drs. Adams, Schmittdiel, and O’Connor was also provided by the Health Delivery Systems Center for Diabetes Translational Research [P30DK092924], funded by the National Institute for Diabetes, Digestive and Kidney Diseases. The funders had no role in the design or conduct of the study, data collection, management, analysis or interpretation, or in the preparation, review or approval of this manuscript. The authors report no conflicts of interest. Dr. Schmittdiel had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We also wish to thank Dr. Alan Go for comments on an earlier version of this manuscript and Ms. Karen R. Hansen for assistance with preparing this manuscript for submission.
References
- 1.LLoyd-Jones DAR, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart Disease and Stroke Statistics--2010 Update. Circulation. 2010;121:e1–e170. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Qureshi AI, Suri MF, Kirmani JF, Divani AA. Prevalence and trends of prehypertension and hypertension in United States: National Health and Nutrition Examination Surveys 1976 to 2000. Med Sci Monit. 2005 Sep;11(9):CR403–409. [PubMed] [Google Scholar]
- 3.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003 Jul 9;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 4.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004 Jul;19(4):357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 5.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000 Dec 19;102(25):3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 6.Fiscella K, Holt K. Racial disparity in hypertension control: tallying the death toll. Ann Fam Med. 2008 Nov-Dec;6(6):497–502. doi: 10.1370/afm.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams AS, Soumerai SB, Ross-Degnan D. Use of antihypertensive drugs by Medicare enrollees: does type of drug coverage matter? Health Aff (Millwood) 2001 Jan-Feb;20(1):276–286. doi: 10.1377/hlthaff.20.1.276. [DOI] [PubMed] [Google Scholar]
- 8.Bagchi AD, Esposito D, Kim M, Verdier J, Bencio D. Utilization of, and adherence to, drug therapy among medicaid beneficiaries with congestive heart failure. Clin Ther. 2007 Aug;29(8):1771–1783. doi: 10.1016/j.clinthera.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Batson B, Belletti D, Wogen J. Effect of African American race on hypertension management: a real-world observational study among 28 US physician practices. Ethn Dis. 2010 Autumn;20(4):409–415. [PubMed] [Google Scholar]
- 10.Go AS, Magid DJ, Wells B, Sung SH, Cassidy-Bushrow AE, Greenlee RT, Langer RD, Lieu TA, Margolis KL, Masoudi FA, McNeal CJ, Murata GH, Newton KM, Novotny R, Reynolds K, Roblin DW, Smith DH, Vupputuri S, White RE, Olson J, Rumsfeld JS, Gurwitz JH. The Cardiovascular Research Network: a new paradigm for cardiovascular quality and outcomes research. Circ Cardiovasc Qual Outcomes. 2008 Nov;1(2):138–47. doi: 10.1161/CIRCOUTCOMES.108.801654. [DOI] [PubMed] [Google Scholar]
- 11.Selby JV, Lee J, Swain BE, Tavel HM, Ho PM, Margolis KL, O’Connor PJ, Fine L, Schmittdiel JA, Magid DJ. Trends in time to confirmation and recognition of new-onset hypertension: 2000–2006. Hypertension. 2010;56:605–611. doi: 10.1161/HYPERTENSIONAHA.110.153528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saunders KW, Davis RL, Stergachis A. Group Health Cooperative. In: Strom BL, editor. Pharmacoepidemiology. 4. New York: Wiley; 2005. pp. 223–239. [Google Scholar]
- 13.Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008 Jan-Feb;11(1):44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 14.Hansen RA, Kim MM, Song L, Tu W, Wu J, Murray MD. Comparison of methods to assess medication adherence and classify nonadherence. Ann Pharmacother. 2009 Mar;43(3):413–422. doi: 10.1345/aph.1L496. [DOI] [PubMed] [Google Scholar]
- 15.Karter AJ, Parker MM, Moffet HH, Ahmed AT, Schmittdiel JA, Selby JV. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009 Oct;44(5 Pt 1):1640–1661. doi: 10.1111/j.1475-6773.2009.00989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Franklin SS, Gustin Wt, Wong ND, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997 Jul 1;96(1):308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 17.Wilking SV, Belanger A, Kannel WB, D’Agostino RB, Steel K. Determinants of isolated systolic hypertension. JAMA. 1988 Dec 16;260(23):3451–3455. [PubMed] [Google Scholar]
- 18.Sagie A, Larson MG, Levy D. The natural history of borderline isolated systolic hypertension. N Engl J Med. 1993 Dec 23;329(26):1912–1917. doi: 10.1056/NEJM199312233292602. [DOI] [PubMed] [Google Scholar]
- 19.Lee M-LTRB, Vokonas PS, Weiss ST. Longitudinal analysis of adult male blood pressure: The Normative Aging Study, 1963–1992. J Epidemiol Biostat. 1996;1:79–87. [Google Scholar]
- 20.Tate RB, Manfreda J, Krahn AD, Cuddy TE. Tracking of blood pressure over a 40-year period in the University of Manitoba Follow-up Study, 1948–1988. Am J Epidemiol. 1995 Nov 1;142(9):946–954. doi: 10.1093/oxfordjournals.aje.a117742. [DOI] [PubMed] [Google Scholar]
- 21.Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998 May 21;338(21):1516–1520. doi: 10.1056/NEJM199805213382106. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Health and Human Services CfDCaP, and the Centers for Medicare and Medicaid Services; U.S. Department of Health and Human Services; Centers for Disease Control and Prevention; Centers for Medicare and Medicaid Services. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) 2005–10 http://hdl.handle.net/1902.29/CD-0177.
- 23.Trinh NH, Youn SJ, Sousa J, et al. Using electronic medical records to determine the diagnosis of clinical depression. Int J Med Inform. 2011 Jul;80(7):533–540. doi: 10.1016/j.ijmedinf.2011.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inc. SI. SAS OnlineDoc 9.1. 2002–2003 http://support.sas.com/91doc/docMainpage.jsp.
- 26.Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens. 2009 Apr;22(4):392–396. doi: 10.1038/ajh.2008.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perreault S, Lamarre D, Blais L, et al. Persistence with treatment in newly treated middle-aged patients with essential hypertension. Ann Pharmacother. 2005 Sep;39(9):1401–1408. doi: 10.1345/aph.1E548. [DOI] [PubMed] [Google Scholar]
- 28.Lester H, Schmittdiel J, Selby J, Fireman B, Campbell S, Lee J, Whippy A, Madvig P. The impact of removing financial incentives from clinical quality indicators: longitudinal analysis of four Kaiser Permanente indicators. BMJ. 2010;340:c1898. doi: 10.1136/bmj.c1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999 Dec;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 30.Huang ES, Brown SE, Thakur N, et al. Racial/ethnic differences in concerns about current and future medications among patients with type 2 diabetes. Diabetes Care. 2009 Feb;32(2):311–316. doi: 10.2337/dc08-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schuz B, Wurm S, Ziegelmann JP, Warner LM, Tesch-Romer C, Schwarzer R. Changes in functional health, changes in medication beliefs, and medication adherence. Health Psychol. 2011 Jan;30(1):31–39. doi: 10.1037/a0021881. [DOI] [PubMed] [Google Scholar]
- 32.Lehane E, McCarthy G. Intentional and unintentional medication non-adherence: a comprehensive framework for clinical research and practice? A discussion paper. Int J Nurs Stud. 2007 Nov;44(8):1468–1477. doi: 10.1016/j.ijnurstu.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 33.Clifford S, Barber N, Horne R. Understanding different beliefs held by adherers, unintentional nonadherers, and intentional nonadherers: application of the Necessity-Concerns Framework. J Psychosom Res. 2008 Jan;64(1):41–46. doi: 10.1016/j.jpsychores.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 34.Schnittker J. Misgivings of medicine?: African Americans’ skepticism of psychiatric medication. J Health Soc Behav. 2003 Dec;44(4):506–524. [PubMed] [Google Scholar]
- 35.Duru OK, Schmittdiel JA, Dyer WT, Parker MM, Uratsu CS, Chan J, Karter AJ. Mail-order pharmacy use and adherence to diabetes-related medications. Am J Manag Care. 2010 Jan;16(1):33–40. [PMC free article] [PubMed] [Google Scholar]
- 36.Schmittdiel JA, Karter AJ, Dyer W, Parker M, Uratsu C, Chan J, Duru OK. The comparative effectiveness of mail order pharmacy use vs. local pharmacy use on LDL-C control in new statin users. J Gen Intern Med. 2011 Dec;26(12):1396–402. doi: 10.1007/s11606-011-1805-7. Epub 2011 Jul 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Devine S, Vlahiotis A, Sundar H. A comparison of diabetes medication adherence and healthcare costs in patients using mail order pharmacy and retail pharmacy. J Med Econ. 2010 Jun;13(2):203–211. doi: 10.3111/13696991003741801. [DOI] [PubMed] [Google Scholar]
- 38.Pittman DG, Tao Z, Chen W, Stettin GD. Antihypertensive medication adherence and subsequent health care utilization and cost. Am J Manag Care. 2010;16(8):568–576. [PubMed] [Google Scholar]
- 39.Zhang L, Zakharyan A, Stockl KM, Harada AS, Curtis BS, Solow BK. Mail order pharmacy use and medication adherence among Medicare Part D beneficiaries with diabetes. J Med Econ. 2011;14(5):562–7. doi: 10.3111/13696998.2011.598200. Epub 2011 Jul 6. [DOI] [PubMed] [Google Scholar]
- 40.Svarstad BL, Kotchen JM, Shireman TI, et al. The Team Education and Adherence Monitoring (TEAM) trial: pharmacy interventions to improve hypertension control in blacks. Circ Cardiovasc Qual Outcomes. 2009 May;2(3):264–271. doi: 10.1161/CIRCOUTCOMES.109.849992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ogedegbe G, Schoenthaler A, Richardson T, et al. An RCT of the effect of motivational interviewing on medication adherence in hypertensive African Americans: rationale and design. Contemp Clin Trials. 2007 Feb;28(2):169–181. doi: 10.1016/j.cct.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 42.Cooper LA, Roter DL, Bone LR, et al. A randomized controlled trial of interventions to enhance patient-physician partnership, patient adherence and high blood pressure control among ethnic minorities and poor persons: study protocol NCT00123045. Implement Sci. 2009;4:7. doi: 10.1186/1748-5908-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cutrona SL, Choudhry NK, Fischer MA, et al. Modes of delivery for interventions to improve cardiovascular medication adherence. Am J Manag Care. 2010;16(12):929–942. [PMC free article] [PubMed] [Google Scholar]
- 44.Crook ED, Bryan NB, Hanks R, et al. A review of interventions to reduce health disparities in cardiovascular disease in African Americans. Ethn Dis. 2009 Spring;19(2):204–208. [PMC free article] [PubMed] [Google Scholar]
- 45.Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007 Oct;64(5 Suppl):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]