Supplemental Digital Content is available in the text
Keywords: blood pressure, lifetime risk, risk assessment, stroke
Abstract
Objective:
Stroke is a major cause of premature death in China. Early prevention of stroke requires a more effective method to differentiate the stroke risk among young-aged and middle-aged individuals than the 10-year risk of cardiovascular disease. This study aimed to establish a lifetime stroke risk model and risk charts for the young-aged and middle-aged population in China.
Methods:
The Chinese Multi-Provincial Cohort Study participants (n = 21 953) aged 35–84 years without cardiovascular disease at baseline were followed for 18 years (263 016 person-years). Modified Kaplan–Meier method was used to estimate the mean lifetime stroke risk up to age of 80 years and the lifetime stroke risk according to major stroke risk factors for the population aged 35–60 years.
Results:
A total of 917 participants developed first-ever strokes. For the participants aged 35–40 years (98 stroke cases), the lifetime stroke risk was 18.0 and 14.7% in men and women, respectively. Blood pressure most effectively discriminated the lifetime stroke risk. The lifetime risk of stroke for the individuals with all risk factors optimal was 8–10 times lower compared with those with two or more high risk factors at age 35–60 years at baseline.
Conclusion:
In young-aged and middle-aged population, the lifetime stroke risk will keep very low if major risk factors especially blood pressure level is at optimal levels, but the risk substantially increases even with a slight elevation of major risk factors, which could not be identified using 10-year risk estimation.
INTRODUCTION
Stroke is the leading cause of death in China. In an international comparison, China ranked third among 19 countries in terms of premature death from stroke [1]. A recent national screening in China found that 54% of stroke patients were less than 65 years of age in community population [2]. Prevention of premature stroke in the young-aged and middle-aged population must be prioritized in the development of a Chinese public health strategy to achieve a 25% reduction in premature death from noncommunity disease by the year 2025, a goal proposed by the WHO [3].
A proper stroke risk assessment method is important for the development of such a prevention strategy in the young-aged and middle-aged population. However, there are notable disadvantages of currently available cardiovascular risk assessment models for the risk assessment in the younger population. First, most of these models are used for assessment of a short-term (5-year or 10-year) total cardiovascular disease (CVD) risk [4–7]. For the young-aged and middle-aged individuals, almost all of them belong to the low-risk category based on the 10-year CVD risk assessment even they have significantly elevated risk factors and increased lifetime CVD risk [4,8]. Second, risk prediction models are only available for the total CVD risk, which combine the risk of stroke with coronary heart disease [4,6]. Rare stroke-specific risk assessment tool is available for either the short-term or long-term risk in China.
Newly updated CVD prevention and treatment guidelines have recommended the lifetime risk of CVD as an adjunction to 10-year risk estimation to distinguish the risk [9–11]. The lifetime risk estimation can not only serve as a tool for individuals to know their long-term risk that was caused by the accumulated damage of risk factors, but also as a basis to differentiate those at higher risk than 10-year risk estimation in clinical practice. Japan and America have developed stroke-specific models for lifetime risk assessment [12,13]. The lifetime stroke risk estimation tools would be urgently needed for the early stroke prevention in China. Moreover, as the SPRINT reported, the relative risk of the first occurrence of stroke was 11% lower with the intensive intervention than with the standard treatment but had no statistical significance (P = 0.50) [14]. The impact of maintaining a SBP less than 120 mmHg on stroke risk in larger population is needed. Therefore, this study aimed to establish a lifetime stroke risk model and risk charts for the young-aged and middle-aged population in China and provide the cerebral vascular benefit when maintaining multiple risk factors especially a blood pressure (BP) in optimal level based on a long-term cohort study.
METHODS
Study population
The participants in this study came from the Chinese Multi-Provincial Cohort Study, a nationwide, multicenter, open-cohort study on CVD including three cohorts. The largest cohort began at 1992 and included 16 811 participants aged 35–64 years who were free of CVD at baseline. The detailed methodology of the sampling has been described in previous publications [15,16]. From 1996 to 1999, 3129 participants aged 35–64 years who were free of CVD at baseline were added, and 2013 participants (45.7% older than 60 years) aged 35–84 years and free of CVD at baseline were added in 2004 to increase the sample size of elderly people. For the present study, we included 21 953 participants aged 35–80 years for the lifetime risk assessment.
All methods for the baseline survey were in accordance with the WHO-MONICA protocol [16]. All participants received informed consent letters to participate in this study at baseline. The lifetime risk of stroke study was approved by the ethics committee of Beijing Anzhen Hospital, Capital Medical University (approval number: 2015012X) and performed in accordance with the standards set forth by the Declaration of Helsinki.
All participants were invited to undergo a face-to-face follow-up every 1 or 2 years from the baseline examination to 31 December 2010. Follow-up rates were 81.5% for the cohort that completed the baseline survey in 1992, and 80.1 and 73.5% for the cohorts that completed the baseline survey in 1996–1999 and 2004, respectively.
Risk factor measurement at baseline
At the baseline survey, the information about demographics, smoking status, family history of CVD, and treatment histories of dyslipidemias and hypertension were collected using a standardized questionnaire and administered by trained researchers. Regular mercury sphygmomanometers were calibrated to measure BP at baseline. Standard cuff bladders with the width of 12.0–12.5 cm and the length of 22 cm were used. Participants were allowed to sit for 5 min in a quiet room before measuring BP. In all patients, BP was measured in the right arm, and at least two measurements were performed at 30-s intervals. Additional measurements were taken if the first two measurements were quite different. Both arms were measured to detect possible differences, and the higher value was used as the reference value if the patient had a peripheral vascular disease. The mean BP values indicated the mean SBP and mean DBP, which were the average levels of two consecutive SBP and DBP measurements [6,17,18]. Weight and height were measured and used to calculate the BMI [18,19]. We collected overnight fasting venous blood samples for the measurement of serum lipid and glucose concentrations. An enzymatic method was used to determine the fasting glucose, total cholesterol (TC), and triglyceride levels, and the phosphotungstic acid/MgCl2 precipitation method was used to determine the HDL-cholesterol (HDL-C) level. The non-HDL-C level was calculated by subtracting the HDL-C from the TC level. Quality control of the laboratory tests was performed by following the protocol of the WHO Regional Lipid Reference Center [20,21].
The combination of risk factors included BP (both SBP and DBP were considered), serum lipid indicators (non-HDL-C and HDL-C), BMI, smoking, and diabetes. Participants were stratified into five mutually exclusive categories based on whether they had all optimal risk factor levels, one or more nonoptimal risk factors, one or more elevated risk factors, one high risk factor only, or two or more high risk factors (the detail definitions were shown at the footnote) according to the stratification criteria of the Framingham Heart Study but some risk factors were adjusted on the basis of the estimation of stroke risk in Chinese population [22]. When low HDL-C (<1.03 mmol/l) and overweight/obesity (BMI from 24 to 28 kg/m2 and BMI ≥ 30 kg/m2) were included in the aggregate risk factor model, lifetime risk for stroke were discriminated better, so BMI and HDL-C being added into aggregate risk factor model. Non-HDL-C replaced TC because it provided better prediction for lifetime risk of stroke in Chinese population.
Case ascertainment
Stroke events were diagnosed as rapidly developing signs of focal (or global) disturbances in cerebral function lasting more than 24 h (unless interrupted by surgery or death) with no apparent nonvascular cause [23]. All fatal and nonfatal acute stroke events were reported; including hemorrhagic and ischemic strokes and unspecified cerebrovascular diseases (ICD-9 codes 430–434 and 436 or ICD-10 codes I60–I64). Hemorrhagic stroke was defined as a stroke event with a diagnosis of subarachnoid hemorrhage or intracerebral hemorrhage; ischemic stroke was defined as a stroke event with a diagnosis of thrombosis or embolism. Transient ischemic attack and chronic cerebral vascular disease were excluded [24].
All other causes of death except stroke were also reported and registered. All reported deaths and suspected stroke events were reviewed by a panel of physicians and neurologists according to the original medical records.
Statistical analysis
Modified Kaplan–Meier method was used to calculate the 10-year and lifetime risk of stroke [25]. The lifetime risk of stroke up to age 80 years was calculated at each index age ranging from 35 to 60 years, and the lifetime risk of stroke at the index ages of 35, 45, and 55 years could represent the age groups of 35–40, 41–50, and 51–60 years, respectively. The risk of all other causes of death except that from stroke is considered to be a competing risk, which was adjusted. The age of 80 years was defined as the end of the lifetime span for mean life expectancy was only 73 years in 2010 in China, which could represent most of Chinese lifetime [26]. The possible impact of antihypertensive treatment was also considered. An additional analysis was performed by classifying the participants receiving antihypertensive therapy as a high-risk group regardless of their BP level.
According to the International Atherosclerosis Society guidelines in 2013 [11], the lifetime risk of CVD can be stratified into low risk (<15%), moderate risk (15–30%), moderately high risk (30–45%), and high risk (≥45%). Because the risk stratification was developed for CVD and not stroke, we performed a recalibration by multiplying the proportion of stroke (70%) of the total acute CVD events in our study. Therefore, we classified the lifetime stroke risk into four risk levels: low risk (<10%), moderate risk (10–20%), moderately high risk (20–30%), and high risk (≥30%). All statistical analyses were performed with SAS 9.2 statistical software (SAS Institute, Inc., Cary, North Carolina, USA).
RESULTS
Baseline and follow-up information
The study included 11 366 men and 10 587 women with complete risk factor data at baseline. The participants were followed up for a total of 263 016 observational person-years (the median follow-up years were 18.0, 8.0, and 6.0 for participants who completed the baseline survey in 1992, 1996–1999, and 2004, respectively.).
During the follow-up, 917 participants developed first-ever acute stroke events, including 681 ischemic strokes, 221 hemorrhagic strokes, and 49 unspecified stroke events (33 participants had both ischemic strokes and hemorrhagic strokes). Out of 1401 deaths of participants, 198 were due to acute stroke events. Among the stroke cases, 161 (17.6%) were from age group 35–45 years, 298 (32.5%) were from age group 45–55 years, 434 (47.3%) were from age group 55–65 years, and 24 (2.6%) were older than 65 years. Baseline characteristics of these participants are shown in Table 1.
TABLE 1.
Baseline characteristics of the study population (n = 21 953)
| Variable | Men (n = 11 366) | Women (n = 10 587) |
| Age (year) | 48.9 ± 9.0 | 47.3 ± 8.8 |
| SBP, mean ± SD (mmHg) | 124.8 ± 19.5 | 122.8 ± 21.4 |
| DBP, mean ± SD (mmHg) | 81.6 ± 12.0 | 78.8 ± 11.8 |
| TC, mean ± SD (mmol/l) | 4.8 ± 1.0 | 4.8 ± 1.0 |
| Non-HDL-C, mean ± SD (mmol/l) | 3.4 ± 1.0 | 3.4 ± 1.0 |
| HDL-C, mean ± SD (mmol/l) | 1.3 ± 0.4 | 1.4 ± 0.4 |
| Triglycerides, median (mmol/l) | 1.3 | 1.1 |
| BMI, mean ± SD (kg/m2) | 24.1 ± 3.2 | 24.2 ± 3.4 |
| Fasting glucose, mean ± SD (mmol/l) | 5.2 ± 1.4 | 5.2 ± 1.4 |
| Smoking (%) | 5928 (52.2) | 385 (3.6) |
| Diabetes (%) | 932 (8.2) | 473 (7.1) |
| Antihypertensive medication (%) | 923 (8.1) | 1038 (9.8) |
| Risk factor profilesa | ||
| All risk factors optimal | 417 (3.7) | 1448 (13.7) |
| ≥1 Risk factor not optimal | 943 (8.3) | 1846 (17.4) |
| ≥1 Risk factor elevated | 6014 (52.9) | 4028 (38.0) |
| 1 High risk factor | 2792 (24.6) | 2286 (21.6) |
| ≥2 High risk factor | 1200 (10.5) | 979 (9.3) |
HDL-C, HDL-cholesterol; non-HDL-C, non-HDL-cholesterol; TC, total cholesterol.
aOptimal risk factors are defined as SBP less than 120 mmHg, DBP less than 80 mmHg, non-HDL-C less than 3.11 mmol/l, BMI less than 24 kg/m2, HDL-C at least 1.04 mmol/l, nonsmoker, and no diabetic. Not optimal risk factors are defined as SBP from 120 to 139 mmHg, DBP from 80 to 89 mmHg, non-HDL-C from 3.11 to 4.14 mmol/l, nonsmoker, and no diabetic. Elevated risk factors are defined as SBP from 140 to 159 mmHg, DBP from 90 to 99 mmHg, non-HDL-C from 4.14 to 5.18 mmol/l, BMI from 24 to 28 kg/m2, smoker, and diabetic. High risk factors are defined SBP at least 160 mmHg, DBP at least 100 mmHg, non-HDL-C at least 5.18 mmol/l, BMI at least 28 kg/m2, and HDL-C less than 1.04 mmol/l.
Lifetime risk of stroke for men and women
Figure 1 presented the 10-year and lifetime risk of stroke for the index age groups 35–40, 41–50, and 51–60 years, respectively. The lifetime stroke risks were 18.0% and 14.7% for men and women aged 35–40 years, which were 25.7 and 29.4 times higher than their 10-year stroke risks, 0.7 and 0.5%, respectively. The lifetime risks of ischemic stroke and hemorrhagic stroke were also estimated as shown in Supplementary Table 1. As to stroke subtypes, the lifetime risk of ischemic stroke was higher than that of hemorrhagic stroke.
FIGURE 1.
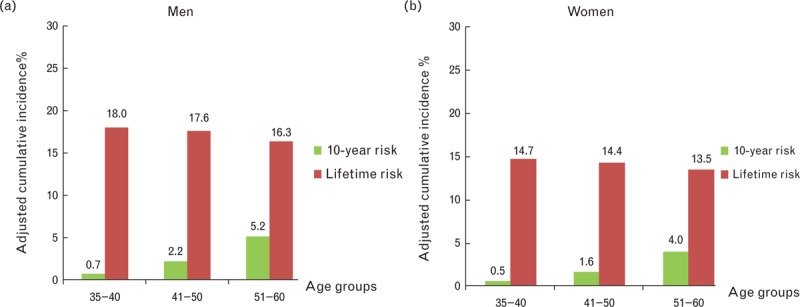
Ten-year and lifetime risk of stroke (all types) for men and women at the index ages.
Lifetime risk of stroke according to single risk factors
The lifetime risk of stroke was estimated in different index age groups for men and women according to single risk factors (Table 2). Among the traditional risk factors, BP had the strongest capacity to differentiate the lifetime stroke risk among young-aged and middle-aged population. In men aged 35–40 years, the lifetime risks of stroke were 10.7 and 38.4% in the lowest and highest BP categories, respectively; those in women were 8.3 and 26.7%, respectively. In all index ages, the lifetime risk of stroke increased as the BP increased in a dose–response pattern. In comparison, the 10-year stroke risk was only 2.9 and 1.6% in men and women in the highest BP categories at the same age (Supplementary Table 2). When all participants receiving antihypertensive therapy were assigned to the SBP at least 160 mmHg or DBP at least 100 mmHg group, the lifetime risk of stroke was the same as the previous results (Supplementary Table 3). We also estimated the lifetime stroke risk according to BP with or without other risk factors (Fig. 2). The association of BP with the lifetime risk of stroke was much stronger than all other risk factors combined.
TABLE 2.
The lifetime risk of stroke up to age 80 years for men and women at age 35–60 years according to single risk factor level at baseline
| Lifetime risk at age 35–40 years, 95% CI | Lifetime risk at age 41–50 years, 95% CI | Lifetime risk at age 51–60 years, 95% CI | ||||
| Variable | Men | Women | Men | Women | Men | Women |
| SBP/DBP (mmHg) | ||||||
| <120 and <80 | 10.7 (6.1–14.6) | 8.0 (3.8–11.8) | 10.6 (6.0–14.5) | 7.9 (3.7–11.7) | 10.0 (5.4–14.0) | 7.4 (3.2–11.3) |
| 120–139 or 80–89 | 14.3 (10.2–17.7) | 12.8 (7.1–17.8) | 14.1 (9.9–17.5) | 12.6 (6.9–17.7) | 13.1 (8.9–16.6) | 11.4 (5.6–16.6) |
| 140–159 or 90–99 | 20.4 (15.9–24.0) | 17.1 (12.9–20.8) | 19.7 (15.3–23.3) | 15.5 (11.6–19.0) | 17.5 (13.0–21.2) | 13.9 (10.0–17.4) |
| ≥160 or ≥100 | 38.4 (31.4–43.8) | 26.7 (18.1–33.7) | 37.3 (30.2–42.7) | 26.1 (17.5–33.1) | 33.6 (26.2–39.2) | 23.4 (14.6–30.6) |
| Non-HDL-C (mmol/l) | ||||||
| <3.11 | 15.4 (11.9–18.3) | 17.7 (8.3–25.5) | 15.1 (11.6–18.0) | 17.6 (8.1–25.4) | 14.0 (10.7–17.1) | 16.7 (7.1–24.7) |
| 3.11–4.14 | 15.8 (13.0–18.1) | 13.2 (10.1–15.9) | 15.7 (12.9–18.1) | 12.8 (9.8–15.5) | 14.0 (11.2–16.4) | 11.7 (8.7–14.5) |
| 4.14–5.18 | 19.5 (14.7–23.8) | 15.0 (7.1–21.6) | 18.4 (13.7–22.6) | 14.9 (7.0–21.6) | 16.7 (11.9–20.9) | 14.0 (6.0–20.8) |
| ≥5.18 | 22.2 (13.5–29.4) | 14.5 (7.6–20.8) | 21.9 (13.3–29.2) | 14.5 (7.6–20.8) | 20.6 (11.9–28.0) | 13.4 (6.7–19.7) |
| HDL-C (mmol/l) | ||||||
| <1.04 | 21.6 (15.4–26.5) | 17.5 (11.9–22.4) | 21.5 (15.3–26.4) | 16.8 (11.2–21.7) | 19.5 (13.2–24.7) | 15.4 (9.8–20.4) |
| 1.04–1.55 | 18.1 (14.9–20.6) | 16.9 (12.1–21.0) | 17.9 (14.7–20.4) | 16.8 (12.0–20.9) | 16.7 (13.5–19.3) | 12.5 (9.8–15.0) |
| ≥1.55 | 13.4 (9.9–16.3) | 7.4 (5.5–9.3) | 12.5 (9.1–15.4) | 7.0 (5.1–8.9) | 11.4 (8.0–14.3) | 6.3 (4.4–8.2) |
| BMI (kg/m2) | ||||||
| <24 | 14.4 (11.2–17.0) | 9.6 (6.5–12.3) | 14.0 (10.8–16.6) | 9.4 (6.3–12.2) | 13.3 (10.0–15.9) | 8.7 (5.6–11.5) |
| 24–28 | 18.4 (15.0–21.3) | 17.1 (11.0–22.4) | 18.1 (14.7–21.0) | 16.9 (10.7–22.1) | 16.7 (13.2–19.6) | 15.8 (9.5–21.2) |
| ≥28 | 31.1 (20.4–39.2) | 23.5 (12.5–32.4) | 30.9 (20.1–39.0) | 22.6 (11.5–31.6) | 27.5 (16.3–36.2) | 20.8 (9.4–30.2) |
| Diabetes | ||||||
| No | 17.6 (14.9–19.7) | 14.1 (10.9–16.9) | 17.4 (14.6–19.5) | 13.9 (10.6–16.8) | 16.0 (13.3–18.2) | 12.9 (9.7–15.8) |
| Yes | 21.6 (14.5–27.3) | 18.5 (7.0–27.4) | 20.9 (13.9–26.7) | 19.3 (6.6–29.5) | 19.2 (12.1–25.0) | 16.3 (4.6–25.9) |
| Smoker | ||||||
| No | 16.4 (13.4–18.9) | 14.8 (11.4–17.7) | 16.0 (13.0–18.6) | 14.6 (11.1–17.5) | 14.8 (11.8–17.4) | 13.6 (10.1–16.6) |
| Yes | 20.4 (15.5–23.9) | 14.9 (6.5–22.3) | 20.1 (15.2–23.7) | 14.9 (6.5–22.3) | 18.9 (13.9–22.6) | 12.4 (4.7–19.1) |
CI, confidence interval; HDL-C, HDL-cholesterol; non-HDL-C, non-HDL-cholesterol.
FIGURE 2.
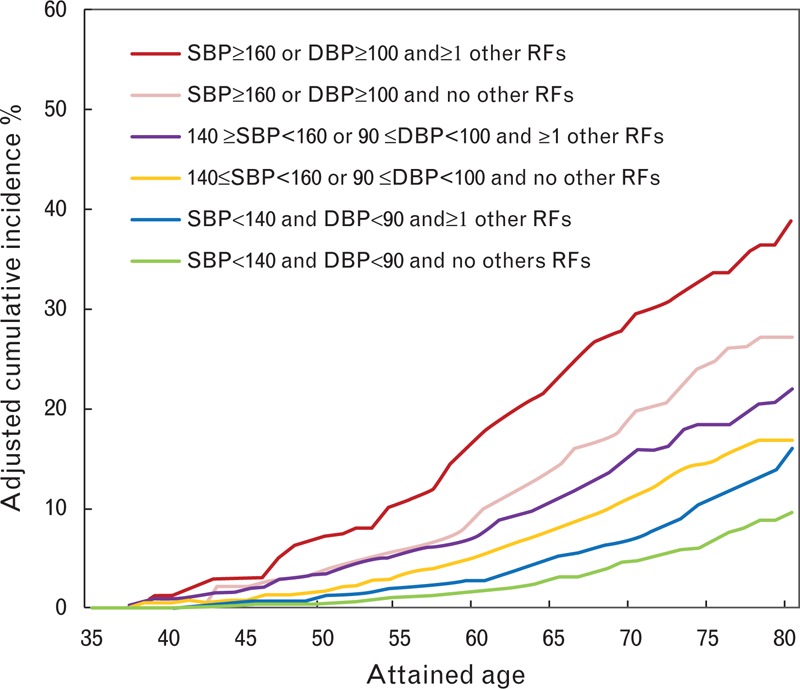
Ten-year risk and lifetime risk of stroke (all types) for Chinese population at age 35 years according to different blood pressure levels. ∗Other risk factors (RFs) were smoking, fat, and diabetes.
An increased non-HDL-C concentration was associated with an increased lifetime stroke risk in men. However, the non-HDL-C concentration could not discriminate the lifetime stroke risk well in women. The BMI, HDL-C concentration, and diabetes status could well discriminate the lifetime stroke risk in both men and women, but the smoking status could not well discriminate the lifetime risk of stroke especially in women.
Lifetime risk of stroke according to aggregate risk factor burden
The integrated effects of risk factors on the lifetime risk of stroke were estimated for men and women in the index age groups 35–40, 41–50, and 51–60 years. For individuals at the index age of 35–40 years, the lifetime risk of stroke was only 3.1 and 1.3% for men and women, respectively, with all risk factors optimal. However, the lifetime risk of stroke was 18.7 and 17.6% for men and women, respectively, with one or more nonoptimal risk factors, which was significantly higher than those with all risk factors optimal (Fig. 3). Among individuals with two or more high risk factors at an index age of 35–40 years, 41.6% of men and 24.6% of women were predicted to have an acute stroke event before the age of 80 years. The comparison of 10-year stroke risk and lifetime stroke was shown in Supplementary Table 4.
FIGURE 3.
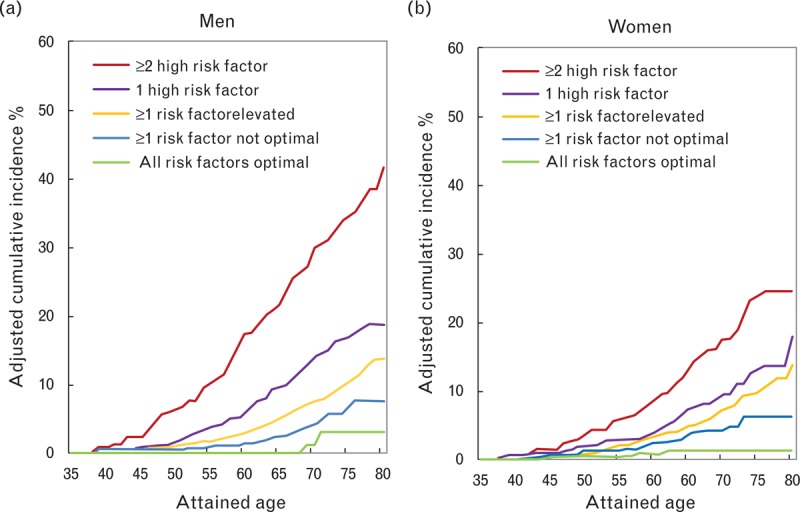
The cumulative incidence and lifetime risk of stroke for men and women by profiles of multiple risk factors at age 35–40 years.
The chart for lifetime risk of stroke
A color chart for lifetime risk of stroke was developed (shown in Fig. 4). An individual with different risk profiles at different ages could easily find the specific stroke risk (categories) during his/her remaining life to the age of 80 years. For men in the 35–40 and 41–50 years age groups, with all risk factors at optimal levels, the stroke risk is almost 0 before the age of 65 years. In comparison, men in the same age group with two or more high risk factors will achieve the same level stroke risk 30 years earlier.
FIGURE 4.
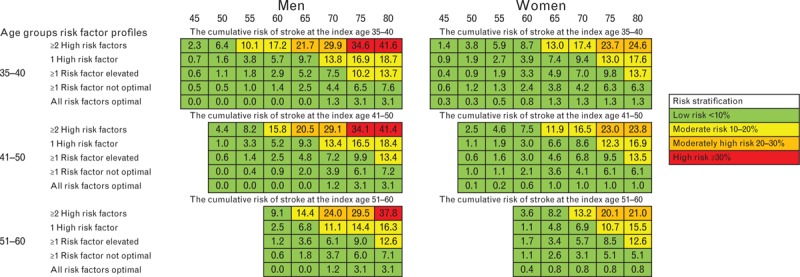
The lifetime risk chart of stroke for men and women by profiles of multiple risk factors at age 35–60 years.
Among all new stroke cases occurred during the follow-up years, the proportions of low risk is 6.9%, moderate risk is 65.3%, and high risk is 27.8%, respectively, based on lifetime risk estimation, respectively; however, less than 0.7% of stroke patients were classified as high-risk using the 10-year risk assessment for CVD.
DISCUSSION
Our data underline the importance of preventing the traditional risk factors’ development at younger ages to increase healthy longevity. We first estimated the lifetime risk of stroke for young-aged and middle-aged people in Chinese population according to the status of known stroke risk factors and developed a novel lifetime risk chart for stroke.
We support lifetime risk estimation as an adjunct to 10-year risk estimation, which has been recommended in the updated guidelines [9–11]. Risk intervention should be focused and performed throughout a patient's lifetime. The 10-year risk of stroke might mislead the young-aged and middle-aged population to ignore their stroke risk because more than 95% of them were considered to be low-risk based on the 10-year risk estimation of CVD. Moreover, our study strongly supports the concept that age is a modifiable risk factor [27]. The lifetime risk of stroke was extremely low in men and women with all major risk factors at optimal levels, almost not affected by age for the stroke risk almost no change as age increased from the index ages to 80 years.
In addition, our study reinforces the maximum benefits obtained from the prevention and management of traditional risk factors. However, only 3.7 and 13.7% of men and women in this study had major risk factors at optimal levels, and 68% of those with all risk factors at optimal levels were younger than 45 years. This study indicates that the stroke burden in China can be effectively relieved if the proportion of individuals with all risk factors at optimal levels substantially increases.
As to the effect of risk factors on stroke, abnormal BP levels can cover up the effects of other risk factors on the lifetime risk of stroke. This is consistent with our previous study of 10-year risk estimation of CVD [28]. Will lower BP reduce the risk of CVD has been debated [14,29]. Our results show that the lifetime risk of stroke was significantly lower for those with optimal BP than those with prehypertension or hypertension from the perspective of lifetime risk estimation. The finding is in accordance with those newly published from the SPRINT research among patients at high risk of CVD [14]. However, we provided the benefit evidence of maintaining a SBP less than 120 mmHg in the younger Chinese population. The smoking status could not well discriminate the lifetime risk of stroke; however, that does not mean that smoking has no overall effect on stroke. Numerous epidemiological evidences have shown that smoking was associated with a substantially higher short-term risk for stroke. However, the competing risk of death over the longer term substantially existed; the smoker might die from nonstroke causes like lung diseases associated with smoking before they suffer a stroke. Moreover, participants who quit smoking subsequently may make their stroke risk low, thereby lowering the lifetime risk of stroke in smokers group.
Another major contribution is that we developed a risk chart and proposed risk stratification based on the lifetime risk of stroke at the index age of 35–60 years. This risk chart provides visibility of the long-term damage of stroke among individuals aged 35–60 years with certain risk factors. These individuals can identify their risk based on risk factor profiling.
The lifetime stroke risk for Chinese individuals is similar to that of Japanese individuals and obviously higher than that of white individuals at the same index age [12,13]. The lifetime stroke risk reported here is likely to be a conservative estimate of the true Chinese population burden of stroke. The increased life expectancy and influence of a Western lifestyle might increase the risk of stroke [30].
There are some limitations of the present study. First, atrial fibrillation can increase the risk of ischemic stroke [31], but it was not included in the lifetime stroke risk model because of the lack of records at the baseline of our study. Second, as a long-term cohort study, it is very hard to keep the lost follow-up rate at a very low level. There was 26.5% lost follow-up rate in the cohort of baseline survey in 2004, even that cohort accounted only 9.2% of the total cohort population. Third, BP measurements were performed in populations of multicenter. Even a series of procedures were performed to ensure high-quality BP measurement, the Bland–Altman analyses, an important statistical method to compare the consistency of BP measurement between centers and investigators, were not performed before the baseline survey. Fourth, only part of the cohort population received re-examinations for the risk factor level. Therefore, we may not be able to evaluate the impacts from the changes of risk factor levels over time by the time-derived analysis. Finally, the association between the risk factors we selected as major risk factors and lifetime risk of stroke may differ from other populations. Therefore, the exploration of these results to other populations may not be suitable.
In conclusion, the lifetime risk of stroke model could discriminate the stroke risk well in young-aged and middle-aged Chinese people. The lifetime risk was extremely low in men and women with all major risk factors at optimal levels, with almost no change with the increase in age, which indicated that the stroke had huge potential can be prevented. Based on that, a risk chart for stroke was developed in the young-aged and middle-aged population, which could be used in stroke prevention in China.
ACKNOWLEDGEMENTS
We appreciate the contribution of the research participants in the study.
Sources of funding: The research work was supported by the China National Grant on Science and Technology (85-915-01-02), funding from China Beijing Municipal Bureau of Science and Technology (953850700), the China National Science & Technology Pillar Program for the Eleventh Five-year Plan (2006BAI01A01 and 2006BAI01A02), the China National Science & Technology Pillar Program for the Twelfth National Five-Year Plan (nos. 2011BAI08B01 and 2011BAI11B03), and National Program on Key Basic Research Project of China (2012CB517806).
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Reviewers’ Summary Evaluations
Reviewer 1
Study aimed to establish a lifetime stroke risk model for young and middle-aged population in China. A large cohort of 21 953 subjects aged 35–84 years without CVD at baseline was followed for 18 years. The mean lifetime stroke risk was 18.0% in men and 14.7% in women aged 35–40 years. BP most effectively discriminated the lifetime stroke risk. The lifetime stroke risk in subjects with optimal risk factor profile was 8–10 times lower than those with >2 high risk factors at baseline. Limitations are: extrapolation of results to subjects with ages different from 35–60 years, or to non-Chinese, and the lost follow-up rate of 9.2% of the total cohort. Also the non-inclusion of atrial fibrillation in the model, which is an important risk factor for ischemic stroke, is a weakness. Lifetime risk of stroke model could discriminate the stroke risk better than 10-year risk models in young and middle-aged Chinese people.
Reviewer 2
Stroke is or is rapidly going to become the major cardiovascular event, the most expensive, that related to the worst quality of residual life, and that which better responds to blood pressure control. Reduction of blood pressure at a population level is mandatory in this respect, although this goal is achieved in a limited number of cases. As high blood pressure is often associated to other risk factors, a multitasking action on cardiovascular risk is the right approach to primary stroke prevention.
Footnotes
Abbreviations: BP, blood pressure; CHD, coronary heart disease; CMCS, the Chinese Multi-Provincial Cohort Study; CVD, cardiovascular disease; HDL-C, HDL-cholesterol; non-HDL-C, non-HDL-cholesterol
REFERENCES
- 1.Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990–2010: findings from the global burden of disease study 2010. Lancet 2013; 381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Longde W, Ling Y, Yang H, Yi Z, Yongjun W, Xunming J, et al. Fixed-dose combination treatment after stroke for secondary prevention in China: a national community-based study. Stroke 2015; 46:1295–1300. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Noncommunicable diseases country profiles 2014. 2014; http://www.who.int/topics/noncommunicable_diseases/en/http://www.who.int/topics/noncommunicable_diseases/en/. [Accessed December 1, 2015]. [Google Scholar]
- 4.Wei W, Dong Z, Jin L, Guixian W, Zechun Z, Jun L, et al. Prospective study on the predictive model of cardiovascular disease risk in a Chinese population aged 35–64. Zhonghua Xin Xue Guan Bing Za Zhi 2003; 31:902–908. [Google Scholar]
- 5.Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003; 24:987–1003. [DOI] [PubMed] [Google Scholar]
- 6.Liu J, Hong Y, D’Agostino RB, Sr, Wu Z, Wang W, Sun J, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multiprovincial Cohort Study. JAMA 2004; 291:2591–2599. [DOI] [PubMed] [Google Scholar]
- 7.D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001; 286:180–187. [DOI] [PubMed] [Google Scholar]
- 8.Di Castelnuovo A, Costanzo S, Persichillo M, Olivieri M, de Curtis A, Zito F, et al. Distribution of short and lifetime risks for cardiovascular disease in Italians. Eur J Prev Cardiol 2012; 19:723–730. [DOI] [PubMed] [Google Scholar]
- 9.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Sr, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129 (25 Suppl 2):S49–S73. [DOI] [PubMed] [Google Scholar]
- 10.JBS3 Board Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014; 100 (Suppl 2):ii1–ii67. [DOI] [PubMed] [Google Scholar]
- 11.International Atherosclerosis Society Global recommendations for the management of dyslipidemia. 2015; www.athero.orgwww.athero.org. [Accessed December 1, 2015]. [Google Scholar]
- 12.Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The lifetime risk of stroke: Estimates from the Framingham study. Stroke 2006; 37:345–350. [DOI] [PubMed] [Google Scholar]
- 13.Turin TC, Kokubo Y, Murakami Y, Higashiyama A, Rumana N, Watanabe M, Okamura T. Lifetime risk of stroke in Japan. Stroke 2010; 41:1552–1554. [DOI] [PubMed] [Google Scholar]
- 14.Wright JT, Jr, Williamson JD, Whelton PKSJ, Sink KM, Rocco MV, Reboussin DM, et al. SPRINT Research Group A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Y, Liu J, Wang W, Wang M, Qi Y, Xie W, et al. Lifetime risk for cardiovascular disease in a Chinese population: the Chinese Multiprovincial Cohort Study. Eur J Prev Cardiol 2015; 22:380–388. [DOI] [PubMed] [Google Scholar]
- 16.Wu Z, Yao C, Zhao D, Wu G, Wang W, Liu J, Zeng Z. Cardiovascular disease risk factor levels and their relations to CVD rates in China – results of Sino-MONICA project. Eur J Cardiovasc Prev Rehabil 2004; 11:275–283. [DOI] [PubMed] [Google Scholar]
- 17.Hense HW, Koivisto AM, Kuulasmaa K, Zaborskis A, Kupsc W, Tuomilehto J. Assessment of blood pressure measurement quality in the baseline surveys of the WHO MONICA project. J Hum Hypertens 1995; 9:935–946. [PubMed] [Google Scholar]
- 18.Ren J, Grundy SM, Liu J, Wang W, Wang M, Sun J, et al. Long-term coronary heart disease risk associated with very-low-density lipoprotein cholesterol in Chinese: the results of a 15-year Chinese Multiprovincial Cohort Study (CMCS). Atherosclerosis 2010; 211:327–332. [DOI] [PubMed] [Google Scholar]
- 19.Zhao D, Grundy SM, Wang W, Liu J, Zeng Z, Wu Z. Ten-year cardiovascular disease risk of metabolic syndrome without central obesity in middle-aged Chinese. Am J Cardiol 2007; 100:835–839. [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Wang W, Wang M, Sun J, Li Y, Qi Y, et al. Impact of diabetes, high triglycerides and low HDL cholesterol on risk for ischemic cardiovascular disease varies by LDL cholesterol level: a 15-year follow-up of the Chinese Multiprovincial Cohort Study. Diabetes Res Clin Pract 2012; 96:217–224. [DOI] [PubMed] [Google Scholar]
- 21.Wu Z, Yao C, Zhao D, Wu G, Wang W, Liu J, et al. Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China, Part i: Morbidity and mortality monitoring. Circulation 2001; 103:462–468. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 2006; 113:791–798. [DOI] [PubMed] [Google Scholar]
- 23.Asplund K, Tuomilehto J, Stegmayr B, Wester PO, Tunstall-Pedoe H. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta Med Scand Suppl 1988; 728:26–39. [DOI] [PubMed] [Google Scholar]
- 24.Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol 2009; 8:345–354. [DOI] [PubMed] [Google Scholar]
- 25.Beiser A, D’Agostino RB, Sr, Seshadri S, Sullivan LM, Wolf PA. Computing estimates of incidence, including lifetime risk: Alzheimer's disease in the Framingham Study. The Practical Incidence Estimators (PIE) macro. Stat Med 2000; 19:1495–1522. [DOI] [PubMed] [Google Scholar]
- 26.Li GQ, Fan J, Liu J, Wang W, Wang M, Qi Y, et al. Impact of cerebrovascular disease mortality on life expectancy in China. Biomed Environ Sci 2014; 27:169–175. [DOI] [PubMed] [Google Scholar]
- 27.Kannel WB. Sixty years of preventive cardiology: a Framingham perspective. Clin Cardiol 2011; 34:342–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu YF, Zhao D, Zhou BF, Wang W, Li X, Liu J, et al. Cut offs and risk stratification of dyslipidemia in Chinese adults. Zhonghua Xin Xue Guan Bing Za Zhi 2007; 35:428–433. [PubMed] [Google Scholar]
- 29.Huang Y, Cai X, Li Y, Su L, Mai W, Wang S, et al. Prehypertension and the risk of stroke: a meta-analysis. Neurology 2014; 82:1153–1161. [DOI] [PubMed] [Google Scholar]
- 30.Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol 2007; 6:456–464. [DOI] [PubMed] [Google Scholar]
- 31.Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am 2008; 92:17–40.ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


