Abstract
Purpose
Prenatal stress can have a lasting effect on women’s mental health after childbirth. The negative effects may be particularly salient in women from low income and ethnic minority backgrounds, who are at increased risk for postpartum depression. However, social support may have the potential to attenuate the negative impact of stress.
Methods
The present study evaluated 269 Mexican American women (ages 18–42; 83% Spanish-speaking; median income $10,000–$15,000) for prenatal stress (daily hassles, family stress, partner stress, and culture-specific stress) in relation to depressive symptoms six weeks postpartum. Prenatal social support was examined as a buffer against the impact of prenatal stress.
Results
Partner stress, family stress, and daily hassles uniquely predicted depressive symptoms. Moderate and high levels of social support attenuated risk for depression due to family stressors.
Conclusions
Prenatal interpersonal and daily stressors negatively impact the mental health of women after birth, but social support can mitigate some of these effects. Among Mexican American pregnant women, effective interpersonal support and stress management may be associated with reduced risk for postpartum depression.
INTRODUCTION
Stress is well-linked to depressive symptoms and may be a particularly salient risk factor for depression for pregnant and postpartum women. Up to 60% of pregnant women report increases in negative mood and anxiety symptoms (Faisal-Cury and Menezes 2007), with postpartum depression (PPD) estimated to occur in 10–15% of the general population (Nonacs and Cohen 1998; O’Hara and Swain 1996). PPD rates of 23–59% have been reported among low income or ethnic minority women (Hobfoll et al. 1995). Prenatal stress has been shown to have stronger effects than prenatal maternal depressive symptoms on mother’s postpartum distress (Matthey et al. 2004) as well as child outcomes, such as low birth weight, preterm delivery, and other birth complications (Dunkel Schetter 2011). Particular subtypes of stress may be more harmful than others for expectant mothers (Milgrom et al. 2008), underscoring a need to identify the most impactful stressors to inform prevention and health promotion strategies. Major predictors for postpartum depression in general populations include low-economic status, general perceived life stress, and poor social support, which uniquely predict depressive symptoms above and beyond prenatal depression (Robertson et al. 2004). For ethnic minority and particularly immigrant women, culturally linked difficulties are also potentially impactful and warrant examination in the context of other stressors (Yoshikawa and Kalil 2011).
Prenatal Stress as Risk for Postpartum Depression
The risk for postpartum depression is intensified with additional life stressors, given that the experience of pregnancy can itself be considered a stressful event (Pfost et al. 1990). Among low-income and immigrant populations, unstable family relationships and chronic daily hassles are also strongly associated with depression surrounding pregnancy (Bolton et al. 1998; Seguin et al. 1995). Mexican Americans living in the United States face specific stressors related to their ethnic minority status and, for some, immigrant status (Cervantes et al. 1991; Viruell-Fuentes et al. 2012). At a societal level, they are exposed to a range of difficulties including structural racism, or lack of access to full social inclusion, and often denial of citizenship status in addition to socioeconomic challenges that commonly co-occur (Yoshikawa and Kalil 2011). Challenges related to culture, immigration, and lack of access to health services may be heightened by the context of pregnancy, but the unique contribution of these culture-specific stressors to the development of postpartum depression has not been well-examined (Zelkowitz et al. 2004). Although there is some evidence that recent immigrants are at elevated risk for postpartum depression (Institute of Medicine 2001; Urquia et al. 2012), few studies have examined stress processes that might account for these findings and studies that address cultural explanatory processes longitudinally are particularly rare.
Interpersonal stressors may be especially harmful for populations that have limited financial resources and for those that place greater emphasis on close family relationships for coping and survival (Diaz et al. 2007). Although the majority of research on interpersonal stress and postpartum depression has examined European American women, available data indicates similar or even intensified associations may exist in Latino women (Campos et al. 2008). Latino family research and related cultural theory emphasize interpersonal relationships within the extended family as uniquely relevant to psychosocial distress and depression for Latinos due to strong expectations that the family is the primary resource for coping during times of stress (Diaz et al. 2007). Thus, high levels of family stress may be especially threatening for women of Mexican heritage because it violates cultural expectations about family relationships (Hernández et al. 2010), particularly during pregnancy, when the traditional role of the family is to support the expectant mother and reduce her exposure to stressful experiences that might compromise her health and her baby (Kruckman 1992; Niska et al. 1998).
Another form of interpersonal stress is strain from a romantic relationship. Partner stress has the potential to undermine an individual’s well-being, particularly when facing parenthood. Some theories such as the Marital Discord Model of Depression (O’Leary et al. 1990) posit that conflict and dissatisfaction in marriage is a primary cause of personal distress that results in depressive symptoms. Psychological effects of romantic partner distress may become intensified during pregnancy, a vulnerable life stage in which the romantic partner relationship may be even more critical for well-being (Brugha et al. 1998; Diaz et al. 2007). Related evolutionary theory, specifically the Parental Investment Theory (Hagen 1999), posits that stress and instability in the couple relationship is the most serious threat that expectant mothers can experience during pregnancy. The combined threat of limited financial resources, romantic partner distress and the resulting low investment on the part of the father all contribute to depression because they diminish the perceived ability of mothers to manage the reproductive costs of a new child. Clearly, pregnancy is a normative period of stress on women’s mental and physical health due to a combination of risks for psychosocial distress (Balcazar et al. 2001).
Social Support as a Buffer of Stress
In the vulnerable and high-stress time of pregnancy, social support can be a major protective factor against depression (Brugha et al. 1998; Diaz et al. 2007), and may be a particularly strong stress buffer for Latinas (Campos et al. 2008). According to theories such as the Buffering Model of Stress (Cohen and Wills 1985), the presence of social support can lessen the effects of stress because it increases perceived assistance in coping and reduces the psychological impact of stressful experiences. Of note, social support that specifically matches the context or type of stressors may have the strongest buffering effect, perhaps highlighting the importance of social support when relationships are strained. For example, emotional support provided by family members and partners or spouses provides more protection against depression than tangible support among mothers, although this seems to depend to some extent on level of poverty (Manuel et al. 2012). Some studies have not found buffering effects of social support on risk for depression (Israel et al. 2002; Wade and Kendler 2000), whereas others have shown evidence of stress buffering (Cohen and Wills 1985; Moak and Agrawal 2010). Especially for women in low-income and ethnic minority groups, further clarification of these mechanisms is critically needed to inform efforts to reduce disparities and improve mental health. This need is best addressed through prospective investigation of specific stressors and social support in the emergence of postpartum depressive symptoms.
The Present Study
The current study aimed to address shortcomings in literature among high-risk perinatal women by testing the effects of prenatal stressors and social support on postpartum depressive symptoms among Mexican origin women living in the United States (hereafter labeled Mexican American). There were two aims for this investigation. The first aim was to test the unique effects of four specific subtypes of prenatal stress on depressive symptoms at six weeks postpartum. Stress measures included the perceived burden of general daily hassles, cultural-specific stressors, and interpersonal stressors within the romantic partner and extended family. We hypothesized that each stressor would uniquely predict depressive symptoms at six weeks postpartum, above and beyond prior levels of symptoms and sociodemographic characteristics (maternal age, education level, income, and immigrant status). The second aim was to examine the stress-buffering effects of social support as a moderator of prenatal stress on depression. We hypothesized that social support would interact with each form of stress, such that high levels of social support would reduce the association between stress and depressive symptoms (i.e., stress-buffering). By including multiple distinct stressors within a single prospective model, this study aimed to clarify dimensions of stress that are most salient for low-income Mexican American mothers during pregnancy and after the birth of a child.
MATERIALS AND METHODS
Participants
Participants consisted of 269 low income Mexican American women living in Maricopa County, AZ, recruited as part of a prospective study on mother and infant coregulatory mechanisms and postpartum depressive symptoms. Initial eligibility criteria included the following: 1) age 18 or older, 2) fluent in either Spanish or English, 3) self-identified as Mexican American, 4) who expected and delivered a singleton baby, 5) no prenatal indication of a significant health or developmental problem with the baby, and 6) low income status (eligible for Medicaid or self-reported income below $25,000. A total of 56% of eligible women agreed to schedule a prenatal home visit and provide informed consent. Of the women who completed the prenatal visit (n = 337), two became ineligible due to problems completing the interview, one became ineligible due to safety issue in the home, and twelve participants were excluded because they were subsequently determined to be of “non-Mexican” Hispanic ancestry. The larger sample consisted of 322 women; the present study only included 269 women reporting a serious romantic partner (married or unmarried) within the six months prior to the initial interview who answered questions about partner-specific stress.
Mothers were, on average, 28 years of age (SD =6.5) ranging from 18 to 42 years old, and had completed on average ten years of education (SD=3.3). Only 39.8% of mothers reported having completed high school, with a range from zero to 18 years of education. The median household income was $10,000–15,000 (M = 16602.81, SD = 13,212.65), with 71% of mothers reporting household income of less than $20,000 per year. Sixty-three percent were not married despite reporting a significant romantic relationship. Most mothers were born in Mexico (88.8%) and were interviewed in Spanish (83.3%).
Procedures
Prospective participants were identified at three county-operated prenatal care clinics in Arizona. In this region, approximately 29% of the population of 3.8 million people are Hispanic. Women were recruited at any point during pregnancy before 34 weeks gestation, and were invited to participate by a female, bilingual interviewer. Informed consent and contact information were obtained for all participants. They completed a prenatal home interview for all participants (T1; 26–38 weeks gestation; mean 35.4 weeks, SD=2.8), followed by a home visit at six weeks postpartum (T2).
In-home computer-assisted interviews were conducted in the participants’ language of choice (English or Spanish); questionnaires were read aloud and the interviews recorded participant responses. Measures previously validated with Latinos were used when available, with minor adaptations to Spanish translations made when necessary to accommodate regional differences. All newly translated measures were forward and back-translated, refined for local cultural adaptation, and field tested for cultural sensitivity for the relevant population (Behling and Law 2000) with final translations reviewed by a third native bilingual translator and discrepancies resolved by the research team. Women were compensated with $75 and small gifts (e.g., body lotion) for their participation at T1 and $50 and small gifts (e.g., bibs) at T2. Each visit was scheduled to last approximately 1.5 hours. Approval to conduct this study was obtained from all relevant Institutional Review Boards. Data collection procedures complied with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Measures
Sociodemographic Covariates
Mothers provided background information in a number of domains that are potentially important in understanding postpartum risk for depression: marital status, number of other children, country of birth, age at intake, years of education completed, and estimated yearly household income.
Depressive Symptoms
Depressive symptoms were assessed at each time point using the ten-item Edinburgh Postpartum Depression Scale (EPDS; Cox et al. 1987) that has been validated in English and Spanish (Garcia-Esteve et al. 2003). Sample items include “Things have been piling up on you” and “You have felt scared or panicky for no very good reason.” Possible responses for each item ranged from zero (“Not at all/Never”) to three (“As much as you always do/most of the time”). Item scores were summed (maximum possible score = 30; prenatal α = .86; 6-week α = .87), with higher scores reflecting higher levels of depressive symptomatology. An error in response sets led to one item on the T1 measure being treated as missing data for 99 participants, and two items on the 6 week T2 measure being treated as missing data for 82 participants. Multiple imputation (Mplus 7; Muthén and Muthén 2012) was used to impute missing item-level values for these participants (Reiter and Raghunathan 2007). Responses were summed and higher scores reflect higher depressive symptomatology.
Daily Hassles
Everyday life hassles (DH) were assessed with the Belsky, Crnic, and Woodworth (1995) adaptation of the Daily Hassles measure developed by Kanner et al. (1981). The adapted measure contains 25 items addressing specific everyday stressors for which mothers were asked to rate the frequency of occurrence (“How often does this happen?”) on a 5 point scale ranging from 1 (“none of the time”) to 5 (“an extreme amount of time”), and the intensity of each hassle (“How much has this been a hassle for you?”) ranging from 1 (“not at all a hassle”) to 5 (“An extreme hassle”). Sample items include “Planning, shopping, and meal preparation” and “House cleaning or maintenance.” Total perceived burden or stress appraisal was calculated by summing the intensity ratings for all items (maximum possible score = 125; α = .91).
Culture-Specific Stressors
The Hispanic Stress Inventory (HSI) is 7-subscale questionnaire aimed at capturing culture-specific stressors among Hispanic individuals (Cervantes et al. 1991). The HSI was developed through a multi-phase process, beginning with interviews with Hispanic adults living in the United States, and has demonstrated cultural relevance, good content and construct validity, and high reliability in both US-born and immigrant Hispanic samples (Cervantes et al. 1990). Items were removed, added, and re-worded to reduce length of the scale to 49 items that capture stressors relevant to our sample of low-income mothers (e.g., items about work stress were dropped as most of our mothers were not working and family and partner stressors were excluded to eliminate conceptual overlap with the interpersonal stress domains). A count score was computed based on the number of items endorsed (0 = “no, did not happen”; 1 = “yes, happened”) across four categories: language (4 items), discrimination (4 items), medical (7 items), and immigration stressors (8 items). Sample items include “It has been difficult for you to deal with day to day situations because you do not know enough English”, “You have not received help or services you need because you are Mexican or Mexican American”, “You had trouble finding medical care you want or need”, and “Someone in your family was deported or questioned by immigration officials.” Higher scores on the Culture-Specific Stress composite (α = .68), indicated more experiences of cultural stressors (maximum possible score = 23).
Family Interpersonal Stress
Mothers answered three questions regarding negativity and criticism from family members (adapted from (Schuster et al. 1990; Turner and Marino 1994). Specifically they were asked to rate from 1 (“Never) to 5 (“All of the time”) on the following items: “You feel that your family places too many demands on you,” “Your family is always pointing out mistakes,” and “Your family is often critical of you.” A Family Interpersonal Stress subscale (maximum possible score = 15; α = .82) was calculated from the sum of scores for these questions.
Partner Interpersonal Stress
Partner stress was measured with selected items from the Dyadic Adjustment Scale (DAS; Spanier 1979). The DAS is one of the most frequently used standard measures of marital quality and has been validated in Mexican American samples (Casas and Ortiz 1985). Of seven items about the marital/partner relationship, four questions that asked about relationship stress or dissatisfaction were selected (“How often do you discuss or have you considered divorce, separation, or terminating your relationship?”, “How often do you regret that you married (or lived together) with your significant other?”, “How often do you and your partner argue?”, and “How often do you and your partner irritate each other?”). Mothers responded according to the frequency of each item, with a range from 1 (“Never”) to 5 (All of the Time”). The total score was created by summing each item (maximum possible score =20; α = .69), with higher scores representing greater levels of marital/partner stress
Social Support
Mothers reported on their perceived social support during the prenatal interview by responding to 17 items from the Medical Outcome Study (MOS; Sherbourne and Stewart 1991) that asked about the people they go to for companionship, advice, and other types of help. Sample items included “How often do you have someone you can count on to listen when you need to talk?” and “How often do you have someone to turn to for suggestions about how to deal with a personal problem?” Mothers answered each question based on frequency of support received, with a range from 1 (“Never”) to 5 (“All of the Time”). A total support score was calculated by summing the score for all items (maximum possible score=85 α = .95), and higher scores reflect greater levels of social support.
Plan of Analysis
All primary analyses were conducted with the sample of women who reported having a romantic partner. To test the first hypothesis that prenatal stressors in multiple domains are uniquely associated with increased postpartum depressive symptoms, path analysis with multiple regressions was conducted using MPlus 7 (Muthén and Muthén 2012) using full information maximum likelihood estimation to account for missing data (Enders 2001). Simultaneous prospective effects on depressive symptoms at six weeks postpartum (Table 2) were estimated in a model that included all four types of stressors (daily hassles, culture-specific stress, partner stress, and family stress), baseline depressive symptoms, and the covariates (age, income, education, marital status, and immigrant status).
To test the moderating role of social support, interaction terms between social support and each stress variable were included in the path model. All variables, including independent variables and the moderator (social support), were centered for all analyses to reduce multicollinearity (Aiken and West 1991). To present the most parsimonious model and reduce increase in standard errors, only significant interaction terms are presented in the final model. Significant interactions were probed, as outlined by Aiken and West (1991), by calculating simple slopes at one standard deviation above and below the mean social support scores. In follow-up analyses, models testing the unique and moderating effects were completed again with the larger study sample of women, including those without a romantic partner, to examine generalizability to the larger population.
RESULTS
Preliminary Analyses
Correlations, means and standard deviations are reported for all variables in Table 1. All variables were within acceptable limits for skew (< 2) and kurtosis (< 7). As expected, stress variables were positively associated with one another, positively associated with prenatal and six week depressive symptoms, and negatively associated with support. Culture-specific stress, however, was not significantly associated with social support.
Table 1.
Correlations and Descriptive Statistics for Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Household Income | - | ||||||||||||
| 2 | Age | .061 | - | |||||||||||
| 3 | Years Education | .245** | −.251** | - | ||||||||||
| 4 | Marital Status | .171** | .197** | .185** | - | |||||||||
| 5 | Num. Other Children | −.113 | .593** | −.422** | .104 | - | ||||||||
| 6 | Immigrant Status | −.051 | .306** | −.150* | .172** | .216** | - | |||||||
| 7 | Prenatal Depression | .044 | .020 | .070 | .055 | −.003 | −.024 | - | ||||||
| 8 | Daily Hassles | .062 | −.080 | .108 | .027 | −.010 | −.083 | .594** | - | |||||
| 9 | Culture-Specific Stress | −.102 | .097 | −.012 | .126* | .052 | .222** | .264** | .273** | - | ||||
| 10 | Partner Stress | −.024 | −.029 | .094 | .047 | −.010 | −.091 | .474** | .398** | .165** | - | |||
| 11 | Family Stress | −.053 | −.025 | −.006 | −.195** | .084 | −.140* | .375** | .422** | .185** | .294** | - | ||
| 12 | Support | .071 | −.098 | .075 | .002 | −.119 | −.087 | −.272** | −.220** | −.111 | −.401** | −.197** | - | |
| 13 | 6-Wk Depression | .133* | .076 | .003 | .022 | .001 | −.168** | .519** | .458** | .184** | .435** | .368** | −.189** | - |
| Mean | 16607.81 | 28.22 | 10.08 | 36.8% | 2.09 | 88.8% | 5.32 | 41.95 | 2.82 | 7.03 | 5.07 | 51.67 | 4.32 | |
| Std. Deviation | 13212.65 | 6.49 | 3.24 | 0.48 | 1.68 | 0.32 | 5.10 | 12.97 | 3.07 | 2.48 | 2.79 | 15.27 | 4.96 |
Note. n= 269. Immigrant status was coded 1 = emigrated from Mexico. Marital status was coded 1 = married.
p < .05;
p <.01 (two-tailed).
Prenatal Stress and Postpartum Depressive Symptoms: Prospective and Moderating Associations
The initial structural equation model testing main effects (Table 2) indicated that higher levels of daily hassles (β = .15, p = .013), partner stress (β = .21, p < .001), and family stress (β = .14, p = .013) were uniquely associated with more postpartum depressive symptoms at six weeks when all stress domains, prenatal depression, and covariates were included as predictors. Culture-specific stress and support were not significant. Regarding covariates, greater household income (β = .12, p = .014), older mother age (β = .16, p = .009), and being a non-immigrant (born in the U.S.) (β = −.16, p = .002) were associated with more depressive symptoms at six weeks.
Table 2.
Path Model Predicting Six-Week Postpartum Depressive Symptoms.
| Variables | B | S.E. B | β |
|---|---|---|---|
| Control Variables (T1) | |||
| Household Income | 0.23 | .09 | .12* |
| Age | 0.12 | .05 | .16** |
| Years Education | −0.17 | .08 | −.11* |
| Marital Status | 0.21 | .54 | .02 |
| Num. Other Children | −0.31 | .19 | −.10 |
| Immigrant Status | −2.53 | .82 | −.16** |
| Prenatal Depression | 0.26 | .06 | .26*** |
| Predictor Variables (T1) | |||
| Daily Hassles | 0.06 | .02 | .15* |
| Culture-Specific Stress | 0.08 | .08 | .05 |
| Partner Stress | 0.42 | .12 | .21*** |
| Family Stress | 0.14 | .10 | .24* |
| Support | 0.01 | .02 | .02 |
| R2 | .41*** | ||
Note. n=269 mothers, all reporting current romantic partner. T1= Time 1 (prenatal), T2= Time 2 (6 weeks postpartum).
p < .05.
p < .01.
p ≤ .001 (two-tailed).
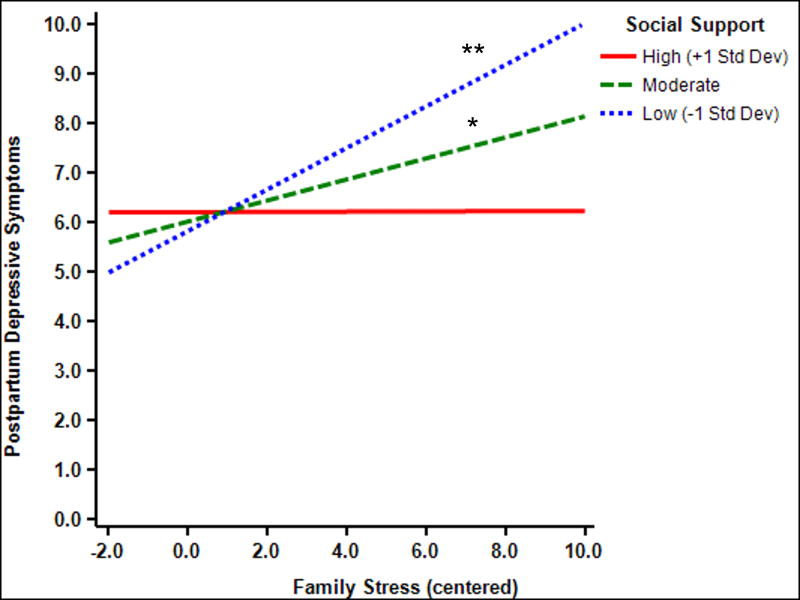
In the model testing interactions between social support and each stress variable (see Table 3), there was an interaction between social support and family stress (β = −.12, p = .015). Effects of support on family stress were probed at low (1 SD below the mean), moderate (within 1 SD) and high (1 SD above the mean) levels of support (Figure 1; graphic created with Interaction software v.1.7.2211; (Soper 2010). Under conditions of low social support (1 SD below the mean) family stress was positively associated with six-week depressive symptoms (β = .21, p = .002). At mean levels of support, family stress was significantly associated with subsequent depressive symptoms (β = .11, p = .041). In contrast, at high levels of social support (1 SD above the mean), family stress showed no association with subsequent depressive symptoms (β = −.01, p = .917). No other significant interactions were found for support with culture-specific stress, partner stress, and daily hassles when examined separately or concurrently within a single model.
Table 3.
Path Model Predicting Six-Week Postpartum Depressive Symptoms Moderated by Support.
| Variables | B | S.E. B | β |
|---|---|---|---|
| Control Variables (T1) | |||
| Household Income | .23 | .05 | .12* |
| Age | .12 | .06 | .15** |
| Years Education | −.17 | .05 | −.11* |
| Marital Status | .17 | .05 | .02 |
| Num. Other Children | −.31 | .06 | −.10 |
| Immigrant Status | −2.43 | .05 | −.15** |
| Prenatal Depression | .26 | .06 | .27*** |
| Predictor Variables (T1) | |||
| Daily Hassles | .07 | .06 | .18** |
| Culture-Specific Stress | .10 | .05 | .06 |
| Partner Stress | .39 | .06 | .20*** |
| Family Stress | .20 | .06 | .11* |
| Support | .01 | .05 | .04 |
| Family Stress X Support | −.01 | .05 | −.12* |
| R2 | .42*** | ||
Note. n=269 mothers, all reporting current romantic partner. T1= Time 1 (prenatal), T2= Time 2 (6 weeks postpartum). Marital status coded 0 = not married or living with partner, 1 = married or living with partner.
p < .05.
p < .01.
p ≤ .001 (two-tailed).
Fig 1.
Association between prenatal family stress and 6-week postpartum depressive symptoms as moderated by prenatal support. * p <.05, **p <.01 (two-tailed).
Follow-up analyses examined additional post hoc questions about immigrant status as well as generalizability to the rest of the sample. First, given the finding that depressive symptoms were lower among women who emigrated from Mexico, follow-up analyses examined differences in prenatal stress predictors of depression as a function of immigrant status (Mexico vs. U.S. nativity). Specifically, we conducted separate tests of the interactions of each stress domain, social support, and prenatal depressive symptoms with immigrant status as predictors of six week postpartum depressive symptoms. No significant interactions were found between immigrant status and any stress domain (culture-specific, partner, family, or daily hassles), social support, or prenatal depressive symptoms. Finally, to determine whether main findings regarding the stress domains and interactions with social support would replicate within the larger sample, follow-up analyses were performed on the full sample of 322 women, with the partner stress variable removed. Effects of all remaining variables in the model were replicated, including the associations found for all covariates and stress domains, and the interaction between social support and family stress.
DISCUSSION
This study examined multiple types of stressors experienced by low-income Mexican American women during the prenatal period to determine their unique contributions to maternal depressive symptoms at six weeks postpartum, controlling for prenatal depressive symptoms and relevant demographic covariates. Additionally, social support was examined as a protective resource that could mitigate the effects of prenatal stress on postpartum depressive symptoms. Results showed that multiple domains of stress were related to depressive symptoms and, when examined together, daily hassles, family stressors, and partner stressors each uniquely predicted postpartum depressive symptoms. Results highlight interpersonal stressors as an impactful type of stress on mothers’ mental health. In particular, stress in the romantic partner relationship emerged as the most robust predictor of depressive symptoms for Mexican American women during the transition to motherhood. Social support significantly buffered the effects of family stress, but did not buffer the impact of other stress domains.
Multiple Stress Domains Predict Postpartum Depressive Symptoms
Overall findings show that women are at increased risk for increased symptoms of depression after giving birth if they experience increased stress during the prenatal period. All types of stress were related to postpartum depressive symptoms. However, when examined together, three of the four stressor domains predicted uniquely. The perceived burden of everyday hassles that include shopping and cooking, cleaning, unexpected company, and traffic predicted depressive symptoms after the birth of a child. As hypothesized, interpersonal stressors also accounted uniquely for postpartum depressive symptoms in this study. Women were likely to show increased postpartum depressive symptoms if they were experiencing negativity, conflict, and strain with their partners during pregnancy. Further, family interpersonal stress also predicted increased symptoms for women who had low levels of emotional support.
The salience of family and partner interpersonal stress in this study is consistent with cultural expectations that emphasize the central role of the family in Mexican American culture, especially during and immediately following pregnancy (Campos et al. 2008). At these times, Mexican origin women may be more deeply affected by conflict and dissatisfaction with their family and particularly with their significant other, who is likely expected to be a primary source of support for the mother and her baby once it is born. However, our exclusive focus on Mexican origin women precludes us from determining whether these findings are specific to our culturally distinct sample. Broader theoretical perspectives such as the Marital Discord Model of Depression (O’Leary et al. 1990) and Parental Investment Theory (Hagen 1999) and prior findings with general population samples (Robertson et al. 2004; Milgrom et al. 2008) suggest these findings would generalize to other cultural groups.
Although we hypothesized that this population may experience culturally-linked difficulties, such as language barriers, immigration concerns, and lack of access to healthcare that might uniquely account for their mental health during and after pregnancy, this hypothesis was not supported. It is possible the items included from the Hispanic Stress Inventory did not capture the types of cultural stressors that were most salient for this sample of pregnant women in the context of other perceived stressors. Pregnancy may be a time when cultural conflicts are minimized as women become more focused on their family and individual health concerns, consistent with Mexican American cultural expectations for pregnant women (Kruckman 1992; Niska et al. 1998). With respect to stressors associated with healthcare access, this sample included women who were receiving prenatal care; thus, these women had succeeded in obtaining needed resources to support their health and their baby. Moreover, the perceived meaning of culturally-linked stressors may represent more distal barriers or threats that operate by amplifying daily hassles and interpersonal stressors within the family and partner, consistent with family stress theory (Conger and Elder Jr 1994) and intersectionality theory (Viruell-Fuentes et al. 2012). These more proximal day-to-day transactions may be most closely linked to changes over time in symptoms of depression. This explanation is consistent with our findings that cultural stressors were moderately related to depressive symptoms when examined independently, but not in the presence of other stress domains.
Social Support as a Buffer of Family Stress
Mothers with high levels of social support did not experience the same negative effects of family stress compared to those lacking social support, consistent with the Buffering Model of Stress (Cohen and Wills 1985). Of note, the presence of social support alone did not reduce risk for depression, contrary to some arguments in the literature (Balcazar et al. 2001; Collins et al. 1993), nor did it buffer the effects of partner stress or other stress domains. However, differences may be explained by the aspect and quality of support examined. For instance, Collins and colleagues (1993) found that poorer quality of social support was associated with increased risk for depression; however, quantity of support alone was only associated with depression in regards to material support. Collins and colleagues (Collins et al. 1993) noted the importance of examining dissatisfaction with prenatal support as a risk factor for depressive symptomatology 6–8 weeks postpartum, which may have been captured in our measures of interpersonal stress. In this context, our findings highlight the complexity of measuring stress and social support in relation to risk for depression. The specificity of the buffering role of social support is consistent with Cohen and Wills’ theory (1985), which has argued that support that matches the context of stressors may have the most impactful buffering effect. Accordingly, perhaps the availability of other sources of emotional support compensated for conflict and challenges that women experienced within their family relationships.
Importantly, strain in a romantic relationship is not offset or compensated by the presence of other supportive resources. Related, others have found that partner support during pregnancy mediates the association between distress in early pregnancy and distress at 6 to 8 weeks postpartum (Stapleton et al. 2012). Thus, building on these findings with the present findings, pregnant women already experiencing emotional distress appear to be affected by the positive and negative influences of their romantic partner. Further, the lack of stress-buffering with respect to partner stress highlights the critical importance of a healthy partner relationship for women during the transition to parenthood.
Immigration and Cultural Considerations
In addition to primary findings, an unexpected finding was that immigrant status was associated with reduced risk for postpartum depressive symptoms. This effect remained after accounting for differences in prenatal stress levels. In fact, immigrant status was associated with lower levels of daily hassles and family stress, but more culturally-related stress in this study. In contrast to some prior research that has found immigrants are at higher risk for postpartum depression (Urquia et al. 2012), these findings potentially offer another example of the Latino immigrant paradox in which immigrants from Latin American countries experience similar or better health outcomes than those born in the U.S. despite greater socioeconomic disadvantage and barriers to health care (Alegría et al. 2008). However, it should be noted that the substantial multicollinearity among immigrant status and other predictors of depression (e.g., age, number of children, education) as well as with culture-specific stress makes it difficult to reliably tease out and interpret their unique contributions. Further, because our sampling strategy was intentionally restricted in terms of socioeconomic status, our findings are not representative of the broader population, particularly for U.S. born Latinas. Nevertheless, this study highlights the contextual realities faced by a substantial population of ethnic minorities in the United States (Diaz et al. 2007). Finally, it is also important to consider the time frame in which this study was completed, during and after the time of Arizona’s “Supporting Our Law Enforcement and Safe Neighborhoods Act” (SB 1070 Ariz 2010). In addition to the bill having the potential to affect experiences of stress across domains, women in our study may have been particularly hesitant to seek public assistance, including health care, as has been found among adolescent mothers during this time (Toomey et al. 2014). The perceived threat from SB 1070 may have posed additional barriers to their already tenuous access to services needed for health care and public assistance during the sensitive period surrounding pregnancy, delivery, and postpartum. Future studies are needed to replicate these findings with more diverse samples of Latinas as well as other immigrant populations (Robertson et al. 2004).
Clinical Implications
Determining the most relevant predictors of postpartum depressive symptoms is an important task due to its major impact on parental well-being, the parent-child relationship, and overall concerns regarding child development. The current findings have important implications for the specific life domains that practitioners should assess when providing prenatal care to expectant Mexican American mothers. Because interpersonal stress is particularly impactful during pregnancy and early motherhood, practitioners should routinely inquire about stress and support that women are experiencing with their families and partners during prenatal visits. Consistent screening of stress and support can identify women at risk who may need additional resources.
Beyond routine screenings, prevention programs can be developed for perinatal women to prevent escalating symptoms of depression during the transition to motherhood. This is a high priority among public health organizations. For instance, the World Health Organization has released reports highlighting the importance of comprehensive efforts to support mothers before, during, and after pregnancy, naming interventions to address mental health problems across childbearing stages (Marmot et al. 2008). Mothers who experience high levels of negativity, conflict, and other challenges with family, in particular, may benefit from additional support services. For example, interventions can work with women prenatally to reduce interpersonal tensions and adjust expectations about the role of their partner and family. Strategies could include communication training, positive events scheduling, and conflict resolution. In particular, programs can build on the cultural strength of immigrant families by highlighting the importance of family bonds and family harmony. Related, culturally sensitive programs can target the prenatal period as an important time to encourage partner and family members to work together to reduce daily hassles and strengthen family connections and social support for the sake of mother and baby alike.
Some women experience the family context as critical and unsupportive and do not have other supportive resources on which they can rely. For such mothers, alternative sources of support could be encouraged or specifically provided in the form of evidence-bases strategies such as peer support programs (Dennis et al. 2009) or integrated systems of care that make use of informal support networks (McGlade et al. 2004). For instance, community health workers (promotoras), midwives (parteras), and caregivers can be employed to provide support during labor and the postpartum period (doulas). Further, in-home services may help women to access care and experience a more positive sense of well-being while engaging in the practice of postpartum confinement known as cuarentena (Blackmore and Chaudron 2014). Although our findings require replication, they indicate that heightened levels of stress, particularly interpersonal stress, may be a stronger indicator of the need for such programs than prenatal depressive symptoms.
This study contributes novel data regarding issues of major public health concern. As with any study, several limitations should be considered. First, this study did not interview other individuals in participants’ lives. Therefore, data were reported by women alone and not verified by other family members or partners. Second, as previously noted, this study was conducted in Arizona during a time in which discriminatory attitudes and practices toward individuals of Mexican origin were at an all-time high and Arizona had recently adopted the nation’s toughest law on illegal immigration (McConnell 2013). These circumstances may have caused women to minimize their distress and problems in order to reduce any perception that they posed a burden or required additional social services. Nonetheless, clear associations between several stressors and depressive symptoms suggest a clear link, even if distress may have been under-reported by participants.
Conclusion
The present study provides longitudinal insight regarding the mechanisms of stress, social support, and postpartum depression in high-risk women. We found that several aspects of stress during the prenatal period poses risk for postpartum depressive symptoms among low-income Mexican American women. Daily hassles, family stress, and partner stress pose particularly important threats to the well-being of women who may already experience increased cultural and socioeconomic disparities. Stress with a romantic partner is a major contributor risk for depressive symptoms, and social support alone does not necessarily reduce depressive symptoms after the birth of a child. Nonetheless, social support can offset the deleterious effects of strained family relationships. Mexican American women may benefit from social support during and after pregnancy because it is consistent with cultural expectations of the importance of family. Therefore, preventative efforts should be made to effectively increase social support when stressors are high. Counseling services and other interventions during the prenatal period could prevent psychosocial distress after the birth of a child.
In addition to the current focus on social support as a resilience-promoting resource, future studies should examine additional protective mechanisms, particularly cultural resources that may help to account for positive maternal adaptation and mental health. Given our plans to maintain the sample over time, our continued follow-up will be important to track women’s mental health and document profiles of continued resilience and declining mental health. Further, segmented assimilation theory has identified the children of immigrants (“the second generation”), as the most vulnerable population, particularly for those born into conditions of poverty (Zhou 1997). Therefore, it will be critical to also follow the children of these mothers over time to understand how their experiences as children of immigrants, born into poor circumstances in the U.S., influence their resilience, developmental trajectories, and health outcomes.
Acknowledgments
This study is supported by a grant, R01 NIMH MH083173 (MPIs: Keith Crnic, Nancy Gonzales and Linda Luecken). The first author of this manuscript was supported by an institutional training grant, T32 MH18387, NIMH. We thank the mothers and infants for their participation; Kirsten Letham, Anne Mauricio, Monica Gutierrez, and Craig Enders, for their assistance with data collection and management; Dr. Dean Coonrod and the Maricopa Integrated Health Systems for their assistance with recruitment; and the interviewers for their commitment and dedication to this project.
Footnotes
Conflict of Interest: The authors of this manuscript have no potential conflicts of interests, including financial interests or gains.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. In: Cohen J, Cohen P, West SG, Aiken LS, editors. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Lawrence Erlbaum Associates, Inc; New Jersey: 1991. [Google Scholar]
- Alegría M, Canino G, Shrout P, Woo M, Duan N, Vila D, Torres M, Chen C, Meng X. Prevalence of mental illness in immigrant and non-immigrant US Latino groups. Am J Psychiatry. 2008;165:359–69. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balcazar H, Krull JL, Peterson G. Acculturation and family functioning are related to health risks among pregnant Mexican American women. Behavioral Medicine. 2001;27:62–70. doi: 10.1080/08964280109595772. [DOI] [PubMed] [Google Scholar]
- Behling O, Law KS. Translating questionnaires and other research instruments: Problems and solutions. Sage; Thousand Oaks, California: 2000. [Google Scholar]
- Belsky J, Crnic K, Woodworth S. Personality and parenting: Exploring the mediating role of transient mood and daily hassles. J Pers. 1995;63:905–29. doi: 10.1111/j.1467-6494.1995.tb00320.x. [DOI] [PubMed] [Google Scholar]
- Blackmore ER, Chaudron L. Anonymous Perinatal Depression among Spanish-Speaking and Latin American Women. Springer; 2014. Psychosocial and cultural considerations in detecting and treating depression in Latina perinatal women in the United States; pp. 83–96. [Google Scholar]
- Bolton H, Hughes P, Turton P, Sedgwick P. Incidence and demographic correlates of depressive symptoms during pregnancy in an inner London population. Journal of Psychosomatic Obstetrics & Gynecology. 1998;19:202–9. doi: 10.3109/01674829809025698. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Sharp H, Cooper S, Weisender C, Britto D, Shinkwin R, Sherrif T, Kirwan P. The Leicester 500 Project. Social support and the development of postnatal depressive symptoms, a prospective cohort survey. Psychol Med. 1998;28:63–79. doi: 10.1017/s0033291797005655. [DOI] [PubMed] [Google Scholar]
- Campos B, Schetter CD, Abdou CM, Hobel CJ, Glynn LM, Sandman CA. Familialism, social support, and stress: Positive implications for pregnant Latinas. Cultural Diversity and Ethnic Minority Psychology. 2008;14:155. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casas JM, Ortiz S. Exploring the applicability of the Dyadic Adjustment Scale for assessing level of marital adjustment with Mexican Americans. Journal of Marriage and the Family. 1985;47(4):1023–7. [Google Scholar]
- Cervantes RC, Padilla AM, De Snyder NS. Reliability and validity of the Hispanic Stress Inventory. Hispanic Journal of Behavioral Sciences. 1990;12:76–82. [Google Scholar]
- Cervantes RC, Padilla AM, Salgado de Snyder N. The Hispanic Stress Inventory: A culturally relevant approach to psychosocial assessment. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:438. [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98:310. [PubMed] [Google Scholar]
- Collins NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC. Social support in pregnancy: psychosocial correlates of birth outcomes and postpartum depression. J Pers Soc Psychol. 1993;65:1243. doi: 10.1037//0022-3514.65.6.1243. [DOI] [PubMed] [Google Scholar]
- Conger RD, Elder GH., Jr . Families in troubled times: Adapting to change in rural america. Transaction Publishers; New York: 1994. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, Kiss A. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ. 2009;338:a3064. doi: 10.1136/bmj.a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz MA, Le H, Cooper BA, Muñoz RF. Interpersonal factors and perinatal depressive symptomatology in a low-income Latina sample. Cultural Diversity and Ethnic Minority Psychology. 2007;13:328. doi: 10.1037/1099-9809.13.4.328. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–58. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Enders CK. The Relative Performance of Full Information Maximum Likelihood Estimation for Missing Data in Structural Equation Models. Structural equation modeling. 2001;8:43057. [PubMed] [Google Scholar]
- Faisal-Cury A, Menezes PR. Prevalence of anxiety and depression during pregnancy in a private setting sample. Archives of women’s mental health. 2007;10:25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- Garcia-Esteve L, Ascaso C, Ojuel J, Navarro P. Validation of the Edinburgh postnatal depression scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75:71–6. doi: 10.1016/s0165-0327(02)00020-4. [DOI] [PubMed] [Google Scholar]
- Hagen EH. The functions of postpartum depression. Evolution and Human Behavior. 1999;20:325–59. [Google Scholar]
- Hernández B, Ramírez García JI, Flynn M. The role of familism in the relation between parent–child discord and psychological distress among emerging adults of Mexican descent. Journal of Family Psychology. 2010;24:105. doi: 10.1037/a0019140. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol. 1995;63:445. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Coverage Matters: Insurance and Health Care. National Academy Press; Washington, D.C: 2001. [Google Scholar]
- Israel BA, Farquhar SA, Schulz AJ, James SA, Parker EA. The relationship between social support, stress, and health among women on Detroit’s East Side. Health Educ Behav. 2002;29:342–60. doi: 10.1177/109019810202900306. [DOI] [PubMed] [Google Scholar]
- Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. J Behav Med. 1981;4:1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- Kruckman LD. Rituals and support: An anthropological view of postpartum depression. In: Hamilton J, Harberger P, editors. Postpartum Psychiatric Illness: A Picture Puzzle. University of Pennsylvania Press; 1992. pp. 137–148. [Google Scholar]
- Manuel JI, Martinson ML, Bledsoe-Mansori SE, Bellamy JL. The influence of stress and social support on depressive symptoms in mothers with young children. Soc Sci Med. 2012;75:2013–20. doi: 10.1016/j.socscimed.2012.07.034. [DOI] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet. 2008;372:1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Matthey S, Phillips J, White T, Glossop P, Hopper U, Panasetis P, Petridis A, Larkin M, Barnett B. Routine psychosocial assessment of women in the antenatal period: frequency of risk factors and implications for clinical services. Archives of Women’s Mental Health. 2004;7:223–9. doi: 10.1007/s00737-004-0064-6. [DOI] [PubMed] [Google Scholar]
- McConnell ED. Latinos in Arizona: Demographic context in the SB 1070 Era. In: Magaña L, Lee E, editors. Latino Politics and Arizona’s Immigration Law SB 1070. Springer; 2013. pp. 1–18. [Google Scholar]
- McGlade MS, Saha S, Dahlstrom ME. The Latina paradox: an opportunity for restructuring prenatal care delivery. Am J Public Health. 2004;94:2062–5. doi: 10.2105/ajph.94.12.2062. 94/12/2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, Ericksen J, Ellwood D, Buist A. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108:147–57. doi: 10.1016/j.jad.2007.10.014. [DOI] [PubMed] [Google Scholar]
- Moak ZB, Agrawal A. The association between perceived interpersonal social support and physical and mental health: Results from the National Epidemiological Survey on Alcohol and Related Conditions. J Public Health (Oxf) 2010;32:191–201. doi: 10.1093/pubmed/fdp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus Version 7: User’s guide. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Niska K, Snyder M, Lia-Hoagberg B. Family ritual facilitates adaptation to parenthood. Public Health Nursing. 1998;15:329–37. doi: 10.1111/j.1525-1446.1998.tb00357.x. [DOI] [PubMed] [Google Scholar]
- Nonacs R, Cohen LS. Postpartum mood disorders: diagnosis and treatment guidelines. J Clin Psychiatry. 1998;59:2134–40. [PubMed] [Google Scholar]
- O’Hara MW, Swain AM. Rates and risk of postpartum depression-a meta-analysis. International review of psychiatry. 1996;8:37–54. [Google Scholar]
- O’Leary KD, Riso LP, Beach SR. Attributions about the marital discord/depression link and therapy outcome. Behavior Therapy. 1990;21:413–22. [Google Scholar]
- Pfost KS, Stevens MJ, Lum CU. The relationship of demographic variables, antepartum depression, and stress to postpartum depression. J Clin Psychol. 1990;46:588–92. doi: 10.1002/1097-4679(199009)46:5<588::aid-jclp2270460507>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Reiter JP, Raghunathan TE. The multiple adaptations of multiple imputation. Journal of the American Statistical Association. 2007;102:1462–71. [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–95. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- SB 1070 (Ariz 2010) Support Our Law Enforcement and Save Our Neighborhoods Act. 49th Leg, 2 Reg. Sess.
- Schuster TL, Kessler RC, Aseltine RH., Jr Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18:423–38. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- Seguin L, Potvin L, Denis MS, Loiselle J. Chronic stressors, social support, and depression during pregnancy. Obstetrics & Gynecology. 1995;85:583–9. doi: 10.1016/0029-7844(94)00449-N. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Soper D. Interaction (Version 1.7.2211).(Software) 2010. [Google Scholar]
- Spanier GB. The measurement of marital quality. J Sex Marital Ther. 1979;5:288–300. doi: 10.1080/00926237908403734. [DOI] [PubMed] [Google Scholar]
- Stapleton LRT, Schetter CD, Westling E, Rini C, Glynn LM, Hobel CJ, Sandman CA. Perceived partner support in pregnancy predicts lower maternal and infant distress. Journal of Family Psychology. 2012;26:453. doi: 10.1037/a0028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey RB, Umaña-Taylor AJ, Williams DR, Harvey-Mendoza E, Jahromi LB, Updegraff KA. Impact of Arizona’s SB 1070 immigration law on utilization of health care and public assistance among Mexican-origin adolescent mothers and their mother figures. Am J Public Health. 2014;104:S28–34. doi: 10.2105/AJPH.2013.301655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, Marino F. Social support and social structure: A descriptive epidemiology. J Health Soc Behav. 1994;35(3):193–212. [PubMed] [Google Scholar]
- Urquia ML, O’Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: the roles of duration of residence and ethnicity. Soc Sci Med. 2012;74:1610–21. doi: 10.1016/j.socscimed.2012.02.013. [DOI] [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75:2099–106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- Wade TD, Kendler KS. The relationship between social support and major depression: cross-sectional, longitudinal, and genetic perspectives. J Nerv Ment Dis. 2000;188:251–8. doi: 10.1097/00005053-200005000-00001. [DOI] [PubMed] [Google Scholar]
- Yoshikawa H, Kalil A. The effects of parental undocumented status on the developmental contexts of young children in immigrant families. Child Development Perspectives. 2011;5:291–7. [Google Scholar]
- Zelkowitz P, Schinazi J, Katofsky L, Saucier JF, Valenzuela M, Westreich R, Dayan J. Factors associated with depression in pregnant immigrant women. Transcult Psychiatry. 2004;41:44564. doi: 10.1177/1363461504047929. [DOI] [PubMed] [Google Scholar]
- Zhou M. Segmented assimilation: Issues, controversies, and recent research on the new second generation. International migration review. 1997;31(120):975–1008. [PubMed] [Google Scholar]