Abstract
Race-based medical mistrust significantly predicts non-adherence to antiretroviral therapy (ART) in people living with HIV. The current study builds on previous research that shows beliefs about medication necessity (i.e., “My medicines protect me from becoming worse”) and concerns (i.e., Having to take my medicines worries me) mediate the association between race-based medical mistrust and medication adherence. Racial and ethnic minority men and women living with HIV and receiving ART (N=178) in a southern US city completed computerized measures of demographic and health characteristics, telephone interviews of race-based medical mistrust and medication beliefs, and unannounced phone-based pill counts for ART adherence. Multiple mediation modeling showed that medical mistrust is related to medication necessity and concerns beliefs and ART adherence. Furthermore, medication necessity beliefs predicted ART adherence. The indirect effect of medical mistrust on adherence through medication necessity beliefs was also significant. Results confirm that medication necessity beliefs, although not concerns beliefs, mediate the association between medical mistrust and ART adherence. Medication necessity beliefs offer a viable target for interventions to improve ART adherence in the context of mistrust that patients may have for medical providers and health care systems.
Introduction
The majority of new HIV infections in the United States occur among African-Americans and Latinos and AIDS-related morbidity is greater for racial and ethnic minorities. Death-rates for blacks living with HIV are 13% higher than for whites (Siddiqi, Hu, & Hall, 2015). These health disparities are at least in part accounted for by late diagnosis of HIV infection and poor adherence to antiretroviral therapy (ART, McFall et al., 2013). While circumstances associated with poverty undermine ART adherence including lacking transportation, food insecurity, and substance abuse (Gaston & Alleyne-Green, 2013), social and economic constraints do not fully account for disparities in ART adherence (Maulsby et al., 2014).
Prejudice and discrimination experiences may lead to health care disengagement and may account for race and ethnic group disparities in HIV treatment and health outcomes. Of particular importance is trust in the health care system and how mistrust translates to poor retention in care and medication adherence (Casagrande, Gary, LaVeist, Gaskin, & Cooper, 2007; Earl et al., 2013). Histories of discrimination in the United States health care system and the legacy of institutional racism, including medical experimentation on African slaves, the Tuskegee Syphilis Study, and unequal access to quality health care have understandably earned a sense of mistrust in the public health system (Gaston & Alleyne-Green, 2013).
Several studies have demonstrated that medical mistrust is more common among minority groups than whites and mistrust reliably predicts ART non-adherence (Saha, Jacobs, Moore, & Beach, 2010). One in five African American men prescribed ART believe that people receiving HIV medications are treated as human guinea pigs and 17% believe that ART is a poison, with individuals who believe that HIV treatments cannot be trusted demonstrating the poorest adherence (Bogart, Wagner, Galvan, & Banks, 2010; Dale, Bogart, Wagner, Galvan, & Klein, 2014). Although medical mistrust is a reliable predictor of ART non-adherence among people of color living with HIV, the association is not well explained and there are few recommendations for how to remedy this problem.
Medical mistrust is theoretically grounded in the historical experiences of minorities by public health and health care systems. While medical mistrust can undermine engagement in health care, more specific attitudes and beliefs may be more closely aligned with particular health behaviors. For example, medication beliefs have been shown to adversely impact treatment adherence (Nozaki et al., 2013). Unlike medical mistrust, which depends more on structural changes, medication beliefs are amenable to patient education and counseling interventions. Taking a cost-benefit approach, Horne et al. (Horne, 1999; Jonsdottir et al., 2009) developed a commonsense approach to explaining non-adherence that emphasizes patient beliefs about the necessity of medications to directly improve health and beliefs regarding concerns over costs, inconveniences and adverse effects of medications (Gonzalez et al., 2007). The Necessity-Concerns Framework predicts medication adherence across chronic health conditions, including HIV infection (Horne et al., 2013). For example, Gonzalez et al. (2007) found that beliefs about medication necessity regarding ART predict better adherence, while medication concerns predict poorer adherence.
Research suggests the association between medical mistrust and medication adherence may to some degree be accounted for by medication beliefs (Altice, Mostashari, & Friedland, 2001; Kalichman, Eaton, Kalichman, & Cherry, 2015). In a cross-sectional study of African American men and women living with HIV and receiving ART, Kalichman et al. (2015) found that medical mistrust was significantly associated with ART adherence, as were beliefs about medication necessity and concerns. Mediation analysis showed that medication beliefs mediated the relationship between medical mistrust and ART adherence. These findings were the first to show that the associations between medical mistrust and medication adherence are partially accounted for by beliefs about medications. Conceptually, while medical mistrust may serve to keep some people out of care, it appears that medication beliefs may account for medication adherence. Beliefs about medications are proximal to pill taking when considered relative to more general experiences and perceptions of the health care system. If beliefs about medications reliably mediate the relationship between medical mistrust and medication adherence, interventions may shift their focus on fostering beliefs that medications are necessary and addressing concerns about medications among patients who mistrust the health care system.
The current study was conducted to replicate and extend Kalichman et al.’s (2015) initial test of the Necessity-Concerns Framework as a mediator of the association between medical mistrust and ART adherence. In our previous research, ART adherence was measured using a single item self-report rating scale to assess ART adherence. Although the single item rating scale has shown evidence for reliability and validity in assessing medication adherence it remains dependent on self-report and is known to be biased toward over-reporting adherence (Pellowski, Kalichman, & Finitsis, 2015). In addition, the study was cross-sectional in design, limiting the test of directional relationships. The current study was undertaken to address these limitations replicating the model where medication beliefs serve as mediators of the association between medical mistrust and ART adherence. We hypothesized that race-based medical mistrust and beliefs about medications would both predict ART adherence over a one-month prospective period using an objective measure of ART adherence. In addition, we hypothesized that beliefs about medication necessity and concerns would mediate the association between race-based medical mistrust and ART adherence after controlling for participant education, years since testing HIV positive, ART side-effects and HIV-related symptoms.
Methods
Participants
Participants were 145 men and 34 women of color living with HIV and receiving ART. Recruitment occurred between December 2013 and March 2014. The site of the study was Atlanta, Georgia, a major urban center with an annual HIV incidence of 30.3 per 100,000 population. Eligible participants were age 18 or older, HIV positive, self-identified as African-American or Hispanic, and currently receiving ART. The average age of the sample was 41.6 years (SD = 10.7), 168 identified as African-American, 5 Latino, and 6 as other non-White racial ethnic background (see Table 1 for sample characteristics).
Table 1.
Demographic and health characteristics of people who had ART adherence below and above 80% of pills taken.
| Characteristics | Less than or equal to 80% Adherence N = 61 | Greater than 80% Adherence N = 117 | X2 | ||
|---|---|---|---|---|---|
|
| |||||
| N | % | N | % | ||
| Male | 49 | 80 | 95 | 81 | |
| Female | 12 | 20 | 22 | 19 | 0.02 |
| African-American | 56 | 92 | 112 | 95 | 0.80 |
| Latino | 2 | 3 | 3 | 2 | |
| Other non-white | 3 | 5 | 3 | 2 | |
| Unemployed | 44 | 74 | 90 | 76 | 0.1 |
| Aware of most recent viral load | 25 | 41 | 68 | 58 | 4.5* |
| Viral load detectable | 22 | 36 | 33 | 28 | 1.2 |
| CD4 < 200 cell/mL | 8 | 13 | 21 | 18 | 0.6 |
|
|
|||||
| M | SD | M | SD | t | |
|
|
|||||
| Age | 38.4 | 11.5 | 43.3 | 9.9 | 2.9** |
| Years of education | 13.2 | 1.7 | 12.9 | 1.7 | 1.1 |
| Years since HIV diagnosis | 9.9 | 7.4 | 11.1 | 8.2 | 0.9 |
| CD4 cell count | 467.9 | 253.5 | 476.2 | 291.3 | 0.2 |
| ART side effects | 0.5 | 0.4 | 0.4 | 0.4 | 1.8+ |
| HIV symptoms | 41 | 3.2 | 3.6 | 3.3 | 0.9 |
| Race-based medical mistrust | 2.0 | 0.6 | 1.9 | 0.6 | 1.4 |
| Necessity beliefs | 3.9 | 0.7 | 4.2 | 0.7 | 2.3** |
| Concerns beliefs | 2.6 | 0.9 | 2.5 | 0.8 | 0.9 |
Note:
p < 10
p < .05
p < .01.
Procedures
Participants were recruited through targeted community sampling with both venue and snowball techniques. Venue recruitment relied on the distribution of study brochures to waiting rooms of HIV service providers and infectious disease clinics throughout Atlanta, GA. At an initial office assessment session, participants provided informed consent and completed an audio-computer assisted self-interview (ACASI) to collect demographics and health information (Morrison-Beedy, Carey, & Tu, 2006). Participants were trained to conduct unannounced pill count assessments on the phone. We also asked participants to obtain their most recent HIV viral load and CD4 cell count results from their medical provider. Participants then completed three unannounced phone-based pill counts and phone assessments over the subsequent month. Participants were reimbursed $145 for completing all measures, pill counts, and providing medical chart information. The university Institutional Review Board approved all procedures.
Computerized Interviews: Demographic and Health Characteristics
Participants were asked their gender, age, years of education, ethnicity, employment status, the year they first tested HIV positive, and whether they were currently taking ART. Participants also completed a 14-item scale to assess the number of HIV symptoms experienced from which we calculated a composite score, alpha = .70 (Kalichman, Rompa, & Cage, 2000). Medication side-effects were measured using 11 common side-effects attributable to current medications, (Carrieri, Villes, & 2007) responses made on 4-point scales 0 = Not experiencing, 3 = Severely experiencing, summed to a total score, alpha = .83.
HIV viral load and CD4 cell counts
We used a participant assisted method for collecting chart abstracted viral load and CD4 cell counts from participants’ medical records. Participants were provided with a form to request their doctor’s office to complete with results and dates of their most recent, and not older than 3-months, viral load and CD4 cell counts. These data were therefore obtained directly by the participant from their HIV care provider. The form included a place for the provider’s office stamp or signature to assure data authenticity. HIV RNA below detection (i.e., viral suppression) was defined as less than 100 copies/mL for uniformity across providers.
Telephone Interviews: Medication beliefs and medical mistrust
During a brief telephone interview conducted after a pill count participants completed the Beliefs About Medicines Questionnaire to assess views of their beliefs about medication necessity and concerns (Horne, Cooper, Gellaitry, Date, & Fisher, 2007). The medication necessity scale consists of five items reflecting the perceived benefits of medications in direct relation to health; example items include “My health, at present, depends on my medicine” and “My medicines protect me from becoming worse”, alpha = .80. The five item medication concerns scale reflects the potential adverse effects and costs of medications; example items include “Having to take my medicines worries me” and “I sometimes worry about the long-term effects of my medicines”, alpha = .73. Items are responded to on a 5-point scale, 1 = Strongly agree, 5 = Strongly disagree.
Participants also completed the five-item Medical Suspicion sub-scale of the Group-Based Medical Mistrust Scale developed by Shelton et al. (2010). The items reflect a sense of mistrust in the medical system stemming from systemic racial prejudice. We modified the items from the original scale to indicate self-identified race rather than specifying ‘Black’ as race. Specifically, items in the original scale asked about perceptions of how ‘Black people’ are treated in health care settings. Because participants in the study may identify as Black or African American, and because we included Hispanics in the study, we changed the racial referent to “people of my race” to apply to all participants. The exact items are shown in the Results section. Items are responded to on a 4-point scale, 1 = Strongly agree, 4 = Strongly disagree. Scores were calculated by taking the mean response, alpha = .86.
Unannounced pill count medication adherence
Participants consented to three unannounced phone-based pill counts that occurred over a one-month prospective period. Unannounced pill counts are reliable and valid in assessing medication adherence (Fredericksen et al., 2014; Haberer et al., 2011; Kalichman et al., 2008; Kalichman et al., 2010). In this study we conducted unannounced phone based pill counts using study-provided free cell phones. Following an office-based interview that included a full accounting of all prescription medications and training in the pill counting procedure, participants were called at three unscheduled times over 12 to 16 day intervals. The first of the three pill counts is used to establish the initial number of pills in possession with the subsequent two pill counts allowing for calculation of adherence, defined as the ratio of pills counted relative to pills prescribed, taking into account the number of pills dispensed. Adherence was calculated as the mean across antiretroviral medications and across pill counts. For descriptive analyses, suboptimal adherence was categorically defined by 80% of medications taken as prescribed, a level of adherence that places patients at risk for developing HIV treatment resistance (Bangsberg & Deeks, 2002; Lima et al., 2010; Parienti et al., 2013). Continuous adherence values were used as the dependent variable in regression models.
Data Analyses
Descriptive analyses first compared participants with less than or equal to 80% adherence to those with adherence greater than 80% (Parienti et al., 2013). Descriptive comparisons were performed for demographic and health characteristics, race-based medical mistrust, and medication beliefs. Statistical significance was tested using chi-square contingency tables for categorical variables and independent t-tests for continuous measures. We also examined the associations of continuous ART adherence with health markers, race-based medical mistrust, and medication beliefs. Bivariate correlations were calculated using Pearson correlation coefficients.
To test our main hypothesis that beliefs about medication necessity and concerns would mediate the association between race-based medical mistrust and ART adherence, we tested a multiple mediation model (Baron & Kenny, 1986) using SPSS mediation model macro designed by Preacher and Hayes (2008). This macro estimates paths for the effects of the predictor variable (medical mistrust) on the mediator variables (medication beliefs, the a paths), the effect of the mediators (medication beliefs) on the outcome (medication adherence, the b paths), and the effects of the predictor (medical mistrust) on the outcome (adherence, the c path). We computed 95% confidence intervals (CI) for the indirect effects of race-based medical mistrust on ART adherence through medication beliefs estimated from 5,000 bootstrap resamples. We included participant education, years since testing HIV positive HIV-related symptoms and medication side-effects as control variables in the model. There were no missing data for any variables included in the model. All analyses used p < .05 to define statistical significance.
Results
Table 1 shows the characteristics of the sample partitioned by adherence less than or equal to 80% of ART taken in the previous month. Overall, one in three (n=61) participants were less than or equal to 80% adherent and 30% had detectable viral loads. As expected, participants who demonstrated greater adherence were significantly more likely to be aware of their viral load, of older age, and held greater medication necessity beliefs. Table 2 shows the distribution of responses to the specific medical mistrust items. Overall more than one third of participants held views that reflected race-based medical mistrust, with participants endorsing views that people of their race receive poorer health care and are more likely discriminated against, with relatively fewer participants endorsing items that reflect suspicion of providers intentionally harming persons of their race.
Table 2.
Race-based medical mistrust among people who had ART adherence below and above 80% of pills taken
| Medical Mistrust Belief | Less than or equal to 80% Adherence N = 61 | Greater than 80% Adherence N = 117 | X2 | ||
|---|---|---|---|---|---|
|
| |||||
| N | % | N | % | ||
| People of my race cannot trust doctors and health care workers | |||||
| Strongly Agree | 4 | 7 | 6 | 5 | 4.4 |
| Agree | 15 | 25 | 15 | 14 | |
| Disagree | 24 | 40 | 48 | 41 | |
| Strongly Disagree | 17 | 28 | 46 | 40 | |
| People of my race should be suspicious of information from doctors and health care workers | |||||
| Strongly Agree | 2 | 3 | 6 | 5 | 5.0 |
| Agree | 12 | 20 | 24 | 20 | |
| Disagree | 31 | 52 | 41 | 35 | |
| Strongly Disagree | 15 | 25 | 45 | 38 | |
| People of my race should not confide in doctors and health care workers because it will be used against them | |||||
| Strongly Agree | 0 | 0 | 1 | 1 | 1.50 |
| Agree | 5 | 8 | 8 | 7 | |
| Disagree | 31 | 52 | 52 | 45 | |
| Strongly Disagree | 24 | 40 | 55 | 47 | |
| People of my race should be suspicious of medicine | |||||
| Strongly Agree | 3 | 5 | 8 | 7 | 3.2 |
| Agree | 13 | 22 | 20 | 17 | |
| Disagree | 27 | 45 | 41 | 35 | |
| Strongly Disagree | 17 | 28 | 47 | 40 | |
| Doctors and health care workers do not take the medical complaints of people of my race seriously | |||||
| Strongly Agree | 3 | 5 | 6 | 5 | 3.0 |
| Agree | 7 | 12 | 21 | 18 | |
| Disagree | 30 | 51 | 44 | 38 | |
| Strongly Disagree | 19 | 32 | 46 | 39 | |
| People of my race are treated the same as people of other groups by doctors and health care workers | |||||
| Strongly Agree | 10 | 17 | 10 | 9 | 3.0 |
| Agree | 10 | 17 | 23 | 20 | |
| Disagree | 22 | 37 | 46 | 39 | |
| Strongly Disagree | 16 | 27 | 38 | 33 | |
| People of my race receive the same medical care from doctors and health care workers as people from other groups | |||||
| Strongly Agree | 7 | 12 | 8 | 7 | 2.0 |
| Agree | 12 | 21 | 21 | 18 | |
| Disagree | 23 | 40 | 48 | 41 | |
| Strongly Disagree | 16 | 28 | 41 | 35 | |
| In most hospitals, people of my race don’t receive as good of care as people of other races. | |||||
| Strongly Agree | 7 | 12 | 10 | 9 | 3.6 |
| Agree | 21 | 36 | 37 | 32 | |
| Disagree | 21 | 36 | 36 | 31 | |
| Strongly Disagree | 9 | 15 | 33 | 28 | |
Bivariate correlations
Pearson correlation coefficients among measures of participant characteristics, medical mistrust, medication beliefs and ART adherence are shown in Table 3. Results indicated that ART adherence was significantly associated with medical mistrust, such that greater mistrust was related to poorer adherence. ART adherence was also significantly correlated with medication necessity beliefs, with greater necessity beliefs associated with greater adherence. However, medication concerns beliefs were not significantly correlated with adherence. Medical mistrust was associated with beliefs about medication necessity and concerns in the expected directions. In addition, greater HIV symptoms and ART side-effects were associated with greater beliefs about medication concerns but not beliefs about medication necessity. This pattern of associations supported moving forward with testing the proposed mediation model.
Table 3.
Correlations among measures of health characteristics, medical mistrust, medication beliefs, and ART adherence.
| Race-Based Medical Mistrust | Medication Necessity Beliefs | Medication Concerns Beliefs | ART Adherence | Years Education | Years Since Testing HIV+ | Medication Side-Effects | ||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Medication Necessity Beliefs | −.14+ | |||||||
| Medication Concerns Beliefs | .40** | −.03 | ||||||
| ART Adherence | −.15* | .19** | −.10 | |||||
| Years Education | .01 | −.02 | .06 | −06 | ||||
| Years Since Testing HIV+ | −.09 | −.02 | −.01 | .05 | −.02 | |||
| Medication Side-Effects | .12 | −.03 | .21** | −.13 | −.04 | −.08 | ||
| HIV Symptoms | .04 | −.02 | .19** | −.08 | .05 | −.06 | .45** | |
Note:
p < 10
p < .05
p < 01
Medication beliefs as a mediator of the medical mistrust - adherence relationship
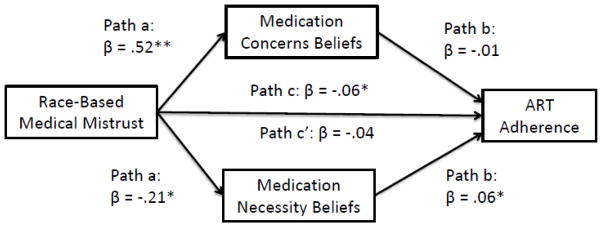
Results of the paths tested in the mediation regression model are shown in Figure 1. The full model accounted for 7.2% of the variance in ART adherence. Results showed medical mistrust significantly predicted medication necessity beliefs, β = −0.21, t = 2.3, p < .02 and medication concerns beliefs, β = 0.52, t = 5.5, p < .01, see Figure 1, a paths. In addition, the direct effect of medication necessity beliefs on ART adherence was significant, β = .06, t = 2.17, p < .05, but medication concerns beliefs did not predict adherence, β = −.01, t = 0.39, n.s., see b paths. The total effect of medical mistrust on adherence was also significant, β = .−0.06, t = 1.98, p < .05, see c path. Accounting for medication beliefs resulted in a non-significant association between medical mistrust and medication adherence, β = −0.04, t = 1.29, p > .1, see c’ path. Based on 5,000 bootstrap resamples, the test of indirect effects of medical mistrust on adherence through medication beliefs was significant, unstandardized b = −0.01, 95%CI: −0.037 to −0.001. Medication concerns beliefs did not significantly contribute to the mediation, b = −0.01, 95%CI: −0.038 to 0.024. Education, years since testing HIV positive, medication side-effects, and HIV symptoms were included as control variables and did not significantly contribute to the model. Thus, results showed that medication necessity beliefs partially mediated the association between race based-medical mistrust and ART adherence.
Figure 1.
Medication beliefs mediate the association between medical mistrust and adherence to antiretroviral therapy.
Discussion
Using 80% of pills taken to descriptively define ART adherence, we found that one in three participants failed to meet this lower-bound threshold, placing individuals at considerable risk for developing drug resistant virus (Bangsberg & Deeks, 2002). Participants with poor adherence were somewhat younger and less likely to be aware of their most recent viral load test results. The less likely participants were to believe their medications were necessary the poorer their adherence. Medical mistrust was common in our sample, with between 15% and 30% of participants endorsing beliefs that people of their race are discriminated against and receive poorer care. Although individual race-based medical mistrust items did not differentiate participants with relatively poorer and better adherence, overall stronger medical mistrust was associated with poorer ART adherence.
The current study results should be interpreted in light of their methodological limitations. The study was conducted in a large metropolitan area of the southeastern United States and may therefore not generalize to other cities or regions. This limitation is particularly important given the potential for medical mistrust to emerge differently among different cultural subgroups. Thus, while other studies conducted in other regions of the United States have found medical mistrust predicts medication adherence (Bogart et al., 2010), it should not be assumed that medication beliefs would mediate this relationship elsewhere. Our sample size was also relatively small, suggesting that the observed mediation model should be tested in a larger and more diverse sample. In addition, we included a small number of Hispanic and no other minorities in our sample, and the number was too small to allow us to examine differences among minority groups. Restricting our sample to racial and ethnic minorities was also a limitation. While African Americans are relevant to questions of medical mistrust and medication adherence, our study should not be interpreted as suggesting that mistrust of health care systems is unique to African Americans, Hispanics or any minority group. Our results are also limited by addressing medications and beliefs about medications in general rather than addressing a specific class of medications because greater specificity may increase the implications for interventions. Finally, our model accounted for a small amount of variance in medication adherence. While this finding replicates past research, and therefore appears reliable, the modest amount of variance accounted for suggests that the model may be of limited clinical utility in and of itself. Addressing medication beliefs to improve ART adherence in the context of medical mistrust should therefore occur within a broader approach to adherence improvement that addresses multiple factors known to impede adherence.
Another limitation of the study is that we measured medical mistrust at the same time point as medication beliefs, prohibiting us from drawing causal conclusions regarding the association between mistrust and medication beliefs. We also cannot rule out other (i.e., third) variables as explanations for our results. In addition to the possibility that medication beliefs may undermine medical trust, or vice versa, it is possible that other variables not measured in this study may account for the association. In addition, our measure of medical mistrust was not specific to participants’ current providers and therefore reflects a more general perception of racism and discrimination in health care systems. With these limitations in mind, the current study findings have implications for improving HIV treatment adherence in people who mistrust health care systems.
Medical mistrust is rooted in historical facts of abuse, neglect, and mistreatment of racial and ethnic minorities by public health services and health care more generally. Although no longer structurally sanctioned there remain health care disadvantages between racial, ethnic and economic subgroups, as reflected in widespread health disparities (Pellowski, Kalichman, Matthews, & Adler, 2013; Simoni et al., 2012). The degree to which racism and anti-immigration sentiments infiltrate health care will also have corrosive effects on patient trust. It is therefore not surprising that medical mistrust is associated with poor treatment retention, adherence and outcomes (Bogart et al., 2010).
Our findings suggest that there are intermediating variables that may serve as viable targets for interventions to improve adherence among mistrusting patients. We showed that beliefs about medication necessity at least in part account for the relationship between medical mistrust and medication adherence. Simply put, when patients perceived their medications as necessary they were more adherent even if they mistrusted the health care system in general. Medications beliefs stem from patient experiences with treatments or indirectly through social interactions. A commonsense approach to medication adherence posits that patients are motivated to take medications when the perceived necessity of treatment outweighs the perceived concerns (Horne, 1999). Patients are therefore motivated to adhere when they believe medications will effectively treat disease or ameliorate symptoms. Conversely, concerns over side-effects, long-term dependence, and costs associated with medications are demotivating. Medication beliefs are amenable to change through well-established educational and motivational interventions (Kalichman et al., 2011; Reynolds et al., 2008). Research is needed to determine whether addressing medication beliefs among patients who mistrust the medical care system can improve medication adherence and health outcomes.
Acknowledgments
This research was supported by National Institute of Nursing Research Grant R01-NR012962 National Institute of Alcohol Abuse and Alcoholism Grant R01-AA021471 and the National Institute on Drug Abuse Grant R01-DA033067.
References
- Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes. 2001;28(1):47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- Bangsberg D, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? Jounal of General Internal Medicine. 2002;17(10):812–813. doi: 10.1046/j.1525-1497.2002.20812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Wagner G, Galvan FH, Banks D. Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among african american men with HIV. Journal of Acquired Immune Deficiency Syndromes. 2010;53(5):648–655. doi: 10.1097/QAI.0b013e3181c57dbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrieri MP, Villes V, et al. Self-reported side-effects of anti-retroviral treatment among IDUs: a 7-year longitudinal study (APROCO-COPILOTE COHORT ANRS CO-8) International Journal of Drug Policy. 2007;18(4):288–295. doi: 10.1016/j.drugpo.2007.01.014. [DOI] [PubMed] [Google Scholar]
- Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. Journal of General Internal Medicine. 2007;22(3):389–395. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale SK, Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Medical mistrust is related to lower longitudinal medication adherence among African-American males with HIV. Journal of Health Psychology. 2014 Oct 7; doi: 10.1177/1359105314551950. pii: 1359105314551950. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earl TR, Beach MC, Lombe M, Korthuis PT, Sharp VL, Cohn JA, … Saha S. Race, Relationships and Trust in Providers among Black Patients with HIV/AIDS. Social Work Research. 2013;37(3):219–226. doi: 10.1093/swr/svt017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredericksen R, Feldman BJ, Brown T, Schmidt S, Crane PK, Harrington RD, … Crane HM. Unannounced telephone-based pill counts: a valid and feasible method for monitoring adherence. AIDS and Behavior. 2014;18(12):2265–2273. doi: 10.1007/s10461-014-0916-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaston GB, Alleyne-Green B. The impact of African Americans’ beliefs about HIV medical care on treatment adherence: a systematic review and recommendations for interventions. AIDS and Behavior. 2013;17(1):31–40. doi: 10.1007/s10461-012-0323-x. [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Penedo FJ, Llabre MM, Duran RE, Antoni MH, Schneiderman N, Horne R. Physical symptoms, beliefs about medications, negative mood, and long-term HIV medication adherence. Annals of Behavioral Medicine. 2007;34(1):46–55. doi: 10.1007/BF02879920. [DOI] [PubMed] [Google Scholar]
- Haberer JE, Robbins GK, Ybarra M, Monk A, Ragland K, Weiser SD, … Bangsberg DR. Real-Time Electronic Adherence Monitoring is Feasible, Comparable to Unannounced Pill Counts, and Acceptable. AIDS and Behavior. 2011;16:375–382. doi: 10.1007/s10461-011-9933-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R. Patients’ beliefs about treatment: the hidden determinant of treatment outcome? Joural of Psychosomatic Research. 1999;47(6):491–495. doi: 10.1016/s0022-3999(99)00058-6. [DOI] [PubMed] [Google Scholar]
- Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PLoS ONE. 2013;8(12):e80633. doi: 10.1371/journal.pone.0080633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R, Cooper V, Gellaitry G, Date HL, Fisher M. Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence: the utility of the necessity-concerns framework. Journal of Acquired Immune Deficiency Syndromes. 2007;45(3):334–341. doi: 10.1097/QAI.0b013e31806910e3. [DOI] [PubMed] [Google Scholar]
- Jonsdottir H, Friis S, Horne R, Pettersen KI, Reikvam A, Andreassen OA. Beliefs about medications: measurement and relationship to adherence in patients with severe mental disorders. Acta Psychiatrica Scandavia. 2009;119(1):78–84. doi: 10.1111/j.1600-0447.2008.01279.x. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Amaral CM, Cherry C, Flanagan JA, Pope H, Eaton L, … Schinazi R. Monitoring Antiretroviral adherence by unannounced pill counts conducted by telephone: Reliability and criterion-related validity. HIV Clinical Trials. 2008;9:298–308. doi: 10.1310/hct0905-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman S, Eaton L, Kalichman M, Cherry C. Medication beliefs mediate the association between medical mistrst and antiretroviral adherence among African-Americans living with HIV. Journa of Health Psychology. 2015 doi: 10.1177/1359105315600239. (epub ahead of print) [DOI] [PubMed] [Google Scholar]
- Kalichman S, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. Journal of Nervous and Mental Disicions. 2000;188(10):662–670. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Amaral C, Swetsze C, Eaton L, Kalichman MO, Cherry C, … Schinazi RF. Monthly unannounced pill counts for monitoring HIV treatment adherence: tests for self-monitoring and reactivity effects. HIV Clinical Trials. 2010;11(6):325–331. doi: 10.1310/hct1106-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Kalichman MO, Cherry C, Swetzes C, Amaral CM, White D, … Eaton L. Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: an initial test of concept trial. AIDS Patient Care STDs. 2011;25(5):303–310. doi: 10.1089/apc.2010.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima VD, Bangsberg DR, Harrigan PR, Deeks SG, Yip B, Hogg RS, Montaner JS. Risk of viral failure declines with duration of suppression on highly active antiretroviral therapy irrespective of adherence level. Journal of Acquired Immune Deficiency Syndromes. 2010;55(4):460–465. doi: 10.1097/QAI.0b013e3181f2ac87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, Holtgrave D. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS and Behavior. 2014;18(1):10–25. doi: 10.1007/s10461-013-0476-2. [DOI] [PubMed] [Google Scholar]
- McFall AM, Dowdy DW, Zelaya CE, Murphy K, Wilson TE, Young MA, … Althoff KN. Understanding the disparity: predictors of virologic failure in women using highly active antiretroviral therapy vary by race and/or ethnicity. Journal of Acquired Immune Deficiency Syndromes. 2013;64(3):289–298. doi: 10.1097/QAI.0b013e3182a095e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison-Beedy D, Carey MP, Tu X. Accuracy of audio computer-assisted self-interviewing (ACASI) and self-administered questionnaires for the assessment of sexual behavior. AIDS and Behavior. 2006;10(5):541–552. doi: 10.1007/s10461-006-9081-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nozaki I, Kuriyama M, Manyepa P, Zyambo MK, Kakimoto K, Barnighausen T. False beliefs about ART effectiveness, side effects and the consequences of non-retention and non-adherence among ART patients in Livingstone, Zambia. AIDS and Behavior. 2013;17(1):122–126. doi: 10.1007/s10461-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parienti JJ, Barrail-Tran A, Duval X, Nembot G, Descamps D, Vigan M, … Goujard C. Adherence profiles and therapeutic responses of treatment-naive HIV-infected patients starting boosted atazanavir-based therapy in the ANRS 134-COPHAR 3 trial. Antimicrob Agents Chemother. 2013;57(5):2265–2271. doi: 10.1128/AAC.02605-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellowski JA, Kalichman SC, Finitsis DJ. Reliability and validity of a single-item rating scale to monitor medication adherence for people living with HIV and lower health literacy. HIV Clin Trials. 2015;16(1):1–9. doi: 10.1179/1528433614Z.0000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the U.S. HIV epidemic. American Psychologist. 2013;68(4):197–209. doi: 10.1037/a0032694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [Research Support, N.I.H., Extramural] [DOI] [PubMed] [Google Scholar]
- Reynolds NR, Testa MA, Su M, Chesney MA, Neidig JL, Frank I, … Robbins GK. Telephone support to improve antiretroviral medication adherence: a multisite, randomized controlled trial. Journal of Acquired Immune Deficiency Syndromes. 2008;47(1):62–68. doi: 10.1097/QAI.0b013e3181582d54. [DOI] [PubMed] [Google Scholar]
- Saha S, Jacobs EA, Moore RD, Beach MC. Trust in physicians and racial disparities in HIV care. AIDS Patient Care STDs. 2010;24(7):415–420. doi: 10.1089/apc.2009.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton RC, Winkel G, Davis SN, Roberts N, Valdimarsdottir H, Hall SJ, Thompson HS. Validation of the group-based medical mistrust scale among urban black men. Journal of General Internal Medicine. 2010;25(6):549–555. doi: 10.1007/s11606-010-1288-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi AE, Hu X, Hall HI. Mortality among blacks or African Americans with HIV infection--United States, 2008–2012. Morbidity and Mortality Weekly Report. 2015;64(4):81–86. [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Huh D, Wilson IB, Shen J, Goggin K, Reynolds NR, … Liu H. Racial/Ethnic disparities in ART adherence in the United States: findings from the MACH14 study. Journal of Acquired Immune Deficiency Syndromes. 2012;60(5):466–472. doi: 10.1097/QAI.0b013e31825db0bd. [DOI] [PMC free article] [PubMed] [Google Scholar]