Recent work in affective science proposes that many forms of emotional symptoms and disorders may be underpinned by a smaller set of transdiagnostic vulnerability processes (Dozois, Seeds, & Collins, 2009; Sauer-Zavala et al., 2012). Within this conceptualization, transdiagnostic vulnerability factors are hypothesized to be “causal, varying, and maintaining factors” for emotional symptoms and disorders (Kraemer et al., 1997). Factors that are intrapersonal and reflect an emotion process appear to be particularly promising for HIV/AIDS research because intrapersonal factors lend themselves well to treatment via behavioral or pharmacologic intervention. Additionally, emotional components of emotional symptoms and disorders (in contrast to somatic, behavioral, or cognitive components) may be most robustly associated with health behavior problems (Leventhal & Zvolensky, 2015).
One such transdiagnostic vulnerability factor is anxiety sensitivity, defined as the extent to which individuals believe anxiety and anxiety-related sensations (e.g., racing heart) have harmful personal consequences (McNally, 2002; Reiss & McNally, 1985). Anxiety sensitivity is a relatively stable, but malleable, factor. The global anxiety sensitivity construct encompasses lower-order fears of physical, mental, and publicly observable experiences (Zinbarg, Barlow, & Brown, 1997). Individuals higher in anxiety sensitivity are more likely to be frightened of harmless heart palpitations because they believe these sensations will lead to cardiac arrest or other feared outcomes, whereas individuals lower in anxiety sensitivity do not fear these same sensations because they believe them to be benign. Empirically, anxiety sensitivity is distinguishable from the tendency to experience more frequent anxiety symptoms (e.g., trait anxiety) and other negative affect propensity variables (e.g., Rapee & Medoro, 1994; Zvolensky, Kotov, Antipova, & Schmidt, 2003).
Theoretically, anxiety sensitivity may be of particular importance among the HIV+ population because of the wide array of interoceptive (e.g., aversive bodily sensations, chronic stress) and exteroceptive (e.g., stigma, discrimination) stressors associated with the disease. To date, a number of studies have examined anxiety sensitivity in relation to negative affect symptoms among Persons Living with HIV/AIDS (PLWHA). For instance, Gonzalez, Zvolensky, Solomon, and Miller (2010) found that among 51 PLWHA (74.5% male, mean age = 45.53), anxiety sensitivity was related to anxiety and depression symptoms, even when controlling for negative affectivity. Other work has found anxiety sensitivity to be associated with a wide variety of aversive internal states, such as anxious arousal, bodily vigilance, and interoceptive fear (Gonzalez, Zvolensky, Grover, & Parent, 2012; Gonzalez, Zvolensky, Parent, Grover, & Hickey, 2012). Additionally, a study of 164 PLWHA demonstrated a link between anxiety sensitivity cognitive concerns and suicidal ideation, above and beyond the effects of demographic variables, CD4 T-cell count, and negative affectivity (Capron, Gonzalez, Parent, Zvolensky, & Schmidt, 2012). Another investigation found that anxiety sensitivity was related to greater HIV symptom severity among 139 PLWHA (Leyro, Vujanovic, & Bonn-Miller, 2015). Together, available work provides initial empirical evidence that anxiety sensitivity is related to negative mood symptoms as well as negative internal physical states among PLWHA.
Non-HIV work has consistently shown that the association between anxiety sensitivity and mental health and health problems is conditional upon a host of moderators, including gender (Zvolensky, Eifert, & Lejuez, 2001), environmental stress (Zvolensky, Kotov, Antipova, & Schmidt, 2005), social determinants of health (Zvolensky et al., 2015), and ethnicity (Talkovsky & Norton, 2015). As one example, the link between anxiety sensitivity and adverse mental health symptoms is stronger in females than males (Feldner, Zvolensky, Schmidt, & Smith, 2008). However, potential moderators in anxiety sensitivity-HIV related work have not yet been explored. Continued identification of theory-based candidate moderators of the anxiety sensitivity-mental health and health behavior relations is important within the HIV+ population because it will help clarify the mechanisms underlying this linkage, and identify individuals who may benefit most for interventions that target this transdiagnostic construct. A maladaptive coping explanation purports that HIV and poorer mental health and physical health problems are related, in part, because emotionally vulnerable persons (e.g., those with higher anxiety sensitivity) engage in unhealthy behavior (e.g., alcohol use, smoking, risky sexual behavior) in an effort to cope with their vulnerability (Brandt et al., 2015). Following from this hypothesis, PLWHA who engage in one such maladaptive health behavior (i.e., smoking) to cope with individual differences in anxiety sensitivity may be more apt to experience more distress, and then, be at greater risk to utilize additional maladaptive health behaviors (e.g., hazardous alcohol use, risky sexual behavior, self-harm) to cope with such amplified distress.
Tobacco use is one such maladaptive health behavior. PLWHA are significantly more apt to smoke compared to the general population. For example, Niaura and colleagues (2000) reported in a critical review of the extant literature that over 70% of HIV+ outpatients smoked on a daily basis. Smoking is commonly cited as a means to cope with aversive mood and counteract fatigue, inactivity, and stress among PLWHA (Grover, Gonzalez, & Zvolensky, 2013). Paradoxically, smoking also is related to poorer mental and physical health over time (Goodwin et al., 2014). Thus, individuals with high anxiety sensitivity who use tobacco as a coping method may be increasing their risk for aversive mental health and physical health symptoms, and may in turn, be placing themselves at a greater risk for other maladaptive health behaviors (e.g., alcohol abuse, risky sexual behavior, and deliberate self-harm) to cope with such distress. This type of perspective is consistent broadly with syndemic models of HIV (Pacek & Crum, 2015). Thus, anxiety sensitivity-health behavior and health outcomes may be particularly robust among smokers compared to non-smokers. This perspective is supported by non-HIV work that has found greater levels of anxiety sensitivity and smoking status (versus non-smoking or greater smoking rate) consistently interact to predict worse mental and physical health outcomes (McLeish, Zvolensky, & Bucossi, 2007; Zvolensky et al., 2003).
Together, the present study evaluated the hypothesis that tobacco use status moderated the relation between anxiety sensitivity and three notable public health problems among PLWHA: hazardous drinking (harmful effects of alcohol use), sexual compulsivity the extent to which they experience sexual behavior as uncontrollable and distressing), and suicidality. Each of these health problems have been found to be common among PLWHA (Benotsch, Kalichman, & Pinkerton, 2001; Keiser et al., 2010; O'Cleirigh et al., 2015) and associated with a variety of negative consequences (Benotsch et al., 2001; Pacek, Harrell, & Martins, 2014; Robertson, Parsons, Van Der Horst, & Hall, 2006). It was hypothesized that smoking status would moderate the role anxiety sensitivity on the dependent variables, such that anxiety sensitivity would be associated with higher rates of hazardous alcohol use, sexual compulsivity, and suicidality among individuals who reported past-month smoking, but not among individuals who did not smoke.
Method
Participants
Participants included 94 adults living with HIV/AIDS recruited from AIDS service organizations. Participants were eligible for inclusion if they were between 18 and 65 years old, were previously diagnosed with HIV/AIDS per self-report, and had the cognitive capacity to give written informed consent, as assessed by their ability to read the consent form and explain the study purpose to assessment personnel. Exclusion criteria included severe suicidality, untreated severe psychological disorders (e.g., Bipolar, schizophrenia), or inability to speak English at a conversational level. The majority of participants (64.5%) were male and the mean age was 48.3 years (SD = 7.5). Ethnically, 54.2% of the sample identified as Black, 29.2% as White/Caucasian, 11.4% as Hispanic, and 5.2% identified as “mixed/other” (e.g., Native American). Although 86.5% reported completion of high school or further education, 77.1% of participants reported current unemployment and 54.2% reported earning less than $10,000 annually. The average CD4 t-cell count within the sample was 552.4 (SD = 277.5; range: 28–1300) and 53.5% self-reported AIDS diagnosis. Past-month smoking was endorsed by 57.3% of the sample, among whom the average number of cigarettes per day was 8.9 (SD = 6.3).
Measures
Demographic (e.g., age, location, sex) and medical information (e.g., HIV/AIDS status, time living with HIV) was self-reported by participants.
M.I.N.I. International Neuropsychiatric Interview 6.0 (MINI; Sheehan et al., 1998)
The MINI is a time-efficient structured diagnostic interview used to index current psychological disorders (e.g., panic disorder, major depressive disorder) based on DSM-IV criteria (APA, 2000). The MINI was utilized to screen for study exclusion criteria, and was administered by trained research personnel under the supervision of an independent doctoral-level rater. The MINI has demonstrated satisfactory inter-rater reliability, test-retest reliability and validity (Sheehan et al., 1998) and has been deemed applicable for use in research settings (Lecrubier et al., 1997). A random selection of interviews (approximately 12%) was checked for accuracy with no cases of diagnostic disagreement noted.
The Timeline Follow-Back Interview (TLFB; Sobell & Sobell, 1992)
TLFB is a calendar-based assessment that was originally developed to assess alcohol use, but has been adapted for other substances, including tobacco (Robinson, Sobell, Sobell, & Leo, 2014). Data on the quantity and frequency of cigarette use was collected using clinician guided retrospective recall. Information about smoking behavior in the past month was utilized in the present study. Participants who indicated not having smoked cigarettes were coded as non-smokers (dummy code = 0) and participants indicating one or more days of cigarette use coded as smokers (dummy code = 1). This method of data collection has been found to have strong psychometric properties for up to 90-days of retrospective recall, including excellent inter-rater reliability, and test–retest reliability, as well as strong convergent validity (Robinson et al., 2014).
Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988)
The PANAS is a 20-item self-report measure on which respondents indicate, on a 5-point Likert-type scale (1 = very slightly or not at all; 5 = extremely), the extent to which they experience a range of different emotions (e.g., “interested”, “nervous”). In the current study, only items indexing negative affect were utilized (PANAS-NA); the subscale displayed good internal consistency (Cronbach's α = .83).
Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007)
The ASI-3 is an 18-item self-report measure on which participants rate the extent to which they concerned about the possible negative consequences of anxiety (e.g. “It scares me when my heart beats fast”) on a Likert-type scale (0 = very little; 4 = very much). In the present study, we utilized the ASI-3 total score (sum of scores for all 18 ASI-3 items; score ranges from 0 to 72). Internal consistency of ASI-3 was excellent (Cronbach’s alpha =.91).
Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993)
The AUDIT is a 10-item self-report measure developed to identify individuals with problematic alcohol use. Scores range from 0 to 30, with higher scores reflecting a greater likelihood of problematic alcohol use. In the current study, the AUDIT hazardous drinking subscale score was used to index levels of risky drinking. Psychometric properties for the AUDIT and its subscales are well documented (e.g., Saunders et al., 1993). In the current investigation, internal consistency for the hazardous drinking subscale was good (Cronbach’s α = .86).
Sexual Compulsivity Scale (SCS; Kalichman & Rompa, 2001)
The SCS is a 10-item self-report questionnaire on which respondents indicate, on a 4-point Likert-type scale (1 = not at all like me; 4 = very much like me) the extent to which they experience sexual behavior as uncontrollable and distressing (e.g., ‘I have to struggle to control my sexual thoughts and behavior.’). The SCS is reliable and valid among persons living with HIV (Kalichman & Rompa, 2001). Consistent with previous research (e.g., Hook, Hook, Davis, Worthington, & Penberthy, 2010), the SCS had good internal consistency in the present sample (Cronbach α = .87).
Beck Scale for Suicide Ideation (BSS; Beck, Kovacs, & Weissman, 1979)
The BSS is a 21-item self-report measure that assesses suicidal thoughts, plans, and attempts in the past week, as well as lifetime suicide attempts. The psychometric properties of the BSS are well-established (de Beurs, Fokkema, de Groot, de Keijser, & Kerkhof, 2015) and the internal consistency of the scale in the current study was found to be good (α = .87).
Procedures
Study procedures were conducted in accordance with the Institutional Review Board. Informed consent was obtained from each participant at the beginning of the research appointment prior to administration of any study assessments. All participants were compensated with $20 in gift cards to a local grocery store. Data for the present investigation was collected between 2012 and 2015.
Analytic Strategy
Bivariate correlations among study variables were evaluated to examine associations between study variables. A series of hierarchical regression analyses were conducted with predictors centered at their respective means. Covariates included sex, race, time living with HIV, and negative affectivity; these were entered in the first step. Anxiety sensitivity and past-month smoking were entered together in the second step. Finally, the interaction of anxiety sensitivity and past-month smoking was entered in the final step. Post-hoc simple slope analyses for significant interaction terms at the two levels of the moderator variable (smoker vs. non-smoker).
Results
Bi-Variate Relations
In the case of missing data, pair-wise deletion was used, resulting in 94 cases for hazardous alcohol use and suicidality, and 77 cases for sexual compulsivity. Descriptive statistics and bivariate correlations are presented in Table 1. Anxiety sensitivity was positively associated with sexual compulsivity (r = .38, p < .01) and suicidality (r = .42, p < .01), but not hazardous drinking (r = .10, p < .05). Smoking status was not associated with any of the criterion variables (r’s from .03 – .21).
Table 1.
Means, standard deviations and bivariate correlations among variables
| Variable |
Mean/n (SD/%) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender (female) | 33 (35.1) | 1 | −.113 | .098 | −.172 | −.180 | .228* | .257* | .197 | −.114 |
| 2. Race (African American) |
52 (55.3) | 1 | −.127 | −.012 | −.088 | −.160 | .023 | −.062 | .058 | |
| 3. Years since HIV diagnosis |
16.5 (8.3) | 1 | −.237* | −.249* | .100 | .148 | −.183 | −.122 | ||
| 4. Negative Affectivity | 23.5 (10.0) | 1 | .677** | −.042 | .133 | .185 | .454** | |||
| 5. Anxiety Sensitivity | 27.6 (18.5) | 1 | −.001 | .103 | .379** | .421** | ||||
| 6. Past-month Smoking | .57 (.49) | 1 | .198 | .206 | .080 | |||||
| 7. Hazardous Drinking | 2.5 (2.5) | 1 | .114 | .232* | ||||||
| 8. Sexual Compulsivity | 14.5 (5.9) | 1 | .340** | |||||||
| 9. Suicidal Symptoms | 3.6 (3.8) | 1 |
p < .05,
p < .01;
Note: Negative Affectivity = Positive and Negative Affect Schedule-Negative Affect subscale score (Watson et al., 1988); Anxiety Sensitivity = Anxiety Sensitivity Index-3 total scale score (Taylor et al., 2007); Past-month Smoking = Timeline Follow-back self-report (0=no, 1=yes) (Sobell & Sobell, 1992); Hazardous Drinking = Alcohol Use Disorders Identification Test-Hazardous Drinking subscale score (Saunders et al., 1993); Sexual Compulsivity = Sexual Compulsivity Scale total scale score (Kalichman & Rompa, 201); Suicidal Symptoms = Beck Scale for Suicide Ideation total scale score (Beck et al., 1979); Gender, race, years since HIV diagnosis, and Negative Affectivity were covariates
Moderation Analyses
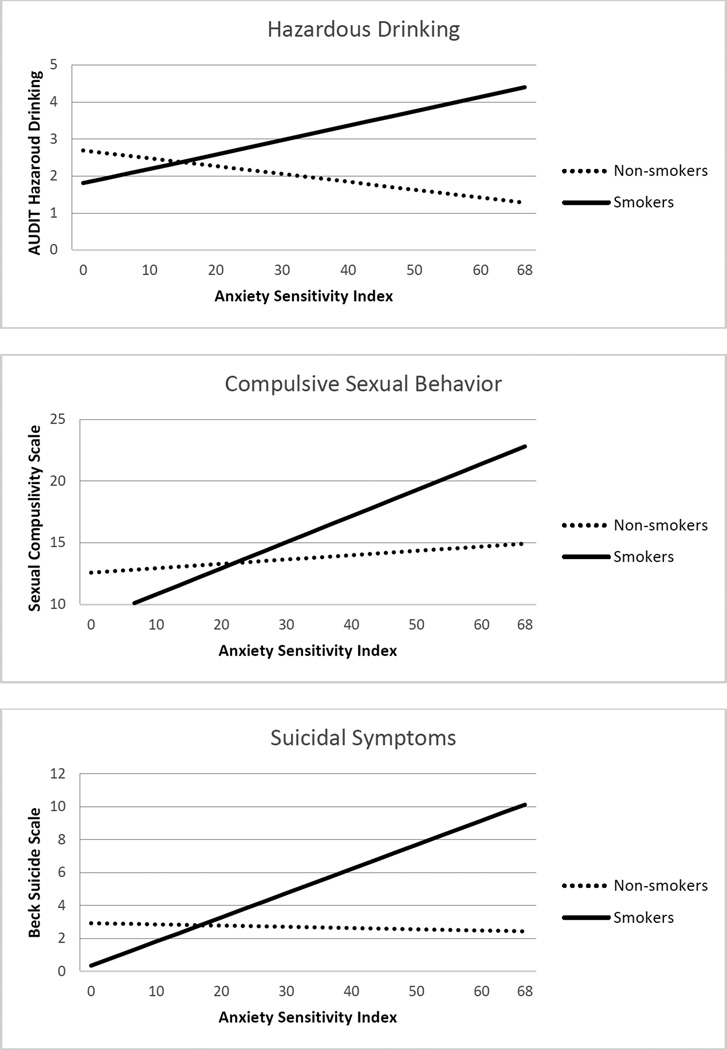
In terms of hazardous alcohol use (n = 94), covariates entered in the first step accounted for a significant amount of variance (R2 = .12, F(4,90) = 3.51, p = .01), with gender and negative affectivity being significant predictors (β =. 29, p = .005; and β = .23, p = .028, respectively). There were no significant main effects for anxiety sensitivity or past-month smoking. As expected, there was a significant interaction between anxiety sensitivity and past-month smoking (β = .456, t = 2.15, p = .035). Simple slope analyses revealed that anxiety sensitivity was positively associated with hazardous alcohol use among individuals who reported past-month smoking (β = .71, p = .041), but not individuals who did not smoke in the past month (β = −.38, p =.39; see Figure 1).
Figure 1.
Plotting the Interactive Effects of Anxiety Sensitivity and Past-month Smoking for the Dependent Variables
In predicting sexual compulsivity (n = 77), covariates entered in the first step accounted for a non-significant amount of variance (R2 = .12, F(4,73) = 2.42, p = .06), with gender being a significant predictor (β = .26, p = .031). There was a significant main effect for anxiety sensitivity (β = .43, p = .004), but not past-month smoking. As expected, there was also a significant interaction between anxiety sensitivity and past-month smoking (β = .63, t = 2.57, p = .013). Simple slope analyses revealed that anxiety sensitivity was positively associated with sexual compulsivity among individuals who reported past-month smoking (β = 4.52, p < .001), but not individuals who did not smoke in the past month (β = .67, p = .55; see Figure 1).
In regard to suicidal symptoms (n = 94), covariates entered in the first step accounted for a significant amount of variance (R2 = .21, F(4,90)= 6.14, p < .001), with negative affectivity being a significant predictor (β = .45, p < .001). There were no significant main effects for anxiety sensitivity or past-month smoking. As hypothesized there was a significant interaction between anxiety sensitivity and past-month smoking (β = .44, p = .030). Simple slope analyses revealed that anxiety sensitivity was positively associated with suicidality among individuals who had reported past-month smoking (β = 2.6, p = .01), but not individuals who did not smoke in the past month (β = -.13, p = .91; see Figure 1).
Discussion
Previous investigations utilizing non-HIV+ samples have found that smoking status moderates the effect of anxiety sensitivity in regard to greater risk for negative emotional symptoms and psychopathology (e.g., anxiety, depression; Zvolensky et al., 2003). The present study extended this literature by examining tobacco use as a novel, theory-based candidate moderator of the anxiety sensitivity-health problem relation among PLWHA in terms of an array of common, clinically significant health problems, including hazardous drinking, sexual compulsivity, and suicidality.
In line with prediction, results indicated that smoking status significantly moderated the predictive influence of anxiety sensitivity in terms of the hazardous drinking, suicidality, and sexual compulsivity. Anxiety sensitivity was significantly and robustly associated with each of the dependent variables among smokers, whereas the corresponding relations among nonsmokers were nonsignificant. Each of these findings remained consistent when adjusting for relevant covariates, including gender, race, years since HIV diagnosis, and negative affectivity. These findings are in accord with transdiagnostic models of smoking comorbidity with mental health and physical health problems (Leventhal & Zvolensky, 2015). Previous investigations among non-HIV+ samples suggest that anxiety sensitivity is associated with greater tendencies to smoke to cope with adverse physical and mental health problems (e.g., Gonzalez, Zvolensky, Vujanovic, Leyro, & Marshall, 2008) and that some of these relations mediate the association between this construct and health problems (Farris, Leventhal, Schmidt, & Zvolensky, 2015). Thus, it is possible that PLWHA who smoke may be especially vulnerable to the effects of anxiety sensitivity. Specifically, individuals with high anxiety sensitivity who use tobacco as a coping method may be increasing their subjective distress, which in turn, could place them at a greater risk for other maladaptive health behaviors (e.g., alcohol abuse, high risk sexual behavior, and deliberate, self-harm) to cope with such amplified distress.
Although the impetus for the present analyses was based on the theoretical position that tobacco use may increase the effect of anxiety sensitivity on health behavior problems among PLWHA, the cross-sectional nature of the study allows for alternative explanations of the present findings. Previous evidence also suggests a prospective effect of smoking on other health behavior problems and disorders among PLWHA (e.g., alcohol dependence; Pacek et al., 2014). As we predicted, it may be that smoking can exacerbate the negative psychological effects of anxiety sensitivity among this group, thereby increasing the likelihood of additional maladaptive (coping) behaviors. Alternatively, smoking may be associated with shared factors that underlie the covariation of anxiety sensitivity and other health behaviors, such as neural abnormalities, genetic factors, and personality traits (e.g., impulsivity, negative urgency). In either case, it is interesting that the current analyses found little evidence indicating significant main effects of anxiety sensitivity or smoking status on the studied dependent variables. The sole exception being that anxiety sensitivity was significantly related to greater sexual compulsivity. These data highlight that the interplay of smoking and anxiety sensitivity is more impactful than their singular influence in terms of hazardous drinking, sexual compulsivity, and suicidality. Such findings generally suggest that it is important to consider the health-related impact of these behavioral mechanisms (anxiety sensitivity and smoking) in terms of the complex and interacting systems in which they function.
This study had several limitations, including a cross-sectional correlational design, self-report of smoking status (no biochemical verification of tobacco use or measure of nicotine dependence), lack of data on underlying mechanisms (e.g., coping responses to negative mood states), and absence of additional measures of other health behavior problems common among PLWHA (e.g., medication adherence, high risk sexual behavior). Despite limitations, this study had several offsetting strengths, such as the use of multiple dependent variables, psychometrically sound instruments, and adjustment for numerous extraneous confounding and explanatory variables.
To our knowledge, this is the first study to examine whether smoking moderates the association between anxiety sensitivity and numerous health behavior problems among PLWHA. The unique moderational relation demonstrated herein warrants future investigation as it points to putative etiological mechanisms that could account for the relation between anxiety sensitivity and adverse health outcomes among PLWHA. Additional clarification of the temporal and causal nature of this moderational relation using longitudinal and experimental research designs would be informative. In addition, future investigations directly measuring additional maladaptive health behaviors, such as diet and physical inactivity, in addition to affective coping patterns as potential mechanisms explaining our findings would be useful for understanding the etiological processes linking anxiety sensitivity and negative health outcomes among this population. Such research could also have implications for matching interventions to patients with individual difference factors that predict unfavorable/favorable treatment response. For example, the present findings may suggest that interventions which target anxiety sensitivity and smoking in an integrative fashion may be useful in offsetting the risk for other health problems among PLWHA, as has been found among non PLWHA samples (Smits et al., in press; Zvolensky et al., 2014).
Table 2.
Main and Interactive Effects of Anxiety Sensitivity and Past-month Smoking in Predicting the Dependent Variables
|
Hazardous Alcohol Use | ||||
|---|---|---|---|---|
| β | t | p |
R2 Change |
|
| Step 1 | .12* | |||
| Gender | .288 | 2.880 | .005 | |
| Race | .082 | .823 | .413 | |
| Years since diagnosis | .184 | 1.812 | .073 | |
| Negative Affectivity | .227 | 2.233 | .028 | |
| Step 2 | .03 | |||
| Anxiety Sensitivity | .093 | .686 | .495 | |
| Past-month Smoking | .144 | 1.423 | .158 | |
| Step 3 | .04* | |||
| Anxiety Sensitivity × Past-month Smoking |
.456 | 2.145 | .035 | |
| Sexual Compulsivity | ||||
| β | t | p |
R2 Change |
|
| Step 1 | .12 | |||
| Gender | .258 | 2.203 | .031 | |
| Race | −.072 | −.616 | .540 | |
| Years since diagnosis | −.197 | −1.645 | .105 | |
| Negative Affectivity | .184 | 1.548 | .126 | |
| Step 2 | .12** | |||
| Anxiety Sensitivity | .431 | 2.992 | .004 | |
| Past-month Smoking | .092 | .790 | .433 | |
| Step 3 | .07* | |||
| Anxiety Sensitivity × Past-month Smoking |
.632 | 2.565 | .013 | |
| Suicidal Symptoms | ||||
| β | t | p |
R2 Change |
|
| Step 1 | .21*** | |||
| Gender | −.029 | −.307 | .760 | |
| Race | .059 | .627 | .532 | |
| Years since diagnosis | −.006 | −.057 | .955 | |
| Negative Affectivity | .448 | 4.613 | < .001 | |
| Step 2 | .04 | |||
| Anxiety Sensitivity | .215 | 1.687 | .095 | |
| Past-month Smoking | .117 | 1.223 | .225 | |
| Step 3 | .04* | |||
| Anxiety Sensitivity×Past-month Smoking |
.443 | 2.211 | .030 | |
Note:
p<.05,
p<.01
p<.001.
Negative affectivity = Positive and Negative Affect Schedule- Negative Affect Subscale (Watson et al., 1988); Anxiety Sensitivity = Anxiety Sensitivity Indx-3 (Taylor et al., 2007); Past-month Smoking = Timeline Followback self-report (0=no, 1=yes) (Sobell & Sobell, 1992); Hazardous Drinking = Alcohol Use Disorders Identification Test-Hazardous drinking sub-scale (Saunders et al., 1993); Sexual Compulsivity = Sexual compulsivity sub-scale (Kalichman & Rompa, 2001); Suicidal Symptoms = Beck Scale for Suicide Ideation (Beck et al., 1979)
References
- APA. Diagnostic and statistical manual of mental disorders (4th ed., text rev.) Washington, DC: 2000. [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Kalichman SC, Pinkerton SD. Sexual compulsivity in HIV-positive men and women: Prevalence, predictors, and consequences of high-risk behaviors. Sexual Addiction & Compulsivity. 2001;8(2):83–99. [Google Scholar]
- Brandt CP, Zvolensky MJ, Vujanovic AA, Grover KW, Hogan J, Bakhshaie J, Gonzalez A. The mediating role of anxiety sensitivity in the relation between avoidant coping and posttraumatic stress among trauma-exposed HIV+ individuals. Psychol Trauma. 2015;7(2):146–153. doi: 10.1037/a0037236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capron DW, Gonzalez A, Parent J, Zvolensky MJ, Schmidt NB. Suicidality and anxiety sensitivity in adults with HIV. AIDS Patient Care and STDs. 2012;26(5):298–303. doi: 10.1089/apc.2011.0429. [DOI] [PubMed] [Google Scholar]
- Catalan J, Harding R, Sibley E, Clucas C, Croome N, Sherr L. HIV infection and mental health: Suicidal behaviour—Systematic review. Psychology, Health & Medicine. 2011;16(5):588–611. doi: 10.1080/13548506.2011.582125. [DOI] [PubMed] [Google Scholar]
- de Beurs DP, Fokkema M, de Groot MH, de Keijser J, Kerkhof AJFM. Longitudinal measurement invariance of the Beck Scale for Suicide Ideation. Psychiatry Research. 2015;225(3):368–373. doi: 10.1016/j.psychres.2014.11.075. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Seeds PM, Collins KA. Transdiagnostic approaches to the prevention of depression and anxiety. Journal of Cognitive Psychotherapy. 2009;23(1):44–59. [Google Scholar]
- Farris SG, Leventhal AM, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and pre-cessation smoking processes: Testing the independent and combined mediating effects of negative affect–reduction expectancies and motives. Journal of Studies on Alcohol and Drugs. 2015;76(2):317–325. doi: 10.15288/jsad.2015.76.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky MJ, Schmidt NB, Smith RC. A prospective test of anxiety sensitivity as a moderator of the relation between gender and posttraumatic symptom maintenance among high anxiety sensitive young adults. Depress Anxiety. 2008;25(3):190–199. doi: 10.1002/da.20281. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Grover KW, Parent J. The role of anxiety sensitivity and mindful attention in anxiety and worry about bodily sensations among adults living with HIV/AIDS. Behavior Therapy. 2012;43(4):768–778. doi: 10.1016/j.beth.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Parent J, Grover KW, Hickey M. HIV symptom distress and anxiety sensitivity in relation to panic, social anxiety, and depression symptoms among HIV-positive adults. AIDS Patient Care and STDs. 2012;26(3):156–164. doi: 10.1089/apc.2011.0309. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Solomon SE, Miller CT. Exploration of the relevance of anxiety sensitivity among adults living with HIV/AIDS for understanding anxiety vulnerability. J Health Psychol. 2010;15(1):138–146. doi: 10.1177/1359105309344898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, Marshall EC. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. Journal of Psychiatric Research. 2008;43(2):138–147. doi: 10.1016/j.jpsychires.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Wall MM, Choo T, Galea S, Horowitz J, Nomura Y, Hasin DS. Changes in the prevalence of mood and anxiety disorders among male and female current smokers in the United States: 1990–2001. Ann Epidemiol. 2014;24(7):493–497. doi: 10.1016/j.annepidem.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover KW, Gonzalez A, Zvolensky MJ. HIV symptom distress and smoking outcome expectancies among HIV + smokers: A pilot test. AIDS Patient Care and STDs. 2013;27(1):17–21. doi: 10.1089/apc.2012.0333. [DOI] [PubMed] [Google Scholar]
- Hook JN, Hook JP, Davis DE, Worthington EL, Jr, Penberthy JK. Measuring sexual addiction and compulsivity: a critical review of instruments. J Sex Marital Ther. 2010;36(3):227–260. doi: 10.1080/00926231003719673. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. The Sexual Compulsivity Scale: further development and use with HIV-positive persons. J Pers Assess. 2001;76(3):379–395. doi: 10.1207/S15327752JPA7603_02. [DOI] [PubMed] [Google Scholar]
- Keiser O, Spoerri A, Brinkhof MWG, Hasse B, Gayet-Ageron A, Tissot F, Egger M. Suicide in HIV-infected individuals and the general population in Switzerland, 1988–2008. The American Journal of Psychiatry. 2010;167(2):143–150. doi: 10.1176/appi.ajp.2009.09050651. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Archives of General Psychiatry. 1997;54(4):337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, Dunbar GC. The Mini International Neuropsychiatric Interview (MINI): A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–231. [Google Scholar]
- Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull. 2015;141(1):176–212. doi: 10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Vujanovic AA, Bonn-Miller MO. Examining associations between cognitive-affective vulnerability and HIV symptom severity, perceived barriers to treatment adherence, and viral load among HIV-positive adults. International Journal of Behavioral Medicine. 2015;22(1):139–148. doi: 10.1007/s12529-014-9404-8. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, Bucossi MM. Interaction between smoking rate and anxiety sensitivity: relation to anticipatory anxiety and panic-relevant avoidance among daily smokers. J Anxiety Disord. 2007;21(6):849–859. doi: 10.1016/j.janxdis.2006.11.003. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52(10):938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Niaura R, Shadel WG, Morrow K, Tashima K, Flanigan T, Abrams DB. Human immunodeficiency virus infection, AIDS, and smoking cessation: the time is now. Clinical Infectious Diseases. 2000;31(3):808–812. doi: 10.1086/314048. [DOI] [PubMed] [Google Scholar]
- O'Cleirigh C, Magidson JF, Skeer MR, Mayer KH, Safren SA. Prevalence of psychiatric and substance abuse symptomatology among HIV-infected gay and bisexual men in HIV primary care. Psychosomatics: Journal of Consultation and Liaison Psychiatry. 2015;56(5):470–478. doi: 10.1016/j.psym.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cleirigh C, Valentine SE, Pinkston M, Herman D, Bedoya CA, Gordon JR, Safren SA. The unique challenges facing HIV-positive patients who smoke cigarettes: HIV viremia, art adherence, engagement in HIV care, and concurrent substance use. AIDS and Behavior. 2015;19(1):178–185. doi: 10.1007/s10461-014-0762-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacek LR, Crum RM. A review of the literature concerning HIV and cigarette smoking: Morbidity and mortality, associations with individual- and social-level characteristics, and smoking cessation efforts. Addiction Research & Theory. 2015;23(1):10–23. doi: 10.3109/16066359.2014.920013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacek LR, Harrell PT, Martins SS. Cigarette smoking and drug use among a nationally representative sample of HIV- positive individuals. The American Journal on Addictions. 2014;23(6):582–590. doi: 10.1111/j.1521-0391.2014.12145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Medoro L. Fear of physical sensations and trait anxiety as mediators of the response to hyperventilation in nonclinical subjects. J Abnorm Psychol. 1994;103(4):693–699. doi: 10.1037//0021-843x.103.4.693. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretcial issues in behavior therapy. San Diego, CA: Academic Press; 1985. [Google Scholar]
- Robertson K, Parsons TD, Van Der Horst C, Hall C. Thoughts of death and suicidal ideation in nonpsychiatric human immunodeficiency virus seropositive individuals. Death Stud. 2006;30(5):455–469. doi: 10.1080/07481180600614435. [DOI] [PubMed] [Google Scholar]
- Robinson SM, Sobell LC, Sobell MB, Leo GI. Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychology of Addictive Behaviors. 2014;28(1):154–162. doi: 10.1037/a0030992. [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Boswell JF, Gallagher MW, Bentley KH, Ametaj A, Barlow DH. The role of negative affectivity and negative reactivity to emotions in predicting outcomes in the unified protocol for the transdiagnostic treatment of emotional disorders. Behav Res Ther. 2012;50(9):551–557. doi: 10.1016/j.brat.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Smits JAJ, Zvolensky MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, Powers MB, Frierson GM, Otto MW, Hopkins LB, Brown RA, Baird SO. The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with high anxiety sensitivity: A randomized controlled trial. Psychosomatic Medicine. doi: 10.1097/PSY.0000000000000264. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ, US: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Talkovsky AM, Norton PJ. Anxiety sensitivity across four ethnoracial groups in an undergraduate sample. Cognitive Behaviour Therapy. 2015;44(1):33–43. doi: 10.1080/16506073.2014.953568. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH, Brown TA. Hierarchical structure and general factor saturation of the Anxiety Sensitivity Index: evidence and implications. Psychological Assessment. 1997;9(3):277. [Google Scholar]
- Zvolensky MJ, Bakhshaie J, Garza M, Valdivieso J, Ortiz M, Bogiaizian D, Vujanovic A. Anxiety sensitivity and subjective social status in relation to anxiety and depressive symptoms and disorders among Latinos in primary care. J Anxiety Disord. 2015;32:38–45. doi: 10.1016/j.janxdis.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Bogiaizian D, Salazar PL, Farris SG, Bakhshaie J. An anxiety sensitivity reduction smoking-cessation program for Spanish-speaking smokers (Argentina) Cognitive And Behavioral Practice. 2014;21(3):350–363. [Google Scholar]
- Zvolensky MJ, Eifert GH, Lejuez CW. Offset control during recurrent 20% carbon dioxide-enriched air induction: relation to individual difference variables. Emotion. 2001;1(2):148–165. doi: 10.1037/1528-3542.1.2.148. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Cross cultural evaluation of smokers risk for panic and anxiety pathology: a test in a Russian epidemiological sample. Behav Res Ther. 2003;41(10):1199–1215. doi: 10.1016/s0005-7967(03)00031-7. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Diathesis stress model for panic-related distress: a test in a Russian epidemiological sample. Behav Res Ther. 2005;43(4):521–532. doi: 10.1016/j.brat.2004.09.001. [DOI] [PubMed] [Google Scholar]